Abstract
A 60-year-old man visited our hospital for further examination of an abnormal chest radiograph. Computed tomography (CT) images revealed enlarged mediastinal lymph nodes and multiple pulmonary nodules.
Further evaluation by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) was performed and he was diagnosed with sarcoidosis. Six weeks after EBUS-TBNA, he presented to the emergency department with a high-grade fever. CT scan revealed an enlarged mediastinal lymph node. He was diagnosed with mediastinal adenitis and treated successfully with antibiotics. EBUS-TBNA is a highly accurate diagnostic tool, but clinicians should be aware of mediastinal infectious complication that could be asymptomatic for long period of time.
Keywords: Mediastinal adenitis, Endobronchial ultrasound-guided transbronchial needle aspiration, Infectious complication, Sarcoidosis
1. Introduction
Due to its high-level of diagnostic accuracy and safety, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has become the standard method for diagnosing mediastinal lesions. However, critical mediastinal infectious complication has been reported. Previously, infectious complication has been reported to occur within a few weeks after the procedure and was suspected from symptoms such as fever, cough, or chest pain. We report a case of mediastinal adenitis that developed 6 weeks after EBUS-TBNA.
2. Case report
A 60-year-old man visited our hospital for further evaluation of an abnormal chest radiograph obtained on a health examination. He had a history of foot drop due to cervical spine injury and prostatic hyperplasia, which was treated with naftopidil. He had a 15-pack-year history of smoking. He did not report any symptoms and his physical examination was unremarkable. Computed tomography (CT) revealed multiple lung nodules and mediastinal and hilar adenopathy (Fig. 1). Mediastinum demonstrated the accumulation of gallium-67. EBUS-TBNA (BF-UC260FW, Olympus, Tokyo, Japan) was performed in the lymph node station 4R using 21 gauge needle (NA-201SX-4021, Olympus, Tokyo, Japan) and a transbronchial lung biopsy (TBLB) was performed for multiple lung nodules. On EBUS-TBNA, echographic images suggested an isoechoic texture. 3 passes were made with 21 gauge needle without any event during the procedure and the patient was discharged the following day.
Fig. 1.
Computed tomography before endobronchial ultrasound-guided transbronchial needle aspiration. Enlarged mediastinal lymph nodes with calcification were observed.
Although only tracheal cartilage was detected from the EBUS-TBNA sample, a non-caseating granuloma was seen in the TBLB samples and he was diagnosed with sarcoidosis. Klebsiella pneumoniae was detected from TBNA needle washing culture but he had no symptom up to two weeks during follow-up and the culture result was considered as contamination during the procedure.
Six weeks after the EBUS-TBNA, the patient developed a fever, chills, and fatigue and presented to the emergency department next day. On arrival, his vital signs were as follows: body temperature, 40.7 °C; blood pressure, 104/43 mmHg; pulse rate, 123 beats/min; SpO2, 97% in ambient air. On physical examination, his extremities were cold but other than that, the remainder of the examination was unremarkable.
Results from blood tests revealed white blood cell count of 3.8 × 109 cells/L, C-reactive protein level of 193.6 mg/L, and procalcitonin level of 42.51 μg/L (Table 1). A widened mediastinum was detected by a chest radiograph and an enhanced CT revealed swelling of station 4R lymph node where the EBUS-TBNA was performed six weeks ago. The lesion had a hypodense center suggestive of an abscess. Severe sepsis due to infectious mediastinal adenitis was suspected and treatment consisting of 1g of doripenem was administered every 8 hours and vasopressor was initiated. Klebsiella pneumoniae, the same species that was identified from TBNA needle washing culture, was detected in a blood and sputum culture. The patient started recovering and the vasopressor was tapered off on day 6. The fever lasted till day 21 and antibiotics were continued for one month.
Table 1.
Blood examination on date of admission.
| Peripheral blood | Biochemistry | ||
|---|---|---|---|
| White blood cells | 3.8 × 109/L | Lactate dehydrogenase | 486 IU/L |
| Neutrophil | 93.2% | Aspartate aminotransferase | 236 IU/L |
| Lymphocyte | 4.2% | Alanine aminotransferase | 73 IU/L |
| Monocyte | 1.6% | Alkaline phosphatase | 405 IU/L |
| Eosinophil | 0.5% | γ-glutamyl transpeptidase | 118 IU/L |
| Basophil | 0.3% | Creatine kinase | 214 IU/L |
| Hemoglobin | 118g/L | Urea nitrogen | 19 IU/L |
| Platelets | 1.64 × 1011/L | Creatinine | 11.9 mg/L |
| Sodium | 140 mEq/L | ||
| Blood coagulation | Potassium | 3.2 mEq/L | |
| Activated partial thromboplastin time | 44.1 sec | Chloride | 106 mEq/L |
| Prothrombin time | 16.3 sec | Calcium | 84 mg/L |
| Prothrombin time-international normalized ratio | 1.26 | ||
| D-dimer | 20.3 mg/L | Serology | |
| C-reactive protein | 193.6 mg/L | ||
| Procalcitonin | 42.51 μg/L |
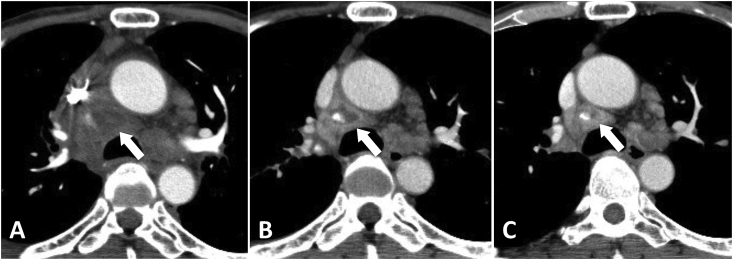
CT on day 28 revealed a shrinkage of the hypodense region in the lymph node and the patient was discharged on day 34 (Fig. 2).
Fig. 2.
Computed tomography on day of admission (A), 2 weeks (B), 4 weeks (C) after treatment. The 4R lymph nodes were shrinking gradually after treatment.
3. Discussion
EBUS-TBNA has been reported to be a safe and useful method of choice for the diagnosis of mediastinal lesion. Sonographic features of EBUS itself is helpful differentiating sarcoidosis from other diseases and the diagnostic accuracy of EBUS-TBNA for sarcoidosis can be as high as 79%, ranging from 54–93% [1,2]. TBLB is another procedure used to establish the diagnosis of sarcoidosis, but its accuracy ranges from 40–90% [3,4] and it carries a risk of a pneumothorax (1–6%) and hemoptysis (0.8%) [5]. A nationwide survey in Japan reported that the complication rate of EBUS-TBNA was relatively low (1.23%) and infectious complications developed in 0.19% of patients, which included 7 cases of mediastinal infection [6]. Other studies also report the rate of severe adverse events from EBUS-TBNA to be less than 1% [7,8]. Complications associated with EBUS-TBNA are rare, but mediastinal infectious complication after EBUS-TBNA has been reported sporadically with fatal clinical course.
From 28 cases of mediastinal infectious complication after EBUS-TBNA (Table 2), the symptom of most cases started with slight illness, such as fever or chest pain but progressed into a severe condition, such as septic shock. In 20 cases, invasive treatment such as thoracotomy were needed and one case resulting in mortality [30]. Epstein SK et al. suggested that the mechanism for infectious complication after TBNA is infection by the oropharyngeal commensal organisms that contaminate the working channel of the EBUS-scope while passing the oropharyngeal airway and being inoculated into the target lesion by a puncture needle [9]. In this case, Klebsiella pneumoniae was cultured from TBNA needle washings which we send for culture routinely. The same organism was found in the blood and sputum cultures six weeks after the procedure, which suggests that infection was established during EBUS-TBNA. Klebsiella pneumoniae is one of the oropharyngeal commensal bacterium. EBUS-scope might have been contaminated with Klebsiella pneumoinae while passing the oropharyngeal airway during EBUS-TBNA.
Table 2.
Case list of infectious complication caused by Endobronchial ultrasound-guided transbronchial needle aspiration.
| Age/Sex | Host factor | Location/Size (mm) | Number of passes | Diagnosis | Lapsed days | Pathogen | Invasive treatment | Ref. |
|---|---|---|---|---|---|---|---|---|
| 50/M | Non | #7/25 × 32 | 2 | Ad of unknown origin | 19 | Actinomyces odontolyticus, Streptococcus mutans | Pericardiocentesis | [15] |
| 58/M | Melanoma | posterior to the bronchus intermedius/34 × 29 | 3 | Lung SCC | 9 | Negative | N.P | [15] |
| 68/M | Diabetes | right paratracheal opacity/N.D | N.D | HCC | N.D | Streptococcus viridans | Thoracotomy | [16] |
| 68/M | Non | pretracheal lymph node/N.D | 10 | Colon cancer | 32 | Candida albicans gamma-hemolytic streptococcus | EBUS-guided aspiration | [17] |
| 66/M | Non | right paratracheal mass/N.D | N.D | Undefined malignant cells | 8 | Proionibacterium acnes, Bacteroides eubacterium | Thoracotomy | [17] |
| 89/F | Non | #7/N.D | 4 | Nonspecific inflammatory change | 14 | Alpha-hemolytic streptococcus, Diphtheroids | Thoracotomy | [18] |
| 48/M | Non | #7/15 | N.D | N.D | 31 | Klebsiella pneumoniae | Thoracotomy | [19] |
| 67/M | Non | #4R/15 × 9 | 3 | Colon cancer | 12 | Negative | N.P | [20] |
| 59/M | Non | N.D/N.D | 1 | SCLC | 7 | Negative | N.P | [21] |
| 64/F | Non | #7/26 | 3 | Lung Ad | 5 | Negative | N.P | [22] |
| 35/F | N.D | #7/52 × 42 | N.D | Bronchogenic cyst | 14 | Group C streptococcus | Thoracotomy | [23] |
| 73/M | Diabetes | #4R/18 × 25 | 5 | Lung SCC | 11 | Negative | N.P | [24] |
| 48/M | Non | #7/19 × 21 | N.D | Lung SCC | 4 | Negative | Thoracotomy | [25] |
| 72/M | Non | #7/N.D | N.D | Lung SCC | 7 | Group C streptococcus | Thoracotomy | [26] |
| 56/F | Non | anterior mediastinum/26 × 16 | 3 | Bronchogenic cyst | 3 | Alpha Streptococcus | N.P | [27] |
| 75/M | Diabetes | #4R/N.D | 2 | Nonspecific inflammatory change | 7 | Streptococcus intermidius | Median sternotomy | [28] |
| 42/M | Non | #4R, #7, #11L/N.D | N.D | Sarcoidosis | 21 | Negative | Mediastinoscopy | [29] |
| 55/F | N.D | #4R, #7/60 | N.D | Lung non SCLC | 6 | Streptococcus viridans | Pericardiocentesis | [30] |
| 54/M | N.D | #4R/N.D | N.D | Colon cancer | 14 | Group C streptococcus | Pericardial window operation | [30] |
| 33/F | Non | posterior mediastinum/48 × 72 | 3 | Bronchogenic cyst | 3 | Staphylococcus epidermidis | Thoracotomy | [31] |
| 61/M | Lung cancer | #7/N.D | N.D | Not diagnosed | 0 | N.D | Thoracotomy | [32] |
| 61/F | Non | #4R, #7/N.D | N.D | Necrotizing lymphadenopathy | 4 | N.D | N.P | [33] |
| 66/M | Non | #4R/48 | 3 | Lung SCC | 7 | Streptococcus pneumoniae | Thoracotomy | [34] |
| 64/M | Non | #4R, #7/N.D | N.D | Colon cancer | 14 | Negative | Thoracotomy | [10] |
| 49/M | Diabetes | #4R, #7/N.D | N.D | Sarcoidosis | 14 | Gemella morbillorum | Mediastinotomy | [10] |
| 36/M | Non | #4R, #7/N.D | N.D | Sarcoidosis | 21 | Prevotella buccae, Streptococcus anginosus, Streptococcus pneumoniae | Thoracotomy | [10] |
| 44/F | Thyroid carcinoma | #4R/60 × 52 × 44 | N.D | Benign cyst | 2 | Streptococcus pneumoniae | Aspiration of cystic mediastinal mass | [35] |
| 57/M | Mantel cell lymphoma | #4R, #7, #11R/N.D | N.D | Granulomatous lymphadenitis | 14 | Pseudomonas aeruginosa | Stent placement with rigid bronchoscopy | [35] |
| 60/M | Non | #4R | 3 | Sarcoidosis | 42 | Klebsiella pneumoniae | N.P | Our case |
M: male, F: female, Ad: adenocarcinoma, SCC: squamous cell carcinoma, HCC: hepatic cell carcinoma, SCLC: small cell lung cancer, Ref.: reference, N.D: no data N.P: not performed.
The risk factors for developing mediastinitis as a complication were identified to be (i) number of times the TBNA-needle is passed into the lymph node; (ii) number of samples per lymph node; (iii) expertise of the operator; (iv) necrotic or cystic lymph node; and (v) contamination of the working channel [10]. In this case, 3 passes were made, but it was difficult to obtain an adequate sample due to the firmness of the lymph node, and long procedure duration might have led to contamination of the working channel.
The time to onset of symptoms was longer than those previously reported, such as 1–32 days after procedure; most cases occurred within two weeks (mean time 11.2 days) (Table 2). In this case, enhanced CT (Fig. 1) showed partial contrast defect and calcification in enlarged mediastinal lymph. These findings suggest a replacement of the granulomas with hyaline tissue over time, which is occasionally observed in sarcoidosis [11]. Bacteria inoculated into the hypovascular hyaline tissue might have been able to escape from the immune system and the patient remained asymptomatic for a long period of time.
For the prevention of mediastinitis, there is no consensus on the routine antibiotic prophylaxis before EBUS-TBNA and we didn't consider using it in this case. However, several studies reported the high positive rate of needle washing culture from the TBNA [12,13]. This suggests that the procedure has the potential risk for inoculating bacteria into the target lesion. Therefore, antibiotic prophylaxis may be considered in high risk patients, such as in immunocompromised hosts or those with necrotizing, cystic, or calcified lesions, including hypovascular lesions. Gargling with chlorhexidine before the procedure might be also helpful in reducing the risk of bacterial adherence to EBUS-scope[14].
In conclusion, we report a case developing complication of mediastinal adenitis after six weeks undergoing EBUS-TBNA. Clinicians should be aware that this critical complication could develop after long period of time.
Conflicts of interest
The authors have no conflicts of interest (COI).
References
- 1.Dhooria S., Agarwal R., Aggarwal A.N., Bal A., Gupta N., Gupta D. Differentiating tuberculosis from sarcoidosis by sonographic characteristics of lymph nodes on endobronchial ultrasonography: a study of 165 patients. J. Thorac. Cardiovasc. Surg. 2014;148(2):662–667. doi: 10.1016/j.jtcvs.2014.01.028. [DOI] [PubMed] [Google Scholar]
- 2.Agarwal R., Srinivasan A., Aggarwal A.N., Gupta D. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: a systematic review and meta-analysis. Respir. Med. 2012;106(6):883–892. doi: 10.1016/j.rmed.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 3.Gilman M.J., Wang K.P. Transbronchial lung biopsy in sarcoidosis. An approach to determine the optimal number of biopsies. Am. Rev. Respir. Dis. 1980;122(5):721–724. doi: 10.1164/arrd.1980.122.5.721. [DOI] [PubMed] [Google Scholar]
- 4.Koonitz C.H., Joyner L.R., Nelson R.A. Transbronchial lung biopsy via the fiberoptic bronchoscope in sarcoidosis. Ann. Intern. Med. 1976;85(1):64–66. doi: 10.7326/0003-4819-85-1-64. [DOI] [PubMed] [Google Scholar]
- 5.Du Rand I.A., Barber P.V., Goldring J., Lewis R.A., Mandal S., Munavvar M., Rintoul R.C., Shah P.L., Singh S., Slade M.G., Woolley A., British G. Thoracic society interventional bronchoscopy guideline, British thoracic society guideline for advanced diagnostic and therapeutic flexible bronchoscopy in adults. Thorax. 2011;66(Suppl 3) doi: 10.1136/thoraxjnl-2011-200713. iii1-21. [DOI] [PubMed] [Google Scholar]
- 6.Asano F., Aoe M., Ohsaki Y., Okada Y., Sasada S., Sato S., Suzuki E., Semba H., Fukuoka K., Fujino S., Ohmori K. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan society for respiratory endoscopy. Respir. Res. 2013;14:50. doi: 10.1186/1465-9921-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Bartheld M.B., van Breda A., Annema J.T. Complication rate of endosonography (endobronchial and endoscopic ultrasound): a systematic review. Respiration. 2014;87(4):343–351. doi: 10.1159/000357066. [DOI] [PubMed] [Google Scholar]
- 8.Dhooria S., Sehgal I.S., Gupta N., Aggarwal A.N., Behera D., Agarwal R. Diagnostic yield and complications of EBUS-TBNA performed under bronchoscopist-directed conscious sedation: single center experience of 1004 subjects. J. Bronchol. Interv. Pulmonol. 2017;24(1):7–14. doi: 10.1097/LBR.0000000000000332. [DOI] [PubMed] [Google Scholar]
- 9.Epstein S.K., Winslow C.J., Brecher S.M., Faling L.J. Polymicrobial bacterial pericarditis after transbronchial needle aspiration. Case report with an investigation on the risk of bacterial contamination during fiberoptic bronchoscopy. Am. Rev. Respir. Dis. 1992;146(2):523–525. doi: 10.1164/ajrccm/146.2.523. [DOI] [PubMed] [Google Scholar]
- 10.Voldby N., Folkersen B.H., Rasmussen T.R. Mediastinitis: a serious complication of endobronchial ultrasound-guided transbronchial needle aspiration. J. Bronchol. Interv. Pulmonol. 2017;24(1):75–79. doi: 10.1097/LBR.0000000000000231. [DOI] [PubMed] [Google Scholar]
- 11.Leslie K., Wick M. second ed. Elsevier/Saunders; Philadelphia: 2011. Practical Pulmonary Pathology: a Diagnostic Approach; pp. 250–252. [Google Scholar]
- 12.Steinfort D.P., Johnson D.F., Irving L.B. Incidence of bacteraemia following endobronchial ultrasound-guided transbronchial needle aspiration. Eur. Respir. J. 2010;36(1):28–32. doi: 10.1183/09031936.00151809. [DOI] [PubMed] [Google Scholar]
- 13.Fujiwara T., Nakajima T., Toyoda T., Kamata T., lshibashi F., Iida T., Yoshino I., Shiba M. Fever incidence after endobronchial ultrasound-guided transbronchial needle aspiration. J. Jpn. Soc. Respir. Endosc. 2015;37(1):11–15. [Google Scholar]
- 14.Donatsky A.M., Holzknecht B.J., Arpi M., Vilmann P., Meisner S., Jorgensen L.N., Rosenberg J. Oral chlorhexidine and microbial contamination during endoscopy: possible implications for transgastric surgery. A randomized, clinical trial. Surg. Endosc. 2013;27(6):1914–1922. doi: 10.1007/s00464-012-2686-5. [DOI] [PubMed] [Google Scholar]
- 15.Haas A.R. Infectious complications from full extension endobronchial ultrasound transbronchial needle aspiration. Eur. Respir. J. 2009;33(4):935–938. doi: 10.1183/09031936.00025708. [DOI] [PubMed] [Google Scholar]
- 16.Huang C.T., Chen C.Y., Ho C.C., Yu C.J. A rare constellation of empyema, lung abscess, and mediastinal abscess as a complication of endobronchial ultrasound-guided transbronchial needle aspiration. Eur. J. Cardiothorac. Surg. 2011;40(1):264–265. doi: 10.1016/j.ejcts.2010.11.037. [DOI] [PubMed] [Google Scholar]
- 17.Kouskov O.S., Almeida F.A., Eapen G.A., Uzbeck M., Deffebach M. Mediastinal infection after ultrasound-guided needle aspiration. J. Bronchol. Interv. Pulmonol. 2010;17(4):338–341. doi: 10.1097/LBR.0b013e3181f30d74. [DOI] [PubMed] [Google Scholar]
- 18.Moffatt-Bruce S.D., Ross P., Jr. Mediastinal abscess after endobronchial ultrasound with transbronchial needle aspiration: a case report. J. Cardiothorac. Surg. 2010;5:33. doi: 10.1186/1749-8090-5-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parker K.L., Bizekis C.S., Zervos M.D. Severe mediastinal infection with abscess formation after endobronchial ultrasound-guided transbrochial needle aspiration. Ann. Thorac. Surg. 2010;89(4):1271–1272. doi: 10.1016/j.athoracsur.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Kurimoto N., Shinmyo T., Tagay R., Andou K., Morita K., Mochizuki A., Nakamura H., Koike J. A case of acute mediastinitis after endobronchial needle aspiration. Nihon Kokyuki Gakkai Zasshi. 2011;49(8):588–591. [PubMed] [Google Scholar]
- 21.Gochi F., Chen F., Aoyama A., Date H. Mediastinal infectious complication after endobronchial ultrasound-guided transbronchial needle aspiration. Interact. Cardiovasc. Thorac. Surg. 2013;17(4):751–752. doi: 10.1093/icvts/ivt273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leong S.C., Marshall H.M., Bint M., Yang I.A., Bowman R.V., Fong K.M. Mediastinal abscess after endobronchial ultrasound-guided transbronchial needle aspiration: a case report and literature review. J. Bronchol. Interv. Pulmonol. 2013;20(4):338–341. doi: 10.1097/LBR.0b013e31829ae243. [DOI] [PubMed] [Google Scholar]
- 23.Gamrekeli A., Kalweit G., Schafer H., Huwer H. Infection of a bronchogenic cyst after ultrasonography-guided fine needle aspiration. Ann. Thorac. Surg. 2013;95(6):2154–2155. doi: 10.1016/j.athoracsur.2012.10.071. [DOI] [PubMed] [Google Scholar]
- 24.Fukunaga K., Kawashima S., Seto R., Nakagawa H., Yamaguchi M., Nakano Y. Mediastinitis and pericarditis after endobronchial ultrasound-guided transbronchial needle aspiration. Respirol. Case Rep. 2015;3(1):16–18. doi: 10.1002/rcr2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jang S.M., Kim M.J., Cho J.S., Lee G., Kim A., Kim J.M., Park C.H., Park J.M., Song B.G., Eom J.S. New-onset malignant pleural effusion after abscess formation of a subcarinal lymph node associated with endobronchial ultrasound-guided transbronchial needle aspiration. Tuberc. Respir. Dis. (Seoul) 2014;77(4):188–192. doi: 10.4046/trd.2014.77.4.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matsuoka K., Ito A., Murata Y., Sakane T., Watanabe R., Imanishi N., Matsuoka T., Nagai S., Ueda M., Miyamoto Y. Severe mediastinitis and pericarditis after transbronchial needle aspiration. Ann. Thorac. Surg. 2015;100(5):1881–1883. doi: 10.1016/j.athoracsur.2014.12.093. [DOI] [PubMed] [Google Scholar]
- 27.Onuki T., Kuramochi M., Inagaki M. Mediastinitis of bronchogenic cyst caused by endobronchial ultrasound-guided transbronchial needle aspiration. Respirol. Case Rep. 2014;2(2):73–75. doi: 10.1002/rcr2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ishimoto H., Yatera K., Uchimura K., Oda K., Takenaka M., Kawanami T., Tanaka F., Mukae H. A serious mediastinum abscess induced by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA): a case report and review of the literature. Intern. Med. 2015;54(20):2647–2650. doi: 10.2169/internalmedicine.54.4465. [DOI] [PubMed] [Google Scholar]
- 29.McGovern Murphy F., Grondin-Beaudoin B., Poulin Y., Boileau R., Dumoulin E. Mediastinal abscess following endobronchial ultrasound transbronchial needle aspiration in a patient with sarcoidosis. J. Bronchol. Interv. Pulmonol. 2015;22(4):370–372. doi: 10.1097/LBR.0000000000000183. [DOI] [PubMed] [Google Scholar]
- 30.Lee H.Y., Kim J., Jo Y.S., Park Y.S. Bacterial pericarditis as a fatal complication after endobronchial ultrasound-guided transbronchial needle aspiration. Eur. J. Cardio Thorac. 2015;48(4):630–632. doi: 10.1093/ejcts/ezu477. [DOI] [PubMed] [Google Scholar]
- 31.Mogal R., Banerjee N., Yung B., Mukherjee D. A young woman with severe chest pain after undergoing endobronchial ultrasound-guided transbronchial needle aspiration for a large mediastinal mass. J. Bronchol. Interv. Pulmonol. 2016;23(3):236–238. doi: 10.1097/LBR.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 32.Yamazaki N., Kawabe M., Tanaka H., Watanabe H., Nakade M. Open drainage for mediastinitis after endobronchial ultrasonography-guided transbronchial needle aspiration. Kyobu Geka. 2016;69(5):384–387. [PubMed] [Google Scholar]
- 33.Giesa C., Heining L., Hecker E., Ewig S. Severe complications of ultrasound guided transbronchial needle aspiration--a case series and review of the literature. Pneumologie. 2016;70(1):23–27. doi: 10.1055/s-0041-109383. [DOI] [PubMed] [Google Scholar]
- 34.Yokoyama Y., Nakagomi T., Shikata D., Higuchi R., Oyama T., Goto T. Surgical treatment for mediastinal abscess induced by endobronchial ultrasound-guided transbronchial needle aspiration: a case report and literature review. World J. Surg. Oncol. 2017;15(1):130. doi: 10.1186/s12957-017-1206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jahoor A., Ghamande S., Jones S., Boethel C., White H.D. Mediastinitis following endobronchial ultrasound-guided transbronchial needle aspiration. J. Bronchol. Interv. Pulmonol. 2017;24(4):323–329. doi: 10.1097/LBR.0000000000000370. [DOI] [PubMed] [Google Scholar]