Abstract
Purpose
The intrasaccular flow disruptor Woven EndoBridge (WEB) device is developed for the treatment of wide-necked aneurysms without supportive devices. We used the WEB as primary treatment for unruptured aneurysms suitable for the device, regardless of neck size.
Methods
Between February 2015 and June 2017, 59 aneurysms in 51 patients were selectively treated with the WEB. There were 15 men and 36 women with a mean age of 59 years. Mean aneurysm size was 7.0 mm (range 3–22 mm). Of 59 aneurysms, 45 (76%) had a wide neck defined as ≥4 mm or dome-neck ratio ≤1.5. No stents or supporting balloons were used.
Results
Initial WEB position was judged good in all 59 unruptured aneurysms.
One patient with a basilar tip aneurysm had a late thrombotic posterior cerebral artery occlusion by protrusion of the WEB over the artery. There were no procedural ruptures. Overall complication rate was 2.0% (1 of 51, 95% CI 0.01–11.3%). Imaging follow-up was available in 55 of 59 aneurysms (93%). At 3 months, 41 of 57 aneurysms (72%) were completely occluded, 12 (21%) had a neck remnant and 4 (7%) were incompletely occluded.
Conclusion
WEB treatment is safe and effective in selected unruptured aneurysms suitable for the device, regardless of neck size or location. There was no need for supportive devices. Three-quarters of all unruptured small aneurysms could be treated with the WEB. In our opinion, the WEB is a valuable alternative to coils, especially in wide-necked aneurysms.
Keywords: Woven EndoBridge, WEB device, intracranial aneurysms, endovascular treatment
Introduction
Endovascular coil treatment of wide-necked intracranial aneurysms commonly requires the use of a temporary protection balloon or a stent to avoid compromising the parent vessel. In general, this makes the procedure more complicated with an inherent higher chance of procedural complications.1–4 With use of stents, periprocedural antiplatelet therapy consisting of clopidogrel and aspirin is required and this has to be prolonged for 3–6 months.
Recently, the intrasaccular flow disruptor Woven EndoBridge (WEB, MicroVention, Tustin, CA, USA) device was developed for the treatment of wide-necked aneurysms without the need for supporting devices. First clinical results of the WEB device show good safety and efficacy profiles. Most of the published series comprised wide-necked unruptured aneurysms.5–24 The first generation of WEBs consisted of dual layer devices (WEB-DL) with a high profile needing 0.027 - or 0.033-in micro catheters. The next generation came with a single layer design (WEB-SL) and a lower profile, suitable for a 0.021-in micro catheter (WEB 21). The latest generation of WEBs is suitable for a 0.017-in micro catheter (WEB 17) and was introduced in clinical practice in December 2016.25
In February 2015, just after introduction of the WEB 21 system, we started to use WEBs for wide-necked unruptured intracranial aneurysms with the intention to avoid the use of stents. Our first results in wide-necked aneurysms were encouraging and we decided to expand the indication to all aneurysms suitable for the WEB, regardless of neck size, rupture status or location.16 We hypothesized that the WEB can occlude selected unruptured aneurysms at a low complication rate.
In this study we present the results of the first 59 unruptured aneurysms treated with the WEB in our institution.
Materials and methods
General
This is a retrospective observational study without defined inclusion and exclusion criteria. Endpoints are occlusion status at 3 months’ imaging follow-up and procedural complications leading to morbidity or mortality.
The study was performed in the St. Elisabeth Ziekenhuis in Tilburg.
The WEB device
The WEB system is a self-expanding, spherical (SLS) or pumpkin-shaped (SL), braided mesh of platinum cored nitinol wires that can be delivered through a micro catheter and deployed in the aneurysm sac. The WEBs with diameters 4–7 mm can be delivered through a 0.021-in internal micro catheter, the WEBs 8–9 mm through a 0.027-in and the WEBs 10–11 mm through a 0.033-in micro catheter (VIA 21, VIA 27 and VIA 33). Recently, a lower profile range of WEBs compliant with a 0.017-in micro catheter (VIA 17) has become available in clinical practice. These comprise smaller and shallower sizes including some 0.5 mm sizes.
Placed in the aneurysm, the WEB alters the blood flow at the level of the neck and induces aneurysmal thrombosis. The WEB is attached to a pusher wire and can be fully retrieved until final detachment by an electrothermal detachment system contained in a hand-held controller.
General indications in this study
Patients with unruptured aneurysms are discussed in a weekly joint meeting with neurosurgeons, neurologists and neuroradiologists. When treatment is indicated, the primary modality is endovascular selective treatment or parent vessel occlusion. When stents or flow diverters are foreseen, the patient is preloaded with dual anti-aggregation therapy. Surgery is considered in patients with aneurysms with unfavorable anatomy for endovascular treatment, such as aneurysms with vessels coming from the sac and shallow wide-necked aneurysms, defined as aneurysms with height/width ratio of ≤0.5 (overwide or undertall). In aneurysms ≤10 mm, the WEB was the primary treatment modality. Although the maximum size of the WEB is 11 mm, the WEB may be used in larger aneurysms. This can be due to aneurysm shape (tall aneurysms) where the WEB may be used to occlude the neck only and the fundus may or may not be filled with coils. Partially thrombosed aneurysms can also be larger but with a small lumen that can be occluded with the WEB.
In aneurysms too large for the WEB, coiling was the treatment of choice.
Under general anesthesia, a micro catheter was advanced into the aneurysm via a coaxial or triaxial approach. Hence, the WEB was placed inside the aneurysm. The WEB was slightly oversized, according to the manufacturer’s recommendations. WEB sizes and shapes were recorded. Apart from heparin in the pressure bags for flushing (1000 IU/L), at the beginning of the procedure a bolus of 2500–5000 IU heparin was administered. Post-procedural anticoagulation was not routinely administered, and only in exceptional cases low dose aspirin was prescribed during 3 months.
Patient demographics and treatment and aneurysm characteristics were collected. The modified Rankin Scale (mRS) at 3 months was assessed by the multidisciplinary treatment group. Angiographic follow-up was scheduled at 3 months and 3T MRI/MRA (3Tesla Magnetic Resonance Imaging/Magnetic Resonance Angiography) follow-up at 6 and 18 months. MRA follow-up was performed on a 3.0-Tesla system (Philips Intera R10, Philips Medical Systems, Best, The Netherlands) using the sensitivity encoding (SENSE) phased array head coil (MRI Devices, Gainesville, Florida, USA) according to a previously validated protocol.26
Quantitative variables were expressed with descriptive statistics, and categorical variables were expressed as frequencies or percentages with 95% confidence intervals (CIs).
Results
Patient and aneurysm characteristics are summarized in Supplementary Table 1.
Patients
Between February 2015 and June 2017, 292 aneurysms were treated with endovascular techniques at our institution. Of these, 204 (70%) were ruptured and 88 (30%) were unruptured. Of the 88 unruptured aneurysms, 57 were an incidental finding, 16 were symptomatic by mass effect and 15 were additional to another ruptured aneurysm.
Of the 88 unruptured aneurysms, 22 were selectively coiled (25%) and 66 (75%) were treated with the WEB, of which 7 with parent vessel occlusion of the internal carotid artery or vertebral artery.27
The 22 aneurysms that were selectively coiled consisted of 12 aneurysms considered too small for the WEB (1.5–4 mm) and 10 aneurysms too large with anatomy unsuitable for coiling and neck occlusion with the WEB.
Fifty-nine unruptured aneurysms in 51 patients were selectively treated with the WEB device and these patients form the subject of this study. Five patients had 2 aneurysms and one patient had 4 aneurysms treated with the WEB. Two patients with posterior communicating artery aneurysms presented with mass effect on the third cranial nerve. There were 15 men and 36 women with a mean age of 59 years (median 61, range 30–76).
Aneurysm location was middle cerebral artery in 17, anterior communicating artery in 10, basilar tip in 8, posterior communicating artery in 7, pericallosal artery in 5, carotid tip in 5, posterior inferior cerebellar artery in 2, superior cerebellar artery in 2 and ophthalmic artery, cavernous sinus and extracranial internal carotid artery each in 1. Mean aneurysm size was 7.0 mm (median 6, range 3–22). Ten aneurysms were large (≥10 mm). One large aneurysm was partially thrombosed (Figure 1) and 8 were taller than wide. In larger aneurysms, the WEB was placed in the base/neck of the aneurysm and in 4 aneurysms additional coils were placed in the fundus. Six unruptured aneurysms were treated in the same session in patients with a ruptured aneurysm. Of 59 aneurysms, 45 (76%) had a wide neck defined as ≥4 mm or dome-neck ratio ≤ 1.5 (Figures 2 and 3). No stents or supporting balloons were used.
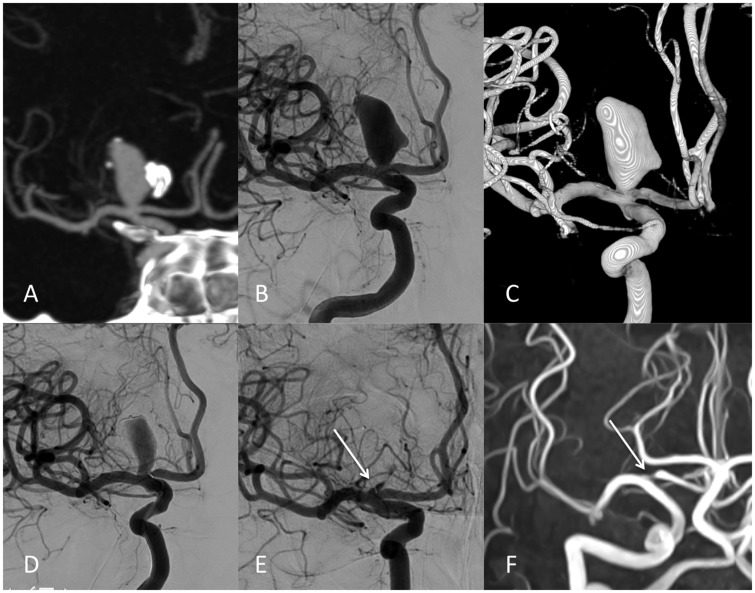
Figure 1.
63-year-old man with an incidentally discovered carotid tip aneurysm treated with the Woven EndoBridge (WEB).
(a) to (c) Coronal CT angiogram (a) and AP carotid angiogram (b) with 3D (c) shows large, partially thrombosed and calcified carotid tip aneurysm with a small neck.
(d) Immediately after WEB placement reduced filling of the aneurysm.
(e) 3 months’ follow-up angiogram shows almost complete occlusion with slide filling at the base of the WEB (arrow).
(f) MRA at 6 months. Note signal loss in A1 by WEB marker (arrow). Since the WEB behaves as a cage of Faraday possible persistent inflow in the WEB may not be visible.
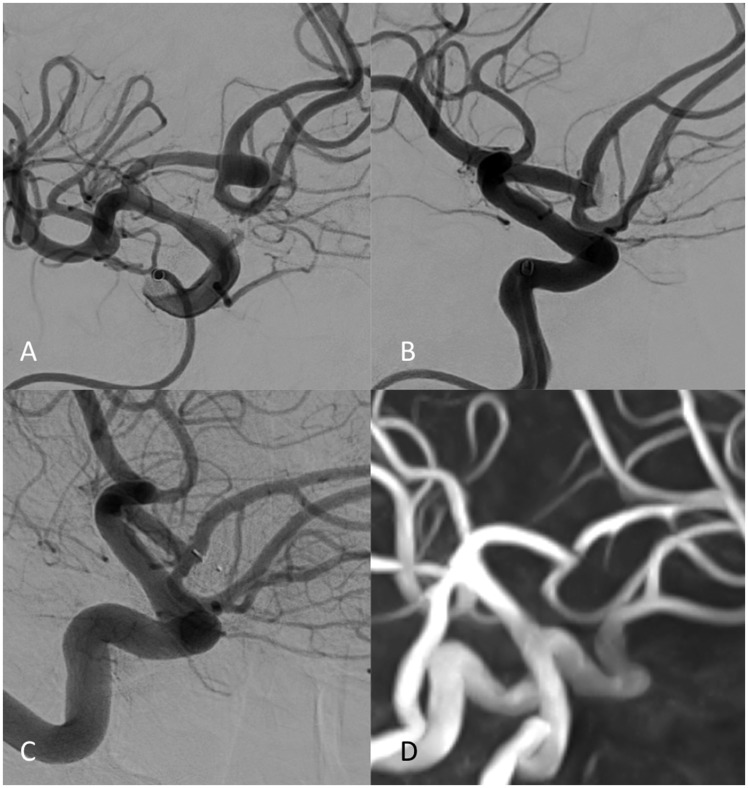
Figure 2.
52-year-old man with incidental anterior communicating artery aneurysm treated with the Woven EndoBridge (WEB).
(a) Oblique right internal carotid angiogram shows small anterior communicating artery aneurysm with wide neck.
(b) Immediately after WEB placement reduced aneurysm filling.
(c) 3 months’ follow-up angiogram shows complete occlusion.
(d) MRA at 18 months with persistent complete occlusion.
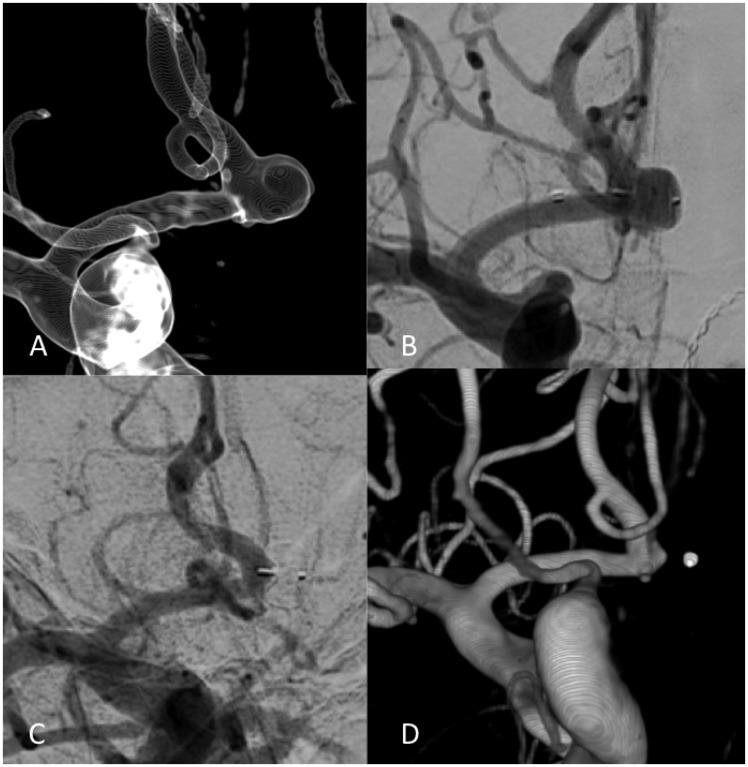
Figure 3.
64-year-old man with incidental anterior communicating artery aneurysm treated with the Woven EndoBridge (WEB).
(a) 3D carotid angiogram shows small anterior communicating artery aneurysm with very wide neck.
(b) WEB placement with complete covering of the aneurysm neck.
(c) and (d) 3 months’ follow-up angiogram (c) with 3D (d) demonstrates complete occlusion.
Initial results and complications
After WEB placement with sealing of the aneurysm neck, the position of the WEB inside the aneurysm was judged good in all 59 unruptured aneurysms.
The WEB sizes 4 and 7 mm were the most frequently used.
In one patient, an ischemic adverse event occurred; a 70-year-old woman with a 10-mm basilar tip aneurysm had a thrombotic posterior cerebral artery occlusion as a result of protrusion of the WEB over the origin of the artery. Her outcome after 3 months was mRS 4. There were no procedural ruptures. Overall complication (morbidity) rate was 2.0% (1 of 51, 95% CI 0.01–11.3%).
Clinical and imaging follow-up
In six patients, the WEB-treated unruptured aneurysm was additional to a ruptured aneurysm and was treated in the same session. One of these patients died on the sequelae of subarachnoid hemorrhage (SAH). The other five patients had mRS 2 in 3 and mRS 1 in 2 at 3 months’ follow-up, all as a result of SAH.
At 3 months, the one patient with a procedural complication had mRS 4 and the remaining 44 patients were clinically intact with mRS 0. The two patients who presented with mass effect on the oculomotor nerve were cured.
Of the 50 eligible patients, 47 with 55 aneurysms had 3 months’ angiographic follow-up. Two patients had MRA follow-up only at 3 months. The one patient with a complication refused follow-up imaging. Overall, imaging follow-up was available in 55 of 59 aneurysms (93%).
At 3 months’ imaging follow-up, 41 of 57 aneurysms (72%) were completely occluded, 12 (21%) had a neck remnant and 4 (7%) were incompletely occluded. One incompletely occluded aneurysm was a trilobular 6-mm anterior communicating artery aneurysm (patient #9). One lobe was not thrombosed on follow-up and was additionally coiled. The second incompletely occluded aneurysm was an 11-mm wide-necked V4 aneurysm in a 73-year-old woman (patient #7) and this aneurysm is being followed with imaging. The third incompletely occluded aneurysm was a 10-mm posterior communicating artery aneurysm in a 51-year-old patient (patient #57) with compression of the WEB and was additionally treated with a second WEB. The fourth patient was a 65-year-old woman (patient #19) with an 8-mm carotid tip aneurysm and a bleb on the base. At follow-up the bleb was not occluded and was additionally coiled.
Extended MRA follow-up was available in 45 patients with 52 aneurysms. In one patient with additionally clipped aneurysms, artifacts disturbed MRA. MRA follow-up ranged from 6–24 months (mean 11.6). Extended MRA follow-up showed no changes in 51 aneurysms.
Overall reopening/retreatment rate was 7.0% (4 of 57, 95% CI 2.3–17.2%).
Discussion
Our first results using the WEB as primary treatment for unruptured aneurysms are in line with other studies using WEBs or coils.5,9,12–14,16–18,21–24 In a meta-analysis by Asnafi et al.13, 15 uncontrolled series were included totaling 565 patients with 588 aneurysms treated with the WEB, of which 127 were ruptured. Initial complete and adequate occlusion rates were 27% and 59%, respectively. Midterm complete and adequate occlusion rates after a median of 7 months were 39% and 85%, respectively. Perioperative morbidity and mortality rates were 4% and 1%, respectively. Midterm adequate occlusion rates for ruptured aneurysms were 85%, compared with 84% for unruptured aneurysms. Both patients with ruptured aneurysms and patients with unruptured aneurysms had perioperative morbidity of 2%. Our results of 93% adequate occlusion at 3 months are in the same range as in this meta-analysis.
In our limited patient cohort CIs are wide and more patients are needed to confirm or refute our encouraging results concerning procedural complications and occlusion rates over time. In the study period, three-quarters of all endovascular-treated unruptured aneurysms were treated with the WEB, either selectively or with parent vessel occlusion.25 Only very small aneurysms (1.5–4 mm) or large aneurysms with anatomy unsuitable for coiling and neck occlusion with the WEB were primarily treated with coiling. Also shallow aneurysms with height/width ratio ≤0.5 were treated otherwise. Most of the treated aneurysms (76%) had a wide neck and with use of the WEB, no additional stents or balloons were needed. This was a great advantage. The anticoagulation protocol with WEB treatment was limited to periprocedural heparinization and thrombo-embolic complications did not occur.
Wide-necked aneurysms are among the most challenging aneurysms encountered for endovascular treatment. Their treatment commonly requires either craniotomy for clipping of the aneurysm or the use of implanted adjunctive devices. Such complex treatment strategies are technically demanding, time intensive, require multiple catheter manipulations, and are likely to be associated with higher complication rates.
Intrasaccular flow disruption theoretically addresses the shortcomings of established endovascular methods for the treatment of wide-necked aneurysms. The WEB allows for a single-step treatment in a procedure that is technically more similar to straightforward coil embolization than stent-assisted coiling or balloon remodeling. Once the micro catheter is placed inside the aneurysm, the deployment of the WEB is a matter of minutes. The position of the WEB can be checked with angiography and additional 3D rotational angiography when needed. Once implanted, the WEB provides a metal surface area coverage at the aneurysm neck ranging from 55% to 100%, increasing centripetally. This high metal coverage provides substantial flow disruption and forms a physical matrix for neo-intimal growth. These physical characteristics theoretically may have a favorable effect on occlusion rates and durability at follow-up. A drawback of WEB treatment is that initial occlusion cannot always be assessed since in most aneurysms there is still slow inflow of contrast material when the procedure is terminated. With 10–20 minutes pause, virtually all aneurysms will be occluded when the WEB has been placed correctly. In our practice, we end the procedure after accurate WEB placement and subsequent detachment.
The vast majority of unruptured aneurysms treated with the WEB in our cohort were adequately occluded at short- or midterm follow-up. Only four aneurysms were incompletely occluded: three aneurysms had a very unfavorable anatomy and in one large aneurysm there was compression of the WEB.10,28,29
Although the use of the WEB has some technical issues, these can readily be learned by anyone with some experience with endovascular aneurysm treatment. The procedure is more or less similar to simple coiling. Proper training on phantoms and proctoring of the first few cases can largely avoid a learning curve. We recommend first-time users to start with the simplest aneurysms with a small neck and not with wide-necked aneurysms. With growing confidence, more challenging aneurysms can be treated, sometimes surprisingly easy.
A limitation of our single-center study is the limited number of patients, keeping CIs wide. We established occlusion status of the aneurysms ourselves, not through a core laboratory . Strong points of the study are the multidisciplinary treatment with neurosurgeons and neurologists, and the complete clinical and almost complete imaging follow-up.
Conclusions
Our results indicate that WEB treatment is safe and effective in unruptured small aneurysms, regardless of neck size or location. There was no need for adjunctive devices and the anticoagulation protocol was simple and effective using heparin only. Three-quarters of all unruptured aneurysms could be treated with the WEB. In our opinion, the WEB is a valuable alternative to coils, especially in wide-necked aneurysms.
Supplemental Material
Supplemental material, Supplementary Table 1 for The Woven EndoBridge (WEB) as primary treatment for unruptured intracranial aneurysms by Sanne BT van Rooij, Willem Jan van Rooij, Jo P Peluso and Menno Sluzewski in Interventional Neuroradiology
Declaration of conflicting interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Prof. Dr WJJ van Rooij: consultant of MicroVention; Dr. Jo Peluso: consultant of MicroVention; Dr. M. Sluzewski: no disclosures.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr SBT van Rooij: recipient of unrestricted institutional grant from MicroVention covering 20% of resident salary during 2 years for scientific research.
References
- 1.Piotin M, Blanc R, Spelle L, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke 210; 41: 110–115. [DOI] [PubMed]
- 2.Bartolini B, Blanc R, Pistocchi S, et al. “Y” and “X” stent-assisted coiling of complex and wide-neck intracranial bifurcation aneurysms. AJNR Am J Neuroradiol 2014; 35: 2153–2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chalouhi N, Jabbour P, Singhal S, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke 2013; 44: 1348–1353. [DOI] [PubMed] [Google Scholar]
- 4.Chung J, Lim YC, Suh SH, et al. Stent-assisted coil embolization of ruptured wide-necked aneurysms in the acute period: incidence of and risk factors for periprocedural complications. J Neurosurg 2014; 121: 4–11. [DOI] [PubMed] [Google Scholar]
- 5.Armoiry X, Turjman F, Hartmann DJ, et al. Endovascular treatment of intracranial aneurysms with the WEB device: a systematic review of clinical outcomes. AJNR Am J Neuroradiol 2016; 37: 868–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sivan-Hoffmann R, Gory B, Riva R, et al. One-year angiographic follow-up after WEB-SL endovascular treatment of wide-neck bifurcation intracranial aneurysms. AJNR Am J Neuroradiol 2015; 36: 2320–2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawson A, Goddard T, Ross S, et al. Endovascular treatment of cerebral aneurysms using the Woven EndoBridge technique in a single center: preliminary results. J Neurosurg 2017; 126: 17–28. [DOI] [PubMed] [Google Scholar]
- 8.Leyon JJ, Chavda S, Lamin S, et al. Corking the WEB and coiling through a jailed microcatheter: WEB assisted coiling, a useful technique avoiding the use of stents in treating wide-necked large intracranial aneurysms. J Neurointerv Surg 2016; 8: e18. [DOI] [PubMed] [Google Scholar]
- 9.Lawson A, Molyneux A, Sellar R, et al. Safety results from the treatment of 109 cerebral aneurysms using the Woven EndoBridge technique: preliminary results in the United Kingdom. J Neurosurg 2018; 128: 144–153. [DOI] [PubMed] [Google Scholar]
- 10.Caroff J, Mihalea C, Tuillier T, et al. Occlusion assessment of intracranial aneurysms treated with the WEB device. Neuroradiology 2016; 58: 887–891. [DOI] [PubMed] [Google Scholar]
- 11.Gherasim DN, Gory B, Sivan-Hoffmann R, et al. Endovascular treatment of wide-neck anterior communicating artery aneurysms using WEB-DL and WEB-SL: short-term results in a multicenter study. AJNR Am J Neuroradiol 2015; 36: 1150–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fiorella D, Molyneux A, Coon A, et al. Demographic, procedural and 30-day safety results from the WEB Intra-saccular Therapy Study (WEB-IT). J Neurointerv Surg 2017; 9: 1191–1196. [DOI] [PubMed] [Google Scholar]
- 13.Asnafi S, Rouchaud A, Pierot L, et al. Efficacy and safety of the Woven EndoBridge (WEB) device for the treatment of intracranial aneurysms: a systemic review and meta-analysis. AJNR Am J Neuroradiol 2016; 37: 2287–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pierot L, Moret J, Turjman F, et al. WEB treatment of intracranial aneurysms: clinical and anatomic results in the French Observatory. AJNR Am J Neuroradiol 2016; 37: 655–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Rooij WJ, Peluso JP, Bechan RS, et al. WEB treatment of ruptured intracranial aneurysms. AJNR Am J Neuroradiol 2016; 37: 1679–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Rooij SB, van Rooij WJ, Peluso JP, et al. WEB treatment of ruptured intracranial aneurysms: a single center cohort of 100 patients. AJNR Am J Neuroradiol 2017; 38: 2282–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierot L, Spelle L, Molyneux A, et al. Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2016; 78: 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016; 124: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 19.Clajus C, Strasilla C, Fiebig T, et al. Initial and mid-term results from 108 consecutive patients with cerebral aneurysms treated with the WEB device. J Neurointerv Surg 2017; 9: 411–417. [DOI] [PubMed] [Google Scholar]
- 20.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017; 38: 1151–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lubicz B, Klisch J, Gauvrit JY, et al. WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: short- and midterm results in a European study. AJNR Am J Neuroradiol 2014; 35: 432–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liebig T, Kabbasch C, Strasilla C, et al. Intrasaccular flow disruption in acutely ruptured aneurysms: a multicenter retrospective review of the use of the WEB. AJNR Am J Neuroradiol 2015; 36: 1721–1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Popielski J, Berlis A, Weber W, et al. Two-center experience in the endovascular treatment of ruptured and unruptured aneurysms using the WEB device: a retrospective analysis. AJNR Am J Neuroradiol 2018; 39: 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferns SP, Sprengers ME, van Rooij WJ, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke 2009; 40: e523–529. [DOI] [PubMed] [Google Scholar]
- 25.van Rooij SB, Peluso JP, Sluzewski M, et al. The new low-profile WEB 17 system for treatment of intracranial aneurysms: first clinical experiences. AJNR Am J Neuroradiol. Epub ahead of print 22 March 2018. DOI: 10.3174/ajnr.A5608. [DOI] [PMC free article] [PubMed]
- 26.Majoie CB, Sprengers ME, van Rooij WJ, et al. MR angiography at 3T versus digital subtraction angiography in the follow-up of intracranial aneurysms treated with detachable coils. AJNR Am J Neuroradiol 2005; 26: 1349–1356. [PMC free article] [PubMed] [Google Scholar]
- 27.van Rooij WJ, Sluzewski M, Bechan R, et al. Therapeutic internal carotid or vertebral artery occlusion using the WEB device. Interv Neuroradiol 2016; 22: 365–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pierot L. Letter: WEB aneurysm treatment: occlusion stability and “compression”. Neurosurgery 2015; 77: E666–667. [DOI] [PubMed] [Google Scholar]
- 29.Cognard C, Januel AC. Remnants and recurrences after the use of the WEB intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015; 76: 522–530. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary Table 1 for The Woven EndoBridge (WEB) as primary treatment for unruptured intracranial aneurysms by Sanne BT van Rooij, Willem Jan van Rooij, Jo P Peluso and Menno Sluzewski in Interventional Neuroradiology