Abstract
OBJECTIVE
We examined the effect of Medicare’s expansion of colorectal cancer (CRC) screening test reimbursement on racial/ethnic disparities in CRC screening.
METHODS
CRC screening was ascertained for Medicare beneficiaries (n=30,893), aged 70-89, who had no history of any tumor and resided in 16 Surveillance, Epidemiology and End Results regions of the United States from 1996 to 2005. CRC screening tests were identified in the 5% sample of Medicare claims. Age-gender-adjusted percentages and adjusted odds of receiving any guideline-specific CRC screening (i.e., annual fecal occult blood test (FOBT), sigmoidoscopy every 5 years or colonoscopy every 10 years) by race/ethnicity and Medicare coverage expansion period (i.e., prior to FOBT coverage, FOBT coverage only and post colonoscopy coverage) were reported.
RESULTS
CRC screening increased as Medicare coverage expanded for white and black Medicare beneficiaries. However, blacks were less likely than whites to receive screening prior to FOBT coverage (OR=0.74, 95% CI: 0.61-0.90), during FOBT coverage only (OR=0.66, 95% CI: 0.52-0.83) and after colonoscopy coverage (OR=0.80, 95% CI: 0.68-0.95). Hispanics were less likely to receive screening after colonoscopy coverage (OR=0.73, 95% CI: 0.54-0.99).
CONCLUSIONS
Despite the expansion of Medicare coverage for CRC screening tests, racial/ethnic differences in CRC screening persisted over time in this universally-insured population, especially for blacks and Hispanics. Future studies should explore other factors beyond health insurance that may contribute to screening disparities in this and younger populations.
IMPACT
Although CRC screening rates increased over time, they were still low according to recommendations. More effort is needed to increase CRC screening among all Medicare beneficiaries.
Keywords: colorectal cancer, cancer screening, disparity, race/ethnicity, Medicare
INTRODUCTION
Colorectal cancer (CRC) is the third most commonly diagnosed non-skin cancer in both men and women in the United States, with an estimated 142,570 new cases in 2010 (1). Because colorectal carcinogenesis involves a long-term process, there are opportunities for prevention (2). Screening reduces mortality by decreasing incidence due to the removal of pre-cancerous polyps and by detecting CRC at an early stage when the disease is amenable to treatment (3). Screening guidelines have been developed by a number of national organizations to target people 50 years and older who are at average risk for CRC (4, 5).
Despite national CRC screening recommendations and evidence for prevention and early detection of CRC, screening rates remain suboptimal. In 2005, only 50.0 % of adults aged ≥ 50 years reported having received a fecal occult blood test (FOBT) within the past year and/or endoscopy (flexible sigmoidoscopy or colonoscopy) within the past 10 years (6). Furthermore, several studies have also documented differences in CRC screening among racial/ethnic groups; most studies found that CRC screening rates are lower among racial/ethnic minorities (7–9). Although these disparities are often attributed to variation in health insurance coverage (10), they also exist among universally-insured Medicare beneficiaries (8–12).
In 1998, Medicare began covering annual FOBT for beneficiaries at average risk for CRC. At the same time, sigmoidoscopy coverage also expanded to every 4 years for beneficiaries 50 years of age and older at average risk (13). Colonoscopy has been covered since 1998 for high-risk individuals, but as of July 1, 2001, coverage was expanded to include average-risk individuals every 10 years (13).
It is unclear whether the expansion of CRC screening test reimbursement has ameliorated or eliminated racial/ethnic disparities in CRC screening in the Medicare population. Therefore, in this study, we examined the effect of Medicare’s expanding coverage of CRC screening tests on racial/ethnic disparities in CRC screening among non-Hispanic white (hereafter white), non-Hispanic black (hereafter black), Asian/Pacific Islander (hereafter Asian) and Hispanic cancer-free Medicare beneficiaries residing in the 16 Surveillance, Epidemiology and End Results (SEER) areas. Results of this study not only will allow us to better understand the impact of Medicare coverage of CRC screening on racial/ethnic disparities, but also will inform our progress towards meeting the following Healthy People 2020 goals and objectives: eliminate health disparities, reduce the number of deaths from CRC and increase the proportion of adults who receive a CRC screening examination(14).
METHODS
Data Sources
Medicare is a federally funded program that provides health insurance primarily for those 65 years of age and older (13). Medicare represents about 97% of the U.S. elderly (15). Since 1991, Medicare claims became available for a 5% random sample of Medicare beneficiaries residing in the SEER areas who do not have cancer (13). This 5% random sample of Medicare database from the 16 SEER areas was the data source for this study. The SEER Program, maintained by the National Cancer Institute, collects demographic, tumor characteristics, and other information for persons with cancer (13). This study included 16 selected geographic areas: San Francisco/Oakland, Detroit, Seattle, Atlanta, Rural Georgia, Los Angeles county, the San Jose-Monterey area, and the rest of California; and the states of Connecticut, Iowa, New Mexico, Utah, Hawaii, Kentucky, Louisiana and New Jersey. The four registries from Kentucky, Louisiana, New Jersey, and greater California became available in 2000, thus increasing the coverage from 14% in 1992-1999 to 25% of the U.S. population in 2000-2002 (15). CRC screening procedures were identified in Medicare claims.
Study Population
The study population consisted of 30,893 Medicare beneficiaries without any cancer, aged 70 to 89 years, continuously enrolled in both Medicare Parts A and B, with no health maintenance organization (HMO) coverage. These beneficiaries were from the 5% random sample of Medicare beneficiaries residing in SEER catchment areas and indexed into Medicare between January 1, 1996 and December 31, 2005. This random sample was broken equally into 11 cohorts in each of the 11 years (index year) between 1996 and 2005. Of these subjects, 88.3% were White, 7.4% were Black, and 4.3% were either Asian or Hispanic.
In this study, a minimum age of 70 years old was used to allow at least 5 years of enrollment in Medicare prior to the eligibility age of 65, so that CRC test use could be assessed according to screening guidelines. There is no consensus on when to stop CRC screening and so a maximum age of 89 years was chosen to ensure a sufficient sample size.
Study Variables
The primary outcome in this study was the proportion of persons receiving CRC screening according to the guidelines by Medicare coverage time period. These time periods included: before FOBT coverage (prior to 1998), during FOBT coverage only (1998-2000), and after colonoscopy coverage (2001+). These coverage periods were defined by index year, which allowed sufficient lead time for the adoption of the screening procedure once Medicare reimbursement went into effect. Also, because it is difficult to distinguish screening from diagnostic tests, including only screening codes could result in a significant undercount of screening rates; therefore, no effort was made to differentiate these tests (16). However, because these subjects were cross-linked with the SEER cancer registry data by the NCI to verify no history of any tumor, these screening codes were likely for CRC screening rather than for diagnosis.
The Current Procedural Terminology (CPT) (17), Healthcare Common Procedural Coding System (HCPCS) (18), and ICD-9-CM procedure codes (19) for CRC screening tests were identified in claims from physician encounters (Carrier Claims file); hospital outpatient encounters (Outpatient file); and inpatient episodes (Medicare Provider Analysis and Review file). FOBTs were identified by the CPT codes 82270-82273 and HCPCS code G0107. Colonoscopies were ascertained using CPT codes of 44388-44389, 44390-44394, 45355, 45378-45380, 45382-45385; HCPCS codes G0105 and G0121; and ICD-9-CM procedure codes 45.23, 45.25, 45.41-45.43, and 48.36. Sigmoidoscopies were classified using CPT codes 45305, 45308-45309, 45315, 45320, 45330-45339; HCPCS code G0104; and ICD-9-CM procedure codes 45.22, 45.24, 48.22, and 48.24 (13). After these codes were identified, a dichotomous variable indicating receipt of a screening procedure within guidelines (i.e., annual FOBT, sigmoidoscopy every 5 years or colonoscopy every 10 years) or not (yes/no) was created (5).
Socio-demographic Characteristics
The following socio-demographic characteristics were available in the database: age (categorized as 70-74, 75-79, 80-84, or 85-89), sex (male or female), marital status (married, unmarried or unknown), geographic areas (16 SEER regions), index year (1996 to 2005), rural residence (big metropolitan, metropolitan, urban, less urban/rural), and median household income in zip code (in quartiles).
Statistical analysis
Socio-demographic variables were summarized using descriptive statistics by race/ethnicity. Differences by race/ethnicity for each characteristic were assessed using the chi-square statistic. P-values less than or equal to 0.05 were deemed statistically significant. CRC screening was evaluated by calculating the crude and age-gender-adjusted percentages of persons who were guideline-adherent (i.e., completion of any CRC test within the recommended time interval: annual FOBT, sigmoidoscopy every 5 years and colonoscopy every 10 years) by race/ethnicity and Medicare coverage time period (i.e., before fecal occult blood test (FOBT) coverage, during FOBT coverage only, and after colonoscopy coverage). The following age categories were used to adjust CRC screening rates for each sex: 1) 70-74, 2) 75-79, 3) 80-84 and 4) 85-89. Using multivariable logistic regression, the effect of race/ethnicity on the odds of receiving guideline-specific CRC screening was estimated by Medicare coverage period. All data were analyzed using the SAS system (version 9.13, Cary, NC) and the statistical software package Intercooled Stata version 10 (Stata Corporation College Station, TX).
RESULTS
There were statistically significant differences for all socio-demographic characteristics by race/ethnicity (Table 1). However, most striking were the substantial racial/ethnic differences in the socioeconomic variables available in this study. Almost 56% of Blacks resided in zip codes with the lowest median household income compared to 21.4% of whites. Furthermore, a larger proportion of black (67.4%) and other ethnic (64.4%) Medicare beneficiaries resided in urban areas relative to whites (54.2%).
Table 1.
Socio-demographic characteristics of Medicare beneficiaries without a previous cancer diagnosis, by race/ethnicity (percent)
| White (n=27,276) |
Black (n=2,278) |
Other* (n=1,339) |
||||
|---|---|---|---|---|---|---|
| Characteristicˆ | N | % | n | % | n | % |
| Age (years) | ||||||
| 70-74 | 7,190 | 26.4 | 716 | 31.4 | 482 | 36.0 |
| 75-79 | 8,405 | 30.8 | 698 | 30.6 | 400 | 29.9 |
| 80-84 | 7,559 | 27.9 | 565 | 24.8 | 312 | 23.3 |
| 85-89 | 4,082 | 15.0 | 299 | 13.1 | 145 | 10.8 |
| Sex | ||||||
| Male | 10,152 | 37.2 | 785 | 34.5 | 585 | 43.7 |
| Female | 17,124 | 62.8 | 1,493 | 65.5 | 754 | 56.3 |
| Median household income in zip code | ||||||
| First quartile, highest | 6,993 | 25.6 | 171 | 7.5 | 268 | 20.0 |
| Second quartile | 6,835 | 25.1 | 262 | 11.5 | 328 | 24.5 |
| Third quartile | 6,607 | 24.2 | 498 | 21.9 | 334 | 24.9 |
| Fourth quartile, lowest | 5,849 | 21.4 | 1,267 | 55.6 | 318 | 23.7 |
| Unknown | 992 | 3.6 | 80 | 3.5 | 91 | 6.8 |
| SEER Registry Area of Residence | ||||||
| California | 7,734 | 28.4 | 479 | 21.0 | 879 | 65.6 |
| Connecticut | 2,096 | 7.7 | 88 | 3.9 | 40 | 3.0 |
| Detroit | 2,174 | 8.0 | 451 | 19.8 | 16 | 1.2 |
| Hawaii | 119 | 0.4 | <11 | <1.0 | 167 | 12.5 |
| Iowa | 2,208 | 8.1 | 26 | 1.1 | <11 | <1.0 |
| New Mexico | 704 | 2.6 | 17 | 0.8 | 83 | 6.2 |
| Seattle-Puget Sound | 1,587 | 5.8 | 34 | 1.5 | 31 | 2.3 |
| Utah | 874 | 3.2 | <11 | <1.0 | <11 | <1.0 |
| Atlanta/Rural Georgia | 892 | 3.3 | 226 | 9.9 | <11 | <1.0 |
| Kentucky | 2,670 | 9.8 | 132 | 5.8 | <11 | <1.0 |
| Louisiana | 1,614 | 5.9 | 473 | 20.8 | 13 | 1.0 |
| New Jersey | 4,604 | 16.9 | 346 | 15.2 | 85 | 6.3 |
| Urban/Rural Residence | ||||||
| Big metropolitan | 14,795 | 54.2 | 1,536 | 67.4 | 862 | 64.4 |
| Metropolitan | 7,640 | 28.0 | 471 | 20.7 | 364 | 27.2 |
| Urban | 1,779 | 6.5 | 92 | 4.0 | 71 | 5.3 |
| Less urban/Rural | 3,062 | 11.2 | 179 | 7.9 | 42 | 3.1 |
| Index Year | ||||||
| 1996 | 3,054 | 11.2 | 262 | 11.5 | 140 | 10.5 |
| 1997 | 3,101 | 11.4 | 279 | 12.3 | 128 | 9.6 |
| 1998 | 3,047 | 11.2 | 259 | 11.4 | 141 | 10.5 |
| 1999 | 3,260 | 12.0 | 261 | 11.5 | 143 | 10.7 |
| 2000 | 3,243 | 11.9 | 283 | 12.4 | 159 | 11.9 |
| 2001 | 3,043 | 11.2 | 257 | 11.3 | 158 | 11.8 |
| 2002 | 2,817 | 10.3 | 231 | 10.1 | 138 | 10.3 |
| 2003 | 2,519 | 9.2 | 185 | 8.1 | 151 | 11.3 |
| 2004 | 1,903 | 7.0 | 168 | 7.4 | 104 | 7.8 |
| 2005 | 1,289 | 4.7 | 93 | 4.1 | 77 | 5.8 |
All chi-square tests for the distribution of demographic and clinical characteristics among these 4 racial/ethnic groups were statistically significant (P <.05).
Other includes Hispanics and Asian/Pacific Islanders.
Categories with cases less than 11 were suppressed as required by the data user agreement at the time of review by the SEER-Medicare office.
Trends in CRC Screening
The age-gender-adjusted percentages of persons who received guideline-specific CRC screening increased for whites and blacks as Medicare coverage expanded to average-risk individuals (Figure 1). Across all Medicare coverage periods, white beneficiaries were more likely to receive guideline-specific CRC screening than blacks and Hispanics. Except for the pre-FOBT period, whites were more likely to receive CRC screening than Asians.
Figure 1.
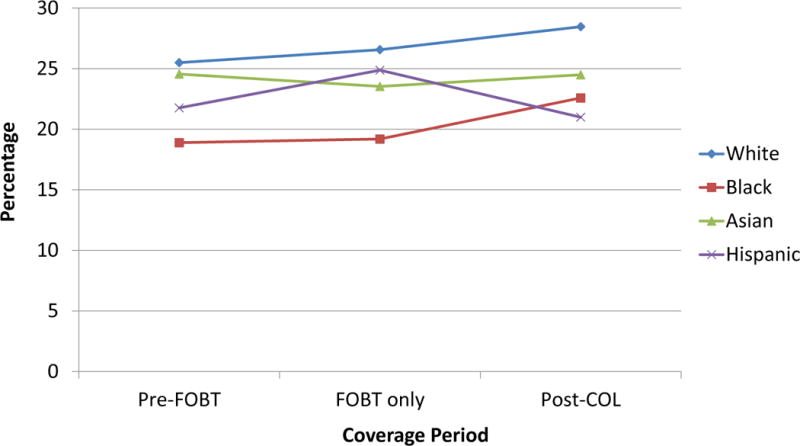
Age-gender-adjusted percentage of persons receiving an endoscopy within 5 years and/or home fecal occult blood test within previous year, by race/ethnicity and Medicare colorectal cancer screening test coverage period
FOBT = fecal occult blood test; COL = colonoscopy
Odds of CRC Screening
Prior to FOBT coverage, compared to whites, Blacks were less likely (OR: 0.74; 95% CI: 0.61-0.90) to receive guideline-specific screening (Table 2) after adjusting for covariates. Subsequently, these odds decreased to 0.66 (95% CI: 0.52-0.83) in FOBT only coverage, then increased to 0.80 (95% CI: 0.68-0.95) following colonoscopy coverage. Also, Hispanics were less likely than Whites to receive CRC screening in the colonoscopy coverage period after adjusting for covariates (OR=0.73, 95% CI: 0.54-0.99). There were no statistically significant differences in CRC screening between whites and Asians/Pacific Islanders.
Table 2.
Association between receiving an endoscopy within 5 years and/or home fecal occult blood test within previous year and Medicare coverage period for Medicare beneficiaries without a previous cancer diagnosis, by race/ethnicity
| Pre-FOBT Odds ratio* (95% CI) |
FOBT only Odds ratio* (95% CI) |
Post-colonoscopy Odds ratio* (95% CI) |
|
|---|---|---|---|
| Non-Hispanic White | 1.0 Ref | 1.0 Ref | 1.0 Ref |
| Non-Hispanic Black | 0.74 (0.61-0.90) | 0.66 (0.52-0.83) | 0.80 (0.68-0.95) |
| Asian/Pacific Islander | 0.90 (0.65-1.24) | 0.84 (0.57-1.25) | 0.77 (0.59-1.00) |
| Hispanic | 0.91 (0.63-1.32) | 0.91 (0.61-1.35) | 0.73 (0.54-0.99) |
Odds ratios are adjusted for age, sex, SES (median household income at zip code level), urban/rural residence and SEER registry.
Statistically significant (p<0.05) odds ratios denoted in bold.
DISCUSSION
Racial disparities in CRC screening persisted, despite the expansion of Medicare CRC screening test reimbursement for average-risk persons. Specifically, overall CRC screening increased for all racial/ethnic groups but disparities persisted for black and Hispanic Medicare beneficiaries. These findings are similar to previous studies that examined the impact of this policy change on racial disparities in CRC screening and found that there has been an increase in CRC screening over time, but racial disparities persisted (9, 20). To our knowledge, this study is the first to use Medicare claims data among beneficiaries without a history of cancer to examine the impact of this change in Medicare policy on racial/ethnic disparities in guideline-specific CRC screening from the period prior to FOBT coverage to after colonoscopy coverage.
These disparities should not exist within this universally-insured population. Possible explanations for these persistent racial/ethnic differences are substantial variations in SES, health beliefs and health education, and healthcare access, which are important determinants of screening within the Medicare population (12, 21). We were not able to control for differences in SES at the individual level because the individual SES variable was not available in Medicare data; therefore, there may have been some residual confounding of SES because zip codes include more heterogeneous populations than census tracts. In addition to SES, the differences observed may be explained by language and cultural barriers, such as cancer fatalism (22, 23).
Although there were racial/ethnic disparities in CRC screening, the analysis of the age-gender-adjusted percentage of persons revealed that utilization was higher after post-colonoscopy coverage for average-risk persons (from 2001) than pre-FOBT coverage (before 1998) for all racial/ethnic groups. Moreover, after adjusting for covariates, there were no statistically significant racial/ethnic disparities in CRC screening between Whites and Asians for any time period, and no statistically significant differences between Whites and Hispanics for pre-FOBT and FOBT only coverage periods. If these trends continue, we may attain the Healthy People 2020 goals and objectives of increasing CRC screening, reducing cancer deaths and eliminating racial disparities for some racial/ethnic groups (14).
There were several limitations of this study. Foremost, CRC screening may have been underestimated due to 4 issues. First, the validity of the Medicare Enrollment Database’s race and ethnicity classifications are less accurate for some ethnic groups. One study in which the Medicare Enrollment Database race variable was compared against a survey of beneficiaries, determined that sensitivity was poor for Asians and Hispanics (24). However, another study found that the positive predictive values for Asians (75.3%) and Hispanics (97.7%) were sufficient to allow meaningful comparison of procedure use with Whites (25). Therefore, the degree to which this potential misclassification of Asian and Hispanic ethnicity may have led to the undercounting of CRC screening among these groups is unclear. In an attempt to improve accuracy of the race/ethnicity codes, particularly for non-black minority groups, the Centers for Medicare and Medicaid Services (CMS) reclassified race/ethnicity using social security information in 1994 and self-reports from Medicare enrollees in 1997 (24). This led to improvements for non-black minorities from 1996 to 1997 (24). However, it remains unclear whether or how the trends in CRC screening during this timeframe for Hispanics and Asians may have been affected. A second potential limitation is that if a polypectomy or biopsy was performed during a colonoscopy, the procedure would have been given a polypectomy or biopsy code rather than a screening colonoscopy code, leading to the underestimation of colonoscopies. A third limitation is that colonoscopy screening is recommended every 10 years, and we were only able to examine colonoscopy use for the 2001-2005 cases. Thus, our study time period may have been too short to fully assess this screening modality. Furthermore, since Medicare did not provide coverage for average-risk individuals until 1998 for FOBT and sigmoidoscopy and 2001 for colonoscopy (13), there may be some undercounting of screening in the years prior to these coverage periods; therefore, during the non-coverage periods, our findings are more likely to be representative of CRC screening among high-risk Medicare beneficiaries (e.g., those with genetic susceptibility to CRC) and, at the same time, under-represent those who were at average risk for CRC. Although each of these circumstances may have led to underestimation of screening colonoscopy, it is unlikely that the latter three issues differentially impacted screening rates among ethnic groups. CRC screening may have also been overestimated in this study. A colonoscopy could be done for other purposes other than CRC screening (e.g., Crohn’s disease) and these may have been unknowingly included in our analysis. Furthermore, no effort was made to distinguish screening from diagnostic CRC tests, because of difficulty differentiating the reason for those tests in claims data (13). This potential bias was minimized by cross-linking the sample of Medicare beneficiaries with the SEER cancer registry data to confirm that no one had a history of any type of cancer; however, even if a cancer was not reported in SEER, there may still be a possibility that a colonoscopy could have been performed for a diagnostic purpose. Also, using index year allowed some lead time for the adoption of the screening procedures; therefore, there could have been a certain degree of misclassification of CRC screening for some beneficiaries. Finally, this study is limited by the SES measures that were available in the dataset. Median household income at the zip code level was used as a measure of SES but it may not be an ideal indicator for the elderly (26, 27). Moreover, individual-level SES or other components of SES such as education were not available in the data set and may have played an important role in CRC screening (23, 28).
There were also a number of strengths. First, our study population included a 5% random sample of Medicare beneficiaries from the 16 SEER areas. The age and sex distribution in SEER areas is comparable to that of the U.S. elderly population (15); however, SEER areas are more affluent, more urban, have lower unemployment (29) and a higher proportion of minorities (15) than non-SEER areas. Therefore, our findings are generalizable to persons 65 years and older who reside in SEER areas and may also provide good estimates for elderly populations outside of these areas. In addition, using a Medicare population allowed us to examine disparities in a population where lack of health insurance, a known barrier to CRC screening, was eliminated (30–33). Thus, our finding that racial/ethnic disparities existed among these universally-insured Medicare beneficiaries suggests that barriers other than access need to be identified and addressed to reduce disparities to CRC screening. Finally, relative to national surveys, the Medicare data provides a much less expensive alternative to ascertaining and monitoring screening change over time.
In conclusion, racial/ethnic differences in CRC screening persisted, regardless of the expansion in Medicare coverage of CRC screening. Future studies should explore other factors beyond health insurance that may contribute to screening disparities such as physician recommendation and language/cultural barriers in this and younger populations.
Acknowledgments
Grant support: This study was supported by a grant from the AHRQ (R01-HS016743). Arica White was the recipient of a pre-doctoral fellowship under a NCI training grant (R25-CA057712).
References
- 1.American Cancer Society. Cancer Facts and Figures 2009. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- 2.Peipins LA, Sandler RS. Epidemiology of colorectal adenomas. Epidemiologic reviews. 1994;16:273–97. doi: 10.1093/oxfordjournals.epirev.a036154. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society. Cancer Facts and Figures 2008. Atlanta, GA: American Cancer Society; 2008. [Google Scholar]
- 4.U.S. Preventive Services Task Force. Screening for colorectal cancer: recommendation and rationale. Annals of internal medicine. 2002;137:129–31. doi: 10.7326/0003-4819-137-2-200207160-00014. [DOI] [PubMed] [Google Scholar]
- 5.Smith RA, von Eschenbach AC, Wender R, et al. American Cancer Society guidelines for the early detection of cancer: update of early detection guidelines for prostate, colorectal, and endometrial cancers. Also: update 2001–testing for early lung cancer detection. CA: a cancer journal for clinicians. 2001;51:38–75. doi: 10.3322/canjclin.51.1.38. quiz 7-80. [DOI] [PubMed] [Google Scholar]
- 6.Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008;17:1623–30. doi: 10.1158/1055-9965.EPI-07-2838. [DOI] [PubMed] [Google Scholar]
- 7.Cooper GS, Koroukian SM. Racial disparities in the use of and indications for colorectal procedures in Medicare beneficiaries. Cancer. 2004;100:418–24. doi: 10.1002/cncr.20014. [DOI] [PubMed] [Google Scholar]
- 8.Fenton JJ, Tancredi DJ, Green P, Franks P, Baldwin LM. Persistent racial and ethnic disparities in up-to-date colorectal cancer testing in medicare enrollees. Journal of the American Geriatrics Society. 2009;57:412–8. doi: 10.1111/j.1532-5415.2008.02143.x. [DOI] [PubMed] [Google Scholar]
- 9.Doubeni CA, Laiyemo AO, Klabunde CN, Young AC, Field TS, Fletcher RH. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. American journal of preventive medicine. 2010;38:184–91. doi: 10.1016/j.amepre.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ioannou GN, Chapko MK, Dominitz JA. Predictors of colorectal cancer screening participation in the United States. Am J Gastroenterol. 2003;98:2082–91. doi: 10.1111/j.1572-0241.2003.07574.x. [DOI] [PubMed] [Google Scholar]
- 11.Fenton JJ, Cai Y, Green P, Beckett LA, Franks P, Baldwin LM. Trends in colorectal cancer testing among medicare subpopulations. American journal of preventive medicine. 2008;35:194–202. doi: 10.1016/j.amepre.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 12.O’Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage: gaps in colorectal cancer screening among Medicare beneficiaries. Archives of internal medicine. 2005;165:2129–35. doi: 10.1001/archinte.165.18.2129. [DOI] [PubMed] [Google Scholar]
- 13.National Cancer Institute. SEER-Medicare. 2009 [cited February 1, 2009]; Available from: http://healthservices.cancer.gov/seermedicare.
- 14.US Department of Health and Human Services. Healthy People 2020. [cited 2011 January 7]; Available from: http://healthypeople.gov/2020/topicsobjectives2020/default.aspx.
- 15.Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Medical care. 2002;40:IV-3-18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 16.Schenck AP, Klabunde CN, Warren JL, et al. Data sources for measuring colorectal endoscopy use among Medicare enrollees. Cancer Epidemiol Biomarkers Prev. 2007;16:2118–27. doi: 10.1158/1055-9965.EPI-07-0123. [DOI] [PubMed] [Google Scholar]
- 17.American Medical Association. Physicians’ Current Procedural Terminology-CPT 2000. Chicago, IL: American Medical Association; 2000. [Google Scholar]
- 18.Health Care Financing Administration. HCFA Common Procedure Coding System (HCPCS): National Level II Medicare Codes. Los Angeles, CA: Practice Management Information Corporation; 2000. [Google Scholar]
- 19.U.S. Public Health Services. International Classification of Diseases, 9th Revision, Clinical Modification. 5th. Los Angeles, CA: Practice Management Information Corporation; 1996. [Google Scholar]
- 20.Shih YC, Zhao L, Elting LS. Does Medicare coverage of colonoscopy reduce racial/ethnic disparities in cancer screening among the elderly? Health Aff (Millwood) 2006;25:1153–62. doi: 10.1377/hlthaff.25.4.1153. [DOI] [PubMed] [Google Scholar]
- 21.Ananthakrishnan AN, Schellhase KG, Sparapani RA, Laud PW, Neuner JM. Disparities in colon cancer screening in the Medicare population. Archives of internal medicine. 2007;167:258–64. doi: 10.1001/archinte.167.3.258. [DOI] [PubMed] [Google Scholar]
- 22.Jerant AF, Arellanes RE, Franks P. Factors associated with Hispanic/non-Hispanic white colorectal cancer screening disparities. J Gen Intern Med. 2008;23:1241–5. doi: 10.1007/s11606-008-0666-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jerant AF, Fenton JJ, Franks P. Determinants of racial/ethnic colorectal cancer screening disparities. Archives of internal medicine. 2008;168:1317–24. doi: 10.1001/archinte.168.12.1317. [DOI] [PubMed] [Google Scholar]
- 24.Arday SL, Arday DR, Monroe S, Zhang J. HCFA’s racial and ethnic data: current accuracy and recent improvements. Health care financing review. 2000;21:107–16. [PMC free article] [PubMed] [Google Scholar]
- 25.Escarce JJ, McGuire TG. Methods for using Medicare data to compare procedure rates among Asians, blacks, Hispanics, Native Americans, and whites. Health services research. 2003;38:1303–17. doi: 10.1111/1475-6773.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Du XL, Fang S, Coker AL, et al. Racial disparity and socioeconomic status in association with survival in older men with local/regional stage prostate carcinoma: findings from a large community-based cohort. Cancer. 2006;106:1276–85. doi: 10.1002/cncr.21732. [DOI] [PubMed] [Google Scholar]
- 27.Smith JP, Kington RS. Race, Socioeconomic Status, and Health Late in Life. In: Soldo LGMaB., editor. Racial and Ethnic Differences in the Health of Older Americans. Washington, D.C.: National Academy Press; 1997. [Google Scholar]
- 28.Shokar NK, Carlson CA, Weller SC. Factors associated with racial/ethnic differences in colorectal cancer screening. J Am Board Fam Med. 2008;21:414–26. doi: 10.3122/jabfm.2008.05.070266. [DOI] [PubMed] [Google Scholar]
- 29.Nattinger AB. Generalizability of the Surveillance, Epidemiology and End Results Registry population: Factors relevant to epidemiologic and health care research. Journal of clinical epidemiology. 1997;50:939–45. doi: 10.1016/s0895-4356(97)00099-1. [DOI] [PubMed] [Google Scholar]
- 30.Adams EK, Thorpe KE, Becker ER, Joski PJ, Flome J. Colorectal cancer screening, 1997-1999: role of income, insurance and policy. Preventive medicine. 2004;38:551–7. doi: 10.1016/j.ypmed.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 31.Cairns CP, Viswanath K. Communication and colorectal cancer screening among the uninsured: data from the Health Information National Trends Survey (United States) Cancer Causes Control. 2006;17:1115–25. doi: 10.1007/s10552-006-0046-2. [DOI] [PubMed] [Google Scholar]
- 32.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 33.Etzioni DA, Ponce NA, Babey SH, et al. A population-based study of colorectal cancer test use: results from the 2001 California Health Interview Survey. Cancer. 2004;101:2523–32. doi: 10.1002/cncr.20692. [DOI] [PubMed] [Google Scholar]


