Abstract
BACKGROUND: Socioeconomic deprivation, obesity, and emotional discomfort are important determinants of health inequalities and poor glycemic control in children and young people with type 1 diabetes mellitus (T1D). OBJECTIVES: The aims of this study were to evaluate the incidence of hospital admissions of T1D children in relation to socioeconomic deprivation, and to determine the effects of social deprivation, body mass index (BMI), and patient-reported emotional well-being on glycemic control. METHODS: All hospital admissions of T1D patients aged 1-18 years were identified during 2007 and 2012. Admission cause and glycemic control were related to social deprivation, BMI, and psychological, emotional well-being. Indices of Multiple Deprivation (IMD) 2010 were applied to the United Kingdom data. The associations were calculated using the Spearman's rank correlation coefficient. RESULTS: A significant correlation was found between hospital admission rates and overall deprivation scores (r = -0.18, p = 0.04). Patients living in deprived areas were more likely to selfpresent to the accident and emergency department (r = -0.24, p = 0.02). Poor glycemic control (n = 124) was significantly associated with lower levels of education (r = -0.22, p = 0.02) and unemployment (r = -0.19, p = 0.04). Significance was not reached for level of income (r = -0.16, p = 0.07) and overall deprivation (r = -0.17, p = 0.06). Glycemic control was not found to be associated with BMI, standard deviation scores (SDS), or emotional well-being. CONCLUSION: Early intervention and education from primary care and specialist diabetes teams within the community in deprived areas may be effective in reducing hospital admissions for diabetes-related problems and improving glycemic control.
Keywords: type 1 diabetes mellitus, social deprivation, hospital admission, glycemic control
Abbreviations: AE - accident and emergency; BMI - body mass index; CYP - children and young people; DKA - diabetic ketoacidosis; HbA1c - glycosylated hemoglobin; HES - hospital episodes statistics; IMD - indices of multiple deprivation; NHS - National Health Service; NICE - National Institute for Health and Care Excellence; NPDA - National Paediatrics Diabetes Audit; SDS - standard deviation score; SPSS - Statistical Package for the Social Sciences; T1D - type 1 diabetes mellitus; UK - United Kingdom; WHO-5 - World Health Organization 5 Well-Being Index
1. Introduction
Type 1 diabetes mellitus (T1D) is a chronic, autoimmune, endocrine condition which results in too little or no insulin being produced by the pancreatic beta-cells. With poor glycemic control, chronic hyperglycemia may occur, and long-standing deranged glycemia leads to vascular complications [1, 2].
The United Kingdom (UK) has the fifth largest population of children and young people (CYP) with T1D. However, despite a wide range of national initiatives and guidelines aimed at improving diabetes services and outcomes, management and control of T1D in CYP remains amongst the poorest in Europe [3]. The recent National Paediatrics Diabetes Audit (NPDA) 2014-15 showed that the majority of CYP in the UK continue to have poor glycemic control, and the incidence of hospital admissions for diabetic ketoacidosis (DKA) has increased. The findings of the UK national pediatric diabetes audit highlighted significant variations in health outcomes geographically within the UK, despite the introduction of best practice tariff for pediatric diabetes along with the National Paediatric Diabetes Service Improvement Delivery Plan [4]. It has been shown that within the UK, the prevalence of T1D is increasing during childhood at a rate of 3-4% per year [1, 5, 6]. In 2014, diabetes cost the National Health Service (NHS) nearly £10 billion, which equate to £1 million every hour. At that time, this amount was almost 10% of the annual NHS budget [7]. An HbA1c value of less than 6.5% or less than 48 mmol/mol has been recommended by National Institute for Health and Care Excellence (NICE) guidance NG18 for good control and to reduce the risk of morbidity and mortality in T1D patients [6, 8].
The association between social deprivation and general health has been described previously in the adult population; however, this has mainly concerned type 2 diabetes [9]. It has also been noted that an "inverse care law" [9] does exist for patients with diabetes. It highlights that patients who require the most care and support for their condition, i.e. those living in more deprived areas, are less likely to receive it [9]. Therefore, it is important for us to look into why this association between poor diabetes outcomes and deprivation is present, and how we can improve this social gradient [9].
The aim of this study was to examine the relationship between the incidence of hospital admissions for children with T1D and their socioeconomic deprivation. It compares diabetes-related admissions with non-diabetes related admissions and the trend of HbA1c prior to hospitalization. The study also aims to evaluate the effect of social deprivation, body mass index (BMI), and patientreported emotional well-being on glycemic control in children and young people with T1D.
2. Methods
2.1 Hospital admissions
All hospital admissions of patients with T1D aged 0-18 years (n = 135) within a large-district general hospital were identified during a five-year period between 2007 and 2012 using the hospital episodes statistics (HES) database. The hospital is the principal healthcare provider to 300,000 people across Southport, Formby, and West Lancashire which have a diverse population. Each hospital admission was classified as either an accident and emergency (AE) admission or inpatient ward admission. Causes of admissions were evaluated from individual hospital medical records.
2.2 Glycemic control
During data collection, 124 patients with T1D aged 1-18 years were recorded. The mean BMI standard deviation scores (SDS) were determined and adjusted for age and sex. The psychological emotional well-being of each patient was measured by using the World Health Organization 5 Well-Being Index (WHO-5) [10]. For all admissions, the average HbA1c during the six months prior to the patients' admissions was obtained.
2.3 Socioeconomic status
The socioeconomic status of the individual patients with T1D was measured using the deprivation data obtained by cross-referencing postcodes with indices of multiple deprivation (IMD) 2010 for overall deprivation scores. The IMD, collected from the Office for National Statistics, calculates area-specific deprivation scores by focusing on seven separate domains [11]:
Income deprivation
Employment deprivation
Health deprivation and disability
Education, skills, and training deprivation
Barriers to housing and services
Crime
Living environment deprivation
Each of the 32,482 small geographic areas (Lower Super Output Areas) in England were ranked from 1 (most deprived) to 32,482 (least deprived).
2.4 Data analysis
The data were analyzed using statistical software, namely the Statistical Package for the Social Sciences (SPSS 20.0, Chicago). Associations between HbA1c (mmol/mol), IMD indices, BMI SDS, WHO-5 well-being index scores, and admissions rates were then determined by the Spearman's rank correlation coefficient.
3. Results
3.1 Hospital admissions
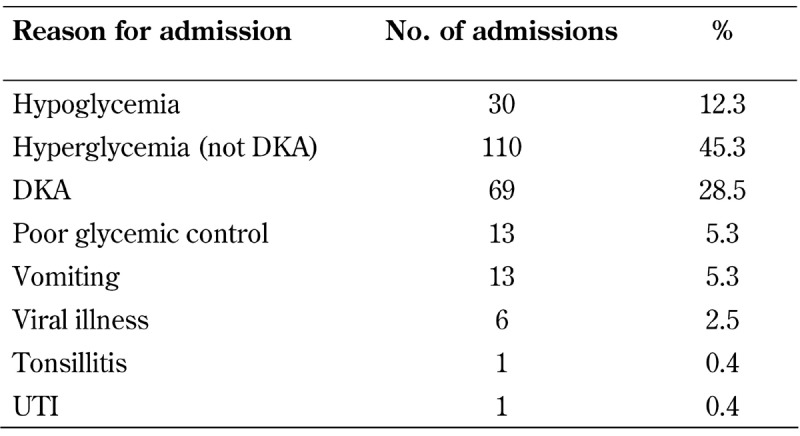
In total, 135 patients were admitted to Ormskirk Hospital between 2007 and 2012. Of these, 66 were female and 69 were male. Table 1 shows the total number of admissions and the reasons why patients attended hospital, including diabetic-related and non-diabetic-related cases.
Table 1. Reasons for admission to hospital including both diabetes-related and non-diabetes-related problems.
We found a significant correlation between hospital admission rates and overall deprivation score (Figure 1). We also found that patients living in deprived areas were more likely to self-present to AE (r = -0.24, p = 0.02). No significant associations were shown between inpatient ward admissions and overall deprivation scores (r = -0.14, p = 0.17).
Figure 1. Association of hospital admissions with overall deprivation.
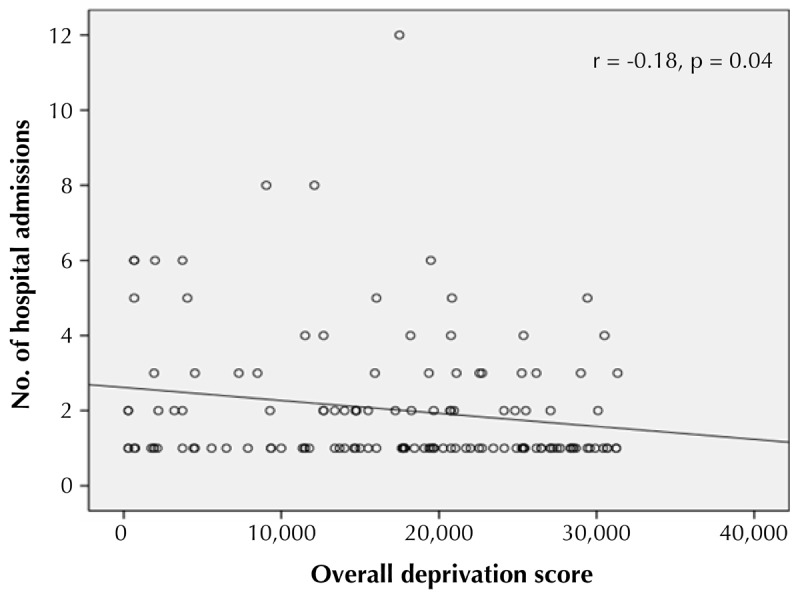
This correlation chart shows the significant association between the number of hospital admissions and overall deprivation (r = -0.18, p = 0.04).
The individual medical records were analyzed, and showed that patients with T1D living in deprived areas were more likely to have a hospital admission for diabetes-related problems (r = -0.50, p = 0.003) (Figure 2). No association was observed between non-diabetes-related hospital admissions with overall deprivation scores (r = -0.1, p = 0.27).
Figure 2. The relationship between the number of admissions and deprivation quintiles.
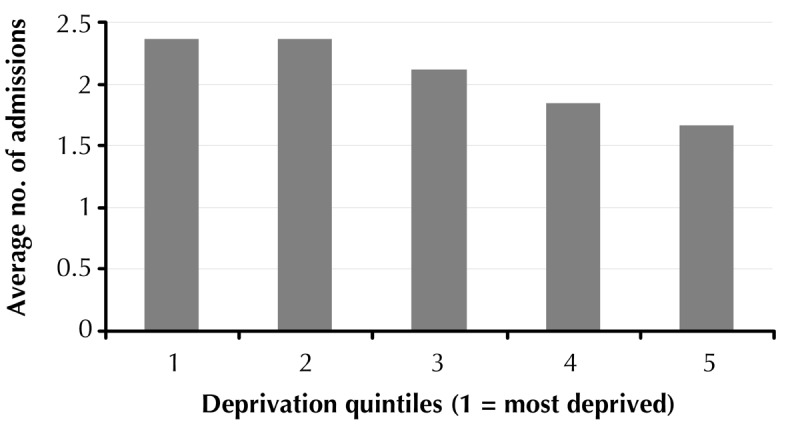
Quintile 1 is the most deprived and quintile 5 the least deprived area. The figure shows that patients with type 1 diabetes who live in a deprived area are more likely to be admitted.
We also looked at the average HbA1c six months prior to each admission (Figure 3). It showed that patients admitted between one to five times during the years 2007-2012 had an average HbA1c of 8.5-9.7% (69-83 mmol/mol). Patients with frequent admissions above five had very poor glycemic control, with average HbA1c >14 % (>119 mmol/mol) during the five-year period.
Figure 3. The relationship between the number of admissions and average HbA1c.
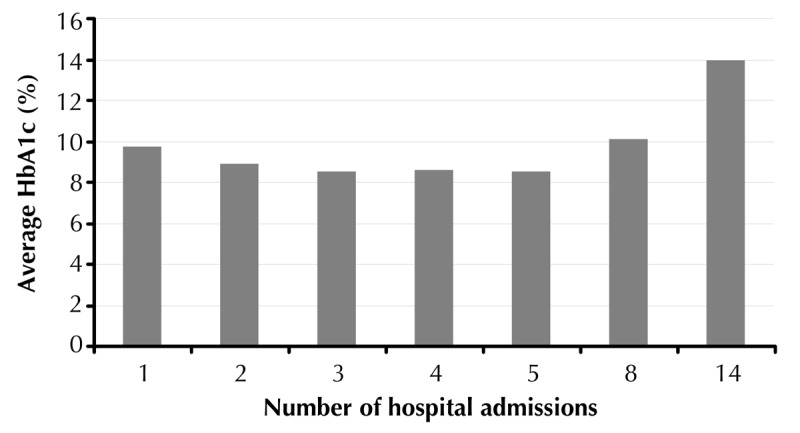
Diabetic patients admitted over five times during the five-year period had poor glycemic control compared to those admitted less than five times.
3.2 Glycemic control
At the time of data collection, there were 124 patients with T1D at our trust. Mean age of diagnosis was 8.2 ± 4.1 years of age (range from 1 to 16 years). The average HbA1c was found to be 68.1 mmol/mol (8.4%), which was higher than the recommended value from the NICE guidance.
Insulin therapy was variable depending on the individual. The number of patients using an insulin pump was increasing all the time. The percentage of patients on an insulin pump was 7% in 2011, 16% in 2012, and 33% in 2013. All other patients, apart from two, were on the twice daily regime.
The results showed that poor glycemic control was significantly associated with lower levels of education (r = -0.22, p = 0.02, Figure 4) and unemployment (r = -0.19, p = 0.04). There was an association between the level of income in the household (r = -0.16, p = 0.07) and overall deprivation (r = -0.17, p = 0.06), although this did not reach significance. Glycemic control was not found to be associated with BMI. SDS, or emotional well-being.
Figure 4. Lower education indices are associated with poor HbA1c control.
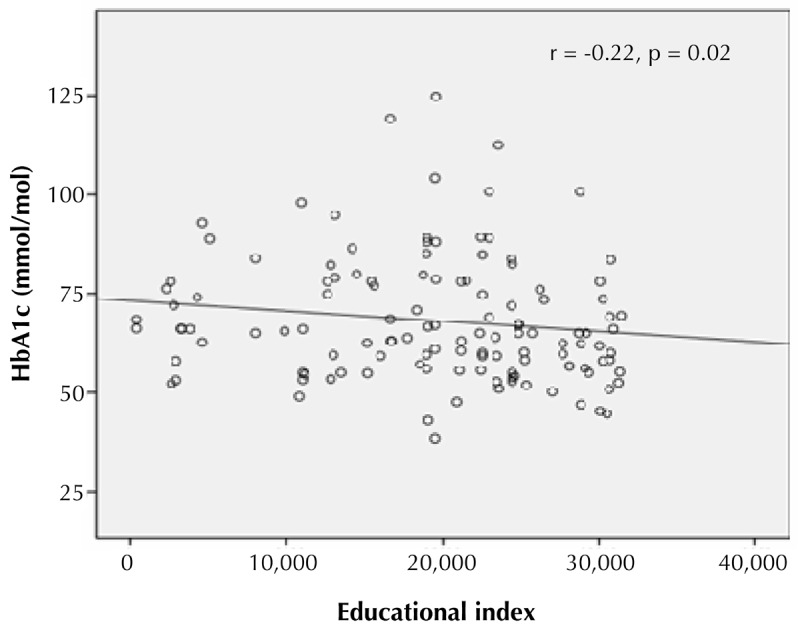
This correlation chart shows that there is a significant associations between lower education status and poor HbA1c control (r = -0.22, p = 0.02).
4. Discussion
Our study showed that glycemic control was significantly poorer in patients living in the most deprived areas of the UK than in those living in the least deprived areas. It also emerged that household levels of education and employment were important determinants in achieving good glycemic control in children and young people with T1D. These findings are consistent with other reports in adult populations that suggest socioeconomic deprivation is associated with poor glycemic control [12-17].
Our results are in agreement with Chen et al. who also found that both education and income levels in the household are important determinants of diabetes control, with low income and/or education levels to be associated with more frequent hospitalization with a preventable diabetes-related problem [18]. A study in the United States showed that poor education and household income increase the risk of diabetes-related mortality by two-fold. These findings emerged after controlling for other potential variables such as age, gender, ethnicity, and BMI [19]. In Israel, Jotkowitz et al. demonstrated that higher numbers of patients with diabetes of all ages, poor glycemic control, and morbidity are more frequent among persons from the most deprived areas [20, 21].
Angus et al. reported that T1D patients had an increased risk of hospitalization, but little evidence was available to explain which factors were causing this [1]. For obvious reasons, it is thought that good HbA1c results will minimize diabetic complications, and thus reduce hospitalization rates [1]. Long-term glycemic control is required to prevent the late vascular complications of diabetes. Community and healthcare professional support such as psychoeducational and behavioral interventions play an important role in diabetes management for patients and their families struggling with the daily management of diabetes [22]. In this study, there was no association between non-diabetes-related hospital admissions and overall deprivation. Interestingly, there were also no associations between overall deprivation and psychological well-being or body mass index in the children.
This report shows that children and young people suffering from T1D are more likely to have a hospital admission for diabetes-related problems if they live in deprived areas. In a systemic review, it was shown that hospital admissions increased in those patients who suffered from unemployment in their household [5]. These findings correspond with our results which show household employment is an important factor for achieving good glycemic control.
Our study also showed that, if improvements in HbA1c levels can be gained, then less diabetes-related admissions to hospital occur. There is a need for practical, cost-effective interventions, which should be applied to the diabetes population within communities that are most deprived, including goal setting, structured education, and psychosocial interventions. An important next step would be to focus on the more deprived areas, especially those affected by poor education or unemployment. Early intervention and education from primary care and specialist diabetes teams within the community in deprived areas may be effective in reducing hospital admissions for diabetes-related problems. Clinicians managing children with diabetes should be aware of the risks associated with poor education and unemployment and incorporate this knowledge into their patient management and psychological counseling. Multidisciplinary teams should ensure that families with poor literacy have an adequate understanding of their children’s diabetes regimen.
Overall, this study shows that in children with T1D, social deprivation is shown to be an important determinant towards poor glycemic control and increased hospital admissions. Further studies may provide evidence for treatment programs to identify high-risk groups and comorbidities. Reduction in hospital admissions would significantly reduce healthcare cost and improve the quality of life of those affected. We believe that efforts should be made to target deprived populations with lower socioeconomic backgrounds, and adapt structured education programs specifically targeted to vulnerable populations when planning health care resources as this will have a significant effect on children and young people with T1D in the future.
5. Conclusions
In this study, poor glycemic control was significantly correlated with increased hospital admissions. Patients with a diabetes-related problem living in deprived areas were more likely to attend the accident and emergency (AE) department. Therefore, efforts should be made to target deprived populations with lower socioeconomic backgrounds, and to adapt educational programs when planning health care resources.
Acknowledgments
Disclosures
The authors reported no conflict of interests.
References
- 1.Angus V, Waugh N. Hospital admission patterns subsequent to diagnosis of type 1 diabetes in children : A systematic review. BMC Health Serv Res. 2007;7:199. doi: 10.1186/1472-6963-7-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clar C, Waugh N, Thomas S. Routine hospital admission versus out-patient or home care in children at diagnosis of type 1 diabetes mellitus (Review) Cochrane Database Syst Rev. 2003;(3):CD004099. doi: 10.1002/14651858.CD004099. [DOI] [PubMed] [Google Scholar]
- 3.Ng S. Improving patient outcomes with technology and social media in paediatric diabetes. BMJ Qual Improv Rep. 2015;4(1):u209396. doi: 10.1136/bmjquality.u209396.w3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Paediatric Diabetes Audit. [Accessed 18.02.2016]. http://www.rcpch.ac.uk/improving-child-health/qualityimprovement-and-clinical-audit/national-paediatricdiabetes-audit-n-02016.
- 5.Sayers A, Thayer D, Harvey J, Luzio S, Atkinson M, French R, Warner J, Dayan C, Wong S, Gregory J. Evidence for a persistent, major excess in all cause admissions to hospital in children with type-1 diabetes: results from a large Welsh national matched community cohort study. BMJ Open. 2015;5(4):E005644. doi: 10.1136/bmjopen-2014-005644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spinks J, Haest J, Ross K, London R, Edge J. Paediatric diabetes services - evidence that expanding the workforce allows intensification of insulin regimens and improves glycaemic control. Arch Dis Child. 2009;94(8):646–647. doi: 10.1136/adc.2009.157891. [DOI] [PubMed] [Google Scholar]
- 7.Challenges for 2015 and beyond. State of the Nation. Diabetes UK; 2015. [Google Scholar]
- 8.National Institute for Health and Care Excellence; 2015. NICE. Diagnosis and management of type 1 diabetes in children, young people and adults. NG18. [Google Scholar]
- 9.Chaturvedi N. Commentary: socioeconomic status and diabetes outcomes; what might we expect and why don't we find out? Int J Epidemiol. 2004;33:871–873. doi: 10.1093/ije/dyh187. [DOI] [PubMed] [Google Scholar]
- 10.WHO (Five) Well-Being Index. WHO Collaborating Centre in Mental Health. WHO; 1998. [Google Scholar]
- 11.Hine S, Senniappan S, Sankart V, Amin R. Deprivation impedes success of insulin intensification in children and adolescents with type 1 diabetes; longitudinal linear mixed modelling of a retrospective observational cohort. Diabet Med. 2011;28(3):338–344. doi: 10.1111/j.1464-5491.2010.03170.x. [DOI] [PubMed] [Google Scholar]
- 12.Thompson R, Agostini K, Potts L, Luscombe J, Christie D, Viner R, White B, Hindmarsh P. Deprivation and ethnicity impact on diabetes control and use of treatment regimen. Diabet Med. 2013;30(4):491–494. doi: 10.1111/dme.12023. [DOI] [PubMed] [Google Scholar]
- 13.Zuijdwijk C, Cuerden M, Mahmud F. Social determinants of health on glycemic control in pediatric type 1 diabetes. J Pediatr. 2013;162(4):730–735. doi: 10.1016/j.jpeds.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 14.Carter P, Cutfield W, Hofman P, Gunn A, Wilson D, Reed P, Jefferies C. Ethnicity and social deprivation independently influence metabolic control in children with type 1 diabetes. Diabetologia. 2008;51(10):1835–1842. doi: 10.1007/s00125-008-1106-9. [DOI] [PubMed] [Google Scholar]
- 15.Hitman G. Ethnicity and social deprivation and its influence on diabetes. Diabet Med. 2013;30(4):385–386. doi: 10.1111/dme.12162. [DOI] [PubMed] [Google Scholar]
- 16.James G, Baker P, Badrick E, Mathur R, Hull S, Robson J. Ethnic and social disparity in glycaemic control in type 2 diabetes; cohort study in general practice 2004-09. J R Soc Med. 2012;105(7):300–308. doi: 10.1258/jrsm.2012.110289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bihan H, Laurent S, Sass C, Nguyen G, Huot C, Moulin J, Guegen R, Le Toumelin P, Le Clesiau H, La Rosa E. et al. Association among individual deprivation, glycemic control, and diabetes complications. Diabetes Care. 2005;28(11):2680–2685. doi: 10.2337/diacare.28.11.2680. [DOI] [PubMed] [Google Scholar]
- 18.Chen P, Tsai C, Woung L, Lee Y. Socioeconomic disparities in preventable hospitalisation among adults with diabetes in Taiwan: a multilevel modelling approach. Int J Equity Health. 2015;14:31. doi: 10.1186/s12939-015-0160-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Savdah S, Lochner K. Socioeconomic status and risk of diabetes-related mortality in the U.S. Public Health Rep. 2010;125(3):377–388. doi: 10.1177/003335491012500306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jotkowitz A, Rabininowitz G, Raskin S, Weitzman R, Epstein L, Porath A. Do patients with diabetes and low socioeconomic status receive less care and have worst outcomes? A national study. Am J Med. 2006;119(8):665–669. doi: 10.1016/j.amjmed.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 21.Dalstra J, Kunst A, Borrell C, Breeze E, Cambois E, Costa G, Geurts J, Lahelma E, Van Oyen H, Rasmussen N. et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005;34:316–326. doi: 10.1093/ije/dyh386. [DOI] [PubMed] [Google Scholar]
- 22.Soni A, Ng S. Intensive diabetes management and goal setting are key aspects of improving metabolic control in children and young people with type 1 diabetes mellitus. World J Diabetes. 2014;5(6):877–881. doi: 10.4239/wjd.v5.i6.877. [DOI] [PMC free article] [PubMed] [Google Scholar]


