Abstract
Purpose:
To evaluate the surgical outcome of precision pulse capsulotomy (PPC) in phacoemulsification surgery.
Methods:
One hundred twenty-three eyes of 99 consecutive patients who underwent phacoemulsification with PPC through a 2.8 mm clear corneal incision were prospectively studied at a tertiary care centre. The size, shape of capsulotomy and intraoperative capsulotomy, and surgery-related complications were noted. Visual outcome, IOL stability, and signs of capsular opacification/contraction were evaluated at 3 and 6 months.
Results:
The mean age of patients was 49.5 ± 7.77 years. Complete, circular capsulotomy averaging 5.5 mm diameter was achieved in 117 of 123 eyes. In seven eyes, we experienced complications like capsulorhexis tear (n = 6) and inadvertent iris capture (n = 1). Probe malfunction occurred in six cases. Stable intracapsular intraocular lens (IOLs) fixation and centration was achieved in all eyes. None of the eyes had any significant posterior capsular opacification or capsular contraction at 3 and 6 months. In one eye anterior capsular opacification at the capsulotomy edge was noted at 6 months.
Conclusion:
PPC is a useful device for achieving a perfectly round capsulorrhexis. However, it has a learning curve and chances of skip areas in capsulorhexis, capsular tag, and its extension should be kept in mind. Special care should be taken in initial cases and while operating on eyes with poorly dilating pupil and mature cataracts.
Keywords: Complete circular capsulotomy, complications, precision pulse capsulotomy, surgical outcome
Continuous curvilinear capsulorhexis (CCC) is of utmost importance while performing phacoemulsification and it significantly determines the overall success of cataract surgery.[1] Thus, the need to have a perfectly sized and circular rhexis cannot be overemphasized. It offers various advantages like optimal intraocular lens (IOLs) centration, and reduced chances of posterior capsular opacification.[2,3,4] Manual capsulorhexis is currently the most commonly employed capsulorhexis technique. But it has a substantial learning curve and may not be consistently accurate in size and shape especially in inexperienced hands. All the more, the advent of premium IOLs like multifocal and toric IOLs has necessitated a perfect capsulorhexis.[5,6,7] The risk of capsulorhexis runoff and capsular tags with capsulotomy techniques, endanger the effective placement of these IOLs and further outcome of phacoemulsification surgery. In order to overcome these problems, new technologies like femtosecond and precision pulse capsulotomy (PPC) have been introduced, but they too come with their own set of challenges. Femtosecond laser assisted capsulotomy is precise in terms of the shape and size of the capsulotomy but involves high cost, and increased operative time.[8,9,10,11] In 2017, Mynosys Cellular Devices Inc. (Fremont, CA, USA) developed a PPC, under the trade name “Zepto,” a new capsulotomy technology that works on the principle of converting very fast electrical pulses into mechanical energy in millisecond timeframe.[1]
To the best of our knowledge, a study on PPC has not been published in Indian eyes till date. Thus, we would like to report our initial clinical experience with the use of PPC device. In this article, we have also compared the three different types of capsulorhexis techniques in our setting.
Methods
This was a prospective case study of patients who underwent phacoemulsification with IOL implantation using PPC technique at a tertiary eye care center. We adhered to all tenets of declaration of Helsinki. Institutional Ethics Committee approval was obtained for this study. Informed written consent was taken from all patients preoperatively. Exclusion criteria for our study included patients with preexisting ocular pathologies like preexisting retinal conditions, preexisting glaucoma, subluxated or traumatic cataract, complicated/uveitic cataract, zonulopathies, and patients who did not follow up. All surgeries were performed by two experienced surgeons. Cataract grading was done on slit lamp examination preoperatively. All aseptic precautions were observed and all surgeries were performed under topical anesthesia. Two paracentesis ports were created using a 15 degree lance tip at 3 and 9 o’clock positions. A 2.8 mm clear corneal incision was made superiorly with a disposable keratome in all cases. Trypan blue was used for clear visualization of the anterior capsule in all mature cataract cases and cases with poorly dilating pupil. The PPC device was primed using balanced salt solution and then the slider was extended forward onto the handpiece by the surgeon, thus elongating the PPC tip. The tip was then introduced through the main incision into the anterior chamber filled with ocular viscoelastic, after stabilizing the eye with corneal forceps if required [Fig. 1a]. Once the tip was in the anterior chamber, the push rod was retracted completely and the device re-expanded to its inherent circular shape [Fig. 1b and c]. The PPC tip was then centered over the desired capsulotomy site and controlled suction was applied via the console system [Fig. 1d]. Eventually, a waveform was created that formed the capsulotomy opening [Fig. 1e]. Suction was released and tip was gently removed from the anterior chamber. The free floating anterior capsule was removed and then both the capsule and capsulotomy edge were inspected for any residual tag or tear [Fig. 1f]. Also the size and shape of the capsulotomy edge were observed. Direct chop phacoemulsification was performed using the Stellaris System (Bausch and Lomb). After performing bimanual irrigation and aspiration, single piece aspheric hydrophobic acrylic IOL (AcrySof IQ, Alcon Labs, Fort Worth, TX, USA) implantation was done in all patients.
Figure 1.
Steps of precision pulse capsulotomy. (a) Introduction of the PPC tip into the anterior chamber through main port. (b) Once the tip is completely inserted into the anterior chamber, the push rod is fully retracted. (c and d) Once the suction cup expands, it assumes its circular shape and is placed over the anterior capsule ensuring followed by application of vacuum. (e) Once the vacuum is applied, a waveform is created that forms the capsulotomy opening. (f) The free floating capsule is then removed from the anterior chamber and the capsulotomy is inspected for any tags or tears
In cases of small dilating pupil, soft, flared lip of the silicone suction cup was manipulated under the iris to seal the suction cup onto the capsule. Anterior and posterior lips were slid under the iris one after another, accompanied by a gentle sideways sweeping motion. Care was taken to ensure that the iris does not get trapped in the suction cup.
Patients were followed up at day 1, 2nd week, 3rd, and 6th months. Best-corrected visual acuity (BCVA), central macular thickness (CMT) on optical coherence tomography (OCT), endothelial cell count, capsulotomy edge, posterior capsular opacification, anterior capsular opacification/contraction, IOL stability, and centration were evaluated at 3rd and 6th months.
We also compared our results of PPC with patients who underwent manual capsulotomy and femtosecond assisted capsulotomy with similar grade of cataract and demographic characteristics.
Results
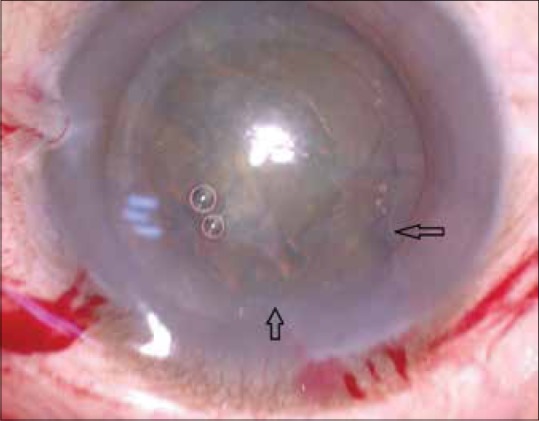
This study comprised of 140 eyes of 119 patients. We evaluated 123 eyes of 99 patients after excluding 17 eyes of 17 patients who lost follow-up. The mean age was 49.5 (±7.77) years with a range of 30–81 years [Table 1]. There were 43 males and 56 females in this study. The cataract grade was nuclear sclerosis (NS) I in 31 eyes, NS II in 55 eyes, NS III in 11eyes, NS IV in 12 eyes, and mature cataract in 14 eyes. Of 123 eyes, 16 eyes had a pupil diameter of 4–5 mm. Rest all eyes were dilated beyond 5 mm. The mean effective phaco time of our patients was 13.09 (±3.71) seconds. Postoperatively BCVA improved to 6/9 or better in all patients. The mean preoperative IOP was 15.21 ± 2.85 mm Hg and mean postoperative IOP was 15.65 ± 2.65 mm Hg. The mean preoperative endothelial cell count was 2,462.73 ± 311.64 and mean postoperative endothelial cell count was 2,201.59 ± 290.51. The mean preoperative CMT was 254.96 (±11.90) microns and mean postoperative CMT was 258.18 (±11.05) microns at 6 months. None of the patients developed cystoid macular edema. At 6 months, one case developed anterior capsular opacification at the capsulotomy edge [Fig. 2] and none of the eyes had any visually significant posterior capsular opacification or capsular contraction. All cases had well-centered IOL with stable fixation.
Table 1.
Age group of patients
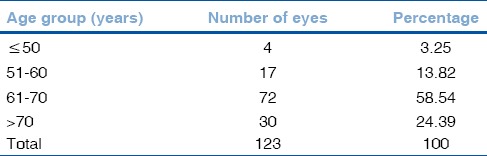
Figure 2.

Anterior capsulotomy opacification is noted at the capsulotomy edge in one patient at 6 months
One hundred seventeen eyes had complete round circular capsulotomy edge without any intraoperative complications. In one case, subincisional iris was inadvertently caught in the suction cup that was released and then the tip was re-introduced resulting in a circular capsulotomy ultimately [Fig. 3]. In five cases the capsulotomy edge was noted to have extended to the periphery subincisionally [Fig. 4]. In one case of mature cataract, a small capsular tag was noted inferiorly and sudden extension of capsulorhexis occured from the capsular tag after removal of irrigation and aspiration cannula [Video 1]. We encountered probe malfunction in six cases. In these cases, while extending the push rod, it penetrated through the silicon cup thus making it nonfunctional. Thus, a new handpiece was used to complete the capsulotomy. The rest of the surgery was uneventful. There was no difficulty observed in hydro dissection, nucleus rotation or cortical clean up, and in none of the patients posterior capsular tear or vitreous loss was encountered.
Figure 3.

Inadvertent iris capture into the suction cup after application of vacuum
Figure 4.
Capsulorhexis extension noted subincisionally in a patient after withdrawal of PPC probe from anterior chamber
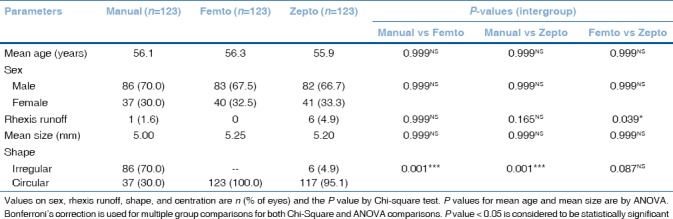
The comparison data of the three techniques of capsulorhexis are presented in Table 2. The distribution of mean age and sex did not differ significantly across the three study groups (P value > 0.05 for all). The distribution of shape differed significantly in manual and Zepto groups (P value < 0.001). It did not differ significantly between femtosecond and Zepto groups (P value > 0.05). The incidence of rhexis runoff was higher in Zepto than manual group but it was not statistically significant. Whereas, it was significantly higher in Zepto compared to femtosecond (P value < 0.05). The distribution of mean size did not differ significantly across the three study groups (P value > 0.05 for all).
Table 2.
Intergroup comparison of parameters studied
Discussion
In the quest of achieving a perfectly sized and circular rhexis, Mynosys developed PPC under the trade name Zepto in 2017. A disposable handpiece is provided along with a console that regulates the vacuum during the procedure. The tip consists of a circular nitinol ring element for a 5.2 mm diameter capsulotomy and is covered by a silicone suction cup that ensures favorable apposition of the ring to the anterior capsular surface. The nitinol alloy has good memory, which ensures adequate deformation of the tip whereas maneuvering through the main incision port. A series of brief fast electrical micropulses create optimum heat to vaporize the water molecules trapped between the anterior capsule and the nitinol ring. The phase transition happens so rapidly that a simultaneous circular anterior capsulotomy is created.[12] This study reports our early clinical experience of PPC in patients undergoing phacoemulsification.
It was Howard Gimbel and Thomas Neuhann, who pioneered the manual capsulorhexis technique that revolutionized the phacoemulsification surgery.[13] Traditionally, surgeons have been successfully performing the manual CCC with needle or forceps but it does have a learning curve. Automated CCC can be performed using the femtosecond laser;[8,9,14,15] however it is expensive, and is difficult to perform in cases with mature cataracts, small pupils, and corneal opacities. Another laser-assisted system “CAPSULaser” has been introduced recently.[16] It is a microscope mounted, noncontact, continuous mode laser system that produces a stronger capsulorhexis with better elasticity.[16] However, it is not yet commercially available.
PPC technique is also an attempt to overcome the pitfalls of performing manual CCC. PPC may be advantageous in challenging case scenarios like mature cataracts, intumescent cataracts, coexisting significant pterygium, and poorly dilating pupils but care must be exercised as the technique is not free of complications. Studies conducted in live rabbits and human cadaver eyes reported that PPC is safe, effective, and produces a stronger capsulotomy edge compared to manual and FLSC technique with no difference in postoperative corneal edema, endothelial cell loss, inflammation, and capsular opacification.[17,18]
First available clinical data in human eyes by Waltz et al. showed that PPC provides consistent, precise capsulotomy during phacoemulsification, in simple as well as challenging cases.[12] They did not report any intraoperative complications. However, the sample size was small (n = 38).
In our initial experience of 123 eyes of 99 patients, successful, circular, free-floating capsulorhexis was achieved in 117 eyes. We faced complications like capsulorhexis runoff (n = 6) and iris capture in the suction cup (n = 1). We believe that inadequate contact of the nitinol ring with anterior capsule in this region may have resulted in skip areas in subincisional area that led to rhexis runoff while pulling out the tip of the device from the anterior chamber. In one case of mature cataract, capsular tag was noted inferiorly and the capsulorhexis extended suddenly at the site of capsular tag due to shallowing of anterior chamber after removal of the irrigation and aspiration cannula. Iris capture also occurred because of inadequate contact of the nitinol ring with anterior capsule and when suction was applied the iris got engaged in the suction cup. It was disengaged by releasing the suction. These complications occurred during the initial cases that may indicate that this technique does have a learning curve. But the learning curve is short as we did not encounter any such complications in further surgeries. Also possible probe malfunction should be kept in mind and a spare probe should be readily available.
The placement of the IOL was stable and well centered in all cases. However, we wish to emphasize the fact that the centration of the ring over the anterior capsule is with relation to the iris rim and also surgeon dependant or manual leading to a few off-centered capsulotomies. But these off-centrations were not significant in relation to IOL centration and stability. To overcome this difficulty, Waltz et al. have recommended placement of the center of the PPC device on the appropriate Purkinje image allowing centration of a PPC capsulotomy on the patient's visual axis.[12] In cases with small pupils, the use of the PPC device is safe because the silicone material forming the suction cup is soft and insulates against heat as shown in a previous study, which reported only a slight temperature change (1 to 2 degrees) immediately adjacent to the suction cup during capsulotomy.[12] At 6 months, we did not encounter any IOL instability, capsular contraction, and PCO that is similar to earlier reports.[17] Although, in one case we observed anterior capsular opacification at the capsulotomy edge at 6 months follow-up.
A study was carried out in human cadaver eyes that tested and compared the tear strength of manual, femtosecond, and presicion pulse capsulotomy.[18] It showed that the strength of the capsulotomy edge was greater in PPC as compared to other two techniques. In our study, we encountered maximum rhexis runoffs in PPC group (4.9%) followed by manual (1.6%) followed by femtosecond (0%) group. The difference between PPC and femtosecond group was statistically significant (P = 0.039). As far as rhexis runoff is concerned, we believe that manual capsulotomy once mastered can give results better than PPC and similar to femtosecond laser assisted capsulotomy. Thus, manual capsulorhexis can still be considered the technique of choice especially where affordability is an issue.
Conclusion
PPC is a useful device for achieving a perfectly round capsulorrhexis. However, the technique has a learning curve and subincisional area can have skip areas leading to torn capsulorhexis. Chances of capsular tag and its extension should also be kept in mind. Special care should be taken in the initial cases and while operating on eyes with poorly dilating pupil, and mature cataract and cataracts with shallow anterior chamber. Future larger clinical studies comparing the manual versus automated capsulotomy techniques in human eyes would help us better understand the long-term safety and efficacy of all these procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.ijo.in
Acknowledgement
We would like to acknowledge the assistance of Dr. Shrivallabh P Sane and Dr. Mehmood G Sayyad, Consultant BioStatistician, NIO, Pune, for statistical analysis.
References
- 1.Chang DF. Zepto precision pulse capsulotomy: A new automated and disposable capsulotomy technology. Indian J Ophthalmol. 2017;65:1411–4. doi: 10.4103/ijo.IJO_737_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Assia EI, Legler UF, Apple DJ. The capsular bag after short-and long-term fixation of intraocular lenses. Ophthalmology. 1995;102:1151–7. doi: 10.1016/s0161-6420(95)30897-4. [DOI] [PubMed] [Google Scholar]
- 3.Ravalico G, Tognetto D, Palomba M, Busatto P, Baccara F. Capsulorhexis size and posterior capsule opacification. J Cataract Refract Surg. 1996;22:98–103. doi: 10.1016/s0886-3350(96)80277-x. [DOI] [PubMed] [Google Scholar]
- 4.Ram J, Pandey SK, Apple DJ, Werner L, Brar GS, Singh R, et al. Effect of in-the-bag intraocular lens fixation on the prevention of posterior capsule opacification. J Cataract Refract Surg. 2001;27:1039–46. doi: 10.1016/s0886-3350(00)00841-5. [DOI] [PubMed] [Google Scholar]
- 5.Liu JW, Haw WW. Optimizing outcomes of multifocal intraocular lenses. Curropinophthalmol. 2014;25:44–8. doi: 10.1097/ICU.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 6.Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35:992–7. doi: 10.1016/j.jcrs.2009.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Altmann GE, Nichamin LD, Lane SS, Pepose JS. Optical performance of 3 intraocular lens designs in the presence of decentration. J Cataract Refract Surg. 2005;31:574–85. doi: 10.1016/j.jcrs.2004.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Kranitz K, Takacs A, Milhaltz K, Kovács I, Knorz MC, Nagy ZZ. Femtosecond laser capsulotomy and manual continuous curvilinear capsulorhexis parameters and their effects on intraocular lens extraction. J Refract Surg. 2011;27:558–63. doi: 10.3928/1081597X-20110623-03. [DOI] [PubMed] [Google Scholar]
- 9.Friedman NJ, Palanker DV, Schuele G, Andersen D, Marcellino G, Seibel BS, et al. Femtosecond laser capsulotomy. J Cataract Refract Surg. 2011;37:1189–98. doi: 10.1016/j.jcrs.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Mastropasqua L, Toto L, Mattei PA, Vecchiarino L, Mastropasqua A, Navarra R, et al. Optical coherence tomography and 3-dimensional confocal structured imaging system–guided femtosecond laser capsulotomy versus manual continuous curvilinear capsulorhexis. J Cataract Refract Surg. 2014;40:2035–43. doi: 10.1016/j.jcrs.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 11.Reddy KP, Kandulla J, Auffarth GU. Effectiveness and safety of femtosecond laser–assisted lens fragmentation and anterior capsulotomy versus the manual technique in cataract surgery. J Cataract Refractive Surg. 2013;39:1297–306. doi: 10.1016/j.jcrs.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 12.Waltz K, Thompson VM, Quesada G. Precision pulse capsulotomy: Initial clinical experience in simple and challenging cataract surgery cases. J Cataract Refract Surg. 2017;43:606–14. doi: 10.1016/j.jcrs.2017.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Gimbel HV, Neuhann T. Continuous curvilinear capsuolorrhexis. J Cataract Refract Surg. 1991;17:110–11. doi: 10.1016/s0886-3350(13)81001-2. [DOI] [PubMed] [Google Scholar]
- 14.Palanker DV, Blumenkranz MS, Andersen D, Wiltberger M, Marcellino G, Gooding P, et al. Femtosecond laser-assisted cataract surgery with integrated optical coherence tomography. SciTransl Med. 2010;2:58ra85. doi: 10.1126/scitranslmed.3001305. [DOI] [PubMed] [Google Scholar]
- 15.Abell RG, Darian- Smith E, Kan JB, Allen PL, Ewe SY, Vote BJ. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: Outcomes and safety in more than 4000 cases at a single centre. J Cataract Refract Surg. 2015;41:47–52. doi: 10.1016/j.jcrs.2014.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Srinivasan S. Capsulorhexis: The perfect circle. J Cataract Refract Surg. 2017;43:303–4. doi: 10.1016/j.jcrs.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Chang DF, Mamalis N, Werner L. Precision pulse capsulotomy: Preclinical safety and performance of a new capsulotomy technology. Ophthalmology. 2016;123:255–64. doi: 10.1016/j.ophtha.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Thompson VM, Berdahl JP, Solano JM, Chang DF. Comparison of Manual, Femtosecond Laser, and Precision Pulse Capsulotomy Edge tear Strength in Paired human cadaver eyes. Ophthalmology. 2016;123:265–74. doi: 10.1016/j.ophtha.2015.10.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



