Abstract
Endometriosis is a common gynecological condition which affects 5–10% of women of reproductive age and up to 50% of women with pelvic pain and infertility. The most commonly affected areas are the pelvic peritoneum, ovaries and rectovaginal septum. Isolated endometriosis of the sciatic nerve is very rare. Our patient suffered from worsening right hip and buttock pain with severe exacerbation during menstruation. Several different imaging modalities (ultrasound of her pelvis and right hip, as well as X-rays and computed tomography scans of her right hip and lumbosacral spine) failed to identify any pathology. Magnetic resonance imaging scans of her pelvis revealed a 3.5 cm endometriotic lesion over the pelvic segment of her right sciatic nerve. Following a multidisciplinary discussion, the patient underwent laparoscopic excision of endometriosis. The patient recovered well from her surgery. She successfully conceived with in vitro fertilization 3 years after her surgery, following a failed course of Clomid (Clomiphene citrate) for ovulatory dysfunction.
Keywords: Endometriosis, laparoscopy, pelvic pain, sciatic nerve
INTRODUCTION
Endometriosis is a common gynecological condition, first described by von Rokitansky in 1860.[1] It is defined as the occurrence of endometriotic tissue (endometrial glands, stroma, or both) outside the uterus. The most affected areas are the pelvic peritoneum, ovaries, and rectovaginal septum. Nearly 5–10% of women in their reproductive years develop endometriosis. However, among patients with pelvic pain and infertility, the prevalence may range from 35% to 50%.[2,3,4] The most common presentation is pain, typically in the form of dysmenorrhea, pelvic pain, and dyspareunia, due to visceral nerve involvement. Infrequently, endometriosis has been described to infiltrate major pelvic nerves and cause sciatic neuropathy or lumbosacral plexopathy. Endometriosis involving sciatic nerve is commonly from direct extension of deeply infiltrative rectovaginal disease through the lateral pelvic sidewall. Less commonly, endometriosis over the sciatic nerve can be present in isolation, without any apparent endometriosis in the pelvic peritoneal cavity.[5] This article will outline the case of a young woman with isolated endometriosis involving the sciatic nerve and discuss the complex issues surrounding its management.
CASE REPORT
Miss AB is a healthy 24-year-old female who developed progressively worsening right hip and buttock pain after cessation of the oral contraceptive pill. Initially, this pain occurred only during menstruation and ovulation; however, it became more constant over the next 6 months with severe exacerbation during menstruation rendering her housebound for 3 days of each month. She had no dysmenorrhea or pelvic pain to suggest endometriosis. Sitting or lying for prolonged periods exacerbated the buttock pain and was associated with paresthesia over the posterior aspect of her right thigh, calf, heel, and dorsum of her right foot in addition to right gluteal muscle atrophy. The pain persisted despite strong analgesia and recommencing the oral contraceptive pill. She trialed physiotherapy and acupuncture without success. Investigations including ultrasound of her pelvis and right hip, as well as X-rays and computed tomography scans of her right hip and lumbosacral spine failed to identify any pathology. Finally, magnetic resonance imaging (MRI) scans of her pelvis revealed a 3.5 cm endometriotic lesion over the pelvic segment of her right sciatic nerve, before exiting the great sciatic foramen. MRI also identified atrophy of the right gluteus medius and minimus muscles, indicating the involvement of superior gluteal nerve [Figure 1].
Figure 1.
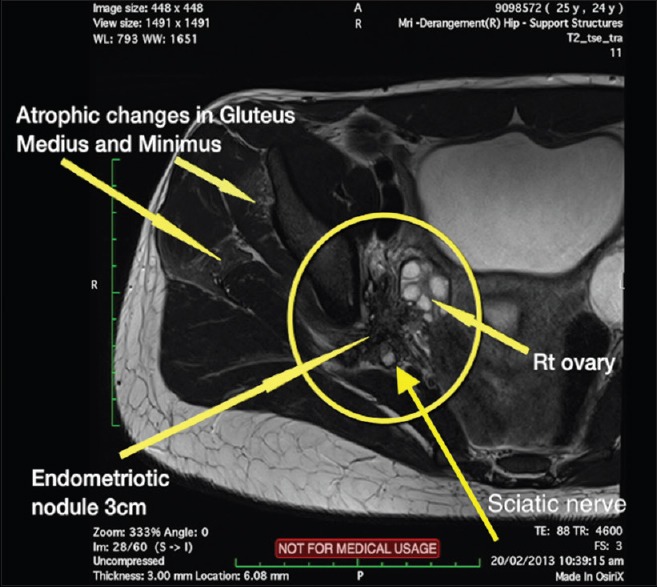
Magnetic resonance imaging of Miss AB, where an endometriotic nodule involving the sciatic nerve can be seen on the right. Atrophic changes in the gluteus minimus and medius can be seen as well
Miss AB was then referred to our unit, and following detailed gynecological consultation, she was also referred for a comprehensive neurosurgical review. Other than limited right straight leg raise, the remainder of her lower limb neurological examination was normal. Electromyography nerve conduction study demonstrated evidence of L5 radiculopathy. Following a multidisciplinary discussion with a neurosurgeon, an orthopedic surgeon, and a gynecological oncologist, the patient underwent laparoscopic excision of endometriosis.
Preoperatively, the patient underwent bowel preparation, with 24 hours of clear fluid and a single dose of PicoPrep (sodium picosulfate, magnesium oxide, and citric acid). The patient was placed in the standard dorsal lithotomy position. Primary trocar was inserted with open Hasson technique followed by three 5 mm accessory ports under direct vision in lower abdomen. Laparoscopic bipolar forceps and scissors without monopolar energy were used when operating close to the nerves to minimize injury due to lateral thermal spread from monopolar currents. Following thorough inspection of abdominal and pelvic cavities, noting no evidence of pelvic endometriosis, the endopelvic portion of the right sciatic nerve was approached through lumbosacral space as described by Possover et al.[6] A peritoneal incision parallel to the lateral aspect of external iliac artery was made, and the underlying vessels were carefully retracting medially, separating them from the adjacent psoas muscles. Dissection was carried out caudally to identify the proximal segment of the obturator nerve typically surrounded by adipose tissue at the level of pelvic brim in an oblique orientation toward the obturator foramen. The lumbosacral trunk was then identified lying caudally to the proximal obturator nerve, traveling toward the greater sciatic foramen, also surrounded by adipose tissue. The lumbosacral trunk at the pelvic brim, consisting primarily of L5 and S1 nerve roots, joins sacral nerve roots from the sacral foramina to form the endopelvic portion of sciatic nerve. By extending the dissection along the lumbosacral trunk, toward the greater sciatic notch, a large area of fibrosis was encountered encapsulating the structures ventral to the sciatic nerve. The fibrosis extended dorsally to the level of the iliolumbar vessels as they cross laterally to the psoas muscle; laterally over the obturator internus muscle fascia but not involving the underlying muscle; medially through the parametrium encasing distal branches of anterior division of internal iliac artery including uterine artery, superior vesical as well as obturator artery; and ventrally along the obturator nerve, reaching 1 cm short of obturator foramen. Within this area of fibrosis, the obturator nerve was also encased with fibrotic tissue and densely adherent to the obturator internus muscle fascia laterally [Figures 2 and 3]. Vessels that had to be divided in the process of excising this diseased fibrotic area included uterine artery, superior vesical, obliterated umbilical artery, and obturator artery as per Possover et al.[6] The fascia over the obturator internus muscle was involved with disease and was removed creating a disease-free interface at the lateral boundary. Disease over the sciatic nerve was removed piecemeal to minimize harm to the underlying nerve [Figure 4]. Significant fibrosis was present in the ventral-caudal border of the sciatic nerve where the pudendal nerve would be expected to exit the pelvis. As there were no symptoms of pudendal nerve involvement, further dissection was not carried out. The superior gluteal nerve could also not be clearly identified. Minimal residual disease and fibrosis were left to minimize potential serious neurovascular injury. Fibrosis and distortion of the anatomy made identification of anatomical landmark and course of vessels very difficult. A Mirena was fitted at the end of the procedure.
Figure 2.
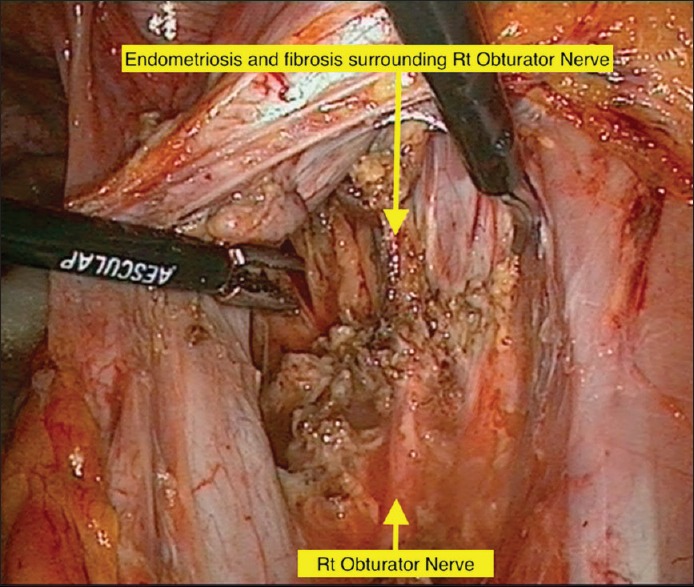
Right pelvic sidewall with right obturator nerve encased with endometriosis
Figure 3.
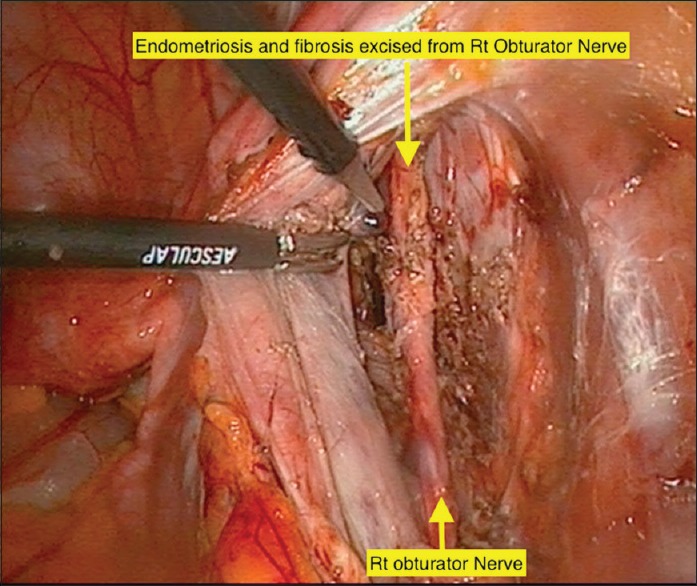
Right pelvic sidewall after having endometriosis excised from right obturator nerve
Figure 4.
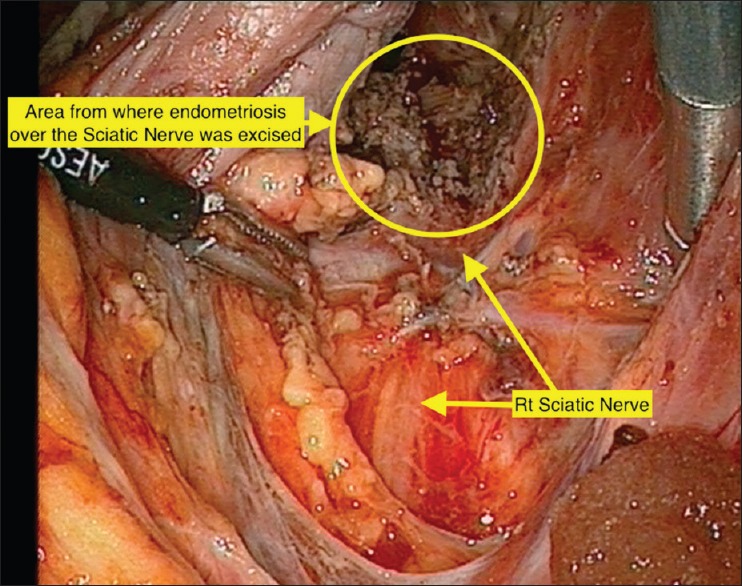
Right pelvic sidewall demonstrating right sciatic nerve and site where endometriosis was excised
Miss AB recovered well from her surgery with significant early improvement of pain and lower limb paresthesia over the first few days. It is not uncommon for patients to experience increased pain due to irritation of the sciatic nerve immediately after surgery. Postoperatively, she received 6 monthly injections of Zoladex (goserelin acetate), as has been used previously,[7] then continued on Primolut N (Norethisterone) 5 mg BD. She successfully conceived with in vitro fertilization 3 years after her surgery, following a failed course of Clomid (Clomiphene citrate) for anovulatory dysfunction. At the time of writing this article, she is 26-week pregnant.
DISCUSSION
Symptoms of endometriosis involving pelvic nerves
This case is an uncommon form of endometriosis with the disease only affecting the sciatic nerve, referred to as isolated endometriosis of the sciatic nerve. The sciatic nerve is the largest somatic nerve in the body. This condition can be very difficult to diagnose as it can present very much like a typical case of sciatica, which is commonly due to prolapsed disc compressing the adjacent nerve root as it exits the spine. Endometriosis over the endopelvic portion of the sciatic nerve, which is formed by the fusion of lumbosacral trunk (consisting of L5 and S1 and S2 nerve roots), can give rise to irritation over all three of these dermatomes. This results in a wider distribution of affected area as opposed to symptoms limited to a single dermatome from compression of a single nerve root by a specific bulging disc. Recent publication of the largest series of sciatic endometriosis by Possover identified the most common location of endometriotic involvement of the sciatic nerve is over the lateral aspect proximal to the greater sciatic foramen.[8] The pain caused by isolated endometriosis of the sciatic nerve is also usually related to the menstrual cycle. It is typically only present during menstruation initially and then becomes more constant over time with significant menstrual exacerbation. Response to hormonal treatment for endometriosis would provide further support for this uncommon diagnosis. While there have been limited reports of successful medical treatment for endometriosis of the sciatic nerve,[9] there are numerous publications of cases requiring surgical intervention due to nonresponse to medical treatment. The condition can progress and timely intervention has been recommended to prevent significant neurological injury. In a subset of 46 patients reported by Possover, who had >30% of sciatic nerve destroyed by sciatic nerve with gait disturbances and recovery required at least 3 years of intensive physiotherapy[8]
Clinical gynecological pelvic examination in patients with isolated endometriosis is usually unremarkable. Neurological findings may be present depending on the extend of neurological injury. Limitation of straight leg raising test is common with alteration of sensation along L5 and S1 dermatome with possible reduced power in ankle and changes to ankle reflex.
Investigations
Accurate diagnosis for this condition is essential for correct planning of surgical treatment. Due to diagnostic difficulty, a multidisciplinary team approach including neurosurgical and orthopedic involvement is necessary. Although there have been reports of using ultrasound for the assessment of endometriosis affecting the extrapelvic segment of the sciatic nerve,[9] MRI remains the imaging modality of choice for sciatic endometriosis. Endometriotic lesions exhibit high signal intensity on T1W images and high and low signal intensity on T2W images, depending on the stage of the hemorrhage.[10] There has been suggestion that the quality of imaging can be influenced by the phase of menstrual cycle.[11]
Unfortunately, not all cases of sciatic endometriosis will be identified on MRI.[5] Nevertheless, it is an important investigative test that will rule out other potential etiologies. Clinical diagnosis based on symptoms and examination findings may indicate a need for exploration of the lumbosacral space despite MRI findings. However, exploration of lumbosacral space should not be undertaken lightly due to its complex anatomy and potential for serious injury to the major neurovascular structures.
Treatment
Hormonal treatments can be tried and improvement in symptoms would support endometriosis as a possible etiology. However, as with this case with Miss AB, resumption of oral contraceptive did not help her symptoms and surgery was required. Possover et al.[6,12] have long advocated the laparoscopic approach to pathology involving pelvic nerves, where all the somatic and autonomic nerves in the pelvis can be identified and accessed. There are two main approaches to the retroperitoneally placed pelvic nerves. The midline approach, starting from the sacral promontory and traversing the hypogastric fascia, allows access to primarily autonomic nerves. These include the superior hypogastric plexus, sympathetic chain, sacral nerve roots and proximal sacral plexus, splanchnic nerves, and inferior hypogastric plexus. The lateral approach to lumbosacral fossa is performed by retracting the external iliac vessels to expose primarily somatic nerves; the obturator nerve, lumbosacral trunk, lateral aspect of sacral plexus, sciatic nerves, pudendal nerves, and superior and inferior gluteal nerves. While sciatic endometriosis in the presence of central disease may require both a midline and lateral approach, this case of isolated sciatic endometriosis only required the lateral approach.
Possover et al.[6] and Ceccaroni et al.[13] give a detailed description of the lateral approach to access the infracardinal portion of sacral plexus including the sciatic nerve. They warn injuring the pudendal vein and gluteal vessels in the area and emphasize the importance of dissecting and identifying the structures before excising of disease, so hemostasis can be conducted with low risk of injury to the neighboring neurological structures. It is also helpful to know that the obturator vessels and the distal branches of internal iliac artery including uterine artery can be divided to improve expose to the area.
This retroperitoneal neuroanatomical knowledge requires specific expertise. Neural structures can be quite difficult to identify due to their location and minuteness as well as their variability in shape and location. They are located in close proximity to major pelvic vessels; thus, injury to these nerves and vessels can lead to catastrophic consequences. Possover has published widely on his extensive work on pelvic nerve including the use of Laparoscopic Neuro-Navigation Techniques to assist the identification of individual sacral nerve roots by motor response of the foot to electrical stimulation.[6,12,13,14] Based on his extensive pioneering work on pelvic nerve anatomy and surgical experience in treating conditions associated with pelvic nerves, Possover has established a unique surgical pelvic medicine discipline called neuropelveology.[15] Better understanding of neuropelveology will improve our recognition of pelvic nerves and lead to a more refined surgery with sparing of these important pelvic structures. Neuropelveology has a wide scope of application to pelvic conditions including neuropelveological evaluation to chronic pelvic pain, vascular entrapment syndrome as well as the use of implantation of electrode for pelvic visceral dysfunction and even implantation of electrodes to pelvic nerve for assisting ambulation in patient with spinal cord injury.[16] In addition to this specialized knowledge, it also requires a high degree of laparoscopic surgical skill.
While multidisciplinary approach is essential, surgery is usually carried out by gynecologists who are more familiar with complex laparoscopic surgery for endometriosis of the pelvis. However, if disease extends beyond the pelvis, into the gluteal region, neurosurgical or orthopedic input will be required to perform a transgluteal approach.[17]
CONCLUSION
Isolated sciatic endometriosis is a rare presentation of endometriosis that can present in a manner similar to typical sciatica, which should be considered in a young female presenting with sciatic symptoms with no obvious etiology. Menstrual relationship to the symptoms should provide a clue to endometriosis as the possible cause. A multidisciplinary approach should be adopted, and a thorough understanding of the pelvic neuroanatomy and safe neurosurgical approach is essential.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.von Rokitansky C. Ueber uterusdrusen-neubildung in uterus and ovarialsarcomen (uterine gland proliferation in uterine and ovarian sarcomas) Z Ges Fur Aerzte Zu Wien. 1860;37:577. [Google Scholar]
- 2.Asante A, Taylor RN. Endometriosis: The role of neuroangio-genesis. Annu Rev Physiol. 2011;73:163–82. doi: 10.1146/annurev-physiol-012110-142158. [DOI] [PubMed] [Google Scholar]
- 3.Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:511–9. doi: 10.1016/j.fertnstert.2012.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: Pathogenesis and treatment. Nat Rev Endocrinol. 2014;10:261–75. doi: 10.1038/nrendo.2013.255. [DOI] [PubMed] [Google Scholar]
- 5.Possover M, Chiantera V. Isolated infiltrative endometriosis of the sciatic nerve: A report of three patients. Fertil Steril. 2007;87:417.e17–9. doi: 10.1016/j.fertnstert.2006.05.084. [DOI] [PubMed] [Google Scholar]
- 6.Possover M, Baekelandt J, Flaskamp C, Li D, Chiantera V. Laparoscopic neurolysis of the sacral plexus and the sciatic nerve for extensive endometriosis of the pelvic wall. Minim Invasive Neurosurg. 2007;50:33–6. doi: 10.1055/s-2007-970075. [DOI] [PubMed] [Google Scholar]
- 7.Ceccaroni M, Clarizia R, Cosma S, Pesci A, Pontrelli G, Minelli L, et al. Cyclic sciatica in a patient with deep monolateral endometriosis infiltrating the right sciatic nerve. J Spinal Disord Tech. 2011;24:474–8. doi: 10.1097/BSD.0b013e31820fc53b. [DOI] [PubMed] [Google Scholar]
- 8.Possover M. Five-year follow-up after laparoscopic large nerve resection for deep infiltrating sciatic nerve endometriosis. J Minim Invasive Gynecol. 2017;24:822–6. doi: 10.1016/j.jmig.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 9.Arányi Z, Polyák I, Tóth N, Vermes G, Göcsei Z. Ultrasonography of sciatic nerve endometriosis. Muscle Nerve. 2016;54:500–5. doi: 10.1002/mus.25152. [DOI] [PubMed] [Google Scholar]
- 10.Cimsit C, Yoldemir T, Akpinar IN. Sciatic neuroendometriosis: Magnetic resonance imaging defined perineural spread of endometriosis. J Obstet Gynaecol Res. 2016;42:890–4. doi: 10.1111/jog.12998. [DOI] [PubMed] [Google Scholar]
- 11.Capek S, Amrami KK, Howe BM, Collins MS, Sandroni P, Cheville JC, et al. Sequential imaging of intraneural sciatic nerve endometriosis provides insight into symptoms of cyclical sciatica. Acta Neurochir (Wien) 2016;158:507–12. doi: 10.1007/s00701-015-2683-2. [DOI] [PubMed] [Google Scholar]
- 12.Possover M, Rhiem K, Chiantera V. The “Laparoscopic neuro-navigation” – LANN: From a functional cartography of the pelvic autonomous neurosystem to a new field of laparoscopic surgery. Minim Invasive Ther Allied Technol. 2004;13:362–7. doi: 10.1080/13645700410005392. [DOI] [PubMed] [Google Scholar]
- 13.Ceccaroni M, Clarizia R, Alboni C, Ruffo G, Bruni F, Roviglione G, et al. Laparoscopic nerve-sparing transperitoneal approach for endometriosis infiltrating the pelvic wall and somatic nerves: Anatomical considerations and surgical technique. Surg Radiol Anat. 2010;32:601–4. doi: 10.1007/s00276-010-0624-6. [DOI] [PubMed] [Google Scholar]
- 14.Possover M, Chiantera V, Baekelandt J. Anatomy of the sacral roots and the pelvic splanchnic nerves in women using the LANN technique. Surg Laparosc Endosc Percutan Tech. 2007;17:508–10. doi: 10.1097/SLE.0b013e31812f81e4. [DOI] [PubMed] [Google Scholar]
- 15.Possover M, Forman A, Rabischong B, Lemos N, Chiantera V. Neuropelveology: New groundbreaking discipline in medicine. J Minim Invasive Gynecol. 2015;22:1140–1. doi: 10.1016/j.jmig.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Possover M, Forman A. Recovery of supraspinal control of leg movement in a chronic complete flaccid paraplegic man after continuous low-frequency pelvic nerve stimulation and FES-assisted training. Spinal Cord Ser Cases. 2017;3:16034. doi: 10.1038/scsandc.2016.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiang H, Liang Y, Li L, Gu L, Yao S. Cyclic sciatica due to endometriosis of the sciatic nerve: Neurolysis with combined laparoscopic and transgluteal approaches: A Case report. JBJS Case Connect. 2014;4:1–4. doi: 10.2106/JBJS.CC.M.00234. [DOI] [PubMed] [Google Scholar]


