Abstract
Objective
The aim of the study was to investigate the root canal morphology of maxillary first and second premolars in a Saudi population using Cone-Beam Computed Tomography (CBCT).
Methods
This retrospective cross-sectional study assessed CBCT images of 707 Saudi patients. The number of roots and canal configuration were identified based on Vertucci's classification. Fisher's exact Chi-square tests were performed to analyze the association between sex and number of roots and sex and root canal configuration.
Results
Most teeth had two roots in maxillary first premolars (75.1%) and one root in maxillary second premolars (85.2%). Type IV was the most prevalent canal configuration in maxillary first premolars (69.1%), while Type I was the most in maxillary second premolars (49.4%). All types of canal configurations were observed in maxillary premolars except Type VII for the maxillary second premolar. Chi-square tests showed no significant association between gender and number of roots and sex and root canal configuration in both maxillary first and second premolars although higher number of roots was seen in men (P > 0.05).
Conclusion
Most maxillary first premolars had two roots with Type IV being the most predominant canal configuration, while a single root with Type I canal configuration was the most frequently observed morphology in maxillary second premolars. In maxillary first premolars, 21.3% had one canal apically, 75.4% had two canals apically, and 3.3% had three canals apically. In maxillary second premolars, 80.2% had one canal apically, 18.9% had two canals apically, and 0.9% had three canals apically.
1. Introduction
Proper knowledge of the anatomy of the root canal system and its morphological variations plays a significant role in all the steps of endodontic treatment [1–3]. Therefore, the clinician should have a thorough understanding of the detailed anatomy of the root canal in order to utilize the most appropriate treatment techniques and protocols and thereby increase the success rate [4].
The anatomical variations of the root canal system are crucial in endodontic treatment. The untreated missing root canal will lead to persistent presence of microorganisms and necrotic tissue inside the canal, which may result in development of apical pathosis [5].
Different classifications have described the root canal systems of human permanent teeth including the Weine [6], Vertucci [1], and Gulabivala [7] classifications. Vertucci's classification is considered the most widely used and includes eight categories: Type I (1), Type II (2-1), Type III (1-2-1), Type IV (2), Type V (1-2), Type VI (2-1-2), Type VII (1-2-1-2), and Type VIII (3). Root canal treatment of premolar teeth is reportedly very challenging due to anatomical variations in the number of roots and types of canal configurations [3, 8–11].
The maxillary first premolars are considered among the most difficult teeth to be endodontically treated because of the number of roots and canals, the direction and longitudinal depressions of the roots, the various pulp cavity configurations, and the difficulties in visualizing the apical limit on periapical radiographs [12]. Moreover, high variability has been reported in the root canal morphology of the maxillary second premolars [1, 13–15].
Different methods have been utilized to investigate root canal anatomy including in vivo and in vitro methods. The in vivo techniques include clinical evaluation during root canal treatment, retrospective assessment of patient records, conventional radiographic evaluation, and advanced radiographic techniques such as cone-beam computed radiography (CBCT) [16–18], while the in vitro methods include canal staining and tooth clearing [1, 19], root sectioning [6], microscopic examination, examination of conventional radiographs, and using three-dimensional modalities such as microcomputed tomography (μ-CT) [20–22].
The CBCT technique has the ability to detect root canal morphology as precisely as the root canal staining and clearing techniques which, in the past, were considered superior to conventional techniques used for studying the root canal system because of their ability to provide three-dimensional views and complete morphologic details [5].
To the best of our knowledge, no study has so far evaluated the root canal morphology of maxillary premolars of both sexes in a Saudi population using CBCT. Therefore, the aim of the study was to investigate the root canal morphology of maxillary first and second premolars in a Saudi population using CBCT.
2. Materials and Methods
Seven hundred and seven CBCT images of Saudi patients (396 female, 311 male) aged between 16 and 71 years, with average age of 41.5 years, seeking routine dental treatment who were referred to the Radiology Department of the College of Dentistry, King Saud University, between 2015 and 2017 were collected.
The sampling was purposive where the presence of at least one maxillary first and/or second premolar with fully developed roots was the inclusion criterion. Unclear or distorted CBCT images, previously endodontically initiated or treated teeth, teeth with posts or crowns, periapical lesions, and any physiological or pathological process such as immature apex were excluded. The total final sample, consisting of 334 maxillary first premolars and 318 maxillary second premolars, was evaluated in terms of number of roots and root canal configuration. The data were observed and recorded for the number of roots and canal configuration based on Vertucci's classification [1]. The sex of the patients was also recorded.
The CBCT images were accessed and evaluated at the Radiology Department of the College of Dentistry, King Saud University, by two endodontists for the number of roots and root canal configuration using the using the Planmeca Romexis Viewer software (Planmeca, Roselle IL). The images were collected from different CBCT machines: CS9300 3D digital imaging system (Carestream, Rochester, NY) with a voxel size of 90 to 300 μm and Planmeca ProMax 3D (Planmeca, Roselle IL) with a voxel size of ≤ 200 μm.
To ensure the reliability of the results, inter- and intraexaminer reliabilities were measured by identifying the root canal anatomy of maxillary premolars of 30 randomly selected CBCT images according to the evaluation criteria. For intraexaminer reliability, the same images were evaluated after 1 week. Both inter- and intraexaminer reliabilities were calculated using the interclass correlation coefficient (ICC). Data were analyzed with Fisher's exact test using SPSS software version 22 (SPSS Inc., Chicago, IL, USA). The significance was set at the 95% confidence level.
3. Results
For interexaminer reliability, the ICC was 0.886 (excellent) for the number of roots and 0.625 (good) for canal configuration. For intraexaminer reliability, the ICC was 1 for the first examiner with regard to number of roots and canal configuration and 1 and 0.95 for the second examiner with regard to number of roots and canal configuration, respectively. The ICCs verified that the procedure was reliable for the evaluations and measurements performed by the two observers.
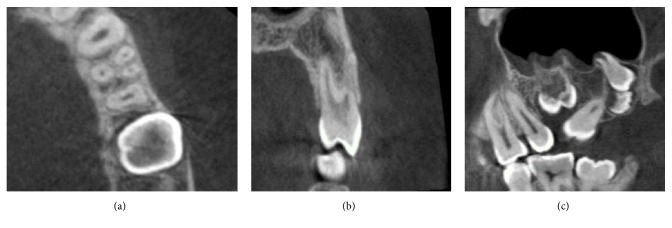
The number of roots recorded in maxillary first and second premolars was up to three roots (Figure 1). In maxillary first premolars, most teeth had two roots (75.1%), while in maxillary second premolars most were single rooted (85.2%). Type IV canal configuration (69.1%) was the most prevalent observation in maxillary first premolars, while Type I (49.4%) was the most prevalent configuration in maxillary second premolars. The frequency and percentage of number of roots and canal configuration in maxillary first and second premolars are shown in Tables 1 and 2, respectively.
Figure 1.
CBCT of maxillary first premolar with three roots: (a) the axial plane, (b) the coronal plane, and (c) the sagittal plane.
Table 1.
The frequency and percentage of number of roots and canal configuration in maxillary first premolar teeth.
| Number of Roots | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| One Root | Two Roots | Three Roots | Total | |||||||
| Frequency (%) | Women | 43 (26.5%) | 119 (73.5%) | 0 (0%) | 162 (100%) | |||||
| Men | 36 (20.9%) | 132 (76.8%) | 4 (2.3%) | 172 (100%) | ||||||
| Total | 79 (23.7%) | 251 (75.1%) | 4 (1.2%) | 334 (100%) | ||||||
|
| ||||||||||
| Canal Configuration | ||||||||||
|
| ||||||||||
| Type I (1) | Type II (2-1) | Type III (1-2-1) | Type IV (2) | Type V (1-2) | Type VI (2-1-2) | Type VII (1-2-1-2) | Type VIII (3) | Total | ||
|
| ||||||||||
| Frequency (%) | Women | 15 (9.3%) | 17 (10.5%) | 5 (3.1%) | 112 (69.1%) | 9 (5.6%) | 3 (1.8%) | 0 (0%) | 1 (0.6%) | 162 (100%) |
| Men | 21 (12.2%) | 11 (6.4%) | 1 (0.6%) | 124 (72.1%) | 4 (2.3%) | 4 (2.3%) | 1 (0.6%) | 6 (3.5%) | 172 (100%) | |
| Total | 36 (10.8%) | 28 (8.4%) | 6 (1.8%) | 236 (70.6%) | 13 (3.9%) | 7 (2.1%) | 1 (0.3%) | 7 (2.1%) | 334 (100%) | |
Table 2.
The frequency and percentage of number of roots and canal configuration in maxillary second premolar teeth.
| Number of Roots | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| One Root | Two Roots | Three Roots | Total | |||||||
| Frequency (%) | Women | 138 (87.3%) | 20 (12.7%) | 0 (0%) | 158 (100%) | |||||
| Men | 133 (83.1%) | 26 (16.3%) | 1 (0.6%) | 159 (100%) | ||||||
| Total | 271 (85.2%) | 46 (14.5%) | 1 (0.3%) | 318 (100%) | ||||||
|
| ||||||||||
| Canal Configuration | ||||||||||
|
| ||||||||||
| Type I (1) | Type II (2-1) | Type III (1-2-1) | Type IV (2) | Type V (1-2) | Type VI (2-1-2) | Type VII (1-2-1-2) | Type VIII (3) | Total | ||
|
| ||||||||||
| Frequency (%) | Women | 80 (50.6%) | 38 (24.0%) | 10 (6.3%) | 15 (9.5%) | 8 (5.1%) | 5 (3.2%) | 0 (0%) | 2 (1.3%) | 158 (100%) |
| Men | 77 (48.1%) | 44 (27.5%) | 6 (3.8%) | 22 (13.8%) | 10 (6.2%) | 0 (0%) | 0 (0%) | 1 (0.6%) | 160 (100%) | |
| Total | 157 (49.4%) | 82 (25.8%) | 16 (5%) | 37 (11.6%) | 18 (5.7%) | 5 (1.6%) | 0 (0%) | 3 (0.9%) | 318 (100%) | |
A higher percentage of three-rooted maxillary first premolars was observed in men (2.3%) and none in women (0%), while the most predominant root morphology seen in both sexes was two rooted, with no statistically significant difference (P = 0.078). In canal configurations, there were no statistically significant differences in all types between the sexes (P = 0.095).
In maxillary second premolars, there was no statistically significant difference in number of roots between the sexes (P = 0.383). Although Type III, VI, and VIII canal configurations were more frequent in female patients and Type II, IV, and V in male patients, the difference was not statistically significant (P = 0.257).
Both right and left maxillary first premolars were present in 170 patients. Symmetrical number of roots and canal configuration were seen in 91.2% of teeth, while 2.3% showed symmetrical number of roots but different canal configuration and 0.6% showed symmetrical canal configuration but different number of roots. Moreover, 5.9% of teeth did not show any type of symmetry.
In 163 patients, right and left maxillary second premolars were present. Symmetrical numbers of roots and canal configuration were seen in 85.3% of teeth, while 11% showed symmetrical number of roots but different canal configuration. Only 3.7% showed no type of symmetry.
4. Discussion
Patient ethnicity is an incontrovertible factor that may affect the perception of the clinician for the suspected root canal anatomy. In the present study, maxillary premolars in a Saudi population, where the majority is Arab, presented with up to three roots and included most of Vertucci's types of canal configuration with similarities and differences to the other reported studies in different populations. Moreover, sex predilection and symmetrical anatomy were investigated to evaluate their significance in the prediction of root canal anatomy.
CBCT is reportedly an excellent tool for more accurately detecting root canal anatomy than intraoral periapical radiography due to its ability to evaluate and assess root canal morphology in three dimensions [5, 23–27]. The data of this retrospective study were collected from a single center, King Saud University Dental Hospital, which is considered one of the largest governmental dental institutes providing free dental services to a large portion of the Saudi population from different regions. To avoid exposing a large number of patients to unnecessary radiation, a CBCT imaging database was accessed regardless of the voxel size to achieve a larger sample size.
In maxillary first premolars, the prevalence of one root was reported to be 22% to 66%, of two roots 33% to 84%, and of three roots 0% to 6% [28–34]. In maxillary second premolars, the prevalence of one root was reported to be 69.6% to 90.3%, of two roots 9.7% to 29.7%, and of three roots 0% to 1.6% [30, 34–37].
In maxillary first premolars in the present study, the most frequently observed root morphology was two rooted (75.1%), followed by single rooted (23.7%), and three rooted (1.2%). These findings are consistent with those reported by Elkady and Allouba, using CBCT, who reported that, in maxillary first premolars in Saudi subpopulation, the prevalence of one root was 28.3% and of two roots 71.7%, while no three roots were observed [38]. In another study with a Saudi population, using visual, digital radiography and transverse sectioning methods, in maxillary first premolars, the prevalence of one root was reported to be 17.9%, of two roots 80.9%, and of three roots 1.2% [16].
Regarding canal configuration, all types of Vertucci's classification were observed in this study, which it is in line with Vertucci and Gegauff's findings [32]. Most patients had Type IV canal configurations, followed by Type I, Type II, and finally Type VII. In comparison to other studies included in a literature review [39], Type IV canal configuration was reported to be 65.3% in Saudi population, followed by Type II (19.7%), Type I (7.6%), Type III (3.3%), Types V, VI, and VII (3.3%), and finally Type VIII (0.8%).
In maxillary second premolars, up to three-rooted teeth were observed. The highest prevalence was single rooted followed by double rooted and three rooted (0.3%). Additionally, the majority exhibited Type I canal configuration, followed by Type II and Type IV. These findings coincide with those of other studies conducted in Saudi Arabia, where one root was observed in 76.4% and 67%, two roots in 23.6% and 30%, and three roots in 0% and 3% teeth [38, 40]. Moreover, Type I canal configuration was seen in 36.3% and 17%, Type II in 10.9% and 7%, and Type IV in 23.6% and 23% teeth [38, 40].
Compared to a recent CBCT study by Abella et al. [37] in Spanish population, in maxillary first premolars, the most prevalent root morphology observed was two rooted (51.4%) and most of the teeth exhibited Type IV canal configuration (52.8%), while in maxillary second premolars, the most prevalent root morphology seen was single rooted (82.9%) and most of these teeth exhibited Type I canal configuration (47.2%). Moreover, two-rooted maxillary first premolars were reported to be 33% with 51% having Type IV canal configuration in a Chinese population [41], 68.6% with 68% having Type I canal configuration in a Pakistani population [42], and 44.8% with 76.8% having Type IV canal configuration in a Turkish Cypriot population [43]. Additionally, single-rooted maxillary second premolars were reported to be 84% with 53.4% having Type I canal configuration in a Pakistani population [42], and Type I canal configuration was the most commonly observed in a Turkish Cypriot population (49.4%) [43].
Sex predilection regarding the number of roots and root canal morphology has been reported [44–47]. Martins et al. [48] reported that female patients in a Portuguese population had a lower number of roots in both maxillary first and second premolars with a statistically significant difference in the maxillary first premolars. Moreover, Type IV canal configuration in maxillary first premolars was more frequent in male patients and Type I canal configuration in maxillary second premolars was more in female patients with a statistical significant difference (P < 0.05), while Abella et al. [37] reported that there was no statistically significant correlation between the number of roots and the sexes in Spanish population. In this study, there was no statistically significant correlation between sex and number of roots or sex and root canal configuration in both maxillary first and second premolars although a higher number of roots were seen in men (P > 0.05).
The degree of bilateral symmetry in root canal morphology using CBCT has been reported in different studies. For maxillary first premolars, bilateral symmetry was observed in 88.5% of teeth for the number of roots and in 77% for canal configuration in Saudi patients [38], and symmetry of 64% was reported for both number of roots and canal configuration in a Chinese population [41]. In maxillary second premolars, bilateral symmetry was observed in 84% of teeth for the number of roots and in 76% for canal configuration [38]. The findings of the present study are in agreement with those of the previous studies where a high degree of symmetry in the number of roots and canal configuration was seen in both maxillary first and second premolars.
5. Conclusion
Within its limitations, in this study with a Saudi population, most maxillary first premolars had two roots with Type IV being the most predominant canal configuration, while a single root with Type I canal configuration was the most frequently observed morphology in maxillary second premolars. Moreover, more than one root with different canal configurations was detected in some cases. Further studies with larger sample sizes are recommended for the generalization of our results.
Acknowledgments
The authors thank College of Dentistry Research Center, King Saud University, for their support in conducting this project (CDRC no. FR 0440, IRB Research Project no. E-18-3090) and the Deanship of Scientific Research and RSSU at King Saud University for their technical support. The authors also thank Dr. Ahmed Qattan (General Practitioner, Thadiq General Hospital, Saudi Arabia) for his efforts in data collection. There was no financial support for this study.
Data Availability
The CBCT images data used to support the findings of this study are restricted by the local institutional review board at King Saud University in order to protect patients' privacy.
Ethical Approval
The study was independently reviewed and approved by the local institutional review board (No. E-18-3090) at King Saud University and conducted in full accordance with the World Medical Association Declaration of Helsinki.
Consent
Consent was not required for this type of study. The data was anonymised and deidentified prior to analysis.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Vertucci F. J. Root canal anatomy of the human permanent teeth. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 1984;58(5):589–599. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 2.Vertucci F. J. Root canal morphology and its relationship to endodontic procedures. Endodontic Topics. 2005;10(1):3–29. doi: 10.1111/j.1601-1546.2005.00129.x. [DOI] [Google Scholar]
- 3.Nallapati S. Three canal mandibular first and second premolars: A treatment approach. Journal of Endodontics. 2005;31(6):474–476. doi: 10.1097/01.don.0000157986.69173.a6. [DOI] [PubMed] [Google Scholar]
- 4.Jou Y., Karabucak B., Levin J., Liu D. Endodontic working width: current concepts and techniques. Dental Clinics of North America. 2004;48(1):323–335. doi: 10.1016/j.cden.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Neelakantan P., Subbarao C., Subbarao C. V. Comparative evaluation of modified canal staining and clearing technique, cone-beam computed tomography, peripheral quantitative computed tomography, spiral computed tomography, and plain and contrast medium-enhanced digital radiography in studying root C. Journal of Endodontics. 2010;36(9):1547–1551. doi: 10.1016/j.joen.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Weine F. S., Healey H. J., Gerstein H., Evanson L. Canal configuration in the mesiobuccal root of the maxillary first molar and its endodontic significance. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 1969;28(3):419–425. doi: 10.1016/0030-4220(69)90237-0. [DOI] [PubMed] [Google Scholar]
- 7.Gulabivala K., Aung T. H., Alavi A., Ng Y.-L. Root and canal morphology of Burmese mandibular molars. International Endodontic Journal. 2001;34(5):359–370. doi: 10.1046/j.1365-2591.2001.00399.x. [DOI] [PubMed] [Google Scholar]
- 8.Cleghorn B. M., Christie W. H., Dong C. C. S. The root and root canal morphology of the human mandibular first premolar: a literature review. Journal of Endodontics. 2007;33(5):509–516. doi: 10.1016/j.joen.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Cleghorn B. M., Christie W. H., Dong C. C. S. The root and root canal morphology of the human mandibular second premolar: a literature review. Journal of Endodontics. 2007;33(9):1031–1037. doi: 10.1016/j.joen.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 10.Kottoor J., Albuquerque D., Velmurugan N., Kuruvilla J. Root anatomy and root canal configuration of human permanent mandibular premolars: a systematic review. Anatomy Research International. 2013;2013:14. doi: 10.1155/2013/254250.254250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slowey R. R. Root canal anatomy. Road map to successful endodontics. Dental Clinics of North America. 1979;23(4):555–573. [PubMed] [Google Scholar]
- 12.Pécora J. D., Saquy P. C., Sousa Neto M. D., Woelfel J. B. Root form and canal anatomy of maxillary first premolars. Brazilian Dental Journal. 1992;2(2):87–94. [PubMed] [Google Scholar]
- 13.Vertucci F., Seelig A., Gillis R. Root canal morphology of the human maxillary second premolar. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 1974;38(3):456–464. doi: 10.1016/0030-4220(74)90374-0. [DOI] [PubMed] [Google Scholar]
- 14.Sert S., Bayirli G. S. Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. Journal of Endodontics. 2004;30(6):391–398. doi: 10.1097/00004770-200406000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Sardar K. P., Khokhar N. H., Siddiqui I. Frequency of two canals in maxillary second premolar tooth. Journal of the College of Physicians and Surgeons--Pakistan: JCPSP. 2007;17:12–14. [PubMed] [Google Scholar]
- 16.Atieh M. A. Root and canal morphology of maxillary first premolars in a Saudi population. The Journal of Contemporary Dental Practice. 2008;9:46–53. [PubMed] [Google Scholar]
- 17.Pattanshetti N., Gaidhane M., Al Kandari A. M. Root and canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait population—a clinical study. International Endodontic Journal. 2008;41(9):755–762. doi: 10.1111/j.1365-2591.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- 18.De Oliveira S. H. G., De Moraes L. C., Faig-Leite H., Afonso Camargo S. E., Camargo C. H. R. In vitro incidence of root canal bifurcation in mandibular incisors by radiovisiography. Journal of Applied Oral Science. 2009;17(3):234–239. doi: 10.1590/S1678-77572009000300020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Awawdeh L., Abdullah H., Al-Qudah A. Root form and canal morphology of jordanian maxillary first premolars. Journal of Endodontics. 2008;34(8):956–961. doi: 10.1016/j.joen.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 20.Grover C., Shetty N. Methods to study root canal morphology: A review. ENDO - Endodontic Practice Today. 2012:171–182. [Google Scholar]
- 21.Cleghorn B. M., Christie W. H., Dong C. C. S. Root and root canal morphology of the human permanent maxillary first molar: a literature review. Journal of Endodontics. 2006;32(9):813–821. doi: 10.1016/j.joen.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 22.Plotino G., Grande N. M., Pecci R., Bedini R., Pameijer C. H., Somma F. Three-dimensional imaging using microcomputed tomography for studying tooth macromorphology. The Journal of the American Dental Association. 2006;137(11):1555–1561. doi: 10.14219/jada.archive.2006.0091. [DOI] [PubMed] [Google Scholar]
- 23.Matherne R. P., Angelopoulos C., Kulild J. C., Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. Journal of Endodontics. 2008;34(1):87–89. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 24.Domark J. D., Hatton J. F., Benison R. P., Hildebolt C. F. An ex vivo comparison of digital radiography and cone-beam and micro computed tomography in the detection of the number of canals in the mesiobuccal roots of maxillary molars. Journal of Endodontics. 2013;39(7):901–905. doi: 10.1016/j.joen.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soares De Toubes K. M. P., Côrtes M. I. D. S., Valadares M. A. D. A., Fonseca L. C., Nunes E., Silveira F. F. Comparative analysis of accessory mesial canal identification in mandibular first molars by using four different diagnostic methods. Journal of Endodontics. 2012;38(4):436–441. doi: 10.1016/j.joen.2011.12.035. [DOI] [PubMed] [Google Scholar]
- 26.Zhang D., Chen J., Lan G., et al. The root canal morphology in mandibular first premolars: a comparative evaluation of cone-beam computed tomography and micro-computed tomography. Clinical Oral Investigations. 2017;21(4):1007–1012. doi: 10.1007/s00784-016-1852-x. [DOI] [PubMed] [Google Scholar]
- 27.Vizzotto M. B., Silveira P. F., Arús N. A., Montagner F., Gomes B. P. F. A., da Silveira H. E. D. CBCT for the assessment of second mesiobuccal (MB2) canals in maxillary molars teeth: effect of voxel size and presence of root filling. International Endodontic Journal. 2013;46(9):870–876. doi: 10.1111/iej.12075. [DOI] [PubMed] [Google Scholar]
- 28.Carns E. J., Skidmore A. E. Configurations and deviations of root canals of maxillary first premolars. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 1973;36(6):880–886. doi: 10.1016/0030-4220(73)90340-X. [DOI] [PubMed] [Google Scholar]
- 29.Loh H. S. Root morphology of the maxillary first premolar in Singaporeans. Australian Dental Journal. 1998;43(6):399–402. doi: 10.1111/j.1834-7819.1998.tb00199.x. [DOI] [PubMed] [Google Scholar]
- 30.Kartal N., Özçelik B., Cimilli H. Root canal morphology of maxillary premolars. Journal of Endodontics. 1998;24(6):417–419. doi: 10.1016/S0099-2399(98)80024-1. [DOI] [PubMed] [Google Scholar]
- 31.Bellizzi R., Hartwell G. Radiographic evaluation of root canal anatomy of in vivo endodontically treated maxillary premolars. Journal of Endodontics. 1985;11(1):37–39. doi: 10.1016/S0099-2399(85)80104-7. [DOI] [PubMed] [Google Scholar]
- 32.Vertucci F. J., Gegauff A. Root canal morphology of the maxillary first premolar. Journal of the American Dental Association. 1979;99(2):194–198. doi: 10.14219/jada.archive.1979.0255. [DOI] [PubMed] [Google Scholar]
- 33.Senan E. M., Alhadainy H. A., Genaid T. M., Madfa A. A. Root form and canal morphology of maxillary first premolars of a Yemeni population. BMC Oral Health. 2018;18, article 94 doi: 10.1186/s12903-018-0555-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martins J. N., Gu Y., Marques D., Francisco H., Caramês J. Differences on the Root and Root Canal Morphologies between Asian and White Ethnic Groups Analyzed by Cone-beam Computed Tomography. Journal of Endodontics. 2018;44(7):1096–1104. doi: 10.1016/j.joen.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Pécora J. D., Sousa Neto M. D., Saquy P. C., Woelfel J. B. In vitro study of root canal anatomy of maxillary second premolars. Brazilian Dental Journal. 1993;3(2):81–85. [PubMed] [Google Scholar]
- 36.Yang L., Chen X., Tian C., Han T., Wang Y. Use of Cone-beam Computed Tomography to Evaluate Root Canal Morphology and Locate Root Canal Orifices of Maxillary Second Premolars in a Chinese Subpopulation. Journal of Endodontics. 2014;40(5):630–634. doi: 10.1016/j.joen.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 37.Abella F., Teixidó L. M., Patel S., Sosa F., Duran-Sindreu F., Roig M. Cone-beam Computed Tomography Analysis of the Root Canal Morphology of Maxillary First and Second Premolars in a Spanish Population. Journal of Endodontics. 2015;41(8):1241–1247. doi: 10.1016/j.joen.2015.03.026. [DOI] [PubMed] [Google Scholar]
- 38.Elkady A., Allouba K. Cone beam computed tomographic analysis of root and canal morphology of maxillary premolars in Saudi subpopulation. Egyptian Dental Journal. 2013;59:3419–3429. [Google Scholar]
- 39.Ahmad I. A. Root and root canal morphology of Saudi Arabian permanent dentition. Saudi Endodontic Journal. 2015;5(2):99–106. doi: 10.4103/1658-5984.155446. [DOI] [Google Scholar]
- 40.Elnour M., Khabeer A., AlShwaimi E. Evaluation of root canal morphology of maxillary second premolars in a Saudi Arabian sub-population: An in vitro microcomputed tomography study. The Saudi Dental Journal. 2016;28(4):162–168. doi: 10.1016/j.sdentj.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tian Y.-., Guo B., Zhang R., et al. Root and canal morphology of maxillary first premolars in a Chinese subpopulation evaluated using cone-beam computed tomography. International Endodontic Journal. 2012;45(11):996–1003. doi: 10.1111/j.1365-2591.2012.02059.x. [DOI] [PubMed] [Google Scholar]
- 42.Nazeer M. R., Khan F. R., Ghafoor R. Evaluation of root morphology and canal configuration of maxillary premolars in a sample of Pakistani population by using cone beam computed tomography. Journal of the Pakistan Medical Association. 2018;68(3):423–427. [PubMed] [Google Scholar]
- 43.Celikten B., Orhan K., Aksoy U., et al. Cone-beam CT evaluation of root canal morphology of maxillary and mandibular premolars in a Turkish Cypriot population. BDJ Open. 2016;2, article 15006 doi: 10.1038/bdjopen.2015.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arslan H., Ertas H., Tarim Ertas E., Kalabalik F., Saygili G., Davut Capar I. Evaluating root canal configuration of mandibular incisors with cone-beam computed tomography in a Turkish population. Journal of Dental Sciences. 2015;10(4):359–364. doi: 10.1016/j.jds.2014.01.002. [DOI] [Google Scholar]
- 45.Caputo B. V., Noro Filho G. A., de Andrade Salgado D. M. R., Moura-Netto C., Giovani E. M., Costa C. Evaluation of the Root Canal Morphology of Molars by Using Cone-beam Computed Tomography in a Brazilian Population: Part I. Journal of Endodontics. 2016;42(11):1604–1607. doi: 10.1016/j.joen.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 46.Bulut D. G., Kose E., Ozcan G., Sekerci A. E., Canger E. M., Sisman Y. Evaluation of root morphology and root canal configuration of premolars in the Turkish individuals using cone beam computed tomography. European Journal of Dentistry. 2015;9(4):551–557. doi: 10.4103/1305-7456.172624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bürklein S., Heck R., Schäfer E. Evaluation of the root canal anatomy of maxillary and mandibular premolars in a selected german population using cone-beam computed tomographic data. Journal of Endodontics. 2017;43(9):1448–1452. doi: 10.1016/j.joen.2017.03.044. [DOI] [PubMed] [Google Scholar]
- 48.Martins J. N. R., Marques D., Francisco H., Caramês J. Gender influence on the number of roots and root canal system configuration in human permanent teeth of a Portuguese subpopulation. Quintessence International. 2018;49(2):103–111. doi: 10.3290/j.qi.a39508. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The CBCT images data used to support the findings of this study are restricted by the local institutional review board at King Saud University in order to protect patients' privacy.