Abstract
Introduction
Soldiers are at risk for acute and chronic pain due to the mental and physical challenges of military duties and ongoing training for force readiness. With the burden of pain on any individual attributable across pain sources, a broad perspective that goes beyond prior characterizations of pain is important. We aim to further the understanding of pain’s effects among non-deployed active duty soldiers and the Military Health System (MHS), by describing prevalence of 10 painful conditions, reported pain levels, duration of pain and impact of pain on military duty limitations.
Methods
Data are from the MHS Data Repository including outpatient MHS direct care encounters, claims for outpatient purchased care from civilian providers, and vital records, for all soldiers continuously enrolled in TRICARE and not deployed in FY 2012. Ten pain-related diagnostic categories were conceptually derived for this analysis and identified using ICD-9-CM diagnostic codes. We report the FY 2012 prevalence at the soldier-level (N = 297,120) for each pain category as a primary diagnosis, as well as in any diagnostic position, and at the soldier-level for reported pain level, duration, and military duty limitations. Institutional Review Board approval was obtained prior to analyses.
Results
Overall, 63% of soldiers had at least one pain diagnosis and 59% had a primary pain diagnosis during FY 2012. Back and neck pain (22%), non-traumatic joint disorders (28%), and other musculoskeletal pain (30%) were the most frequent categories for primary diagnosis. Nearly two-thirds of soldiers had a primary pain diagnosis in more than one category, and 23% in four or more categories. Moderate or severe pain levels were reported at least once during the year by 55% of soldiers who had a primary pain diagnosis. In the subsample of soldiers with primary pain in the first quarter, duration and chronicity of pain diagnoses varied by pain category: the back and neck pain category was the most common for both persistent pain occurring in each quarter of FY 2012 (23%) and chronic pain lasting for at least 3 mo (62%). In most pain categories, the majority of soldiers were released without duty limitations.
Conclusion
These data provide a deeper understanding of pain diagnoses and burden of pain among active duty soldiers. A substantial proportion of soldiers with pain diagnoses were seen for pain self-reported as only mild, or that did not result in significant restrictions in military duty limitations. However, given the prevalence of multiple pain diagnoses and common reports of moderate or severe pain and long duration, complex interventions may be required to minimize the effect of pain on force readiness. This encounters-based analysis is likely an underestimate of presence of pain, and does not include contextual factors that could better describe the true effect of pain among this population.
Keywords: pain, military, duration, work limitations
INTRODUCTION
Chronic pain is a significant burden to individuals and the health system as it is often accompanied by significant physical, emotional and social symptoms.1–3 It is frequently associated with depression,2,4 anxiety,2,4 substance use disorders,5,6 and post-traumatic stress disorder (PTSD).7,8 Severe chronic pain has also been linked to increased mortality.9 Further, individuals with chronic pain report reduced quality of life.3,10 Service members are at particular risk for acute and chronic pain due to the mental and physical challenges of military duties and ongoing training for force readiness11–14 and/or injuries associated with a prior deployment.15,16 Sub-acute pain may go untreated as service members “tough it out,” increasing the opportunity for pain to become chronic.17 From 1997 to 2011, joint and back pain have increased three- to four-fold among active duty service members, with 45% reporting joint pain and 60% reporting back pain in 2011.11 The experience of pain among service members may differ significantly from that of civilians, because of high rates of traumatic brain injury (TBI), PTSD and polytrauma, compounded by other psychological distress which may increase the complexity of pain and pain management.8,18–20
The Department of Defense/Veterans Health Affairs (DoD/VHA) Pain Management Task Force Final Report emphasized a holistic, multidisciplinary and multimodal approach to its pain management strategy.17 The Institute of Medicine, in its seminal report Treating Pain in America, also identified pain as a public health challenge that requires a population health perspective;3 this approach was re-emphasized in the National Pain Strategy.21 A population approach differs from the clinical literature which typically focuses on one source of pain (e.g., headache, back pain) or specific population (e.g., women,22 Veterans with polytrauma20,23). The burden of pain on any individual or health system is additive across pain sources, although the specific impact may vary by specific diagnosis. Thus, a population approach allows a broader understanding of the burden of pain on soldiers and the Military Health System (MHS). This may allow the MHS to better focus prevention and treatment efforts.21
In this paper, we identify the prevalence of diagnoses in 10 major pain categories among active duty non-deployed soldiers, and examine measures of burden of pain, including self-reported pain levels, military duty limitations, and duration of pain. Understanding this broad picture of pain in this sample is an essential step in addressing the needs of soldiers with pain as well as the readiness of the Army.
METHODS
Analytic Sample and Data Sources
Data are from all Army active duty soldiers who were continuously enrolled in TRICARE and not deployed for any portion of FY 2012 (N = 297,120). Data sources included deployment information from the Contingency Tracking System; demographic and military characteristics from the Defense Enrollment Eligibility Reporting System; outpatient medical record diagnoses and encounters from the MHS Data Repository (MDR), including “purchased care” in civilian settings that accept TRICARE insurance; pain severity ratings from the Clinical Data Repository vitals file; and a measure of military duty limitations associated with direct care encounters in the MDR.
Measures
Pain categories were assessed based on the presence of ICD-9-CM diagnosis codes, in any position, for outpatient encounters. We created a detailed taxonomy of pain diagnoses, drawing from a comprehensive review of military, Veterans Administration (VA) and pain literature, as described below. Expert consultants representing internal medicine and pain specialties reviewed the taxonomy, which was then refined. Starting with the American Pain Society’s Pain Taxonomy,24 which included four major categories focused on pathological mechanism, we created subcategories that reflected both civilian and military literature (e.g., osteoarthritis,20,25 other musculoskeletal,19,26,27 visceral/pelvic,26 and wounds/injury20).
The 10 major pain categories examined in this analysis are: peripheral/central nervous system; osteoarthritis; back and neck; headache/migraine; non-traumatic joint disorders; other musculoskeletal; visceral/pelvic; wounds/injury/fractures; acute pain; and chronic pain from an undefined source. For the back and neck pain category, we created five not mutually-exclusive subcategories: lumbago; intervertebral disc; cervicalgia; spondylosis; and other; these reflected major diagnostic categories, and are reported for prevalence purposes only. We disregarded cancer pain and other disease-specific categories (e.g., sickle-cell) not expected to be common.
We defined each pain category based on presence of ICD-9-CM diagnosis codes, using a health services research diagnostic code grouper system (Clinical Classifications Software (CCS)28) and prior research on Veteran and military populations. First, if a CCS code or a unique ICD-9-CM diagnostic code existed for that category (e.g., osteoarthritis), we relied on those codes. Second, in the absence of a unique CCS or ICD-9-CM code, for categories that included multiple types of diagnoses (e.g., back and neck pain), we relied on a VA Office of the Inspector General Report29,30 for specific diagnosis codes. Last, we supplemented specific pain categories with diagnosis codes found in military-specific literature. The final set of diagnostic codes is available as a supplemental document. For each pain category, we identified the presence of at least one eligible diagnosis code for each soldier in the analytic timeframe (FY 2012), in any diagnosis position and as the primary diagnosis. We report most results based on the primary pain diagnosis. We also counted the number of different pain categories per soldier.
Pain levels were obtained from vital records for encounters in military treatment facilities and based on soldier self-report on a numerical scale (0–10) administered by clinicians during medical encounters. We constructed an ordinal variable to reflect highest pain level31 across encounters for each primary pain diagnosis during FY 2012: no pain (0) or mild (1–3) pain, moderate (4–6), and severe (7–10). Not reported or missing pain level was coded for 16.3% of soldiers with encounters for pain diagnoses in purchased care settings where vital records are not used.32
Military duty limitations were based on dispositions assigned by clinicians at selected outpatient medical encounters in military treatment facilities and are a marker of the impact of pain on functioning. The most restricted limitation for a primary pain diagnosis encounter in FY 2012 was coded as: released without limitations; released with work duty limitations; sick at home or quarters; immediate referral; or other (left against medical advice, admitted). Military duty limitations were not recorded in purchased care settings.
Duration was coded as either once only, intermittent, or persistent. Persistent duration was defined as an encounter with the primary pain diagnosis at least once in each quarter for the full 1-yr period of FY 2012; intermittent was defined as more than one primary pain diagnosis over FY 2012, but not persistent. Chronic pain was defined as more than one encounter with the same primary pain category in FY 2012 at least 3 mo apart.33,34 Duration and chronicity were analyzed only for the subsample of soldiers with a primary pain diagnosis in the first quarter of FY 2012 (n = 87,650) in order to track additional diagnoses for three quarters following a diagnosis.
Statistical Analysis
We report the annual prevalence of each pain category as both a primary pain diagnosis (restricted to the first diagnostic position), as well as in any diagnostic position, and associate pain category with measures of pain. Severity, duration, and chronicity, and military duty limitations are reported only for primary pain diagnoses. Data are reported at the soldier-level. To assess whether pain category was associated with duration and chronicity of pain, we restricted analyses to the subsample that had a pain encounter in the first quarter.
For each pair of pain categories, t-tests were conducted to compare the following proportions: (1) severe pain, (2) persistent pain, (3) chronic pain, (4) release from work with duty limitations, and (5) sick at home or in quarters. Separate analytic files were created to compare these outcomes between the members belonging to each pair of pain categories. Each t-test utilized Levene’s test to determine equality of variances and Bonferroni’s correction to adjust for multiple comparisons. Except as noted in the footnote on tables, all comparisons were statistically significant at p < 0.05. All calculations were performed using SPSS version 19.0.0.
Brandeis University’s Institutional Review Board and the Human Research Protection Program at the Office of the Assistant Secretary of Defense for Health Affairs/Defense Health Agency conducted the human subjects review and approved the study. The Defense Health Agency’s Privacy and Civil Liberties Office executed the data use agreements.
RESULTS
The analytic sample of all non-deployed active duty soldiers in FY 2012 (N = 297,120) was predominantly male (86.6%) and younger in age (26.8% aged 17–24 and 42.6% aged 25–34) [data not shown]. Sixty percent were white (59.9%), 20.4% black, and 11.2% Hispanic. Over half were junior enlisted with a paygrade of E1–E4 (53.7%); nearly 20% were officers. Almost two-thirds had a deployment before FY 2012 (64.4%).
Prevalence of Pain Category Diagnoses
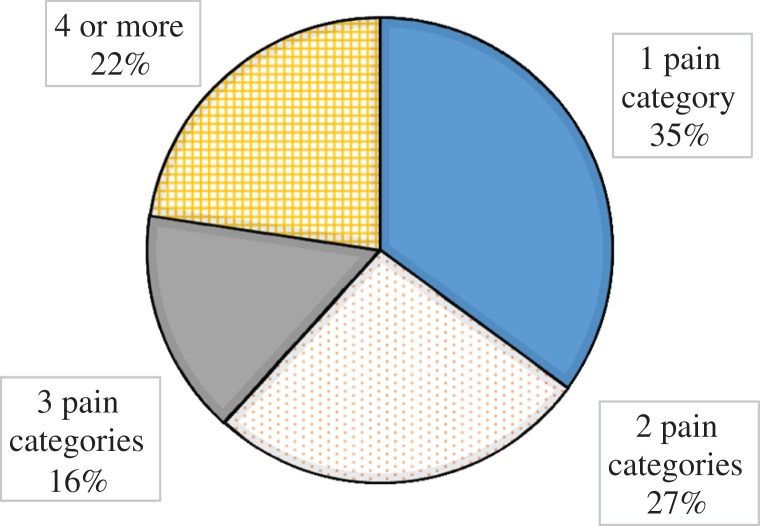
Among the 297,120 soldiers included in the analysis, 63.3% had any pain diagnosis during FY 2012 and 59.2% had a primary pain diagnosis (Table I). Thus, most soldiers with any pain diagnosis during FY 2012 had pain coded as the primary reason for at least one medical visit during the year. The most common primary pain diagnoses among soldiers were other musculoskeletal (29.5%), non-traumatic joint disorders (28.1%), and back and neck pain (22.4%). Figure 1 shows that, of soldiers who had a primary pain diagnosis, almost two-thirds had a diagnosis in more than one category and more than one in five had primary pain diagnoses in four or more pain categories.
Table I.
Distribution of Types of Pain Diagnoses, Army Active Duty Soldiers (Non-Deployed), FY2012
| Soldiers (N = 297,120)a | ||||
|---|---|---|---|---|
| Any Diagnosis | Primary Diagnosis | |||
| N | % | N | % | |
| Any pain diagnosis | 188,037 | 63.3 | 175,753 | 59.2 |
| Pain categoriesb | ||||
| Peripheral/Central nervous system | 8,535 | 2.9 | 5,889 | 2.0 |
| Osteoarthritis | 11,398 | 3.8 | 7,661 | 2.6 |
| Back and neck pain (any type)c | 79,050 | 26.6 | 66,407 | 22.4 |
| Back – lumbago | 54,585 | 18.4 | 43,243 | 14.6 |
| Back and neck – intervertebral disc | 21,472 | 7.2 | 17,674 | 5.9 |
| Back and neck – cervicalgia | 17,851 | 6.0 | 12,159 | 4.1 |
| Back and neck – spondylosis | 9,859 | 3.3 | 6,844 | 2.3 |
| Back and neck – other | 41,956 | 14.1 | 31,056 | 10.5 |
| Headache/migraine | 31,694 | 10.7 | 21,152 | 7.1 |
| Non-traumatic joint disorders | 100,669 | 33.9 | 83,614 | 28.1 |
| Other musculoskeletal | 102,609 | 34.5 | 87,759 | 29.5 |
| Visceral/pelvic | 27,991 | 9.4 | 22,259 | 7.5 |
| Wounds/injury/fractures | 26,657 | 9.0 | 23,926 | 8.1 |
| Acute | 6,315 | 2.1 | 4,085 | 1.4 |
| Chronic non-specific | 14,317 | 4.8 | 7,634 | 2.6 |
aAll soldiers with 12-mo continuous TRICARE enrollment in 2012, whether or not they have encounters.
bCategories are not mutually exclusive.
cBack and neck pain (any type) is coded if any of the subcategories are yes. Subcategories are not mutually exclusive.
FIGURE 1.
Count of different primary diagnosis pain categories, Army active duty soldiers (non-deployed), FY2012.
Highest Pain Level
Among all soldiers with a primary pain diagnosis in FY 2012, over half had moderate (28.2%) or severe pain (26.6%), recorded as the highest pain level on a medical encounter (Table II). Just over a quarter of soldiers with a primary pain diagnosis had only encounters with no pain rating, consistent with the volume of care provided in the purchased care setting. For most primary pain categories, 60–70% of soldiers reported moderate or severe pain as the highest pain level on a medical encounter. A higher proportion of soldiers with chronic, non-specific pain had a moderate or severe pain level (83.2%). In contrast, a lower proportion of those in the wounds/injury/fracture category had a moderate or severe pain level (54.5%). Severe pain was most common for diagnoses of chronic, non-specific pain (54.4%), headache/migraine (42.5%), peripheral/central nervous system (37.8%), and back and neck pain (37.2%).
Table II.
Reported Pain Level by Types of Primary Pain Diagnoses, Army Active Duty Soldiers (Non-Deployed), FY2012
| Soldiers with a Primary Pain Diagnosis (N = 175,753) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Highest Pain Level for Primary Diagnosisa,b,c | |||||||||
| Total | No/Mild (0, 1–3) | Moderate (4–6) | Severe (7–10)d | Missing/ Not Reported | |||||
| N | N | % | N | % | N | % | N | % | |
| Anyprimary pain diagnosis | 175,173 | 33,478 | 19.0 | 49,505 | 28.2 | 46,787 | 26.6 | 45,983 | 26.2 |
| Pain categoriese | |||||||||
| Peripheral/CNS | 5,889 | 991 | 16.8 | 1,811 | 30.8 | 2,224 | 37.8 | 863 | 14.7 |
| Osteoarthritis | 7,661 | 1,252 | 16.3 | 2,445 | 31.9 | 2,674 | 34.9 | 1,290 | 16.8 |
| Back and neck pain (any type) | 66,407 | 9,209 | 13.9 | 20,521 | 30.9 | 24,691 | 37.2 | 11,986 | 18.0 |
| Headache/migraine | 21,152 | 3,318 | 15.7 | 5,725 | 27.1 | 8,985 | 42.5 | 3,124 | 14.8 |
| Non-traumatic joint disorders | 83,614 | 16,189 | 19.4 | 26,071 | 31.2 | 24,699 | 29.5 | 16,655 | 19.9 |
| Other musculoskeletal | 87,759 | 15,230 | 17.4 | 26,590 | 30.3 | 27,349 | 31.2 | 18,590 | 21.2 |
| Visceral/pelvic | 22,259 | 3,748 | 16.8 | 5,918 | 26.6 | 7,682 | 34.5 | 4,911 | 22.1 |
| Wounds/injury/fracture | 23,926 | 4,360 | 18.2 | 6,264 | 26.2 | 6,764 | 28.3 | 6,538 | 27.3 |
| Chronic non-specific | 7,634 | 627 | 8.2 | 2,200 | 28.8 | 4,155 | 54.4 | 652 | 8.5 |
Subsample of 297,120 Army active duty soldiers (non-deployed), continuously enrolled in TRICARE in FY2012
aPain level ratings are on a 0–10 scale: 0 = no pain, 1–3 = mild, 4–6 = moderate 7–10 = severe.
bHighest pain level among all encounters (by soldier) with primary diagnosis for each pain category.
cPain level was only captured during encounters in the military’s direct care setting, and therefore was coded as missing for the 16.3% of outpatient encounters that were in purchased care settings.
dT-tests with Levene’s test to determine equality of variances and Bonferroni’s correction to adjust for multiple comparisons were utilized to test for associations of severe pain between types of pain categories. All pairwise tests were significant at p < 0.05, with the exception of peripheral/CNS-back/neck (p = ns) and visceral/pelvic-osteoarthritis (p = ns).
eCategories are not mutually exclusive.
Military Duty Limitations
For military treatment encounters, a substantial proportion of soldiers had some military work restrictions associated with their primary pain diagnoses and the proportion varied by pain category (Table III). However, 45–62% of soldiers were released with no military duty limitations. Return to work with some duty limitation was most common for non-traumatic joint disorders (43.6%), other musculoskeletal pain (39.0%), and back and neck pain (35.3%). Assigned to home or in quarters was highest among soldiers with headache/migraine (15.8%) and visceral/pelvic pain (10.5%).
Table III.
Disposition on Selected Encounters with Primary Pain Diagnoses, Army Active Duty Soldiers (non-deployed), FY2012
| Soldiers with a Primary Pain Diagnosis (N = 175,753) | |||||||
|---|---|---|---|---|---|---|---|
| Outpatient Military Encounter Dispositiona | |||||||
| N | Released No Limitations | Released Work Duty Limitsd | Sick at Home or in Quartersd | Immediate Referral | Otherb | Missing | |
| % | % | % | % | % | % | ||
| Pain categoriesc | |||||||
| Peripheral/CNS | 5,889 | 53.6 | 23.3 | 1.7 | 0.5 | 0.1 | 20.8 |
| Osteoarthritis | 7,661 | 44.7 | 30.9 | 1.4 | 0.2 | 0.0 | 22.8 |
| Back and neck pain (any type) | 66,407 | 49.0 | 35.3 | 6.7 | 1.0 | 0.1 | 7.9 |
| Headache/migraine | 21,152 | 61.5 | 10.0 | 15.8 | 1.8 | 0.3 | 10.4 |
| Non-traumatic joint disorders | 83,614 | 45.7 | 43.6 | 1.7 | 0.8 | 0.1 | 8.0 |
| Other musculoskeletal | 87,759 | 46.1 | 39.0 | 3.6 | 0.9 | 0.1 | 10.3 |
| Visceral/pelvic | 22,259 | 54.0 | 12.0 | 10.5 | 3.8 | 1.3 | 18.5 |
| Chronic non-specific | 7,634 | 54.0 | 25.1 | 2.9 | 0.5 | 0.2 | 17.2 |
aHighest disposition among all encounters (by soldier) with primary diagnosis for each pain category. Military duty limitations were only captured in the direct care setting, and thus was coded as missing for the 16.3% of outpatient encounters that were in purchased care settings.
bOther: left AMA, admitted, expired.
cCategories are not mutually exclusive.
dT-tests with Levene’s test to determine equality of variances and Bonferroni’s correction to adjust for multiple comparisons were utilized to test for associations of work duty limitations and sick at home/quarters between types of pain categories. All pairwise tests were significant at p < 0.05, with the exception of osteoarthritis-other musculoskeletal (p = ns).
Duration and Chronicity
We examined the duration of pain among a subsample of soldiers with a primary pain diagnosis in the first quarter (Table IV). Intermittent pain characterized the majority of soldiers, defined as repeat encounters for each pain category but not in each quarter. For each pain category, a substantial proportion had only one encounter (Table IV). Persistent pain, defined as at least one encounter in each quarter for a primary diagnosis in the same pain category, was infrequent overall except for back and neck pain (23.3%). Chronic pain, defined as receiving at least 2 primary pain diagnoses at least 3 mo apart, varied by pain category, with the highest occurrence among back and neck pain (61.8%) and the lowest occurrence among visceral/pelvic pain (28.1%).
Table IV.
Duration and Chronicity of Pain Diagnoses, Army Active Duty Soldiers (Non-Deployed), FY2012
| Soldiers with a Primary Pain Diagnosis (N = 175,753) | Soldiers with a Primary Pain Diagnosis 1st Quarter of FY2012 (N = 87,650) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Durationa | Chronicityb | |||||||||
| Total | Total | Once only | Intermittent | Persistentd | Chronicd | |||||
| N | N | N | % | N | % | N | % | N | % | |
| Pain categoriesc | ||||||||||
| Peripheral/CNS | 5,889 | 4,182 | 1,875 | 44.8 | 2,100 | 50.2 | 207 | 4.9 | 1,322 | 31.6 |
| Osteoarthritis | 7,661 | 5,385 | 2,389 | 44.4 | 2,779 | 51.6 | 217 | 4.0 | 1,930 | 35.8 |
| Back and neck pain (any type) | 66,407 | 39,914 | 8,910 | 22.3 | 21,697 | 54.4 | 9,307 | 23.3 | 24,668 | 61.8 |
| Headache/migraine | 21,152 | 13,604 | 5,482 | 40.3 | 6,908 | 50.8 | 1,214 | 8.9 | 5,792 | 42.6 |
| Non-traumatic joint disorders | 83,614 | 48,391 | 12,822 | 26.5 | 31,117 | 64.3 | 4,452 | 9.2 | 25,914 | 53.6 |
| Other musculoskeletal | 87,759 | 48,592 | 17,772 | 36.6 | 28,434 | 58.5 | 2,386 | 4.9 | 21,239 | 43.7 |
| Visceral/pelvic | 22,259 | 13,183 | 6,043 | 45.8 | 6,808 | 51.6 | 332 | 2.5 | 3,698 | 28.1 |
| Chronic non-specific | 7,634 | 6,118 | 2,354 | 38.5 | 3,149 | 51.5 | 615 | 10.1 | 2,760 | 45.1 |
aPersistent duration defined as an encounter with the primary pain diagnosis at least once in each quarter for a 1-yr period; intermittent defined as more than one primary pain diagnosis over a 1-yr period, but not persistent.
bChronic defined as more than one encounter with the primary pain diagnosis, at least 3 mo apart, over a 1-yr period.
cCategories are not mutually exclusive.
dT-tests with Levene’s test to determine equality of variances and Bonferroni’s correction to adjust for multiple comparisons were utilized to test for associations of persistent pain and chronic pain between types of pain categories. All pairwise tests were significant at p < 0.05, with the exception of other musculoskeletal-non-traumatic joint (p = ns) for persistent pain and peripheral/CNS-osteoarthritis for chronic pain (p = ns).
DISCUSSION
Our findings demonstrate that painful conditions are common among a non-deployed Army active duty population, during a 1-yr period, with rates for specific conditions similar to ambulatory visits reported in the DHA’s Medical Surveillance Monthly Report.27 Our analysis utilized a population health perspective to describe the burden of pain in the Army, showing that overall prevalence, severity and duration of pain are high, and pain has some effect on ability to fully participate in military work duties. The majority of soldiers (63%) had at least one outpatient encounter where the pain diagnosis was the reason for the visit and almost two-thirds of these soldiers were seen for more than one major pain category. Among soldiers treated for their pain, one in four experienced severe pain at least once during the year and chronic pain (lasting more than 3 mo) was common. Around half had a work limitation during the year, consistent with presence of moderate to severe pain.
It is notable that a substantial minority of soldiers with pain diagnoses were seen for pain self-reported as only mild or that did not require significant restrictions in work. Yet, these soldiers were still accessing medical care, perhaps an indication of ongoing pain conditions requiring occasional follow-up visits or a culture of heightened attention to pain. In addition, the proportion of these soldiers that had only one visit for pain indicates that there is good access to care for acute pain. While we did not analyze treatments received, these findings suggest that many pain problems are resolving with minimal health service interventions.
However, one in four soldiers with pain reported that it was severe during at least one encounter during the year and this was especially high among those with headache/migraine. It is also notable that nearly 4 in 10 reported pain in three or more major categories. Complex interventions may be required to minimize the impact of pain on the force readiness of the Army, including complementary and integrative health approaches that assist soldiers to cope with pain and to remain physically active. Further, it is essential to consider and address the factors that contribute to the often preventable transition from acute to chronic pain.35 Guidelines for treatment of pain recommend a comprehensive approach,36–39 which often incorporates education as well as a range of approaches such as physical therapy, exercise, stress management, cognitive behavioral therapy, pharmacology, and other non-pharmacologic approaches (e.g., acupuncture, meditation).3,40
The DoD has established the Stepped Care Model of Pain Management41 program, recognizing that military members are performing their duties in the presence of episodic and chronic pain. A cornerstone of the stepped care model is a comprehensive assessment of the impact of pain on functioning. DoD has developed and validated the Defense and Veterans Pain Rating Scale (DVPRS) to improve assessment of pain intensity and communication during transitions of care, and has begun to implement the Pain Assessment Screening Tool and Outcomes Registry (PASTOR).41–43 The DoD uses the medical home approach as the first step in approaching comprehensive pain management managed by the primary care provider. If needed, service members with more complex pain are treated within the medical home by teams that include primary care, pain specialists, and behavioral specialists, and the most complex cases are referred to specialty pain management programs.41 With this recent focus on comprehensive, complementary and integrative health approaches to pain management, the Army has developed tools to address the needs of soldiers who have less severe needs without relying on medications.
Work limitations are one indicator of the functional effect of pain; we found that a sizeable proportion of soldiers with pain had some military duty limitations. In contrast, many soldiers had no work limitations even though the medical visit was associated with a painful condition. The nature of military culture, for example, “tough it out” or decreased willingness to seek treatment17,44 suggests that medical visits due to pain and reported pain levels are likely to underestimate the true prevalence and severity of painful conditions. It is possible that military members may focus on meeting the expectations of their work duties. Thus, they may minimize the true effects of painful conditions in order to complete their duties.44 Yet pain has wide-ranging effects beyond the mere ability to be present for duty. People who are in pain are less able to focus, respond rapidly, and be productive.3 Pain interferes with routine work and other activities.45 People with pain are likely to have emotional distress, reduced quality of life and sleep, and often anger, depression and anxiety.3,45
These findings also imply a cost to the military, given the high burden for the MHS, as well as the soldiers themselves. For those who become disabled or leave active duty with pain, the VHA is often the health care system that must absorb the associated costs.11 Further, although not studied here, chronic pain is associated with many comorbidities including TBI, PTSD, depression, and sleep disorders,20,23 as well as increased health care utilization including emergency department use.10,46,47 The DoD stepped care model and incorporation of integrative and complementary treatments would likely reduce this burden.
This study has some limitations. Our findings are restricted to pain that resulted in a health care encounter. In using claims to identify pain diagnoses, the diagnoses are not verified and we are unable to specify any underlying etiology for the pain diagnosis that was recorded. Because we examined the population with a full year in the MHS, we excluded those returning during the year from deployment or leaving for deployments. Nevertheless, two-thirds of the sample had been deployed in prior years. Our sample may include soldiers in the process of Medical Evaluation Board review, who are likely to have more painful conditions and report greater severity of pain. Further, we analyzed only outpatient encounters, and do not capture inpatient stays associated with more serious injuries or with surgery, including soldiers treated in polytrauma units. Thus, our findings do not generalize to all active duty soldiers.
Our analysis of the duration of pain was restricted to a subsample with pain in the first quarter, and should not be extrapolated to all soldiers with pain. Since some soldiers may have had pain prior to that first quarter, we may underestimate the frequency of chronic pain. The use of claims or encounter data rely on diagnoses and severity levels as reported in the medical record. If a visit is for another medical condition, the pain diagnosis may not be noted even if it is still present; alternatively, the pain diagnosis may be noted by the provider even if not of concern to the soldier at that visit. In addition, pain may be present in any given soldier, but if he or she does not seek medical care or report it when seeking medical care for other conditions, the true prevalence is greater than estimated here.
CONCLUSIONS
Pain diagnoses are common among non-deployed Army active duty soldiers and pain is frequently chronic. Musculoskeletal conditions are associated with the greatest burden on the MHS among the painful conditions examined in this study. Our findings provide support for the value of the comprehensive stepped approach to pain management given a broad burden of pain and highlight the need for health service planning to minimize the impact on military readiness. Prevention efforts are also valuable to reduce injury and re-injury rates and to promote recovery from pain. For example, Army leaders could incorporate physical activity into unit training that could serve to reduce the likelihood of injury and to aid in recovery. Future research could delve more deeply into the questions of the functional impact of pain diagnoses on military readiness using sources beyond encounter data. The patterns described here could be evaluated by soldier characteristics, such as gender or occupation, and expanded into a deployed population and across all treatment settings. A fuller picture of the burden of pain in this population would also account for the known overlaps with other conditions (e.g., TBI, PTSD, sleep disorders). This encounters-based analysis offers a step forward in understanding the burden of pain across 10 major conditions, but is likely an underestimate of the prevalence of pain, and does not include contextual factors that would offer a more complete understanding of the true effect of pain diagnoses in this population.
Supplementary Material
Acknowledgements
We acknowledge Richard Gromadzki, D.Sc., of AXIOM Resource Management, Inc. for compiling the data files used in these analyses and Andrea Linton, M.S., of AXIOM Resource Management for conducting the data analyses; William Becker, M.D., of Yale University School of Medicine and Mark Bauer, M.D., for clinical consultation; and Alex H.S. Harris, Ph.D. of the VA Palo Alto Health Care System. LTC Thomas V. Williams MS USA (RET) formerly of the Department of Defense’s (DoD) Defense Health Agency (DHA) was the data sponsor. The DHA’s Privacy and Civil Liberties Office provided access to DoD data.
Presentation
A preliminary version of this paper was presented at the American Pain Society 35th Annual Scientific Meeting, Austin, TX, May 2016.
Funding
This study was funded by the National Center for Complementary and Integrative Health (NCCIH; R01 AT008404).
References
- 1. Veterans Health Administration : Chronic Pain Primer. 2017; Available at https://www.va.gov/painmanagement/chronic_pain_primer.asp; accessed April 7, 2017.
- 2. Von Korff M, Dworkin SF, Le Resche L, Kruger A: An epidemiologic comparison of pain complaints. Pain 1988; 32(2): 173–83. [DOI] [PubMed] [Google Scholar]
- 3. IOM (Institute of Medicine) : Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, D.C., National Academies Press, 2011. [PubMed] [Google Scholar]
- 4. McWilliams LA, Cox BJ, Enns MW: Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain 2003; 106(1–2): 127–33. [DOI] [PubMed] [Google Scholar]
- 5. Larson MJ, Paasche-Orlow M, Cheng DM, Lloyd-Travaglini C, Saitz R, Samet JH: Persistent pain is associated with substance use after detoxification: a prospective cohort analysis. Addiction 2007; 102(5): 752–60. [DOI] [PubMed] [Google Scholar]
- 6. Gallagher RM, Koob G, Popescu A: The pathophysiology of chronic pain and clinical interfaces with addiction In: Principles of Addiction Medicine, Ed 5, pp. 1435–56. Edited by Ries RK, Fiellin DA, Miller SC, Saitz R. Chevy Chase, MD, American Society of Addiction Medicine, 2014. [Google Scholar]
- 7. Villano CL, Rosenblum A, Magura S, Fong C, Cleland C, Betzler TF: Prevalence and correlates of posttraumatic stress disorder and chronic severe pain in psychiatric outpatients. J Rehabil Res Dev 2007; 44(2): 167–78. Available at http://www.rehab.research.va.gov/jour/07/44/2/Villano.html; accessed July 14, 2017. [DOI] [PubMed] [Google Scholar]
- 8. Otis JD, Gregor K, Hardway C, Morrison J, Scioli E, Sanderson K: An examination of the co-morbidity between chronic pain and posttraumatic stress disorder on U.S. Veterans. Psychol Serv 2010; 7(3): 126–35. [Google Scholar]
- 9. Torrance N, Elliott AM, Lee AJ, Smith BH: Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain 2010; 14(4): 380–6. [DOI] [PubMed] [Google Scholar]
- 10. Kerns RD, Otis J, Rosenberg R, Reid MC: Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev 2003; 40(5): 371–9. Available at http://www.rehab.research.va.gov/jour/03/40/5/Kerns.html; accessed July 14, 2017. [DOI] [PubMed] [Google Scholar]
- 11. McGeary CA, McGeary DD: New trends of musculosketetal disorders in the military In: Handbook of Musculosketetal Pain and Disability Disorders in the Military, Handbooks in Health, Work, and Disability, pp 143–58. Edited by Gatchel RJ, Schulz IZ. New York, Springer Science+Business Media, 2014. [Google Scholar]
- 12. Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ: The incidence of low back pain in active duty United States military service members. Spine 2011; 36(18): 1492–1500. [DOI] [PubMed] [Google Scholar]
- 13. Cohen SP, Griffith S, Larkin TM, Villena F, Larkin R: Presentation, diagnoses, mechanisms of injury, and treatment of soldiers injured in Operation Iraqi Freedom: an epidemiological study conducted at two military pain management centers. Anesth Analg 2005; 101(4): 1098–1103. [DOI] [PubMed] [Google Scholar]
- 14. George SZ, Childs JD, Teyhen DS, et al. : Predictors of occurrence and severity of first time low back pain episodes: findings from a military inception cohort. PLoS One 2012; 7(2): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gironda RJ, Clark ME, Massengale JP, Walker RL: Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med 2006; 7(4): 339–43. [DOI] [PubMed] [Google Scholar]
- 16. Clark ME: Post-deployment pain: a need for rapid detection and intervention. Pain Med 2004; 5(4): 333–4. [DOI] [PubMed] [Google Scholar]
- 17. Office of The Army Surgeon General : Pain Management Task Force: Providing a Standardized DoD and VHA Vision and Approach to Pain Management to Optimize the Care for Warriors and their Families. Final Report. 2010. Available at https://www.usuhs.edu/sites/default/files/media/dvcipm/pdf/pain-task-force-final-report-may-2010.pdf; accessed February 20, 2018.
- 18. Otis JD, McGlinchey R, Vasterling JJ, Kerns RD: Complicating factors associated with mild traumatic brain injury: impact on pain and posttraumatic stress disorder treatment. J Clin Psychol Med Settings 2011; 18(2): 145–54. [DOI] [PubMed] [Google Scholar]
- 19. Cifu DX, Taylor BC, Carne WF, et al. : Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND Veterans. J Rehabil Res Dev 2013; 50(9): 1169–76. Available at http://www.rehab.research.va.gov/jour/2013/509/page1169.html; accessed July 14, 2017. [DOI] [PubMed] [Google Scholar]
- 20. Pugh MJ, Finley EP, Copeland LA, et al. : Complex comorbidity clusters in OEF/OIF veterans: the polytrauma clinical triad and beyond. Med Care 2014; 52(2): 172–81. [DOI] [PubMed] [Google Scholar]
- 21. Interagency Pain Research Coordinating Committee : National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. 2015; Available at https://iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf; accessed February 20, 2018.
- 22. Haskell SG, Brandt CA, Krebs EE, Skanderson M, Kerns RD, Goulet JL: Pain among veterans of Operations Enduring Freedom and Iraqi Freedom: do women and men differ? Pain Med 2009; 10(7): 1167–73. [DOI] [PubMed] [Google Scholar]
- 23. Lew H, Otis J, Tun C, Kerns R, Clark M, Cifu D: Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: Polytrauma clinical triad. J Rehabil Res Dev 2009; 46(6): 697–702. Available at http://www.rehab.research.va.gov/jour/09/46/6/page697.html; accessed July 14, 2017. [DOI] [PubMed] [Google Scholar]
- 24. Fillingim RB, Bruehl S, Dworkin RH, et al. : The ACTTION-American Pain Society Pain Taxonomy (AAPT): an evidence-based and multidimensional approach to classifying chronic pain conditions. J Pain 2014; 15(3): 241–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M: Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain 2007; 129(3): 355–62. [DOI] [PubMed] [Google Scholar]
- 26. Cicero TJ, Wong G, Tian Y, Lynskey M, Todorov A, Isenberg K: Co-morbidity and utilization of medical services by pain patients receiving opioid medications: data from an insurance claims database. Pain 2009; 144(1–2): 20–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Armed Forces Health Surveillance Center : Absolute and relative morbidity burdens attributable to various illnesses and injuries, active component, U.S. Armed Forces, 2015. MSMR 2016; 23(4): 2–7. Available at https://health.mil/Reference-Center/Reports/2016/01/01/Medical-Surveillance-Monthly-Report-Volume-23-Number-4; accessed July 14, 2017. [PubMed] [Google Scholar]
- 28. Agency for Healthcare Research and Quality – Healthcare Cost and Utilization Project (HCUP) : Clinical Classifications Software (CCS). 2014; Available at https://hcup-us.ahrq.gov/toolssoftware/ccs/CCSUsersGuide.pdf; accessed Jan 17, 2016.
- 29. Department of Veterans Affairs – Office of Inspector General : Healthcare Inspection – VA Patterns of Dispensing Take-Home Opioids and Monitoring Patients on Opioid Therapy. 2014; Available at https://www.va.gov/oig/pubs/VAOIG-14-00895-163.pdf; accessed July 14, 2017.
- 30. Seal KH, Shi Y, Cohen G, et al. : Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA 2012; 307(9): 940–7. [DOI] [PubMed] [Google Scholar]
- 31. Goulet JL, Brandt C, Crystal S, et al. : Agreement between electronic medical record-based and self-administered pain numeric rating scale: clinical and research implications. Med Care 2013; 51(3): 245–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Veterans Health Administration : Pain as the 5th Vital Sign Toolkit, revised edition. 2000; Available at https://www.va.gov/PAINMANAGEMENT/docs/TOOLKIT.pdf; accessed February 20, 2018.
- 33. National Institutes of Health : Chronic pain: Symptoms, diagnosis, & treatment. NIH Medline Plus 2011;Spring. Available at https://medlineplus.gov/magazine/issues/spring11/articles/spring11pg5-6.html; accessed January 16, 2017.
- 34. International Association for the Study of Pain (IASP) : Classification of Chronic Pain. Seattle, IASP Press, 2002. Available at http://www.iasp-pain.org/files/Content/ContentFolders/Publications2/FreeBooks/Classification-of-Chronic-Pain.pdf; accessed January 16, 2017. [Google Scholar]
- 35. Clark ME, Scholten JD, Walker RL, Gironda RJ: Assessment and treatment of pain associated with combat-related polytrauma. Pain Med 2009; 10(3): 456–69. [DOI] [PubMed] [Google Scholar]
- 36. American Society of Anesthesiologists Task Force on Chronic Pain Management, American Society of Regional Anesthesia and Pain Medicine : Practice guidelines for chronic pain management: an updated report by the American Society of Anesthesiologists Task Force on Chronic Pain Management and the American Society of Regional Anesthesia and Pain Medicine. Anesthesiology 2010; 112(4): 810–33. [DOI] [PubMed] [Google Scholar]
- 37. Chou R, Deyo R, Friedly J, et al. : Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017; 166(7): 493–505. [DOI] [PubMed] [Google Scholar]
- 38. International Association for the Study of Pain (IASP) : Pain Treatment Services. n.d. Available at http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1381; accessed April 7, 2017.
- 39. Office of The Army Surgeon General : Pain Management Task Force: Providing a Standardized DoD and VHA Vision and Approach to Pain Management to Optimize the Care for Warriors and their Families. 2010. Available at https://www.usuhs.edu/sites/default/files/media/dvcipm/pdf/pain-task-force-final-report-may-2010.pdf; accessed February 20, 2018
- 40. Lee C, Crawford C, Swann S. Active Self-Care Therapies for Pain Working Group : Multimodal, integrative therapies for the self-management of chronic pain symptoms. Pain Med 2014; 15(Suppl 1): S76–85. [DOI] [PubMed] [Google Scholar]
- 41. Department of Defense - Office of the Secretary of Defense : The Implementation of a Comprehensive Policy on Pain Management by the Military Health Care System for Fiscal Year 2015: Report to Congress. 2016. Available at https://health.mil/Reference-Center/Reports/2015/11/12/Comprehensive-Policy-on-Pain-Management; accessed July 14, 2017.
- 42. Buckenmaier CC 3rd, Galloway KT, Polomano RC, McDuffie M, Kwon N, Gallagher RM: Preliminary validation of the Defense and Veterans Pain Rating Scale (DVPRS) in a military population. Pain Med 2013; 14(1): 110–23. [DOI] [PubMed] [Google Scholar]
- 43. Cook KF, Buckenmaier C 3rd, Gershon RC: PASTOR/PROMIS (R) pain outcomes system: what does it mean to pain specialists? Pain Manag 2014; 4(4): 277–83. [DOI] [PubMed] [Google Scholar]
- 44. Ernat J, Knox J, Orchowski J, Owens B: Incidence and risk factors for acute low back pain in active duty infantry. Mil Med 2012; 177(11): 1348–51. [DOI] [PubMed] [Google Scholar]
- 45. Eilat-Tsanani S, Tabenkin H, Lavie I, Cohen Castel O, Lior M: The effect of low back pain on work absenteeism among soldiers on active service. Spine 2010; 35(19): E995–999. [DOI] [PubMed] [Google Scholar]
- 46. Blyth FM, March LM, Brnabic AJ, Cousins MJ: Chronic pain and frequent use of health care. Pain 2004; 111(1–2): 51–8. [DOI] [PubMed] [Google Scholar]
- 47. Von Korff M, Lin EH, Fenton JJ, Saunders K: Frequency and priority of pain patients’ health care use. Clin J Pain 2007; 23(5): 400–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.