Abstract
Background:
Previous studies have analyzed the treatment patterns used to manage injuries in National Football League (NFL) players.
Hypothesis:
Treatment patterns for injuries in NFL players will have changed over the study period.
Study Design:
Descriptive epidemiology study.
Level of Evidence:
Level 5.
Methods:
The head orthopaedic team physicians for all 32 NFL teams were asked to complete a survey containing questions regarding experience as team physician, medical coverage of the team, and treatment preferences for some of the most common injuries occurring in football players. Responses from the current survey were compared with responses from the same survey sent to NFL team physicians in 2008.
Results:
Responses were received from 31 (31/32, 97%) NFL team physicians in 2008 and 29 (29/32, 91%) NFL team physicians between April 2016 and May 2017. The proportion of physicians preferring patellar tendon autograft in anterior cruciate ligament (ACL) reconstruction increased from 87% in 2008 to 97% in 2016 (P = 0.054). In 2008, 49% of physicians allowed return to contact after ACL reconstruction at 6 months or less as compared with only 14% of physicians in 2016 (P = 0.033). In 2008, 93% of physicians used Toradol injections prior to a game to help with nagging injuries. Toradol injection utilization decreased to 48% of physicians in 2016 (P < 0.001). Seventy-nine percent of physicians would administer 5 or more Toradol injections prior to a game in 2008, as compared with 28% of physicians in 2016 (P < 0.0001).
Conclusion:
Orthopaedic physicians have changed their injury treatment preferences for professional football players. In particular, physicians have become more cautious with allowing players to return to play after ACL reconstruction and with the use of pregame Toradol injections.
Clinical Relevance:
Expert opinions can help guide treatment decisions and lead to better care of all athletes.
Keywords: football, treatment patterns, NFL, anterior cruciate ligament reconstruction, Toradol
With the high level of play in the National Football League (NFL), players are often subject to many injuries. As players depend on the health of their bodies to perform, their careers and livelihoods can suffer greatly with these injures. Secrist et al24 found that players who suffered from anterior cruciate ligament (ACL) injuries were less likely to remain in the NFL and earned an average salary of $2,070,521 less when compared with uninjured counterparts over the study period. Unfortunately, for several football-related injuries, there is no definitive treatment option that is regarded as superior to all others, as data are often inconclusive. In such cases, expert opinion can be sought out to help guide treatment decisions.
In 2008, McCarty et al18 surveyed NFL orthopaedic team physicians regarding their preferred treatment options for several common football-related injuries. However, treatment patterns often change with advancements in medical research and technology, and these previously established treatment patterns are now outdated. Therefore, the purpose of this study was to update the literature on the treatment preferences of NFL team physicians.
Methods
This study was reviewed but was found exempt from institutional review board approval. The head orthopaedic team physicians for all 32 NFL teams were asked to complete a survey containing questions regarding the experience of team physicians, medical coverage of the team, and management of common football injuries (see Appendix 1, available in the online version of this article). This survey was identical to that used in a prior study.1,18 The link to the survey was sent out to each team physician in an email that explained the purpose behind the study, with reminder emails sent every 2 weeks. For physicians without a known email address, alternate contacts were asked to provide the email address of the physician. Physicians were surveyed once in 200818 and again in 2016 in an anonymous survey using SurveyGizmo. The survey results were then compared with the results of the same survey sent to NFL team physicians in 2008.
Statistical Analysis
Chi-square tests were used to determine significant differences between the results of the 2008 and 2016 surveys. A P value <0.05 was considered statistically significant.
Results
Team Physician Demographics
Responses were received from 31 of 32 (97%) NFL orthopaedic team physicians in 2008 and 29 of 32 (91%) NFL orthopaedic team physicians between April 2016 and May 2017. In 2008, 39% of physicians had been the head team physician for more than 15 years, compared with 67% in 2016 (P = 0.034). The proportion of orthopaedic team physicians who were fellowship-trained in sports medicine increased from 81% in 2008 to 93% in 2016 (P = 0.16). The proportion of orthopaedic team physicians who received a monetary stipend for providing orthopaedic coverage remained consistent over the study period (2008, 97%; 2016, 100%; P = 0.32). The proportion of orthopaedic team physicians who received advertising from their respective teams in exchange for their services remained constant from 2008 (10%) to 2016 (10%) (P = 0.97). There was an increase in the proportion of team physicians reporting 4 or more physicians traveling to away games (2008, 20%; 2016, 55%; P = 0.011). The proportion of teams using an orthopaedic surgeon as the head team physician did not change over the study period (2008, 90%; 2016, 90%; P = 0.55).
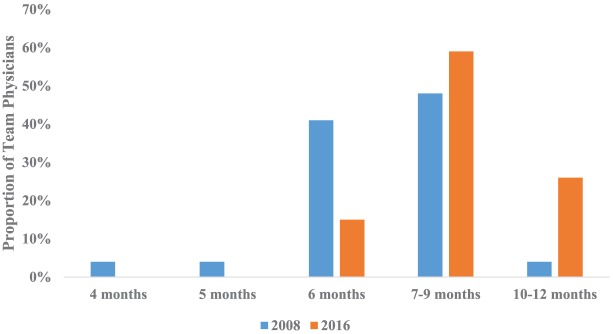
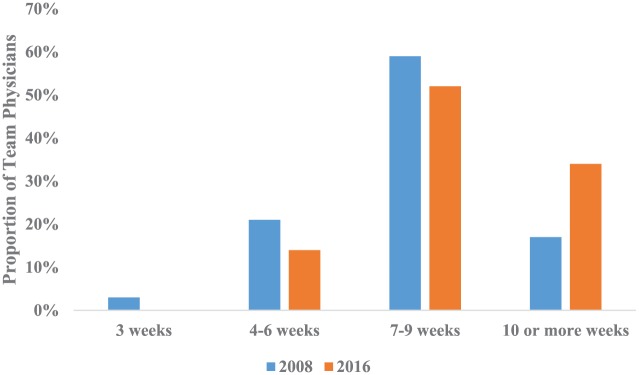
ACL Reconstruction
The proportion of physicians preferring patellar tendon autograft for ACL reconstruction increased from 87% in 2008 to 97% in 2016 (P = 0.054) (Table 1). In 2008, 49% of physicians allowed return to contact after ACL reconstruction by 6 months, as compared with 14% of physicians in 2016 (P = 0.033) (Figure 1). Twenty-four percent of physicians allowed return to contact between 10 and 12 months in 2016, an increase from 4% in 2008 (P = 0.033). The use of a functional brace after an isolated ACL reconstruction stayed relatively the same over the study period (2008, 57%; 2016, 62%; P = 0.70). Among those using a brace, the majority of team physicians did so for offensive linemen (2008, 56%; 2016, 69%) and defensive linemen (2008, 41%; 2016, 52%). Physicians preferred to brace other positions to a lesser extent in 2008 and 2016 (Table 2). In 2008, 31% of orthopaedic team physicians used the brace for less than 6 months, increasing to 41% in 2016 (P = 0.56).
Table 1.
Preferred graft choice for anterior cruciate ligament reconstruction a
| Graft Type | 2008 (N = 30) | 2016 (N = 29) |
|---|---|---|
| Hamstring autograft | 2 (7) | 0 (0) |
| Patellar tendon autograft | 26 (87) | 28 (97) |
| Achilles tendon allograft | 4 (13) | 0 (0) |
| Hybrid auto/allograft | 0 (0) | 1 (3) |
Data presented as n (%).
Figure 1.
Return to play after anterior cruciate ligament (ACL) reconstruction. Y-axis represents the proportion of team physicians allowing return to play after primary ACL reconstruction.
Table 2.
Positions that receive a brace after anterior cruciate ligament reconstruction a
| Position | 2008 (N = 27) | 2016 (N = 29) |
|---|---|---|
| OL | 15 (56) | 20 (69) |
| RB/WR/DB | 6 (22) | 10 (34) |
| DL | 11 (41) | 15 (52) |
| LB | 9 (33) | 12 (41) |
| QB | 10 (37) | 13 (45) |
DB, defensive back; DL, defensive lineman; LB, linebacker; OL, offensive lineman; QB, quarterback; RB, running back; WR, wide receiver.
Team physicians were able to select multiple answers. Data presented as n (%).
Anterior Shoulder Dislocation (Without Bony Bankart)
After closed reduction of an anterior shoulder dislocation, all orthopaedic team physicians had athletes wear a sling in 2008, though 17% of physicians chose not to use a sling in 2016 (P = 0.066) (Table 3). When this injury occurred during the season and the athlete returned to play without surgery, the majority of orthopaedic team physicians had their athletes play using a harness (2008, 93%; 2016, 90%; P = 0.67).
Table 3.
Use of sling after anterior shoulder dislocation a
| Duration of Sling Use After Reduction | 2008 (N = 29) | 2016 (N = 29) |
|---|---|---|
| Do not use a sling | 0 (0) | 5 (17) |
| <1 wk | 16 (55) | 17 (59) |
| 1-2 wk | 10 (35) | 4 (14) |
| 3-4 wk | 3 (10) | 2 (7) |
| >4 wk | 0 (0) | 1 (3) |
Team physicians were asked how long they require athletes to wear a sling after reduction. Data presented as n (%).
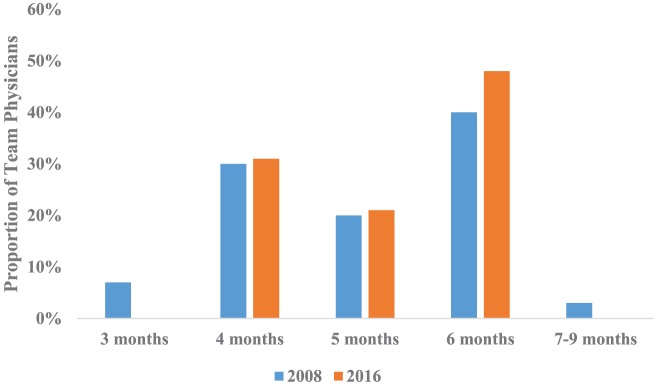
The majority of orthopaedic team physicians performed anterior shoulder stabilization arthroscopically (2008, 79%; 2016, 90%; P = 0.28). In 2008, 40% of physicians allowed return to contact activity after 6 months, compared with 48% in 2016 (P = 0.54) (Figure 2). The majority of physicians did not require athletes to wear a harness after anterior shoulder stabilization, (2008, 73%; 2016, 76%; P = 0.97) (Table 4).
Figure 2.
Return to play after anterior shoulder stabilization. Y-axis represents the proportion of team physicians allowing return to play after anterior shoulder stabilization.
Table 4.
Use of harness after anterior shoulder stabilization a
| Response | 2008 (N = 30) | 2016 (N = 29) |
|---|---|---|
| Yes | 1 (3) | 1 (3) |
| No | 22 (73) | 22 (76) |
| Depends on the player’s position | 7 (23) | 6 (21) |
Team physicians were asked whether they require athletes to use a harness after anterior shoulder stabilization. Data presented as n (%).
Acromioclavicular Joint Injury
The proportion of physicians using a local anesthetic injection for players sustaining a type I or II acromioclavicular (AC) joint injury increased from 60% in 2008 to 86% in 2016 (P = 0.024). Ninety percent of physicians in 2008 and 100% of physicians in 2016 injected athletes prior to games to allow play (P = 0.080). Cortisone injections to decrease inflammation during the acute/subacute period remained consistent over the study period (2008, 57%; 2016, 66%; P = 0.49). The majority of physicians preferred to treat AC joint type III injuries nonoperatively (2008, 72%; 2016, 83%; P = 0.34) (Table 5).
Table 5.
Treatment of type III acromioclavicular joint injuries a
| Treatment Method | 2008 (N = 29) | 2016 (N = 29) |
|---|---|---|
| Treat nonoperatively | 21 (72) | 24 (83) |
| Operate only in quarterback (throwing arm) | 8 (28) | 4 (14) |
| Operate in all players | 0 (0) | 1 (3) |
Data presented as n (%).
Medial Collateral Ligament Bracing
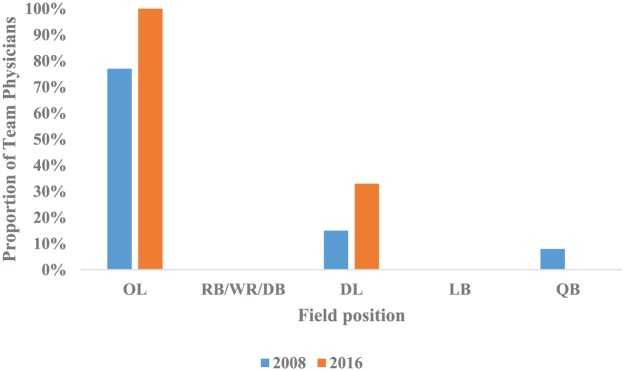
Prophylactic bracing to prevent medial collateral ligament (MCL) injuries stayed relatively constant over the study period (2008, 27%; 2016, 28%; P = 0.94). Of those who recommended MCL bracing, most did so with offensive linemen (2008, 77%; 2016, 100%; P = 0.75) (Figure 3).
Figure 3.
Field positions in which a medial collateral ligament (MCL) knee brace is used. Y-axis represents the proportion of team physicians using an MCL knee brace. DB, defensive back; DL, defensive lineman; LB, linebacker; OL, offensive lineman; QB, quarterback; RB, running back; WR, wide receiver.
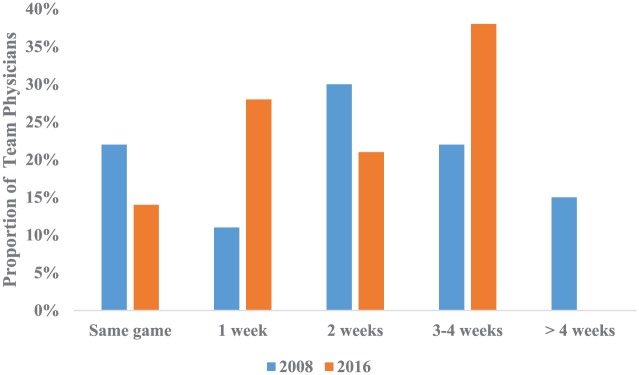
Posterior Cruciate Ligament Injuries
Same-game return to play for athletes suffering a grade I/II posterior cruciate ligament (PCL) injury was allowed by 22% of team physicians in 2008 and 14% in 2016 (P = 0.079) (Figure 4). Isolated grade III PCL injuries were treated nonoperatively by 57% of surgeons in 2008 and 62% of surgeons in 2016 (P = 0.72) (Table 6). Among surgeons who operate for these injuries, the majority continued to do so with the arthroscopic single-bundle technique (2008, 54%; 2016, 63%; P = 0.29) (Figure 5).
Figure 4.
Return to play after grade I/II posterior cruciate ligament (PCL) injury. Y-axis represents the proportion of team physicians allowing return to play after grade I/II PCL injury.
Table 6.
Frequency of fixing a grade III posterior cruciate ligament injury a
| Frequency | 2008 (N = 28) | 2016 (N = 29) |
|---|---|---|
| Never | 16 (57) | 18 (62) |
| One-third of the time | 9 (32) | 8 (28) |
| Two-thirds of the time | 2 (7) | 3 (10) |
| Always | 1 (4) | 0 (0) |
Team physicians were asked how often they fix isolated grade III posterior cruciate ligament injuries in National Football League players. Data presented as n (%).
Figure 5.
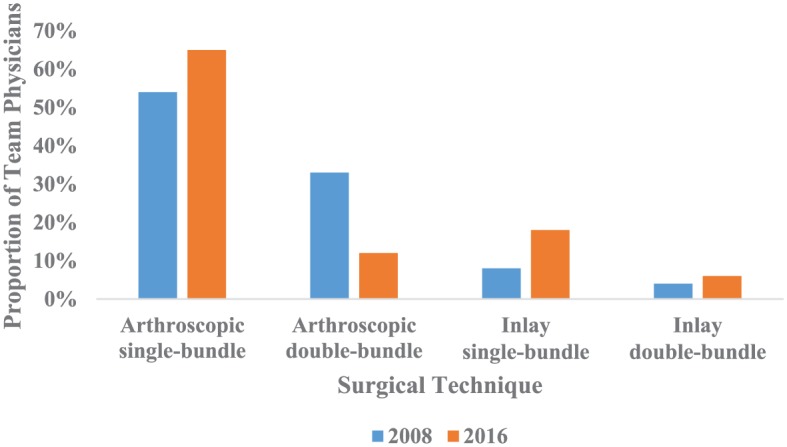
Technique used for posterior cruciate ligament reconstruction.
Ulnar Collateral Ligament
Elbow
Complete ulnar collateral ligament (UCL) injuries of the elbow were never fixed in NFL players by 27% and 48% of surgeons in 2008 and 2016, respectively (P = 0.24) (Table 7). Among those who preferred operative fixation of this injury, the majority did so in quarterbacks (2008, 96%; 2016, 93%; P = 0.24).
Table 7.
Frequency of surgically repairing a complete elbow ulnar collateral ligament injury a
| Position | 2008(N = 25) | 2016 (N = 15) |
|---|---|---|
| Never fix in a football player | 8 b (27) | 14 c (48) |
| QB | 24 (96) | 14 (93) |
| RB/WR/DB | 2 (8) | 2 (13) |
| OL | 1 (4) | 1 (7) |
| DL | 1 (4) | 1 (7) |
| LB | 1 (4) | 1 (7) |
DB, defensive back; DL, defensive lineman; LB, linebacker; OL, offensive lineman; QB, quarterback; RB, running back; WR, wide receiver.
Team physicians were asked in which players they fix a complete elbow ulnar collateral ligament tear. Physicians were able to select multiple responses. Data presented as n (%).
N = 30.
N = 29.
Thumb
The majority of surgeons in 2008 and 2016 treated thumb UCL tears by casting and allowing return to play (2008, 63%; 2016, 55%; P = 0.58).
Fifth Metatarsal Fracture
Screw fixation was the preferred treatment for fifth metatarsal fractures by 100% of team orthopaedic surgeons in 2008 and 2016. Players with this injury were allowed to return to play most frequently between 7 and 9 weeks (2008, 59%; 2016, 52%; P = 0.37) (Figure 6). The proportion of team physicians who allowed return to play at 10 or more weeks increased from 17% in 2008 to 34% in 2016 (P = 0.37) (Figure 6).
Figure 6.
Return to play after fifth metatarsal treatment. Y-axis represents the proportion of team physicians allowing return to play after fifth metatarsal treatment.
Tibial Fractures
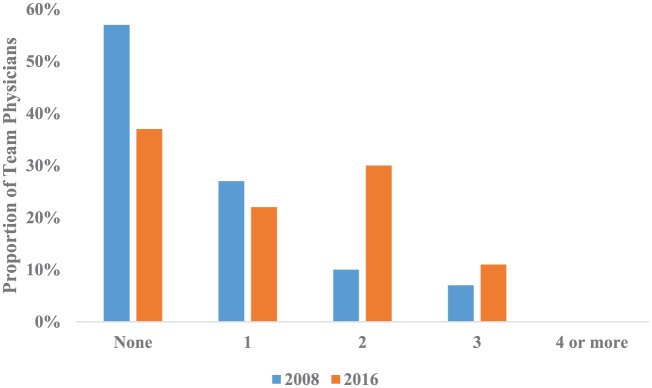
There was an increase in the number of tibial fractures encountered by the team physicians surveyed in 2016 compared with 2008, as the number of surgeons who had not treated a tibial fracture in the previous 5 years decreased from 57% in 2008 to 38% in 2016 (P = 0.28) (Figure 7). The preferred treatment for tibial fractures was intramedullary nailing by 100% of surgeons in 2008 and 2016. No surgeon reported tibial nonunion in 2008 or 2016. All surgeons in 2008 and 2016 preferred not to remove the nail prior to return to play.
Figure 7.
Number of tibial fractures encountered over the past 5 years.
Toradol Injections
In 2008, 93% of physicians used Toradol (Roche) injections prior to a game to help with nagging injuries, compared with 48% of physicians in 2016 (P < 0.001). Seventy-nine percent of physicians would administer 5 or more Toradol injections prior to a game in 2008, as compared with 28% of physicians in 2016 (P < 0.0001) (Table 8).
Table 8.
Average number of Toradol injections administered prior to games a
| No. of injections | 2008 (N = 28) | 2016 (N = 29) |
|---|---|---|
| 0 | 1 (4) | 16 (55) |
| 1 | 1 (4) | 3 (10) |
| 2 | 0 (0) | 0 (0) |
| 3 | 0 (0) | 0 (0) |
| 4 | 4 (14) | 2 (7) |
| ≥5 | 22 (79) | 8 (28) |
Team physicians were asked, on average, how many Toradol injections they administered to National Football League players prior to games. Data presented as n (%).
Discussion
This study is the first to analyze changes and trends in the treatment patterns used to manage common injuries in professional football players over an extended period of time. There was an overall response rate of 94% of NFL team physicians in 2008 and 2016. Each NFL division was represented in both years. This survey indicated that 90% of head NFL team physicians were orthopaedic surgeons in 2008 and 2016.
There has been an increase in the proportion of fellowship-trained team physicians, and a high proportion of team physicians continue to receive a monetary stipend for providing orthopaedic coverage to NFL teams. A low proportion of team physicians in 2008 and 2016 received advertising for their practice.
Injury Management
ACL Injuries
ACL injuries are a common injury encountered by NFL players and often have negative implications on players’ careers.24 In the present study, NFL team physicians who preferred patellar tendon autograft for ACL reconstruction increased from 87% to 97% during the study period. Interestingly, no physician preferred allograft in 2016, as compared with 13% in 2008. In 2014, Erickson et al7 surveyed NFL team physicians and found that 86% preferred patellar tendon autograft. The same study7 found only 1 physician (0.7%) who preferred allograft, similar to the present study results. Recent literature8-10 has demonstrated lower rates of graft rupture with patellar tendon autograft when compared with both hamstring autograft8 and patellar tendon allograft.9,10 This recent literature could be the motivation behind the trend toward increased use of patellar tendon autograft. The present study also found 1 physician who preferred a hybrid autograft/allograft for ACL reconstruction. However, there have not been published data on hybrid graft use in elite athletes, and hybrid grafts may result in a greater risk of graft rupture than autografts.2
Over the study period, NFL physicians have become more conservative with time to return to play after ACL reconstruction. Only 14% of physicians in 2016 allowed return to play by 6 months, as compared with 49% in 2008. The most common return-to-play time in 2016 was 7 to 9 months (62%), with 24% of NFL physicians waiting as long as 10 to 12 months before allowing return to play. This is similar to results reported by Erickson et al,7 who found that 55% of physicians allowed return to play at a minimum of 6 months. However, Erickson et al7 also found that only 12% of physicians waited at least 9 months before allowing return to play. Recent studies have shown the financial impacts of ACL injury on NFL players,24 which may lead to physicians taking a more conservative approach after ACL reconstruction.
Anterior Shoulder Dislocation
With regard to the management of anterior shoulder dislocations, NFL physicians did not change their preferences on harness use or return-to-play time after anterior shoulder stabilization. Most NFL physicians required players to wear a sling for less than 1 week after reduction. Interestingly, 17% of physicians elected not to use a sling at all in 2016, whereas no surgeon chose this as the preferred treatment in 2008. This may suggest a more aggressive approach to the treatment of shoulder dislocations by NFL physicians. Treating shoulder dislocations with stabilization surgery has proven to be a successful procedure,4 and the majority of NFL physicians choose to perform this procedure arthroscopically.
Acromioclavicular Joint Sprains
AC joint injuries are common among NFL players, especially at the quarterback position.14 The general consensus among most NFL team physicians in 2008 was to treat type III AC joint injuries nonoperatively (72%), with 28% choosing surgical intervention only on a quarterback’s throwing arm. Physician preferences remained unchanged over the study period, with only slightly more physicians preferring nonoperative intervention in 2016 (83%). Nonoperative management has shown to be an adequate treatment for type III AC joint injuries in past studies.17,19,23,26 Lynch et al14 found that NFL players who underwent surgical treatment for AC joint injuries lost more time than players undergoing nonoperative treatment. Therefore, NFL physicians may prefer nonoperative treatment to prevent players from losing playing time. Additionally, because AC joint injuries are common among NFL players,14 NFL team physicians may wish to avoid surgery and the risk of recurrence.
More NFL physicians chose to inject local anesthetic during games for AC joint injuries to allow continued play in 2016 compared with 2008. AC joint anesthetic injections are also commonly used on professional rugby athletes.20 Orchard et al20 found this treatment to be both safe and effective, as 98% of athletes stated they would have the procedure performed again.
MCL Bracing
There was no change seen in the use of prophylactic knee bracing to prevent MCL injuries over the study period, with a relatively low percentage of NFL physicians choosing to do so. The recommendation for the use of prophylactic bracing may come from the team physician initially, but it may also be based on player choice. Of physicians choosing to use prophylactic MCL bracing, most choose only to do so in offensive and defensive linemen. Previous studies5,22 have shown inconclusive results regarding the effectiveness of prophylactic bracing. However, no recent studies have been published on this issue.
PCL Injuries
Management of PCL injuries remained unchanged over the study period, with most NFL physicians choosing to treat grade III PCL injuries nonoperatively. This is similar to results reported by Shino et al,25 who found that only 14% of athletes in their study underwent surgical management for a PCL injury. Shino et al25 also found nonoperative treatment to be a successful management strategy for isolated PCL injuries, which may reinforce current NFL physician preferences. However, recent studies12 have shown greater rates of surgical intervention for isolated PCL injuries as a result of improved knowledge of PCL anatomy and biomechanics.
Elbow UCL Injuries
The proportion of team physicians who preferred to treat elbow UCL injuries nonoperatively increased from 2008 to 2016. Current literature suggests UCL reconstruction as the optimal treatment strategy in the throwing athlete, as a number of studies have shown a high rate of baseball pitchers returning to their previous level of performance after the procedure.11,27 Among team physicians who prefer operative treatment, a high percentage continue to do so for the quarterback. Dodson et al3 reviewed UCL injuries in NFL quarterbacks over a 14-year span. Among 10 cases, 9 were treated nonoperatively, and the mean return-to-play time was approximately 4 weeks.3 The authors determined that this injury is rather uncommon in professional quarterbacks, and that these athletes can be successfully treated nonoperatively.3
Thumb UCL Injuries
The majority of team physicians continued to prefer to treat in-season thumb UCL injuries by casting and allowing return to play, although there was a slight shift toward operating first and then casting and allowing return to play. A small percentage of team physicians preferred to operate and then allow the ligament to heal before allowing return to play in both 2008 and 2016. In a case series of NFL players, Werner et al28 determined that 63% of isolated thumb UCL injuries required surgical repair. It was determined in a previous study that delayed surgery for thumb UCL injuries was not associated with adverse clinical outcomes in collegiate football players.29
Fifth Metatarsal Injuries
Screw fixation is overwhelmingly the treatment preference of team physicians for fifth metatarsal injuries, as every team physician in 2008 and 2016 preferred screw fixation rather than casting. In 2008, 76% of team physicians allowed return to play after 6 weeks, increasing to 86% of team physicians in 2016. Lareau et al13 reported a mean return to play of less than 9 weeks in 25 NFL players treated for fifth metatarsal injury with screw fixation. The authors highlighted the importance of radiographic healing in addition to physical examination in determining return to play after this treatment.13
Tibial Fractures
The number of tibial fractures treated over the past 5 years increased for team physicians. Every team physician in 2008 and 2016 preferred intramedullary nailing as treatment, with no physician removing the nail prior to the athlete returning to play. Tibial intramedullary nailing has been shown to lead to a high rate of return to play in NFL players as well as a high rate of return to baseline performance.15
Toradol Injections
Toradol has been described for the treatment of acute or pregame pain in the professional football player.6,21 In a previous study,18 the use of Toradol injections declined significantly since the NFL Physician Society Task Force published recommendations on its use.16 Based on the present study, the proportion of team physicians using Toradol injections prior to football games continued to decrease, from 93% of physicians in 2008 to less than half in 2016.
Strengths and Limitations
The strengths of this study include the large proportion of NFL team physicians surveyed. This study is also the first to analyze changes and trends in the treatment patterns used to manage common injuries in professional football players over an extended period of time. The main limitation of this study is that it is based solely on expert opinion rather than clinical outcomes. Additionally, it is unknown how many team physicians remained consistent over the study period, although 67% stated that they had been the team physician for more than 15 years. Finally, many treatment decisions are based on a number of factors in addition to physician preference, such as player position, time during the season/offseason, handedness, injury type/grade, and team preferences.
Conclusion
Treatment patterns used by NFL physicians have changed over the study period. In particular, physicians have become more conservative with return-to-play time after ACL reconstruction and pregame Toradol injections. Graft preferences for ACL reconstruction have also changed with time. Understanding current treatment patterns and how they change over time can guide treatment decisions and lead to further research geared toward improving the treatment of athletes.
Footnotes
The following author declared potential conflicts of interest: Eric C. McCarty, MD, is a paid consultant for Biomet and receives royalties from Elsevier.
References
- 1. Carver TJ, Schrock JB, Kraeutler MJ, McCarty EC. The evolving treatment patterns of NCAA Division I football players by orthopaedic team physicians over the past decade, 2008-2016 [published online January 3, 2018]. Sports Health. doi: 10.1177/1941738117745488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Darnley JE, Leger-St-Jean B, Pedroza AD, Flanigan DC, Kaeding CC, Magnussen RA. Anterior cruciate ligament reconstruction using a combination of autograft and allograft tendon: a MOON cohort study. Orthop J Sports Med. 2016;4:2325967116662249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19:1276-1280. [DOI] [PubMed] [Google Scholar]
- 4. Donohue MA, Owens BD, Dickens JF. Return to play following anterior shoulder dislocation and stabilization surgery. Clin Sports Med. 2016;35:545-551. [DOI] [PubMed] [Google Scholar]
- 5. Duffy PS, Miyamoto RG. Management of medial collateral ligament injuries in the knee: an update and review. Phys Sportsmed. 2010;38:48-54. [DOI] [PubMed] [Google Scholar]
- 6. Eichner ER. Intramuscular ketorolac injections: the pregame Toradol parade. Curr Sports Med Rep. 2012;11:169-170. [DOI] [PubMed] [Google Scholar]
- 7. Erickson BJ, Harris JD, Fillingham YA, et al. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30:731-738. [DOI] [PubMed] [Google Scholar]
- 8. Gifstad T, Foss OA, Engebretsen L, et al. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319-2328. [DOI] [PubMed] [Google Scholar]
- 9. Kane PW, Wascher J, Dodson CC, Hammoud S, Cohen SB, Ciccotti MG. Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft in skeletally mature patients aged 25 years or younger. Knee Surg Sports Traumatol Arthrosc. 2016;25:3627-3633. [DOI] [PubMed] [Google Scholar]
- 10. Kraeutler MJ, Bravman JT, McCarty EC. Bone–patellar tendon–bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41:2439-2448. [DOI] [PubMed] [Google Scholar]
- 11. Langer P, Fadale M, Hulstyn M. Evolution of the treatment options of ulnar collateral ligament injuries of the elbow. Br J Sports Med. 2006;40:499-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. LaPrade CM, Civitarese DM, Rasmussen MT, LaPrade RF. Emerging updates on the posterior cruciate ligament: a review of the current literature. Am J Sports Med. 2015;43:3077-3092. [DOI] [PubMed] [Google Scholar]
- 13. Lareau CR, Hsu AR, Anderson RB. Return to play in National Football League players after operative Jones fracture treatment. Foot Ankle Int. 2016;37:8-16. [DOI] [PubMed] [Google Scholar]
- 14. Lynch TS, Saltzman MD, Ghodasra JH, Bilimoria KY, Bowen MK, Nuber GW. Acromioclavicular joint injuries in the National Football League: epidemiology and management. Am J Sports Med. 2013;41:2904-2908. [DOI] [PubMed] [Google Scholar]
- 15. Mai HT, Alvarez AP, Freshman RD, et al. The NFL Orthopaedic Surgery Outcomes Database (NO-SOD): the effect of common orthopaedic procedures on football careers. Am J Sports Med. 2016;44:2255-2262. [DOI] [PubMed] [Google Scholar]
- 16. Matava M, Brater DC, Gritter N, et al. Recommendations of the National Football League Physician Society Task Force on the use of Toradol® ketorolac in the National Football League. Sports Health. 2012;4:377-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316-329. [DOI] [PubMed] [Google Scholar]
- 18. McCarty EC, Kraeutler MJ, Langner P, Cook S, Ellis B, Godfrey JM. Historical patterns and variation in treatment of injuries in NFL (National Football League) players and NCAA (National Collegiate Athletic Association) Division I football players. Am J Orthop (Belle Mead NJ). 2016;45:E319-E327. [PubMed] [Google Scholar]
- 19. Natera Cisneros LG, Sarasquete Reiriz J. Acute high-grade acromioclavicular joint injuries: quality of life comparison between patients managed operatively with a hook plate versus patients managed non-operatively. Eur J Orthop Surg Traumatol. 2017;27:341-350. [DOI] [PubMed] [Google Scholar]
- 20. Orchard JW, Street E, Massey A, Dan S, Gardiner B, Ibrahim A. Long-term safety of using local anesthetic injections in professional rugby league. Am J Sports Med. 2010;38:2259-2266. [DOI] [PubMed] [Google Scholar]
- 21. Powell ET, Tokish JM, Hawkins RJ. Toradol use in the athletic population. Curr Sports Med Rep. 2002;1:191. [DOI] [PubMed] [Google Scholar]
- 22. Salata MJ, Gibbs AE, Sekiya JK. The effectiveness of prophylactic knee bracing in American football: a systematic review. Sports Health. 2010;2:375-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schlegel TF, Burks RT, Marcus RL, Dunn HK. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29:699-703. [DOI] [PubMed] [Google Scholar]
- 24. Secrist ES, Bhat SB, Dodson CC. The financial and professional impact of anterior cruciate ligament injuries in National Football League athletes. Orthop J Sports Med. 2016;4:2325967116663921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shino K, Horibe S, Nakata K, Maeda A, Hamada M, Nakamura N. Conservative treatment of isolated injuries to the posterior cruciate ligament in athletes. J Bone Joint Surg Br. 1995;77:895-900. [PubMed] [Google Scholar]
- 26. Spencer EE., Jr. Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res. 2007;455:38-44. [DOI] [PubMed] [Google Scholar]
- 27. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1193-1205. [DOI] [PubMed] [Google Scholar]
- 28. Werner BC, Belkin NS, Kennelly S, et al. Injuries to the collateral ligaments of the metacarpophalangeal joint of the thumb, including simultaneous combined thumb ulnar and radial collateral ligament injuries, in National Football League athletes. Am J Sports Med. 2017;45:195-200. [DOI] [PubMed] [Google Scholar]
- 29. Werner BC, Hadeed MM, Lyons ML, Gluck JS, Diduch DR, Chhabra AB. Return to football and long-term clinical outcomes after thumb ulnar collateral ligament suture anchor repair in collegiate athletes. J Hand Surg Am. 2014;39:1992-1998. [DOI] [PubMed] [Google Scholar]