Abstract
Idiopathic intracranial hypertension (IIH) is a common cause of papilledema in young females and causes headache with transient visual loss. Severe visual loss occurs due to optic atrophy or peripapillary choroidal neovascular membrane (PCNVM). PCNVM in IIH has an incidence of 0.5% with a benign course in the majority of patients. Intravitreal Anti-vascular endothelial growth factor agents have anecdotally been used to manage these patients, with complete resolution reported in all cases after a single injection. Our case of IIH-associated PCNVM was treated with three injections of intravitreal ranibizumab with no recurrence at 6-month follow-up.
Keywords: Idiopathic intracranial hypertension, intravitreal ranibizumab, peripapillary choroidal neovascular membrane
Idiopathic intracranial hypertension (IIH) is a disorder of unknown cause, characterized by elevated intracranial pressure in the absence of a mass lesion, venous sinus thrombosis, or meningitis.[1] Peripapillary choroidal neovascular membrane (PCNVM) formation is a rare complication of IIH, seen in 0.5%–0.53% cases.[2,3] PCNVM in IIH is generally benign and is known to regress spontaneously.[2,4] However, severe visual loss may occur if the fovea is involved by subretinal fluid (SRF) or subretinal hemorrhage (SRH).[4,5] Treatment modalities such as photodynamic therapy, surgical excision, argon laser photocoagulation, and intravitreal anti-vascular endothelial growth factor (Vegf) injections (IvAVI) have been advocated to manage these cases.[2,4,5,6,7,8,9] Anecdotal evidence to support the use of IvAVI in PCNVM secondary to IIH exists in medical literature.[6,7,8,9] We present a case of severe visual loss due to SRF and SRH in a patient of IIH with PCNVM who was successfully managed with multiple intravitreal ranibizumab (IVR) injections.
Case Report
A 35-year-old female presented with sudden decrease of vision in her left eye (LE) for 1 week. Her best-corrected visual acuity (BCVA) was 6/9 and counting fingers at 1 feet in the right eye (RE) and LE, respectively. Intraocular pressure was 12 mmHg in both eyes. Anterior segment examination was unremarkable in both eyes. Fundus examination showed media clarity Grade 1, hyperemia of optic disc, blurring of disc margins, and edema of the peripapillary retinal nerve fiber layer in the RE [Fig. 1a]. Along with the aforementioned findings, the LE had a 4 disc diameter (DD) area of SRH between the optic disc and the fovea, extending beyond the inferior arcade. SRF was present at the fovea along with a 1/3 DD area of convoluted blood vessels between the temporal margin of the disc and the fovea [Fig. 1b]. Retrospective history revealed that the patient had intermittent episodes of holocranial headaches for the past 1 year. Neurology consultation was sought. Magnetic resonance (MR) imaging of the brain was normal, but MR venography of cerebral vessels revealed narrowing of both transverse and sigmoid sinus. Lumbar puncture showed increased opening pressure of cerebrospinal fluid (CSF). Rest of the CSF and neurological examination were normal. Working diagnosis of IIH with LE PCNVM was made and 250 mg oral acetazolamide (OA) was started, thrice a day.
Figure 1.
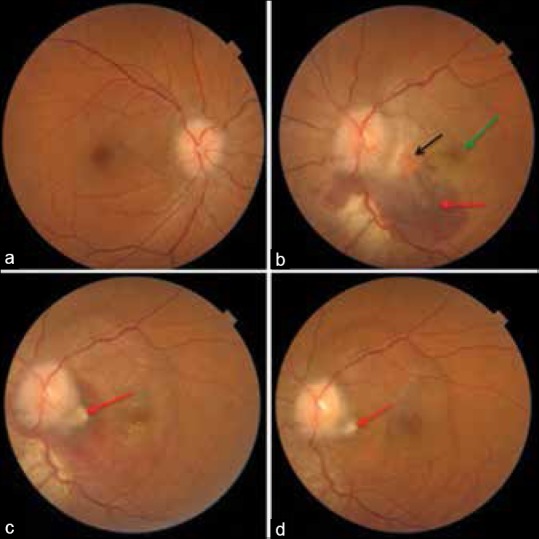
(a and b) Fundus photograph of both eye at presentation, showing hyperemic optic discs with blurred margins and presence of a 4 disc diameter area of subretinal hemorrhage (red arrow) inferotemporal to the optic disc in the left eye along with subretinal fluid involving the fovea (green arrow) and a 1/3 disc diameter choroidal neovascular membrane complex just temporal to the optic disc (black arrow), (c) 3 weeks after intravitreal ranibizumab decrease in subretinal hemorrhage with healing of choroidal neovascular membrane (red arrow), (d) at 3 months there is complete resolution of hemorrhage and fluid with a scarred choroidal neovascular membrane (red arrow)
Humphrey's visual field testing showed enlargement of the blind spot in the LE, while the fields of the RE were not reliable. Fundus fluorescein angiography of the LE showed blocked fluorescence in the area of the SRH with a 1/3 DD area of lacy hyperfluorescence temporal to the disc, suggestive of an active Type 2 PCNVM [Fig. 2a–c]. Swept source optical coherence tomography (SS-OCT) passing through the PCNVM and the fovea showed a hyperreflective CNVM complex, SRF at the fovea, and intraretinal fluid between the optic disc and fovea [Fig. 3a]. As the patient had an active PCNVM in the LE, IVR (0.5 mg/0.05 ml) was injected.
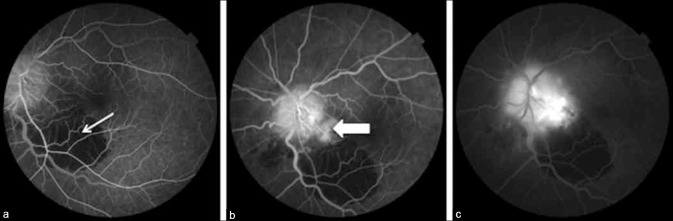
Figure 2.
Fundus fluorescein angiography images of the left eye showing blocked fluorescence due to subretinal hemorrhage (white arrow) in the arteriovenous phase (a) and hyperflourescence temporal to the disc in the venous phase with leakage due to active peripapillary choroidal neovascular membrane (broad white arrow) in the late phase (b and c)
Figure 3.
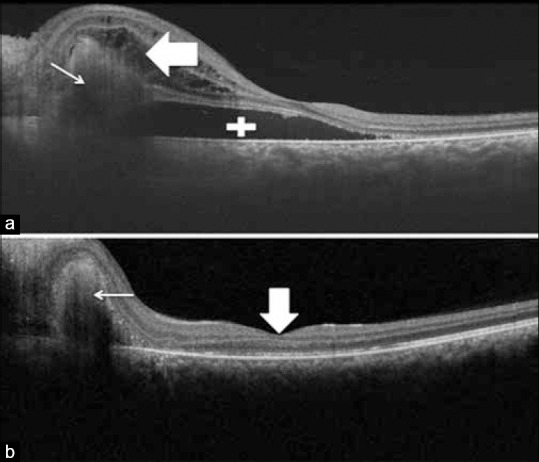
Swept source optical coherence tomography line scan of the left eye passing through the choroidal neovascular membrane complex and the fovea, (a) at presentation showing the mixed hypo and hyper-reflective choroidal neovascular membrane complex (white arrow) with subretinal fluid at the fovea (white addition sign) and intraretinal fluid (broad white arrow), (b) after 3 intravitreal ranibizumab injections showing regression of the choroidal neovascular membrane (white arrow) with normalization of the foveal architecture (broad white arrow)
Three weeks after the first IVR, LE BCVA improved to 6/24 with reduction in the SRF and SRH [Fig. 1c]. The patient also had improvement in the severity and frequency of headaches and did not report any side effects to OA. Hence, OA was increased to 500 mg three times a day. The patient went on to receive two additional IVR injections in her LE, at 1-month interval. Three months after presentation, BCVA in the LE improved to 6/6 with complete resolution of SRH and scarring of the PCNVM [Fig. 1d]. SS-OCT showed decrease in size of the CNVM with restoration of foveal architecture [Fig. 3b]. The patient had no neurological or ocular complaints and was being maintained on 250 mg OA, twice a day. At 6-month follow up, the patient was maintaining BCVA of 6/6 with resolved disc edema in both eyes. LE showed a scarred PCNVM with normal foveal contour.
Discussion
IIH is defined as increase in intracranial pressure due to unspecified cause leading to headache, papilledema, and transient vision loss.[1] Most patients of IIH have mild visual loss but about 25% may develop permanent visual loss due to irreversible optic disc damage.[1,10] PCNVM is a rare complication of IIH with the potential to cause severe vision loss.[2,3]
There are fewer than twenty reported cases of PCNVM associated with IIH. Morse et al. proposed that pressure deformity due to raised intracranial pressure transmitted at the level of optic nerve head leads to discontinuity of chorioretinal layers in patients of IIH. He further postulated that hypoxia created due to axonal swelling promotes angiogenesis leading to neovascular membrane formation.[4,5] These neovascular membranes have been known to regress spontaneously.[2,4] Wendel et al. reported PCNVM prevalence of 0.53% in 1140 cases of IIH. Out of six patients with PCNVM, three had spontaneous regression, two underwent argon laser photocoagulation, and one underwent photodynamic therapy.[2] Sathornsumetee et al. reported detection of PCNVM after optic nerve fenestration led to decrease in disc edema in a patient of IIH. They highlighted that PCNVM can be a cause of sudden visual loss and that the diagnosis may be difficult in the absence of SRH.[4]
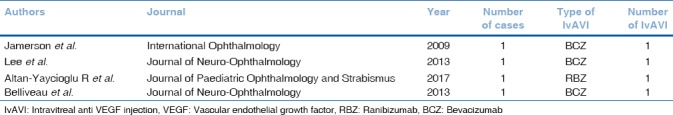
Jamerson et al. first reported the use of IvAVI for PCNVM in IIH.[6] A single injection of intravitreal bevacizumab led to involution of PCNVM and restoration of vision in their patient. All cases of IvAVI use for PCNVM secondary to IIH have reported resolution of the PCNVM with a single injection of IvAVI [Table 1]. Our patient had a large SRH with intraretinal and SRF. Three IvAVIs were needed for complete resorption of SRH and restoration of vision in our patient. Hence, although most cases of PCNVM in IIH respond to a single IvAVI, severe cases may need more number of intravitreal injections and intensive follow-up.
Table 1.
List of case reports of intravitreal anti-vascular endothelial growth factor for peripapillary choroidal neovascular membrane secondary to idiopathic intracranial hypertension
Conclusion
Accurate diagnosis with timely institution of IvAVI in patients of IIH with fovea involving PCNVM leads to favorable outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wall M. Update on idiopathic intracranial hypertension. Neurol Clin. 2017;35:45–57. doi: 10.1016/j.ncl.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wendel L, Lee AG, Boldt HC, Kardon RH, Wall M. Subretinal neovascular membrane in idiopathic intracranial hypertension. Am J Ophthalmol. 2006;141:573–4. doi: 10.1016/j.ajo.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 3.Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol. 1988;45:875–7. doi: 10.1001/archneur.1988.00520320065016. [DOI] [PubMed] [Google Scholar]
- 4.Sathornsumetee B, Webb A, Hill DL, Newman NJ, Biousse V. Subretinal hemorrhage from a peripapillary choroidal neovascular membrane in papilledema caused by idiopathic intracranial hypertension. J Neuroophthalmol. 2006;26:197–9. doi: 10.1097/01.wno.0000235583.10546.0a. [DOI] [PubMed] [Google Scholar]
- 5.Morse PH, Leveille AS, Antel JP, Burch JV. Bilateral juxtapapillary subretinal neovascularization associated with pseudotumor cerebri. Am J Ophthalmol. 1981;91:312–7. doi: 10.1016/0002-9394(81)90282-8. [DOI] [PubMed] [Google Scholar]
- 6.Jamerson SC, Arunagiri G, Ellis BD, Leys MJ. Intravitreal bevacizumab for the treatment of choroidal neovascularization secondary to pseudotumor cerebri. Int Ophthalmol. 2009;29:183–5. doi: 10.1007/s10792-007-9186-y. [DOI] [PubMed] [Google Scholar]
- 7.Lee IJ, Maccheron LJ, Kwan AS. Intravitreal bevacizumab in the treatment of peripapillary choroidal neovascular membrane secondary to idiopathic intracranial hypertension. J Neuroophthalmol. 2013;33:155–7. doi: 10.1097/WNO.0b013e31827c6b49. [DOI] [PubMed] [Google Scholar]
- 8.Altan-Yaycioglu R, Canan H, Saygi S. Intravitreal ranibizumab injection in peripapillary CNVM related to idiopathic intracranial hypertension. J Pediatr Ophthalmol Strabismus. 2017;54:e27–30. doi: 10.3928/01913913-20170201-04. [DOI] [PubMed] [Google Scholar]
- 9.Belliveau MJ, Xing L, Almeida DR, Gale JS, ten Hove MW. Peripapillary choroidal neovascular membrane in a teenage boy: Presenting feature of idiopathic intracranial hypertension and resolution with intravitreal bevacizumab. J Neuroophthalmol. 2013;33:48–50. doi: 10.1097/WNO.0b013e318281b7b9. [DOI] [PubMed] [Google Scholar]
- 10.Hainline C, Rucker JC, Balcer LJ. Current concepts in pseudotumor cerebri. Curr Opin Neurol. 2016;29:84–93. doi: 10.1097/WCO.0000000000000273. [DOI] [PubMed] [Google Scholar]