Abstract
Objectives:
This study aimed to determine the causal effect of the number of lay counselors removed from a primary care clinic in rural South Africa on the number of clinic-based HIV tests performed.
Design:
Fixed-effects panel analysis.
Methods:
We collected monthly data on the number of lay counselors employed and HIV tests performed at nine primary care clinics in rural KwaZulu-Natal from January 2014 to December 2015. Using clinic- and month-level fixed-effects regressions, we exploited the fact that lay counselors were removed from clinics at two quasi-random time points by a redeployment policy.
Results:
A total of 24,526 HIV tests were conducted over the study period. 21 of 27 lay counselors were removed across the nine clinics in the two redeployment waves. A ten percent reduction in the number of lay counselors was associated with a 4.9% (95% confidence interval [CI]: 2.8 – 7.0, p<0.001) decrease in the number of HIV tests performed. In absolute terms, losing one lay counselor from a clinic was associated with a mean of 29.7 (95% CI: 21.2 – 38.2, p<0.001) fewer HIV tests carried out at the clinic per month.
Conclusions:
This study provides some evidence that lay counselors play an important role in the HIV response in rural South Africa. More broadly, this analysis adds some empirical support to plans to increase the involvement of lay health workers in the HIV response.
Keywords: HIV testing, lay counselors, task shifting, South Africa
Introduction
Sub-Saharan Africa is experiencing an epidemiological transition from acute infectious to chronic non-communicable diseases.[1] Concurrently, HIV is continuing to cause a high disease burden.[2] Partly due to the success of antiretroviral therapy (ART), the number of people living with HIV in SSA has been steadily increasing over the last decade, and is projected to continue doing so over the coming years.[2] This rise in the number of chronic disease patients, particularly as ART eligibility is expanding,[3] is expected to place an increasing stress on health systems in SSA that are already faced with a vast shortage in physicians and nurses.[4]
One promising solution for health systems to successfully manage this projected increase in chronic disease patients is task-shifting to less highly trained health worker cadres. A key cadre for task-shifting in HIV care in many countries in SSA has been facility-based lay counselors.[5] In South Africa, these counselors perform HIV counseling and testing (HCT), enhanced adherence counseling, and support HIV literacy. In addition, lay counselors working at clinics that are supported by non-governmental organizations or research institutions often carry out further tasks, such as point-of-care CD4-cell testing. In the coming years, lay counselors’ role in providing HIV tests is crucial given that the success of the World Health Organization’s “test and treat” strategy will largely hinge on health systems’ ability to identify individuals who are unaware of their HIV status and successfully link them to ART care.[3] Lay counselors may improve HIV testing rates from both the supply- and demand-side of the health system. On the supply-side, they provide HCT services and thus reduce the workload of more highly trained health worker cadres.[6, 7] On the demand-side, lay counselors may increase uptake of HCT services through other pathways, such as reductions in waiting times.[7]
Despite the extensive use of task shifting in SSA,[8] there is little rigorous evidence on the impact of task-shifting on the quantity and quality of care delivered by the health system. In 2015, HIV lay counselors in a high HIV-prevalence region of KwaZulu-Natal, South Africa, were withdrawn in two waves from primary care clinics as part of a redeployment policy that aimed to identify new careers for lay counselors. In this study in nine primary care clinics in rural KwaZulu-Natal, South Africa, we exploit this natural quasi-random variation in the timing of lay counselor removal to estimate the causal impact of the number of lay counselors removed from a clinic on the number of HIV tests performed at the clinic.
Methods
Study setting:
This study took place from January 2014 to December 2015 in the uMlalazi municipality, which is a rural area in KwaZulu-Natal, South Africa. In 2011, uMlalazi’s population was 213,601.[9] KwaZulu-Natal is South Africa’s province that was hardest hit by the HIV epidemic.[10] In uMlalazi, around one quarter of the population aged 15–49 years lived with HIV in 2014, with an estimated overall HIV incidence of 1.2 per 100 person-years.[11]
The municipality’s health services are divided into three areas – Eshowe, Mbongolwane, and Catherine Booth – each with their own district hospital and community health centres. In South Africa, public primary care clinics (which include district hospitals and community health centres), provide nurse-led services such as antenatal care and HIV treatment.[12] The employment of lay cadres, such as facility-based lay counselors, is not standardized in South Africa, and employment practices vary within and across provinces. For the duration of the study period, Médecins sans Frontières’ (MSF) ‘Bending the Curves’ project supported nine primary care clinics in the uMlalazi municipality. This study used data from these nine clinics, which comprised three clinics in the Eshowe and six clinics in the Mbongolwane Health Service Area.
Ethics:
Ethics permission for analysis of the data was obtained as part of the MSF ‘Bending the Curves’ project in KwaZulu-Natal from the Human Research Ethics Committee of the University of Cape Town. The study received an exemption for non-human subjects research from the Institutional Review Board at the Harvard T.H. Chan School of Public Health, because the Harvard-based researchers had access to de-identified data only.
Exposure
The exposure in this analysis was the number of lay counselors employed at a clinic. In 2015, many (but not all) lay counselors in KwaZulu-Natal were withdrawn as part of a redeployment policy with the stated aim of retraining and identifying new careers for these individuals, such as nursing and social work. As a result, HCT and other functions that the lay counselors were fulfilling had to be carried out by other health worker cadres, in particular nurses, or the few remaining lay counselors. Figure 1 describes the tasks carried out by lay counselors and nurses in South Africa prior to the removal of the counselors. As nurses have many tasks, shifting the responsibility of HCT back to nurses may have decreased clinic capacity to test incoming patients. Lay counselor position end dates were used to measure presence of counselors in the clinics. These dates were obtained using operational data from MSF. The nine clinics began with a total of 27 counselors prior to the redeployment policy. The first wave of counselor redeployment occurred on January 5th, 2015, after which a total of 15 counselors remained. The second wave of counselor redeployment occurred on June 15th, 2015, after which a total of six counselors remained across the nine clinics.
Figure 1. HIV care tasks carried out by lay counselors (red) and nurses (blue) at healthcare facilities in rural South Africa in 2014.

Abbreviations: HIV- = HIV-negative; CD4 = Cluster of Differentiation 4; WHO = World Health Organization; µL = microliter; TB = Tuberculosis; ART = Antiretroviral Therapy; ARVs = Antiretroviral drugs
Causal identification strategy
As shown in Figure 2, the only factor that appears to have affected the number of lay counselors employed in a given clinic-month during the study period was the two redeployment waves. Our effect estimates are, therefore, causal under two assumptions: i) the six (out of 27) lay counselors who were not redeployed are exchangeable (with respect to the outcome) with those who were redeployed, and ii) no third factor exists that both correlates with the timing of redeployment and affected the outcome. We elaborate on the plausibility of these assumptions in the discussion section.
Figure 2.
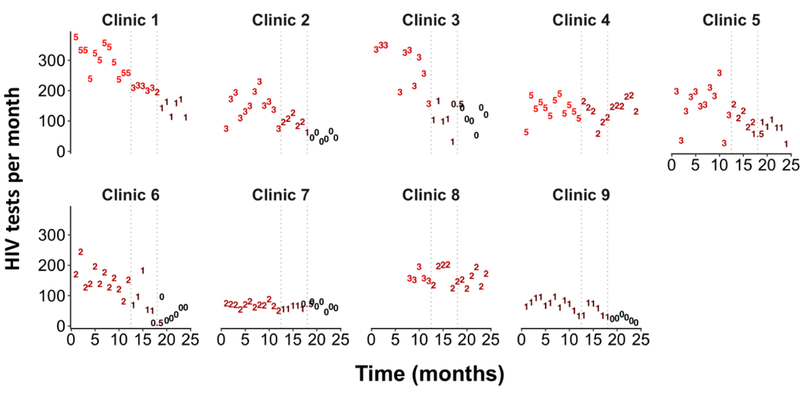
Number of HIV tests per month over time (raw data), by clinic1,2
Outcome
Given that lay counselors’ main task was HCT, the outcome of this study was the monthly number of HIV tests performed at each of the nine MSF-supported clinics.
Analysis
In the primary analysis, we used feasible generalized least squares regression to regress the monthly number of HIV tests at a clinic onto the number of lay counselors at a clinic, a binary indicator (‘clinic-level fixed effect’) for each clinic, and a binary indicator for each month of the study period (‘month-level fixed effect’). The clinic-level fixed effect controls for both observed and unobserved time-invariant confounding factors at the level of the clinic. The month-level fixed effect controls for time trends that are common across the nine clinics. To investigate whether the effect of the number of lay counselors at a clinic on the number of HIV tests performed was different between patient subgroups, we divided the dataset into four subsets (i) male patients; ii) female patients; iii) patients ≥15 years; and iv) patients <15 years) and then fitted the same regression model as described above in each of these four datasets. In addition, to more easily compare coefficients across sub-groups, we regressed the natural logarithm of the outcome variable (number of HIV tests performed at a clinic per month) onto the natural logarithm of the primary explanatory variable (the number of lay counselors present at a clinic in a given month) as well as clinic- and month-level fixed effects. Testing for serial correlation within clinics over time (using the Durban-Watson test, autocorrelation and partial autocorrelation plots, and likelihood ratio tests that compare models with different autoregressive structures) and a heteroskedastic error structure (using a likelihood ratio test comparing a model with and without heteroscedasticity-robust standard errors), we found that heteroscedasticity-robust standard errors adjusted for panel-specific AR(1) autocorrelation provided the best fit. We excluded June 2015 from the descriptive statistics by wave shown in Table 1 because this month was split into two redeployment waves (the second redeployment wave occurred on June 15th 2015). For the regression analysis, we considered a given clinic in June 2015 to have had the mean of the number of counselors it had in wave 1 and wave 2. Statistical analyses were implemented in Stata 13.0 (StataCorp, College Station, TX, USA).
Table 1.
Descriptive characteristics of the nine clinics included in this study
| Period I (Jan - Dec 2014) |
Period II (Jan – May 2015) |
Period III (July – Dec 2015) |
All periods* |
|
|---|---|---|---|---|
|
Months of
observation |
12 | 5 | 6 | 23 |
|
HIV Tests†
(number) |
||||
| Male adult | 4043 | 1231 | 818 | 6092 |
| Female adult | 10045 | 3198 | 1898 | 15141 |
| Male child | 1003 | 353 | 270 | 1626 |
| Female child | 1045 | 343 | 279 | 1667 |
| Total | 16136 | 5125 | 3265 | 24526 |
|
HIV Tests†
(monthly average) |
||||
| Male adult | 37.4 | 27.4 | 15.2 | 30.7 |
| Female adult | 93.0 | 71.1 | 35.2 | 78.4 |
| Male child | 9.3 | 7.8 | 5.0 | 8.3 |
| Female child | 9.7 | 7.6 | 5.2 | 8.3 |
| Counselors present | 27 | 15 | 6 | -- |
Excludes June 2015 because counselors left midway through the month. There were 1208 total tests in June 2015 (321 male adults, 786 female adults, 43 male children, and 58 female children).
Adults are defined as individuals ≥15 years of age; children are defined as individuals <15 years of age.
Results
Descriptive statistics:
The monthly number of HIV tests (total as well as by sex and adults versus children) was available for all clinics except for two months at Eshowe clinic (April and May 2014) and seven months at Syphile clinic (January to July 2014). A total of 24,526 HIV tests were carried out at the nine clinics over the study period: 15,141 (61%) on female adults, 6,092 (25%) on male adults, 1,667 (7%) on female children, and 1,626 (7%) on male children. Of the 24,536 total tests, 16,136 (66%) were administered during the 12 months preceding the first redeployment, 5,125 (21%) during the five months between the first and second redeployment waves, and 3,265 (13%) over the six months after the second redeployment (Table 1).
Figure 2 shows that i) the monthly number of HIV tests conducted at a clinic decreased in some clinics already prior to the first redeployment wave (e.g., clinic 3); ii) some clinics maintained a similar monthly number of HIV tests over time despite experiencing a substantial reduction in the number of lay counselors (e.g., clinic 4); and iii) there is little evidence over this study period that clinics required time to adapt to the loss of the lay counselors (i.e., we do not see rebounding of the monthly number of HIV tests after an initial decrease following the redeployment).
Regression analysis:
Using regression with a clinic- and month-level fixed effect, we estimate that the loss of one lay counselor at a clinic was associated with a mean decrease of 29.7 (95% CI: 21.2–38.2, p<0.001) HIV tests performed at the clinic per month (Table 2). In relative terms, we found that, on average, a ten percent reduction in the number of lay counselors at a clinic was associated with a 4.9% (95% CI: 2.8% - 7.0%, p<0.001) drop in the number of HIV tests performed at a clinic per month. The same relative reduction in the number of lay counselors at a clinic was associated with a similar percent reduction in the number of HIV tests performed across all four subgroups (females, males, adults, and children).
Table 2.
Effect of the loss of lay counselors on the monthly number of HIV tests conducted at a clinic1
| All tests | Females | Males | Adults | Children | |
|---|---|---|---|---|---|
| Absolute effect | |||||
| One counselor removed |
‒29.7 | ‒19.6 | ‒7.0 | ‒24.2 | ‒2.6 |
| 95% CI | ‒21.2, −38.2 | ‒13.3, −25.9 | ‒3.6, −10.4 | ‒16.0, −32.4 | ‒0.4, −4.7 |
| p-value |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
0.020 |
| n | 207 | 207 | 207 | 207 | 207 |
| Relative effect2,3,4 | |||||
| 10% reduction in lay counselors |
‒4.9% | ‒5.1% | ‒4.4% | ‒4.8% | ‒4.9% |
| 95% CI | ‒2.8%, −7.0% | ‒2.9%, −7.3% | ‒2.2%, −6.6% | ‒2.7%, −6.8% | ‒1.6%, −8.2% |
| p-value |
<0.001 | <0.001 | <0.001 | <0.001 |
0.003 |
| n | 177 | 177 | 177 | 177 | 174 |
Abbreviations: CI = Confidence interval
Each model included a binary indicator for each clinic and each month as explanatory variables.
These models regressed the natural logarithm of the number of HIV tests conducted at a clinic in each month on the natural logarithm of the number of counselors at a clinic each month, and a binary indicator for each clinic and each month.
The number of observations for the relative effect analysis was smaller than for the absolute effect analysis because there were zero lay counselors in 30 clinic-months and zero HIV tests among children in an additional three clinic-months (leading to missing values when the logarithm of the number of counselors and/or number of tests among children was calculated).
Discussion
A recent redeployment policy has led to severe losses of HIV lay counselors across the province of KwaZulu-Natal, and we illustrate here the impact of that policy in nine primary care clinics located in a rural municipality of the province. On average, for a ten percent reduction in the number of lay counselors at a clinic, 4.9% (95% CI: 2.8% - 7.0%) fewer HIV tests were carried out at that clinic per month. While fewer HIV tests were carried out among males than females, the relative impact of the number of lay counselors on the number of HIV tests conducted was similar for females as for males.
Because the redeployment policy appears to have been the only factor that affected the number of lay counselors employed in each clinic-month during the study period (see Figure 2), our effect estimates are causal under two assumptions: i) the six (out of 27) lay counselors who were not redeployed are exchangeable (with respect to the outcome) with those who were redeployed, and ii) no third factor exists that both correlates with the timing of the two redeployment waves and affected the outcome. The first assumption is unlikely to hold because personal characteristics of lay counselors (which in turn may be related to the number of HIV tests that they support) likely played a role in their decision to not take part in the redeployment. However, a large majority (78% [21/27]) of lay counselors were redeployed and five clinics were left with zero lay counselors at the end of the study period. Thus, even in the most extreme scenario – one where only the ‘best’ counselors (in terms of the number of HIV tests they support) were redeployed – this study still provides the causal effect of a reduction in the number of the 78% ‘best’ lay counselors at the study clinics on the outcome. The second assumption is, in our view, likely to hold in this study because there were no obvious changes in the supply or demand of HIV-related healthcare services that coincided with the timing of the two redeployment waves.
Given the well-documented health worker shortages in SSA[4] – and the threat that this shortage poses to the long-term success of the HIV response – shifting tasks from highly to less well trained health workers has been proposed to quickly and cost-effectively increase the capacity of the health system to provide HIV-related services.[13, 14] While we have not conducted a systematic literature review on the subject, this study provides, to our knowledge, the first estimate of the effect of lay counselors on HIV testing rates in primary care clinics in SSA. The comparatively large effect size demonstrates that lay health workers are a resource that can substantially boost health systems capacity to provide HIV-related services. More broadly, therefore, this observation lends support to the recent announcement by UNAIDS that it will lead a major international effort (endorsed by the African Union) to train and deploy two million additional community health workers in SSA (with a primary focus on HIV) by 2020, which would triple the number of community health workers in the region.[15, 16]
While HCT is only one among several essential HIV-related services provided by health systems in SSA, it is the entry point to the HIV care cascade. It is therefore important to note that for every person who did not receive an HIV test because the redeployment policy reduced the number of lay health workers, there may well be major individual- and population-level consequences. HIV-positive individuals who are not aware of their status will not initiate antiretroviral therapy (ART), and subsequently fail to achieve viral suppression—leading to increased risks to individual health and an increased likelihood of transmitting HIV.[17, 18] While it is difficult to predict how knowledge of HIV status affects risk behavior, there is some evidence that HIV-positive individuals who learn their HIV status may decrease their total number of partners and increase condom use.[19] In addition, individuals learning their HIV negative status may also be more likely to exhibit safe behavior to remain uninfected, such as by reliably using condoms.[20, 21] Lastly, the counseling that accompanies HIV testing at clinics may also reduce risk-taking behavior.[20, 21]
A major strength of this study is that it estimated the real-life effect of lay counselor reductions in primary care clinics. Specifically, our estimated effect size incorporates any actions that the nurses and other health workers who remained in a clinic undertook in response to the lay counselor loss. While the effect size that we estimate is the one that is most relevant for policy making (because it shows the real-life effect of withdrawing lay counselors from a clinic), to estimate the full value of a lay health worker, it will be important in future work to measure the net effect of the compensating actions that the remaining health workers undertake. If the remaining health workers compensated for the loss of a lay counselor by working harder and carrying out some of the tasks that the lay counselor would have carried out had he/she continued to work in the clinic, then the effect estimated in this study will lead to an underestimate of the true value of lay counselors. For instance, if nurses did indeed carry out some of the HCT services that the lay counselors would have carried out had they remained in the clinic (as appears to have been the case, for example, in clinic 4 and clinic 7), this change in action would either have led to greater nurse workload (with potential negative consequences, such as job dissatisfaction and reduced quality of care) or to a reduction in nurse activities other than HCT.
This study has several limitations. First, we only examined the effect of lay counselors on one health system function. The lay counselors, however, were responsible for carrying out activities beyond HCT, including ART adherence support, CD4-count testing, HIV education, pulling and re-filing records, and triaging and filing of test results. In addition, being HIV-positive themselves, lay counselors may also alleviate patients’ concerns about being stigmatized by healthcare workers, which in turn may have positive effects on retention in care, medication adherence, and ultimately viral suppression. The true negative effect of losing a lay counselor on the output of HIV-related services is thus likely substantially larger than estimated in this study. Second, we only had data until December 2015. We were, thus, unable to investigate the longer term effect of lay counselor removal on HIV testing rates. Third, we only examined the quantity of HIV counseling and testing performed, and not the quality of these services. Since a fair cost-effectiveness comparison of the performance of different cadres of health workers in carrying out the same activity needs to account for quality differences, future studies should also measure the quality of HIV counseling, and investigate whether differences in the sensitivity and specificity of HIV test results exist when the testing is performed by different cadres. Lastly, this study was conducted at a relatively small number (nine) of clinics in only one municipality of South Africa, and these clinics were all supported by MSF (which is not the case for other clinics in South Africa), which limits the external validity of our findings. It is also possible that inclusion of the municipality’s third Health Services Area (Catherine Booth), from which we did not have data, would have changed the estimates.
Some of the most important future policy developments in the HIV response demand substantial increases in the capacity to provide HCT. “Test and treat” requires frequent and routine HIV testing to ensure that people are detected soon after newly acquiring HIV to ensure rapid ART initiation for prevention of transmission. Similarly, pre-exposure prophylaxis of HIV requires frequent HIV testing to ensure that people who seroconvert while taking prophylactic antiretroviral medicines are quickly transferred to HIV treatment and care programs. To provide these additional HIV testing services, substantial increases in the capacity of health systems in SSA for HCT, including through facility-based, mobile, and self-testing, will be required. As demonstrated by this study, lay health workers (e.g., lay counselors) are one effective source of this capacity, and should be increasingly trained and utilized as part of future HIV care models in South Africa and beyond.
Acknowledgements
JH and PG are joint first authors. JH, PG, and TB conceptualized the study, performed the data analysis, and drafted the manuscript. All authors provided critical inputs to the manuscript text and analysis, and approved the final version of the manuscript. PG is the guarantor of the work. TB received funding from the Alexander von Humboldt Foundation. The corresponding author had full access to the data and had final responsibility for the decision to submit for publication.
Funding: Alexander von Humboldt Foundation
Footnotes
The numbers in the plot indicate the number of lay counselors employed at a given clinic in a given month.
The vertical gray dashed lines indicate when each of the two redeployment waves occurred.
References:
- 1.Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390(10100):1260–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang H, Wolock TM, Carter A, Nguyen G, Kyu HH, Gakidou E, et al. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. The lancet HIV 2016; 3(8):e361-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection - Recommendations for a public health approach In. Second ed. Geneva: World Health Organization; 2016. pp. 480. [PubMed] [Google Scholar]
- 4.World Health Organization. World Health Statistics 2017: Monitoring health for the SDGs In. Geneva: World Health Organization; 2017. [Google Scholar]
- 5.Callaghan M, Ford N, Schneider H. A systematic review of task- shifting for HIV treatment and care in Africa. Hum Resour Health 2010; 8:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bemelmans M, van den Akker T, Ford N, Philips M, Zachariah R, Harries A, et al. Providing universal access to antiretroviral therapy in Thyolo, Malawi through task shifting and decentralization of HIV/AIDS care. Tropical medicine & international health : TM & IH 2010; 15(12):1413–1420. [DOI] [PubMed] [Google Scholar]
- 7.Sanjana P, Torpey K, Schwarzwalder A, Simumba C, Kasonde P, Nyirenda L, et al. Task-shifting HIV counselling and testing services in Zambia: the role of lay counsellors. Hum Resour Health 2009; 7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M, Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health 2011; 9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics South Africa. Census 2011 In. Pretoria, South Africa: Government of South Africa; 2011. [Google Scholar]
- 10.O Shisana TR, Simbayi LC, Zuma K, Jooste S, Zungu N, Labadarios D, Onoya D. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012 In. Cape Town, South Africa: Human Sciences Research Council; 2014. [DOI] [PubMed] [Google Scholar]
- 11.Huerga H. Mbongolwane and Eshowe HIV Impact in Population Survey In. Pretoria, South Africa: Médecines Sans Frontières; 2014. [Google Scholar]
- 12.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet 2009; 374(9692):817–834. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Task shifting to tackle health worker shortages In. Geneva: World Health Organzization; 2007. [Google Scholar]
- 14.World Health Organization. Task shifting: global recommendations and guidelines In. Geneva: World Health Organization; 2008. [Google Scholar]
- 15.African Union. 2 million African community health workers In. Addis Ababa, Ethiopia: African Union; 2017. [Google Scholar]
- 16.UNAIDS, One Million Community Health Workers. UNAIDS joins forces with the One Million Community Health Workers campaign to achieve the 90–90–90 treatment target In. Geneva: UNAIDS,; 2016. [Google Scholar]
- 17.Tanser F, Bärnighausen T, Grapsa E, Zaidi J, Newell M- L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science (New York, NY) 2013; 339:966–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. The New England journal of medicine 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delavande A, Kohler HP. The impact of HIV testing on subjective expectations and risky behavior in Malawi. Demography 2012; 49(3):1011–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Denison JA, O’Reilly KR, Schmid GP, Kennedy CE, Sweat MD. HIV Voluntary Counseling and Testing and Behavioral Risk Reduction in Developing Countries: A Meta-analysis, 1990–2005. AIDS and Behavior 2008; 12(3):363–373. [DOI] [PubMed] [Google Scholar]
- 21.Allen S, Meinzen-Derr J, Kautzman M, Zulu I, Trask S, Fideli U, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. Aids 2003; 17(5):733–740. [DOI] [PubMed] [Google Scholar]


