Abstract
Introduction:
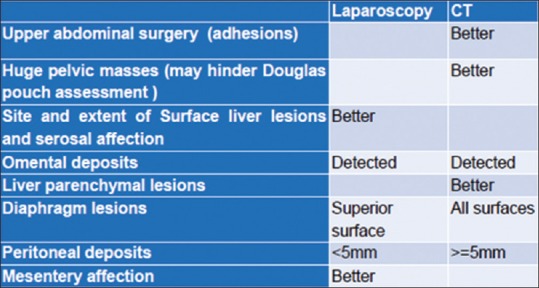
Comprehensive staging laparotomy and cytoreductive surgery followed by chemotherapy has been the standard of care in advanced ovarian cancer. Neoadjuvant chemotherapy is an alternative in inoperable advanced cases. To select patients amenable for successful cytoreduction, major determinants including CT imaging and laparoscopy could be of value. There is no general accepted model for selection and reproducibility of techniques are a major challenge due to different clinical practice and complexity of scoring systems. Some lesions as small size (<5 mm) peritoneal deposits and mesenteric affection are hard to see on CT so, complementary laparoscopy may play a role in the preoperative assessment. The aim of this study was evaluation of the role of laparoscopy in advanced ovarian tumors for prediction of optimal cytoreductive surgery in relation to CT and surgical peritoneal carcinomatosis index (PCI).
Aim:
Was to evaluate laparoscopic assessment in advanced ovarian tumors for prediction of optimal cytoreductive surgery in relation to CT and surgical peritoneal carcinomatosis index (PCI).
Setting:
Gyne-oncology specialized center, El-Shatby maternity university hospital, Alexandria Egypt.
Methods:
From January 2016 to December 2016, 15 patients were recruited from gyne-oncology specialized center, Alexandria, Egypt. Patients underwent a special design described later then laparoscopy using palmar point entry was done for assessing small lesions and the extent of affection in surface peritoneal, mesentery, serosa of the gut especially small intestine (terminal ileum affection, more or less than 50% affection) mainly with evaluating other sites as liver surface and diaphragm peritoneal surface affection after removal of ascites by aspiration. Findings were correlated with laparotomy and CT scan findings. Surgery was performed in the same setting which is better or with in two weeks.
Results:
There were two cases with upper abdominal surgeries (cholecystectomy and splenectomy) where no visualization of liver and stomach on laparoscopy but were free on CT scan and surgical evaluation. Douglas pouch was not assessed in two patients with large fixed bilateral ovarian masses on laparoscopy. Two cases with diaphragmatic affection on CT scan related to the posterior surface were not detected on laparoscopy. These findings were correlated with surgical findings as the gold standard. The pathology was ranging from low grade to high grade serous cyst adenocarcinoma.
Conclusions:
Laparoscopic evaluation is a useful adjunct with CT prior to performing ovarian cancer cytoreductive surgery for assessment of operability. Laparoscopy is better for evaluating extent of serosal affection in advanced tumors in cases with omental cakes on CT. A roadmap for prediction of operability in advanced ovarian cancer can be used by combing CT PCI and laparoscopic assessment.
Keywords: Cytoreductive surgery, CT, laparoscopy, Ovarian cancer, PCI
STUDY
From January 2016 to December 2016, 15 patients were recruited from gyne-oncology specialized center, El-Shatby maternity university hospital, Egypt. The study was approved by Alexandria university ethics committee. Inclusion criteria were patients diagnosed with advanced ovarian cancers by RMI II score (malignancy risk index). The RMI II score (malignancy risk index) was calculated based on the serum CA 125 value, menopausal status (M), and evaluation of ultrasound (U). Using cut-off RMI score above 200 to indicate high malignancy risk was used.[1] Patients underwent the following study design [Figure 1]. CT staging was performed for detection of omental cake, liver metastasis and lymph node affection where PCI scoring was done if positive. PCI score ranges from 0 to 39 with more than 15 indicating advanced tumors. The peritoneal cancer index (PCI) is the method of measuring the amount and distribution of metastatic tumor in the peritoneal cavity on CT scan and laparotomy. It is based on tumor extent in 13 separate regions. Tumor spread, localization and size were described and documented applying Sugarbaker's PCI. Two transverse planes and two sagittal planes divide the abdomen into 9 regions. Lesion size scores in the individual regions are summed up to the PCI score which can assume a minimum score of 0 and maximum score of 39.[1,2,3,4,5] Patients with PCI score less than 20 were included in our study. Patients underwent laparoscopy. Laparoscopy was used to complete the information provided by imaging and provides the histological diagnosis (biopsy) if needed. All patients underwent three port laparoscopy using palmar point entry using 10 mm zero degree scope except in one case with umblical entry due to adhesions at the palmar point and accessory 5mm paraumblical ports above the mass. Removal of ascites by aspiration before inspection.[1] Laparoscopy was used mainly for assessing five lesions (surface peritoneal lesions, mesentery affection and serosal affection of the gut especially small intestine with its extent, liver surface lesions, diaphragm surface lesions). Assessment was correlated with aparotomy and CT scan using Sugarbaker's Peritoneal Cancer Index. If mesentry affection or less than 1.5 meter of small intestine was affected by surface lesions, patients were guided for neoadjuvant chemotherapy and others underwent surgery in the same setting. The exploratory laparotomy and intra-operative data evaluations were conducted by a surgical team of surgeon. Surgery included at least: Complete hysterectomy with oophorectomy, Infragastric total omentectomy without dissection of pelvic and lumboaortic lymph nodes except in clinically palpable ones more than 1cm.
Figure 1.
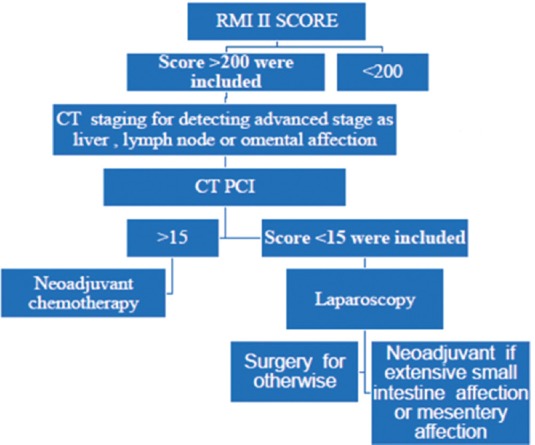
Study design
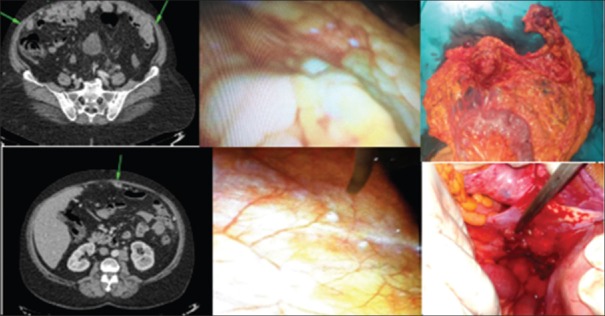
Patients underwent the following study design [Figure 1] then laparoscopy using palmar point entry was done for assessing small lesions and the extent of affection in surface peritoneal, mesentery, serosa of the gut especially small intestine (terminal ileum affection, more or less than 50% affection) mainly with evaluating other sites as liver surface and diaphragm peritoneal surface affection after removal of ascites by aspiration. (1) Findings were correlated with laparotomy and CT scan findings [Figure 2]. Surgery was performed in the same setting which is better or with in two weeks.
Figure 2.
CT images showing large peritoneal deposits on PCI. Laparoscopy showing small peritoneal deposits not seen on laparoscopy. Operative photos showing omental and peritoneal deposits
RESULTS
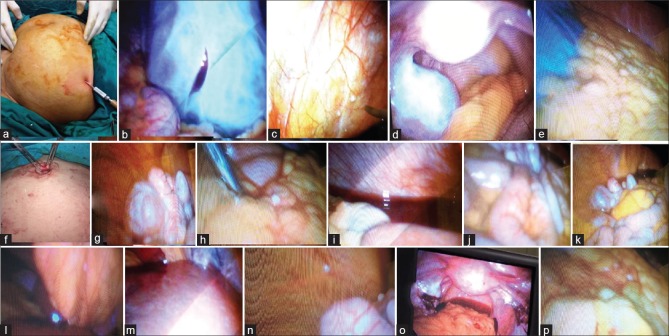
A total of 15 patients were included in the study. The female age ranged from 45 years to 70 years. Eleven cases underwent complete cytoreduction with no lymphadenectomy. Four cases (26.6%) underwent neoadjuvant chemotherapy with hepatic and diaphragmatic deposits. Two diaphragmatic affection on CT scan related to posterior surface that were not detected on laparoscopy, one case with mesentery affection and once case with extensive serosal affection of small intestine more than 50% that were detected on laparoscopy and not on CT scan. Two cases with upper abdominal surgeries of cholecytsctomy and splenectomy where non visualization of liver and stomach on laparoscopy but were free on CT scan and surgery. Eleven patients had omental cake on CT scan. Peritoneal deposits and mesenteric affection were not detected on CT but were detected during laparoscopy. Largest ovarian mass detected was about 20 cm reaching the umbilicus and was successfully scored after direct trocar insertion and aspirating the fluid. Douglas pouch was not assessed in patients with large solid fixed bilateral masses. No gastric or intestinal infiltration were detected on surgery. The pathologies were ranging from low grade to high grade serous cyst adenocarcinoma [Figures 3,4].
Figure 3.
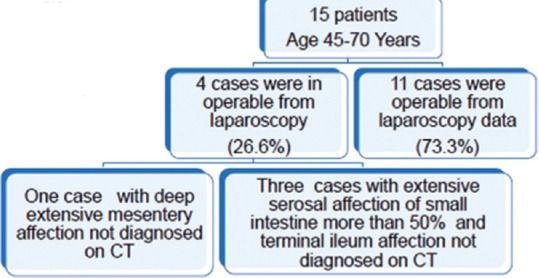
Summary of results
Figure 4.
Palmar point entry (a), trocar puncture of mass for decompression (b), peritoneal implants not detected by imaging (c and n), ovarian mass with Douglas pouch evaluation and free intestine (d), free omentum (e), Everting the umbilicus for entry in pelvic masses (f), ovarian mass (g), omental deposits not detected by imaging (h), normal diaphragm with hemorrhagic ascites (i), normal intestine and mesentery (j and k) Falciform deposits not detected on imaging (l), normal liver (m), oophorectomy with other side biopsies (o), omental deposits not detected by imaging (p)
DISCUSSION
Comprehensive staging laparotomy and cytoreductive surgery followed by chemotherapy has been the standard of care in newly diagnosed advanced ovarian cancer. Currently, a cut-off of 1 cm of residual tumor size is defined as optimal cytoreduction. Neoadjuvant chemotherapy is alternative if inoperable advanced cases. To select patients amenable or not for successful cytoreduction, various predictive tests have been published. Major determinants include CT and laparoscopy. However, the problem is that there is no general accepted model and that reproducibility is a major challenge due to different clinical practice. Other limitations include complexity of scoring systems.[5]
The accurate mapping of tumor burden and distribution of disease plays a central role in treatment stratification. Site, size, and distribution of metastases have been used as radiological predictors for the outcome of cytoreductive surgery. Mesenteric involvement, bowel affection and small size (<5 mm) peritoneal deposits are hard to see in CT, complementary laparoscopy may play a role in the preoperative assessment of ovarian cancer.[6]
Eight laparoscopic features were investigated as potential indicators of surgical outcome by Fagotti et al.[1]: presence of ovarian masses (unilateral or bilateral); omental cake with tumor diffusion to the small and large curvature of the stomach; extensive carcinomatosis of the diaphragm, peritoneum, bowel, and liver; and large and/or small-bowel infiltration necessitating resection. Mesentery of the small bowel was evaluated by folding back the various intestinal segments were possible, whereas lymph nodal status, was not included.[6] Each of the previous sites except the ovarian mass was given score of if positive with total score of 8 necessitates neoadjuvant chemotherapy. We did not use this score because site is better scoring system as may be mesenteric retraction or extensive affection of small intestine alone which is inoperable and the score is 2-4.
The occurrence of port-site metastases has raised concern about the use of laparoscopic surgery for procedures associated with malignant disease. The actual incidence of port-site metastases estimates range from 0% to 1.2%[6,7] but as early cytoreduction immediate or within two weeks (high risk of vascular adhesions and edema) this concern is so low.[7]
Disadvantages of laparoscopy are absence of a direct tactile evaluation by palpation and the presence of fixed masses in Douglas pouch and upper abdominal adhesions hindering the visualization of certain anatomical spaces.[4]
Despite improvements in MRI and CT, resectability of intra peritoneal disease remains difficult to determine therefore addition of laparoscopy evaluation can be useful.[5,6]
CONCLUSIONS
A roadmap for prediction of operability in advanced ovarian cancer can be used by combing CT PCI and laparoscopic assessment [Figure 5].
Figure 5.
Conclusion summary
Authors Contribution
All the authors contributed to protocol development, data collection and management, Data analysis and Manuscript writing/editing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fagotti A, Ferrandina G, Fanfani F, Ercoli A, Lorusso D, Rossi M, et al. A laparoscopy-based score to predict surgical outcome in patients with advanced ovarian carcinoma: A pilot study. Ann Surg Oncol. 2006;13:1156–61. doi: 10.1245/ASO.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Duhr C, Kenn W, Kickuth R, Kerscher AG, Germer CT, Hahn D, et al. Optimizing of preoperative computed tomography for diagnosis in patients with peritoneal carcinomatosis. World Journal of Surgical Oncology. 2011;9:171. doi: 10.1186/1477-7819-9-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chandrashekhara SH, Thulkar S, Srivastava DN, Kumar L, Hariprasad R, Kumar S, et al. Pre-operative evaluation of peritoneal deposits using multidetector computed tomography in ovarian cancer. Br J Radiol. 2011;84:38–43. doi: 10.1259/bjr/87415692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meleis MH, El-Agwany AMS. Peritoneal Carcinomatosis Index in Advanced Ovarian Malignancy either by Multislice CT verus Laparotomy: A Comparative Study. Indian J Gynecol Oncolog. 2015:13:24. [Google Scholar]
- 5.Gómez-Hidalgo NR, Martinez-Cannon BA, Nick AM, Lu KH, Sood AK, Coleman RL, et al. Predictors of optimal cytoreduction in patients with newly diagnosed advanced-stage epithelial ovarian cancer: Time to incorporate laparoscopic assessment into the standard of care. Gynecol Oncol. 2015;137:553–8. doi: 10.1016/j.ygyno.2015.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener H, Lopes T, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): An open-label, randomised, controlled, non-inferiority trial. Lancet. 2015;386:249–57. doi: 10.1016/S0140-6736(14)62223-6. [DOI] [PubMed] [Google Scholar]
- 7.Manvelyan V, Khemarangsan V, Huang KG, Adlan AS, Lee CL. Port-site metastasis in laparoscopic gynecological oncology surgery: An overview. Gynecol Minim Invasive Ther. 2016;5:1–6. [Google Scholar]