Multifocal Best disease (MBD) is a rare disease characterized by multiple sharply demarcated yellowish lesions in the posterior pole and beyond arcades. This is considered an atypical variant of Best vitelliform macular dystrophy (VMD).[1] This photo essay describes the multimodal imaging (MI) characteristic of MBD.
Case
A 14-year-old male presented with gradual loss of vision in both the eyes for 2 years. Best-corrected visual acuity was 6/18, N6 both eyes. Color fundus photograph [Fig. 1a and b] showed multiple small round yellow subretinal lesions on the posterior pole extending beyond the arcades along with macular thickening. Multicolor image [Fig. 1c and d] showed greenish hue over the macula and multiple orange spots corresponding to yellow lesions. Blue-light fundus autofluorescence (FAF) [Fig. 2a and b] showed multiple hyperautofluorescent lesions. Near-infrared reflectance image [Fig. 3a and b] showed multiple white hyper-reflective spots suggestive of alterations at retinal pigment epithelium (RPE) level, while green [Fig. 3c and d] and blue [Fig. 3e and f] reflectance image showed no abnormality. Enhanced depth imaging-optical coherence tomography (EDI-OCT) scan through the fovea [Fig. 4a and b] showed thickened ellipsoid zone which is separated from the RPE-Bruch complex by an optically clear space; EDI-OCT line scan through peripheral yellow lesions [Fig. 4c and d] shows vitelliform lesions. Fundus fluorescein angiography (FFA) [Fig. 5a and b] showed no leak. Full-field electroretinography and electro-oculography (EOG) were normal.
Figure 1.

Color fundus photograph of the right eye and left eye (a and b) showing multiple yellow subretinal spots on the posterior pole (white arrow) extending beyond the arcades with central foveal thickening with a pale yellowish clump temporal to the fovea in the right eye and gliotic band temporal to the fovea in the left eye; Multicolor image (c and d) showing greenish hue over the macula, more in the left eye, suggestive of retinal thickening and multiple discrete orange spots (arrowhead) corresponding to yellow lesions visible on color fundus
Figure 2.

Blue-light fundus autofluorescence (a and b) showing multiple hyperautofluorescent lesions on the posterior pole and extending beyond the arcade corresponding to the yellow lesions visible in color fundus
Figure 3.

Near-infrared reflectance image (a and b) of the right eye and left eye showing multiple white hyper-reflective spots (arrowhead) over the posterior pole extending beyond the arcades suggestive of alterations at retinal pigment epithelium level, while green (c and d) and blue (e and f) reflectance image fails to highlight lesions clearly
Figure 4.
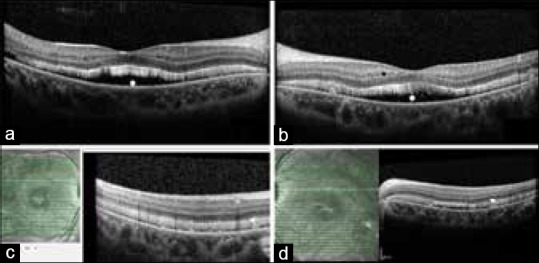
Enhanced depth imaging-optical coherence tomography imaging of the right and left eye (a and b) showing thickened ellipsoid zone which is separated from the retinal pigment epithelium/Bruch complex by an optically clear space (asterisk); optical coherence tomography line scan (c and d) through the peripheral yellow lesion visible on the color fundus showing hyper-reflective lesion at the level of retinal pigment epithelium with a narrow optically clear space in subretinal space typical of vitelliform lesion
Figure 5.
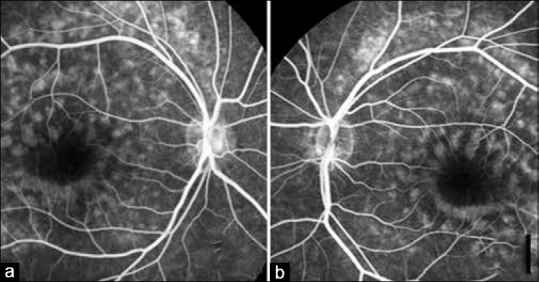
Fundus fluorescein angiography (a and b) mid phase showing multiple hyperfluorescent spots over the posterior pole sparing the fovea corresponding to yellow lesions seen in color fundus with no active leakage
Discussion
MBD presents with typical features, has association with VMD2 gene mutation, and may have normal EOG.[2,3] MI is important to differentiate this entity from acute exudative polymorphous vitelliform maculopathy syndrome, pattern dystrophies, drusenoid pigment epithelial detachment, birdshot chorioretinitis, central serous chorioretinopathy, and paraneoplastic syndromes.[4] Multicolor imaging localizes the lesion to RPE as seen in IR image while Blue Reflectance (BR) and Green Reflectance (GR) which highlight the superficial retinal lesions are silent.[5] EDI-OCT shows characteristic vitelliform deposits with normal subfoveal choroidal thickness and vasculature. FFA and indocyanine green show no leak. FAF is striking and highlights the vitelliform deposits due to their rich lipofuscin content. MBD is primarily a benign condition and does not warrant any treatment unless associated with secondary complications such as choroidal neovascular membrane. Genetic testing can add paramount significance to such cases.[6]
Conclusion
This report highlights the MI of MBD and will help clinicians to differentiate it from similar lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Miss. Marina Parvin and Miss. Moupiya Das, ophthalmic photographer.
References
- 1.Caumon C, Bernard JA, Mondon H, Quentel G, Hamard H, Chevaleraud J, et al. Multifocal vitelliform dystrophy: A case report (author's transl) J Fr Ophtalmol. 1981;4:279–85. [PubMed] [Google Scholar]
- 2.Pollack K, Kreuz FR, Pillunat LE. Best's disease with normal EOG. Case report of familial macular dystrophy. Ophthalmologe. 2005;102:891–4. doi: 10.1007/s00347-004-1088-z. [DOI] [PubMed] [Google Scholar]
- 3.Chan CK, Gass JD, Lin SG. Acute exudative polymorphous vitelliform maculopathy syndrome. Retina. 2003;23:453–62. doi: 10.1097/00006982-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Spaide RF, Noble K, Morgan A, Freund KB. Vitelliform macular dystrophy. Ophthalmology. 2006;113:1392–400. doi: 10.1016/j.ophtha.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 5.Roy R, Saurabh K, Bhattacharyya S, Thomas NR, Datta K. Multimodal imaging in dominant cystoid macular dystrophy. Indian J Ophthalmol. 2017;65:865–6. doi: 10.4103/ijo.IJO_328_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alba Linero C, Rodríguez Calvo de Mora M, España Contreras M, Hernando Ayala C. Multifocal best's disease: The importance of genetic tests. Arch Soc Esp Oftalmol. 2018;93:136–8. doi: 10.1016/j.oftal.2017.08.003. [DOI] [PubMed] [Google Scholar]


