Abstract
A pyrogen is a substance that causes fever after intravenous administration or inhalation. Gram negative endotoxins are the most important pyrogens to pharmaceutical laboratories. In the International, United States, Japanese and European Pharmacopoeias, there are two official methods to evaluate pyrogenicity—that is, the bacterial endotoxin test, and the pyrogen test. The main objective of this review is to compare the monographs of each test among the different Pharmacopeias, to detect similarities and differences. The former can be considered fully harmonized, and only non-significant differences were detected. The latter, which is the only available assay for some products and formulations to demonstrate apyrogenicity, shows large differences, which should be considered.
Keywords: endotoxins, pyrogens, parenteral drug products, pharmacopoeial test, harmonization
1. Introduction
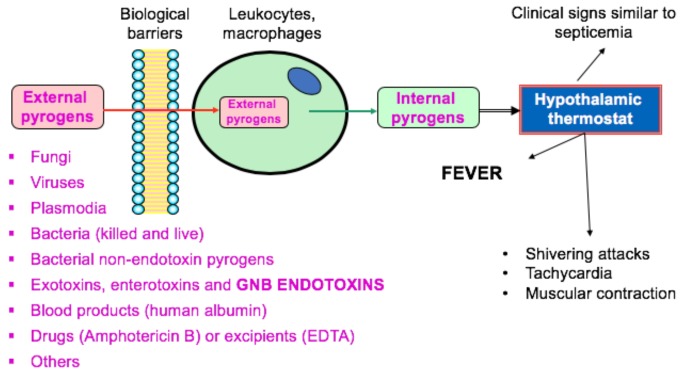
Pyrogens are defined as substances that cause exacerbate febrile reactions when sufficient amounts gain access to the circulatory system after parenteral administration or inhalation. Although “pyrogen” is a general term to define fever-producing agents (Figure 1), it is frequently used to specifically describe Gram-negative bacteria (GNB) endotoxins in the pharmaceutical industry. Other pyrogenic substances can occur, although the risks are lower [1].
Figure 1.
Most significant pyrogens for pharmaceutical manufacturers and sequential events of fever. GNB = Gram-negative bacteria.
GNB endotoxin is a high molecular weight complex that contains lipopolysaccharide (LPS), protein, and phospholipid originating from the outer membrane of Gram-negative bacteria. Most pharmacopoeial endotoxin reference standards should be more correctly described as purified LPS since its chemical nature after purification is a lipid component called Lipid A, covalently bound to a polysaccharide composed of two parts, the core and a variable O-specific side chain, responsible for the specific immune reaction evoked in the host.
Depyrogenation is one of the most important challenges for pharmaceutical manufactures of parenteral drugs, since fever in a patient depends on the total amount of pyrogen delivered to that patient. Dry heat at temperatures above 180 °C is the method of choice for heat-resistant products, since GNB endotoxins are thermostable in the presence of moist heat and are not significantly destroyed by conventional autoclaving processes [2]. Moreover, another interesting property of GNB endotoxin is its tendency to aggregate into vesicles due to the attraction between hydrophobic groups of the LPS. These vesicles are large enough to be removed by reverse-osmosis processes or size exclusion chromatography. It should be considered, that in an aqueous environment the endotoxin aggregation state depends on its surrounding environment, i.e., divalent cations such as calcium or magnesium forms larger, more stable and lower soluble endotoxin aggregates. This property can be of particular interest in depyrogenation by ultrafiltration processes. Utilizing the electrostatic properties of GNB endotoxin can offer another interesting alternative for depyrogenation. It has been described that endotoxins are positively charged at pH levels above 5, and negatively charged at pH levels under 2. This property is very useful since it accounts for the attraction that GNB endotoxins have for stationary phases in chromatographic isolation [3].
The origins of the rabbit pyrogen test data back to studies by Seibert, who developed a mammalian test between 1923 and 1925, in response to concerns from surgeons about fever [4]. In 1943, Welch and coworkers published two reference papers outlining the results of a collaborative study performed by the U.S. Food & Drug Administration (FDA), the National Institutes of Health (NIH), and several pharmaceutical companies [5,6], resulting in the first rabbit pyrogen test (RPT) to be included in the United States Pharmacopoeia (USP). The current USP monograph, based on the evaluation of the rectal temperature of rabbits before and after an intravenous injection of a test solution into the ear, is not substantially different from the original one.
The bacterial endotoxin test (BET)—also known as LAL-test—is an alternative in vitro endotoxin assay, accepted by the main regulatory drug agencies (FDA, European Medicines Agency (EMA) or Pharmaceuticals and Medical Devices Agency (PMDA), among others). There are three techniques to perform this test, all of them based on the Limulus amebocyte lysate (LAL). In 1964, Levin and Bang first recognized the coagulation of the lysate in the presence of GNB endotoxin [7,8]. However, some complex formulations such as radiopharmaceuticals, biotechnology formulations, etc. cannot be assayed by BET. Despite scientist having proposed several in vitro methods which are faster and more easily automated than the original LAL-tests of Cooper and Mills, the latter still remains the only official in the main pharmacopeias [9,10,11,12,13,14,15,16,17].
FDA and EMA have considered the monocyte activation test (MAT) as a humane alternative method to RPT [18,19]. The assay involves incubating a diluted test sample with a source of human monocytes or human monocytoid cells. Monocytes activated by pyrogens produce cytokines/interleukins that are detected in an immunological assay. Human whole blood, peripheral blood mononuclear cells (PBMC) or monocytic cell lines, are appropriate sources of monocytes and are commercially available [20,21,22,23,24]. As MAT has higher sensitivity and accuracy than RPT, promises to replace it in the near future.
Although some interesting reviews about the RPT and the BET were previously published, to our knowledge, none of them provide an in-depth comparison of the two currently available official methods to evaluate pyrogenicity (RPT and BET). The goal of this review is to highlight the differences and similarities of each assay throughout the USP, European Pharmacopoeia (EP), Japanese Pharmacopoeia (JP) and International Pharmacopoeia (IP), taking into account the current thinking of the regulatory authorities, as well as the suggestions and recommendations of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH).
2. In Vivo Pyrogen Assay: Rabbit Pyrogen Test (RPT)
In Table 1, Table 2, Table 3 and Table 4, comparative specifications, procedures, and characteristics have been extracted from the official monographs regarding animals and good laboratory practice (GLP) conditions, temperature recording, acceptance criteria, and judgement [25,26,27,28].
Table 1.
Experimental conditions referring to animals involved in the assay.
| Experimental | IP | USP | JP | EP |
|---|---|---|---|---|
| Number | 3 | 3 | 3 | 3 |
| Condition | Healthy | Healthy | Healthy | Healthy |
| Age | Adult | Mature | Mature | Adult |
| Weight | - | - | ≥1.5 kg | ≥ 1.5kg |
| Sex | - | - | - | either |
| Variety | The same, ideally | - | - | - |
| Housing: | ||||
| temperature | uniform (±2 °C) | uniform (20–23 °C) (±3 °C) | constant = 20 °C–27 °C | uniform, appropriate |
| humidity | uniform | - | - | - |
| watering | ad libitum | - | - | - |
| feeding | usual food ad libitum | - | constant diet | complete, balanced, antibiotics free diet |
| Environs | Not exciting | Not exciting | Not exciting | Quiet |
| Individually or in group | Individually | Individually | Individually | Individually |
| Rejection reasons | ▪ Last use, in a pyrogen test, in the last 48 h ▪ T rise in the last test ≥ 0.5 °C ▪ Last use in a pyrogen-positive test in the previous 2 weeks |
▪ Last use, in a pyrogen test, in the last 48 h ▪ T rise ≥ 0.6 °C in a pyrogen test in the previous 2 weeks ▪ Last use in a pyrogen-positive test in the previous 2 weeks |
▪ Last use, in a pyrogen test, in the last 48 h ▪ Last use in a pyrogen-positive test ▪ Loss of body mass in the previous week |
▪ Loss of body mass in the previous week ▪ Last use, in a pyrogen test, in the last 3 days ▪ Last use, in a pyrogen-positive test, in the last 3 weeks ▪ Use, in a pyrogen test, where the rabbits’ temperature mean rise > 1.2 °C |
IP: International Pharmacopoeia; USP: United States Pharmacopoeia; JP: Japanese Pharmacopoeia; EP: European Pharmacopoeia.
Table 2.
Experimental conditions referring to temperature recording in the rabbit pyrogen test (RPT).
| Experimental | IP | USP | JP | EP |
|---|---|---|---|---|
| Test room | Housing area or similar separate room | Separate area designated solely for pyrogen testing | Separate room | Housing area or separate room (at least 18h of previous staying) |
| Room T | Similar to the housing T | Similar to the housing T | Similar to the housing T | Within 3 °C of the housing T |
| Instrument | Accurate thermometer or T-recording device | Accurate T-sensing device (clinical thermometer or thermistor probe) | Rectal thermometer or T-measuring apparatus | Thermometer or electrical device |
| Precision | 0.1 °C | ± 0.1 °C | ≤ ± 0.1 °C | 0.1 °C |
| Time | Sufficient to reach a maximum T | Sufficient to reach a maximum T and < 5 min | - | An electrical device may be left throughout the test. |
| Site and depth | Rectum, ≈ 6 cm | Rectum, ≥ 7.5 cm | Rectum, 6–9 cm constant | Rectum, ≈ 5 cm constant |
| Restraint | By a loosely fitting neck stock | With lightly fitting neck stock | By a loosely fitting neck stock | By a loosely fitting neck stock (at least 1h before and throughout the test) |
| Posture | Natural resting | Natural resting | Natural resting | Normal |
| Feeding | Not allowed (2h before and during test) | Not allowed | Not allowed (several hours before and during test) | Not allowed (previous overnight and during test) |
| Watering | Allowed | Allowed, may be restricted | - | Not allowed |
T: temperature; IP: International Pharmacopoeia; USP: United States Pharmacopoeia; JP: Japanese Pharmacopoeia; EP: European Pharmacopoeia.
Table 3.
RPT procedure.
| Experimental | IP | USP | JP | EP |
|---|---|---|---|---|
| Pretraining for rabbits not previously used | Same test omitting the injection, 1–3 days before | Same test omitting the injection, not more than 7 days before; for rabbits never used before | Same test omitting the injection, 1–3 days before | Same test injecting pyrogen-free 9 g/L solution of sodium chloride R, 1–3 days before. Non-use period = 2 weeks |
| Pre-injection conditioning time | ≥ 1 h | - | ≥ 48 h | 18 h |
| Control T (CT) | Mean of two T readings (T1, T2) at an interval of 30 min in the 40 min preceding the injection | Taken no more than 30 min prior to the injection | Mean of two T readings (T1, T2) at an interval of 30 min in the 40 min preceding the injection | Mean of two T readings (T1, T2) at an interval of 30 min in the 40 min preceding the injection |
| Rabbit selection criteria | ▪ ΔCT among rabbits ≤ 1.0 °C ▪ T1-T2 ≤ mean ± 0.2 °C ▪ 38 °C ≤ CT ≤ 39.8 °C |
▪ ΔCT among rabbits ≤ 1.0 °C ▪ CT < 39.8 °C |
▪ T1-T2 ≤ ± 0.2 °C ▪ CT ≤ 39.8 °C |
▪ ΔT ≤ 0.6 °C in the pretraining ▪ T1-T2 ≤ ± 0.2 °C ▪ 38 °C ≤ CT ≤ 39.8 °C ▪ ΔCT among rabbits ≤ 1.0 °C |
| Syringe, needle and glassware | Free of pyrogens by any suitable method (250 °C, 30 min) |
Free of pyrogens by any suitable method (250 °C, 30 min) |
Free of pyrogens | Thorough wash and heating in a hot-air oven (250 °C, 30 min or 200 °C, 1h) |
| Test material | Solution of the substance being examined | Either the product or the product treated as directed in the monograph | Solution of the substance being examined. When hypotonic, may be made isotonic. | Sterile solution of the substance being examined |
| Tested product amount | As specified in the monograph | As prescribed in the monograph | - | As prescribed in the monograph |
| Volume injected | 10 mL/kg (or as specified in the monograph) | 10 mL/kg (or as specified in the monograph) | 10 mL/kg (or as specified in the monograph) | 0.5 mL/kg–10 mL/kg |
| Test solution T | ≈ 38 °C | 37 °C ± 2 °C | 37 °C ± 2 °C | ≈ 38 °C |
| Injection site | Marginal vein of the ear | Ear vein | Marginal vein of the ear | Marginal vein of the ear |
| Injecting time | ≤ 4 min (or as specified in the monograph) | ≤ 10 min | ≤ 10 min | ≤ 4 min (or as specified in the monograph) |
| Measurement period, after injection | 3 h | 3 h | 3 h | 3 h |
| Measurement frequency | Continuously or every 30 min | Every 30 min between 1 and 3 h subsequent to the injection | ≤ 30 min | ≤ 30 min (starting at least 90 min before the injection) |
| Rabbit T rise (TR) = response | ▪ TR = Tmax − CT ▪ TR = 0 when Tmax < CT (Tmax = maximum T recorded after injection/rabbit) |
▪ TR = T − CT ▪ TR = 0 when T < CT (T = any T recorded after injection/rabbit) |
▪ TR = Tmax − CT ▪ TR = 0 when Tmax < CT (Tmax = maximum T recorded after injection/rabbit) |
▪ TR = Tmax − CT ▪ TR = 0 when Tmax < CT (Tmax = maximum T recorded after injection/rabbit) |
T: temperature; IP: International Pharmacopoeia; USP: United States Pharmacopoeia; JP: Japanese Pharmacopoeia; EP: European Pharmacopoeia
Table 4.
RPT acceptance criteria and judgement.
| Experimental | IP | USP | JP | EP |
|---|---|---|---|---|
| Number of rabbits extra-groups | 1 | 1 | Up to 2 | Up to 3 |
| Number of rabbits per extra-group | 5 | 5 | 3 | 3 |
| Case 1 and judgment | ▪ No individual TR ≥ 0.6 °C and Σ TR ≤ 1.4 °C ▪ Absence of pyrogens |
▪ No individual TR ≥ 0.5 °C ▪ Absence of pyrogens |
▪ Σ TR ≤ 1.3 °C ▪ Pyrogen-negative |
▪ Σ TR (n = 3, 6, 9 or 12) ≤ 1.15, 2.80, 4.45 or 6.60 (°C) respectively ▪ Product passes |
| Case 2 and judgment | ▪ 1 or 2 individual TR ≥ 0.6 °C or Σ TR (n = 3) > 1.4 °C ▪ Test 5 other rabbits |
▪ Any individual TR ≥ 0.5 °C ▪ Test 5 other rabbits |
▪ Σ TR > 2.5 °C ▪ Pyrogen-positive |
▪ Σ TR (n = 3, 6, 9 or 12) > 2.65, 4.30, 5.95 or 6.60 (°C) respectively ▪ Product fails |
| Case 3 and judgment | ▪ Not more than 3 of the TR (n = 8) ≥ 0.6 °C and Σ TR (n = 8) ≤ 3.7 °C ▪ Absence of pyrogens |
▪ Not more than 3 of the TR (n = 8) ≥ 0.5 °C and Σ TR (n = 8) ≤ 3.3 °C ▪ Absence of pyrogens |
▪ 1.3 °C < Σ TR < 2.5 °C ▪ Test 3 other rabbits |
▪ Σ TR does not meet neither case 1 nor case 2 ▪ Test 3 other rabbits up to 12 |
| Case 4 and judgment | - | - | ▪ Σ TR (n = 6) ≤ 3.0 °C ▪ Pyrogen-negative |
- |
| Case 5 and judgment | - | - | ▪ Σ TR (n = 6) > 4.2 °C ▪ Pyrogen-positive |
- |
| Case 6 and judgment | - | - | ▪ 3.0 °C < Σ TR (n = 6) < 4.2 °C ▪ Test 3 other rabbits |
- |
| Case 7 and judgment | - | - | ▪ Σ TR (n = 9) ≤ 5.0 °C ▪ Pyrogen-negative |
- |
| Case 8 and judgment | - | - | ▪ Σ TR (n = 9) > 5.0 °C ▪ Pyrogen-positive |
- |
TR. Rabbit temperature rise; IP: International Pharmacopoeia; USP: United States Pharmacopoeia; JP: Japanese Pharmacopoeia; EP: European Pharmacopoeia.
Among the evaluated pharmacopoeias, the most significant differences related to the experimental conditions for the animals involved in the assay are housing temperature (USP and JP the most restrictive), feeding during housing (only the EP demands a diet without antibiotics), and initial rabbit rejection reasons (the IP and the EP are the most restrictive).
For the experimental conditions regarding temperature recording, the most important differences among the selected pharmacopoeias are: the depth of the temperature recorder device, the feeding and the watering. These factors can influence the obtained results significantly.
There are also important differences in the RPT procedure among the main pharmacopoeias. From our point of view, the most important ones are the pre-training, the pre-injection conditioning time and the injecting time.
Regarding the acceptance criteria and judgement, the main differences are the number of rabbits in the extra-group and above all, the acceptance criteria.
It should be noted that the USP and the EP make some remarks about the number of rabbits, the overall treatment of the rabbits, and the replacement of the rabbit pyrogen test by an “in vitro” test. In addition, the USP is the only test to give instructions for pyrogen testing of medical devices, injection assemblies and radioactive pharmaceuticals.
3. In Vitro Pyrogen Assay: Bacterial Endotoxins Test (BET)
Bacterial Endotoxins Test is completely harmonized according to the Q4B annex 14 published by the ICH in 2012 [29]. In the IP and USP there are three possible alternatives: The gel-clot technique, which is based on gel formation; the turbidimetric technique, based on the development of turbidity after cleavage of an endogenous substrate; and the chromogenic technique, based on the development of color after cleavage of a synthetic peptide-chromogen complex [30,31]. The JP outlines two detailed assays: the gel-clot techniques, which are based on gel formation by the reaction of the lysate TS with endotoxins and the photometric techniques, based on endotoxin-induced optical changes of the lysate TS. In the EP and related pharmacopoeias (The British Pharmacopoeia (BP), Real Farmacopea Española (RFE), etc.), six methods are described: Method A, or gel-clot method limit test; method B or gel-clot method quantitative test; method C, or turbidimetric kinetic method; method D or chromogenic kinetic method; method E, or chromogenic end-point method; and method F, or turbidimetric end-point method [32,33]. In all the pharmacopoeias, the gel-clot limit test should be used if there are doubts about the results of the other proposed methods.
Regarding the apparatus, reagents, test solutions and determination of maximum valid dilution (MVD), no differences between the four pharmacopoeias can be determined. Authors only find little variations between JP and the other pharmacopoeias in some specific points (Table 5 and Tables S1–S3).
Table 5.
Differences in harmonized bacterial endotoxins test (BET) between JP and IP, USP and EP.
| Experimental | IP-USP-EP | JP |
|---|---|---|
| Gel-clot techniques: valid test conditions | The lowest concentration of the standard solutions shows a (-) result | When 0.25λ of the standard solution shows a (-) result |
| Photometric quantitative techniques: requirements | ▪ Sol. C comply assurance of criteria ▪ endotoxin recovery: 50–200% ▪ Sol. D: ≤ blank value of the lysate employed or < endotoxin detection limit |
▪ |r| of sol. C: ≥ 0.980 ▪ endotoxin recovery: 50–200% ▪ Sol. D: ≤ blank value of the lysate employed or < endotoxin detection limit |
IP: International Pharmacopoeia; USP: United States Pharmacopoeia; JP: Japanese Pharmacopoeia; EP: European Pharmacopoeia.
4. Conclusions
The RPT is not harmonized between the IP and the ICH pharmacopoeias (JP, USP and EP). There are important differences in the design, procedure, temperature recording, acceptance criteria and judgement. Although the current thinking of the regulatory authorities is the transition from the in vivo test to a validated in vitro test, such as the LAL-test in accordance with 21 CFR 610.9. Nowadays, the only way for some products to demonstrate apyrogenicity during the preclinical phase is the RPT, especially if the risk assessment indicates that non-endotoxin pyrogens may be present. In Europe, the EP has an alternative test to the rabbit test. This is the monocyte activation test, a whole blood assay. Thus, pharmaceutical laboratories should consider these differences in their dossiers.
The harmonized ICH-BET, the most popular quality control endotoxin test, has as expected no significant differences across the published official monographs, and all of them may be considered interchangeable. Nevertheless, the pharmaceutical companies should demonstrate to the regulatory authorities that the selected method is acceptable and suitable for a specific material or formulation.
Acknowledgments
We thank J.E. Basterrechea for technical assistance.
Supplementary Materials
The following is available online at http://www.mdpi.com/2072-6651/10/8/331/s1, Table S1: Comparative analysis of the BET conditions between IP, USP, JP, EP and also BP and RFE, Table S2: Comparative analysis of the Gel-clot techniques between IP, USP, JP, EP and also BP and RFE, Table S3: Comparative analysis of the Photometric quantitative techniques between IP, USP, JP, EP and also BP and RFE.
Author Contributions
M.C.-D. and D.C.D conceived and designed this manuscript; V.G.-R. and E.F. collected and analyzed the pharmacopeial monographies; M.C.-D., P.J., T.G. and M.G. contributed to the critical reading of the draft manuscript; V.G.-R., E.F. and D.C.-D. wrote the paper; T.G., M.C.-D. and D.C.-D. reviewed the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Key Contribution
The bacterial endotoxin test is completely harmonized in the ICH region, but the pyrogen test shows large differences which should be considered by pharmaceutical laboratories from a regulatory point of view.
References
- 1.Sandel T. Assesing non-endotoxin microbial pyrogens in relation in pharmaceutical processing. J. GXP Compliance. 2015;19:1–12. [Google Scholar]
- 2.Tours N., Sandle T. Comparison of dry-heat depyrogenation using three different types of Gram-negative bacterial endotoxin. Eur. J. Parenter. Pharm. Sci. 2008;13:17–20. [Google Scholar]
- 3.Ensor D.S., Foarde K.K. The behavior of particles in cleanrooms. In: Dixon A.M., editor. Environmental Monitoring for Cleanrooms and Controlled Environments. 1st ed. CRC Press Taylor & Francis; Boca Raton, FL, USA: 2016. pp. 1–28. [Google Scholar]
- 4.Seibert F.B. The cause of many febrile reactions following intravenous injections. I. Am. J. Physiol. 1925;71:621–651. doi: 10.1152/ajplegacy.1925.71.3.621. [DOI] [Google Scholar]
- 5.Welch H., Calvery H.D., McClosky W.T., Price C.W. Method of preparation and test for bacterial pyrogens. J. Am. Pharm. Assoc. 1943;32:65–69. doi: 10.1002/jps.3030320301. [DOI] [Google Scholar]
- 6.McClosky W.T., Price C.W., Van Winkle W.J., Welch H., Calvery H.O. Results of the first USP collaborative study of pyrogens. J. Am. Pharm. Assoc. 1943;32:69–73. doi: 10.1002/jps.3030320302. [DOI] [Google Scholar]
- 7.Levin J., Bang F.B. A description of cellular coagulation in the limulus. Bull. Johns Hopkins Hosp. 1964;115:337–345. [PubMed] [Google Scholar]
- 8.Levin J., Bang F.B. The role of endotoxin in the extracellular coagulation of limulus blood. Bull. Johns Hopkins Hosp. 1964;115:265–274. [PubMed] [Google Scholar]
- 9.Altintas Z., Abdin M.J., Tothill A.M., Karim K., Tothill I.E. Ultrasensitive detection of endotoxins using computationally designed nanoMIPs. Anal. Chem. Acta. 2016;935:239–248. doi: 10.1016/j.aca.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 10.Solano G., Gómez A., León G. Assessing endotoxins in equine-derived snake antivenoms: Comparison of the USP pyrogen test and the Limulus Amoebocyte Lysate assay (LAL) Toxicon. 2015;105:13–18. doi: 10.1016/j.toxicon.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Fingola F.F., Albertino S.R.G., Abrantes S.M.P., Zamith H.P.S. Intralaboratory validation of kinetic chromogenic Limulus amebocyte lysate assay for bacterial endotoxin determination in anti-bothropic serum. J. Pharm. Biomed. Anal. 2013;85:93–98. doi: 10.1016/j.jpba.2013.06.034. [DOI] [PubMed] [Google Scholar]
- 12.Kalita P., Chaturvedula L.M., Sritharan V., Gupta S. In vitro flow-through assay for rapid detection of endotoxin in human sera: A proof-of-concept. Nanomed. Nanotechnol. Biol. Med. 2017;13:1483–1490. doi: 10.1016/j.nano.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Mujika M., Zuzuarregui A., Sánchez-Gómez S., Martínez de Tejada G., Arana S., Pérez-Lorenzo E. Screening and selection of synthetic peptides for a novel and optimized endotoxin detection method. J. Biotechnol. 2014;186:162–168. doi: 10.1016/j.jbiotec.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 14.Caldeira da Siva C., Franca Presgrave O.A., Hartung T., Lage de Moraes A.M., Fernandes Delgado I. Applicability of the Monocyte Activation Test (MAT) for hyperimmune sera in the routine of the quality control laboratory: Comparison with the Rabbit Pyrogen Test (RPT) Toxicol. Vitr. 2016;32:70–75. doi: 10.1016/j.tiv.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Reich J., Lang P., Grallert H., Motschmann H. Masking of endotoxin in surfactant samples: Effects on Limulus-based detection systems. Biologicals. 2016;44:417–422. doi: 10.1016/j.biologicals.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Bolden J., Knight M., Stockman S., Omokoko B. Results of a harmonized endotoxin recovery study protocol evaluation by 14 BioPhorum Operations Group (BPOG) member companies. Biologicals. 2017;48:74–81. doi: 10.1016/j.biologicals.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Jin Y., Jia J., Li C., Xue J., Sun J., Wang K., Gan Y., Xu J., Shi Y., Liang X. LAL test and RPT for endotoxin detection of CPT-11/DSPE-mPEG2000 nanoformulation: What if traditional methods are not applicable? Asian J. Pharm. Sci. 2018 doi: 10.1016/j.ajps.2017.11.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Pharmacopeia 9.0. 9th ed. Council of Europe; Strasbourg, France: 2017. 2.6.30. Monocyte Activation Test; pp. 193–194. [Google Scholar]
- 19.U.S. Food and Drug Administration; 2012. [(accessed on 3 August 2018)]. Guidance for Industry Pyrogen and Endotoxins Testing: Questions and Answers. Available online: www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm. [Google Scholar]
- 20.Hartung T., Wendel A. Detection of Pyrogens using human whole blood. Altex. 1995;12:70–75. [PubMed] [Google Scholar]
- 21.Schindler S., von Aulock S., Daneshian M., Hartung T. Development, validation and applications of the monocyte activation test for pyrogens based on human whole blood. Altex. 2009;26:265–277. doi: 10.14573/altex.2009.4.265. [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann S., Peterbauer A., Schindler S., Fennrich S., Poole S., Mistry Y., Montag-Lessing T., Spreitzer I., Löschner B., Van Aalderen M., et al. International validation of novel pyrogen tests based on human monocytoid cells. J. Immunol. Methods. 2005;298:161–173. doi: 10.1016/j.jim.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 23.De Mattos K.A., Navega E.C.A., Silva V.F., Almeida A.S., Da Silva C.C., Presgrave O.A.F., Junior D.D.S.G., Delgado I.F. Applicability of the monocyte activation test (MAT) in the quality control of the 17DD yellow fever vaccine. Altern. Lab. Anim. 2018;46:23–37. doi: 10.1177/026119291804600107. [DOI] [PubMed] [Google Scholar]
- 24.Nordgren I.K. Leukoreduction system chambers provide a valuable source of functional monocytes for the monocyte activation test by comparison with internationally validated methods. J. Immunol. Methods. 2016;428:42–49. doi: 10.1016/j.jim.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Pharmacopeia 41. United States Pharmacopeial Convention, Inc.; Rockville, MD, USA: 2018. <151> Pyrogen Test; pp. 6083–6085. [Google Scholar]
- 26.European Pharmacopeia 9.0. 9th ed. Council of Europe; Strasbourg, France: 2017. 2.6.8. Pyrogens; pp. 193–194. [Google Scholar]
- 27.The Japanese Pharmacopoeia. 17th ed. The Ministry of Health, Labour and Welfare; Tokyo, Japan: 2016. [(accessed on 23 May 2018)]. 4.04 Pyrogen Test; pp. 120–194. Available online: www.pmda.go.jp/english. [Google Scholar]
- 28.The International Pharmacopoeia. 7th ed. WHO Department of Essential Medicines and Health Products; Geneva, Switzerland: 2017. [(accessed on 21 May 2018)]. 3.4 Test for bacterial endotoxins. Available online: www.who.int/phint/ [Google Scholar]
- 29.International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use; 2012. [(accessed on 30 May 2018)]. Evaluation and Recommendation of Pharmacopoeial Texts for Use in the ICH Regions on Bacterial Endotoxins Test. General Chapter. Q4b Annex 14. Available online: www.ich.org. [Google Scholar]
- 30.The International Pharmacopoeia. 7th ed. WHO Department of Essential Medicines and Health Products; Geneva, Switzerland: 2017. [(accessed on 21 May 2018)]. 3.5 Test for pyrogens. Available online: www.who.int/phint/ [Google Scholar]
- 31.U.S. Pharmacopeia 41. United States Pharmacopeial Convention, Inc.; Rockville, MD, USA: 2018. <85> Bacterial Endotoxins Test; pp. 6011–6017. [Google Scholar]
- 32.the Japanese Pharmacopoeia. 17th ed. The Ministry of Health, Labour and Welfare; Tokyo, Japan: 2016. [(accessed on 23 May 2018)]. 4.01 Bacterial Endotoxins Test; pp. 110–114. Available online: www.pmda.go.jp/english. [Google Scholar]
- 33.European Pharmacopeia 9.0. 9th ed. Council of Europe; Strasbourg, France: 2017. 2.6.14. Bacterial Endotoxins; pp. 204–207. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.