Case
We report two cases of 35-year and 25-year-old females presented with visual acuity of 6/60 and 5/60 for the right and left eye on Snellen's chart. On evaluation, both eyes showed central retinal vein occlusion (CRVO) [Figs. 1a and b, 2a and b]. The fundus fluorescein angiography showed delayed venous filling and blocked fluorescence with no evidence of neovascularization [Figs. 1e and 2c]. The optical coherence tomography showed cystoid macular edema (CME) [Figs. 1f and 3a]. Investigations for Case 1 revealed marked iron deficiency anemia and thrombocytosis and for Case 2 showed moderate anemia [Table 1]. On physician evaluation, serum antitissue transglutaminase antibody titers were done due to suspicion of celiac disease (CD), which was highly positive. Upper gastrointestinal endoscopy showed scalloping of duodenal folds and loss of villi and thus duodenal biopsy was performed which showed signs of atrophic villi, decreased villous/crypt ratio (<1.1), and cryptic hyperplasia [Figs. 4a and b] graded as Modified Marsh Grade Type 3c,[1] confirming the diagnosis of CD. The patients were managed with gluten-free diet and iron and folate supplementation and each eye underwent intravitreal bevacizumab (1.25 mg/0.5 ml) for the management of CME which showed improvement in vision, resolution of hemorrhages [Figs. 1b–e and 2d–f], and CME [Figs. 1g, 3b and c] over subsequent follow-ups.
Figure 1.
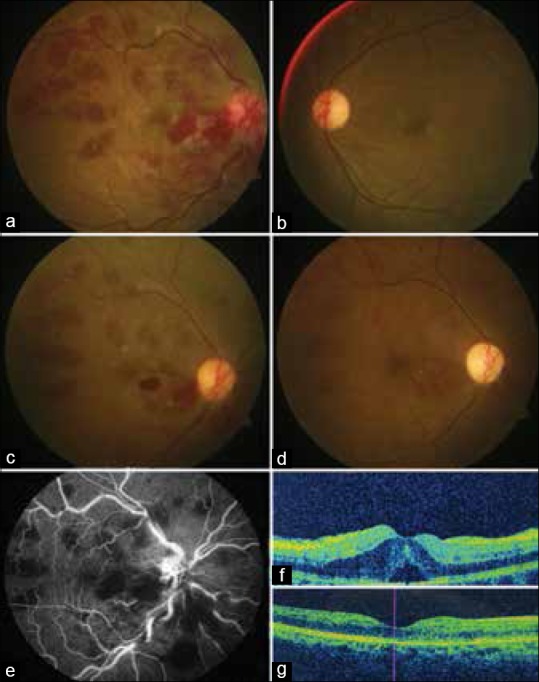
(a and b) Posterior pole fundus photograph of right and left eye at initial presentation, (c and d) images of the right eye at subsequent follow-up at 2 monthly intervals after change of diet plan with regard to celiac disease and subsequent clearing of the retinal hemorrhages; (e) the mid arteriovenous phase of fundus fluorescein angiography shows blocked fluorescence due to hemorrhages; (f) the presence of cystoid macular edema at fovea, and (g) the resolution of cystoid macular edema postintravitreal injection of bevacizumab
Figure 2.
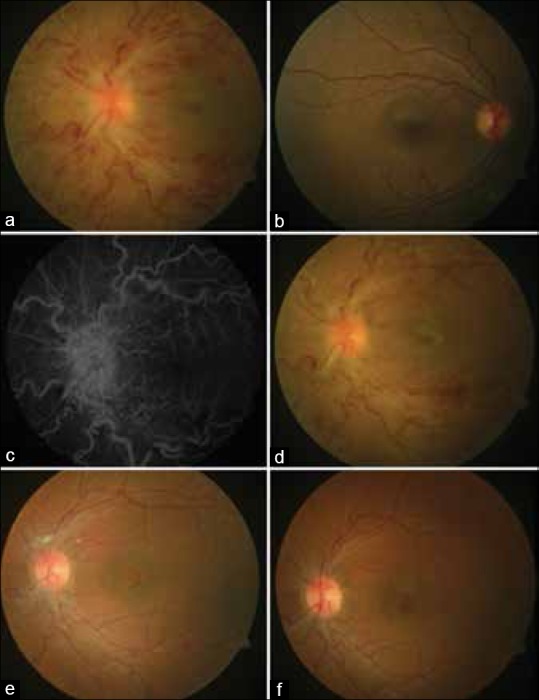
(a and b) Posterior pole fundus photograph of left and right eye at initial presentation, (c) the mid arteriovenous phase of fundus fluorescein angiography increased optic disc vascularity and increased early and late disc fluorescence with blocked fluorescence due to hemorrhages. (d-f) Images of the left eye at subsequent follow-up at 2 monthly intervals after change of diet plan with regard to celiac disease and subsequent clearing of the retinal hemorrhages
Figure 3.
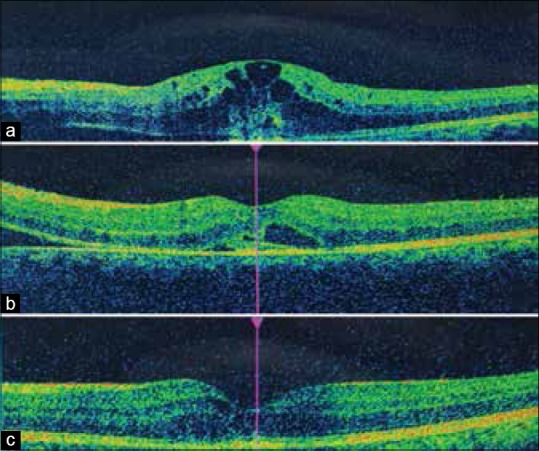
(a) The presence of cystoid macular edema for the second case at initial presentation and (b and c) the subsequent decrease in cystoid macular edema after intravitreal bevacizumab injection
Table 1.
The details of investigation for both Case 1 and Case 2

Figure 4.
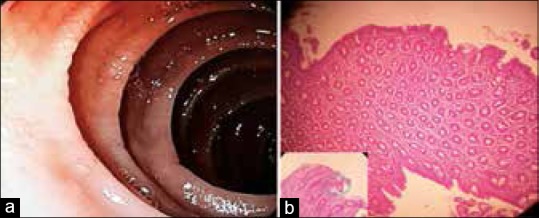
(a) Areas of duodenal erosions with scalloping of duodenal folds and loss of villi, (b) histopathology of duodenal biopsy showing signs of atrophic villi, decreased villous/crypt ratio (<1.1), crypt hyperplasia, increased intraepithelial lymphocytes, and lamina propria showing moderate infiltration with plasma cells, (H and E, ×200)
Discussion
The classic triad of CD: diarrhea, abdominal pain, and malabsorption are seen only in 10%–20% of cases only.[2,3] In India, most cases of CD are in the northern part of country, as wheat is the staple diet. CD patients have a lifelong risk to develop thrombosis. Reported mechanisms for retinal vein occlusion (RVO) include (a) lack of absorption of Vitamin K, deficiencies of protein C and S, antithrombin, Vitamin B12 and folate, (b) hyperhomocysteinemia, and (c) dehydration and hyperviscosity of blood due to malabsorption and chronic diarrhea.[1]
Conclusion
We recommend inclusion of Anti-Ttg titers in young patients presenting with a RVO, as it is a highly sensitive (74%–94%) and specific test (97%–100%)[1] and can save the patient from life-threatening thrombotic complications.[2,3,4]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yachha SK, Poddar U. Celiac disease in India. Indian J Gastroenterol. 2007;26:230–7. [PubMed] [Google Scholar]
- 2.Jomni T, Bellakhal S, Abouda M, Abdelaali I, Douggui H. An atypical presentation of celiac disease: Central retinal vein occlusion. Pan Afr Med J. 2015;22:300. doi: 10.11604/pamj.2015.22.300.8196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee ES, Pulido JS. Nonischemic central retinal vein occlusion associated with celiac disease. Mayo Clin Proc. 2005;80:157. doi: 10.4065/80.2.157. [DOI] [PubMed] [Google Scholar]
- 4.Martins TG, Costa AL, Oyamada MK, Schor P, Sipahi AM. Ophthalmologic manifestations of celiac disease. Int J Ophthalmol. 2016;9:159–62. doi: 10.18240/ijo.2016.01.26. [DOI] [PMC free article] [PubMed] [Google Scholar]


