Abstract
Anti-N-methyl-D-aspartate (NMDA) receptor antibody encephalitis is an autoimmune form of limbic encephalitis. Eighty percent of patients with anti-NMDA receptor (NMDAR) encephalitis are women, and 39% of those women are reported to have an ovarian teratoma also. When a tumor is also present, prompt surgery can prevent the development of more severe symptoms or the prolongation of symptoms of encephalitis. The current authors encountered two cases in which anti-NMDAR encephalitis was suspected. In these cases, abdominal computed tomography (CT) revealed an ovarian teratoma and both patients underwent a laparoscopic salpingo-oophorectomy. Both patients underwent surgery before a definitive diagnosis was made. Findings in one case did not lead to a diagnosis of anti-NMDAR encephalitis, but symptoms rapidly improved after surgery in both cases. Laparoscopic surgery is minimally invasive, so this approach may be the first step in a treatment algorithm for treatment of a tumor in a patient with anti-NMDAR encephalitis.
Keywords: laparoscopic surgery, NMDA receptor antibody encephalitis, teratoma
Introduction
The N-methyl-D-aspartate (NMDA) receptor is a glutamate receptor that is located on the postsynaptic membrane. Anti-NMDA receptor antibody encephalitis (or simply anti-NMDAR encephalitis) is an autoimmune form of limbic encephalitis that develops when antibodies to the NMDA receptor (NMDAR) are produced. Eighty percent of patients with anti-NMDAR encephalitis are women, and 39% of those women are reported to have an ovarian teratoma also.1 Symptoms of anti-NMDAR encephalitis are classified into a prodromal phase, a psychotic phase, an unresponsive phase, a hyperkinetic phase, and a recovery phase.2 The current authors encountered two cases in which anti-NMDAR encephalitis was suspected. Abdominal computed tomography (CT) revealed an ovarian teratoma, and a laparoscopic salpingo-oophorectomy was promptly performed. The general condition of both patients improved. These cases are reported here, along with a review of the literature.
Case 1
This case involved a 40-year-old woman, gravida 1, para 1, with bipolar disorder. Six years prior, the woman had been visiting a nearby physician for treatment of Graves’ disease, but she often failed to attend her appointments. Several days prior to her illness, the woman developed symptoms such as forgetfulness and wandering. On Day 1 of hospitalization, the woman was discovered after she had lost consciousness and fallen in the street. The woman was transported to a psychiatric hospital. At the psychiatric hospital, the woman was semicomatose, disoriented, and laughing for no reason. On Day 5 of hospitalization, the woman developed a fever and she had repeated generalized tonic–clonic seizures. On Day 6 of hospitalization, the woman was transported to the Department of Neurology in St. Mary’s Hospital. Upon arrival, tonic seizures involving the left arm and involuntary movement of the mouth were noted. Contrast-enhanced magnetic resonance imaging (MRI) revealed contrast enhancement in the cortex of the right temporal and parietal lobes followed by fluid attenuated inversion recovery (FLAIR) hyperintensities. There were slight hyperintensities in some diffusion-weighted images also. Anti-NMDAR encephalitis was included in the differential. Abdominal CT revealed a tumor on the left ovary that was suspected of being a teratoma. Seizures due to electrolyte abnormalities or abnormal blood glucose levels were ruled out and specimens tested negative for antinuclear antibodies and other common autoantibodies. The titer of antibodies to viruses such as the herpes virus was not elevated. Based on these findings, the patient was thought to have limbic encephalitis (i.e., nonherpetic encephalitis). On Day 9 of hospitalization, pulse steroids were initiated. Improvement in symptoms was not noted despite the initiation of steroids. The patient had a history of Graves’ disease and the patient tested strongly positive for antithyroid peroxidase (anti-TPO) antibodies and antithyroglobulin antibodies, so Hashimoto’s encephalopathy could not be ruled out, but anti-NMDAR encephalitis was considered a possibility based on the course of symptoms and laboratory results. This fact was fully explained to the patient’s family. On Day 12 of hospitalization, the decision was made to perform a laparoscopic left salpingo-oophorectomy. Perioperative findings indicated that the left ovary was enlarged to the size of a chicken’s egg. The surface of the ovary was smooth and whitish in color. Abnormal findings were not noted in the right ovary. A laparoscopic left salpingo-oophorectomy was performed (Figure 1A and B). Operating time was 39 minutes and blood loss was 0 g. After surgery, the patient was sedated and placed on a ventilator. On Day 8 postoperatively, the patient was deemed capable of spontaneous breathing and the patient was extubated. However, involuntary movement and seizures were noted, so pulse steroids and gamma globulin were initiated. On Day 32 postoperatively, the patient was able to ambulate with assistance. After early rehabilitation, the patient was able to perform most activity of daily life (ADL) without assistance, but her higher brain function remained impaired. On Day 54 postoperatively, the patient was transferred to a hospital for chronic care so later rehabilitation could continue. After surgery, histopathology results revealed a mature cystic teratoma that contained central nervous system tissue. In addition, cerebrospinal fluid obtained prior to surgery tested positive for serum anti-NMDAR antibodies.
Figure 1.
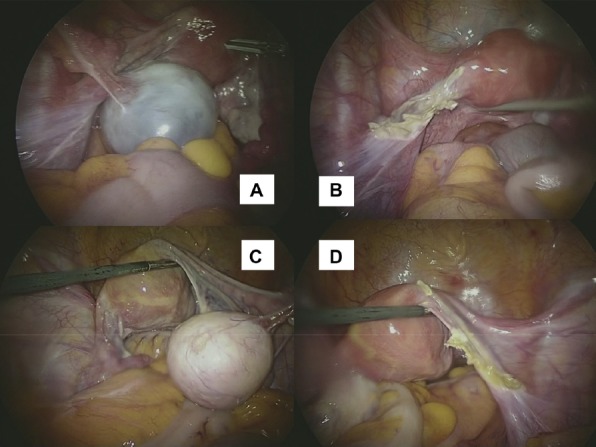
(A) Case 1 left ovarian tumor; (B) Case 1 after adnexectomy; (C) Case 2 right ovarian tumor; (D) Case 2 after adnexectomy.
Case 2
This case involved a 44-year-old woman, gravida 4, para 4. Three months prior, the woman had difficulty sleeping, inability to collect her thoughts, and noticeable forgetfulness. Two days prior to her current visit, the woman developed a fever, vomiting, and diarrhea. On Day 1 of hospitalization, the woman developed central nervous system symptoms such as impaired consciousness, seizures, and abnormal behavior, so the woman was seen by her previous physician. Upon arrival, her pupils were dilated and the woman was restless. The woman had involuntary movement of the mouth followed by spasming resembling opisthotonus every 20 minutes or so. An anticonvulsant was administered but failed to control the spasms, so that day the woman was transported to St. Mary’s Hospital. Upon arrival, the patient remained restless and her consciousness was I-3-II-20 on the Japan coma scale (JCS). The patient was unable to follow orders. A contrast-enhanced MRI scan of the head revealed no abnormal contrast enhancement. Anti-NMDAR encephalitis was included in the differential. Abdominal CT revealed a tumor on the right ovary that was suspected of being a teratoma. Seizures due to electrolyte abnormalities or abnormal blood glucose levels were ruled out and specimens tested negative for antinuclear antibodies and other common autoantibodies. The titer of antibodies to viruses such as the herpes virus was not elevated. Based on these findings, the patient was thought to have limbic encephalitis (nonherpetic encephalitis). Other conditions were ruled out and the clinical manifestations were quite typical, so anti-NMDAR encephalitis was suspected. This fact was fully explained to the patient’s family. On Day 1 of hospitalization, the decision was made to perform a laparoscopic right salpingo-oophorectomy. Perioperative findings indicated that the right ovary was enlarged to the size of a chicken’s egg. The surface of the ovary was smooth and whitish in color. There was no evidence of abnormalities in the left ovary. A laparoscopic right salpingo-oophorectomy was performed (Figure 1C and D). Operating time was 31 minutes and blood loss was 0 g. On the day of surgery, the patient was sedated and placed on a ventilator. On Day 1 post-operatively, sedation was halted. The patient was alert and able to follow commands, so the patient was extubated. There were no issues with the postoperative course but short-term memory remained impaired, so pulse steroids and gamma globulin were initiated. The patient’s short-term memory gradually improved and the patient’s course was satisfactory, so the patient was discharged on Day 15 postoperatively. After surgery, histopathology results revealed a mature cystic teratoma that did not contain central nervous system tissue. In addition, cerebrospinal fluid obtained prior to surgery tested negative for serum anti-NMDAR antibodies.
Discussion
Anti-NMDA receptor encephalitis is an autoimmune form of limbic encephalitis that develops when antibodies to the NMDA receptor are produced. When clinical manifestations and imaging findings suggest acute limbic encephalitis, viral encephalitis, Hashimoto’s encephalopathy, and other forms of autoimmune encephalitis need to be excluded. When a female patient is suspected of having anti-NMDAR encephalitis, a search for an ovarian teratoma must be conducted. Anti-NMDAR antibodies in serum and cerebrospinal fluid provide a definitive diagnosis. Since Dalmau et al3 reported on teratomas in patients with anti-NMDAR encephalitis in 2007, prompt surgery has been used to prevent the development of more severe symptoms or the prolongation of symptoms of encephalitis when a tumor is present along with anti-NMDAR encephalitis. In 2011, Dalmau et al2 devised a treatment algorithm for anti-NMDAR encephalitis (Figure 2). Determining the anti-NMDAR antibody titer in serum and cerebrospinal fluid is the first step in this algorithm. However, very few facilities in Japan are able to test for those antibodies. Thus, deciphering test results takes time. In the two cases encountered by the current authors, anti-NMDAR encephalitis was suspected. Abdominal CT revealed an ovarian teratoma. In both cases, a definitive diagnosis had yet to be made, but once an ovarian teratoma was identified a laparoscopic adnexectomy of the affected side was performed. This resulted in relatively rapid improvement in neurologic symptoms after surgery. In Case 1, the patient had a psychiatric disorder that hampered the determination of symptoms in the psychotic phase of anti-NMDAR encephalitis. The patient also had a history of Graves’ disease and laboratory results were unable to rule out Hashimoto’s encephalopathy. In Case 2, laboratory results were able to rule out other forms of acute limbic encephalitis, but serum and cerebrospinal fluid tested negative for anti-NMDAR antibodies. Findings did not lead to a definitive diagnosis of anti-NMDAR encephalitis. As a result, the pathology in that case could not be determined. However, rapid improvement in clinical manifestations was noted after tumor removal. Oophorectomy was performed in both cases because of the presence of unilateral cysts and because they were over the age of 40. Previous reports do not present a consensus on which of oophorectomy or cystectomy should be performed. In the case of younger patients before marriage, it might be better to select oophorectomy because of the severity of the symptoms. However, in cases of younger patients with bilateral tumors, it might be acceptable to select cystectomy after giving sufficient information regarding the relative risks and benefits and gaining informed consent. Nonetheless, it is necessary to perform an oophorectomy in cases that do not improve after cystectomy.
Figure 2.
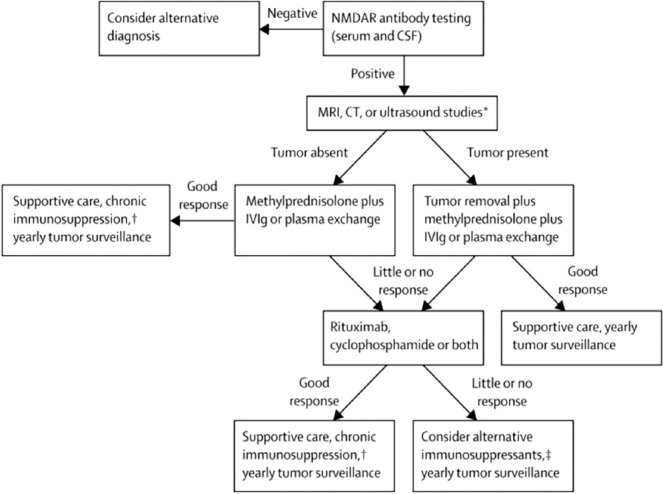
Algorithm for the treatment of anti-NMDAR encephalitis (quoted from reference 2). Anti-NMDAR = anti-N-methyl-D-aspartate receptor.
Laparoscopic surgery can be performed with a vessel-sealing device, allowing a shorter operating time and less invasive surgery. Even if encephalitis results in prolonged bed rest, complications such as postoperative adhesions and ileus are unlikely to occur. The current cases were probably discovered incidentally. Although an antibody titer takes time, laparoscopic surgery can be quickly and safely performed by many facilities in Japan. In cases of limbic encephalitis (nonherpetic encephalitis) in a patient with an ovarian teratoma, prompt laparoscopic tumor removal prior to a definitive diagnosis may represent a new treatment algorithm for anti-NMDAR encephalitis.
Footnotes
Conflicts of interest: The authors have no conflicts of interest relevant to this article.
References
- 1.Titulaer MJ, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12:157–165. doi: 10.1016/S1474-4422(12)70310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dalmau J, Lancaster E, Martinez-Hernandez E, et al. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011;10:63–74. doi: 10.1016/S1474-4422(10)70253-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalmau J, Tüzün E, Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]


