Abstract
This article describes the successful endovascular treatment of a dural arteriovenous fistula of a rare localization (the area of sphenoid bone lesser region). We examine one report of an unusually located dural arteriovenous fistula successfully treated with Onyx (ev3, Irvine, USA) using a combination of endovascular adjuvant techniques: pressure cooker and remodeling balloon protection of cerebral artery. The article includes previously published observations of such fistulas and discusses anatomic features and venous drainage of dural arteriovenous fistulas in the given location.
Keywords: Arteriovenous malformation, endovascular treatment, Onyx, technical aspects
Introduction
Intracranial dural arteriovenous fistula (DAVF) is a pathological connection between the branches of meningeal arteries and venous sinuses and/or pial vessels of the cerebrum.1, 2 Characteristics of venous drainage and, subsequently, severity of venous hypertension are major factors that determine its clinical presentation and natural course. The most common locations for DAVF are the superior sagittal sinus (SSS) and transversus sinuses, whereas other locations are less frequent.1
This article is a case report of a rare DAVF in the region of the lesser sphenoid wing successfully treated by a combination of endovascular adjuvant techniques. There was simultaneous temporary balloon occlusion of the internal carotid artery (ICA) with transarterial Onyx injection through the middle meningeal artery using the ‘pressure cooker’ technique. To our knowledge, this is the first case of a DAVF in this region being treated with such a combination of techniques.
The discussion includes a literature review regarding the diagnosis and treatment of DAVF in the region of the lesser sphenoid wing. It contains а description of the DAVF’s anatomic features, which determine the clinical presentation.
Case report
A 27-year-old male presented with a 3-month history of acute left-side headache.
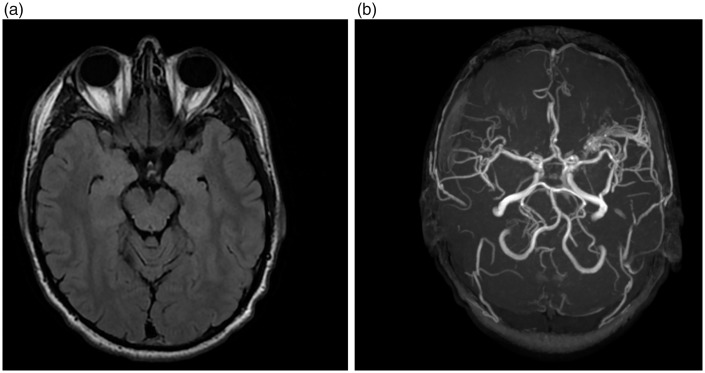
Clinical examination was completely normal. Magnetic resonance imaging demonstrated a DAVF in the left-side lesser wing of sphenoid bone, draining into the cortical veins (Figure 1). It should be noted that there was no history of previous head trauma or neurosurgical procedure.
Figure 1.
Magnetic resonance imaging (MRI) data. (a) Lack of significant changes in the left side lesser wing of sphenoid bone at T1- and T2-weighted MRI. (b) Non-enhanced magnetic resonance angiography (3D-TOF) reveals a dural arteriovenous fistula.
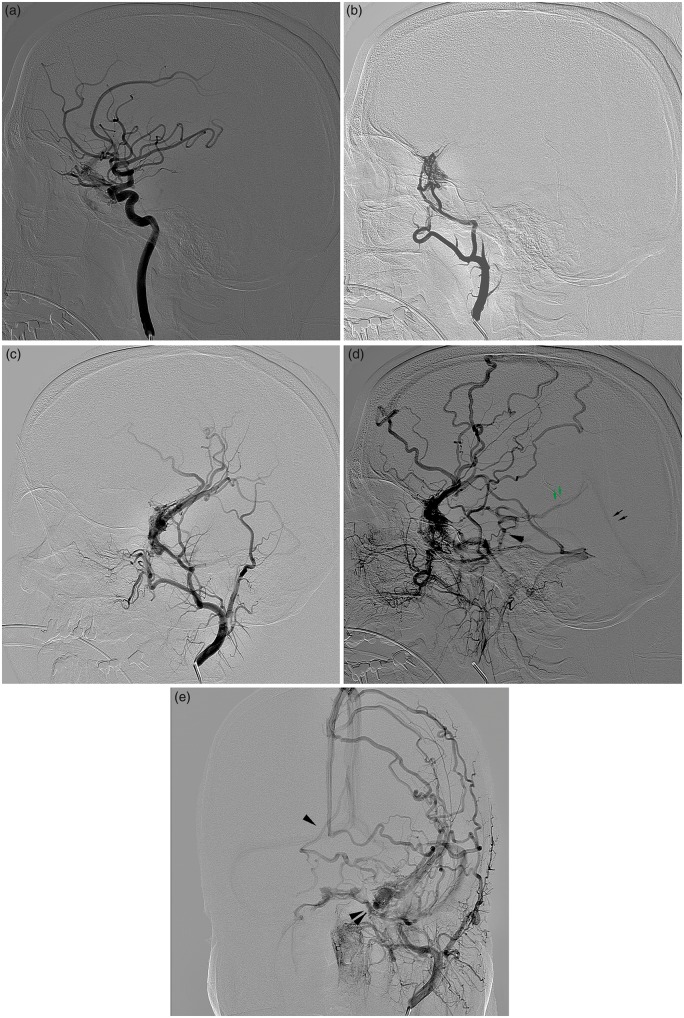
The diagnosis was confirmed by digital subtraction angiography, which showed a DAVF fed by branches arising from the left middle meningeal and the recurrent meningeal branch of the left ophthalmic artery. There were also additional branches from the inferolateral trunk of the left ICA, which participated in the supply of the DAVF. The fistula drained directly into the left superficial middle cerebral vein, spreading both in the superficial cortical veins and further in the SSS, as well as the paracavernous sinus with further outflow into the cavernous and superior petrosal sinuses. The sphenoparietal sinus in the fistula region was not observed, presumably due to previous reduction. There was retrograde filling into deep cerebral veins with reflux into the right basal vein of Rosenthal via peduncular veins. Some features of basal vein anatomy were identified: a lack of the second and third segment of the left basal veinof Rosenthal, with a reflux into the right basal vein via the left superior petrosal sinus: sinus ► left mesencephalic vein ► peduncular vein ► right vein of Rosenthal (Figure 2). The presence of DAVF with the drainage into dilated cortical veins (III–IV type DAVF according to Cognard et al.)2 was the indication for endovascular treatment.
Figure 2.
Dural arteriovenous fistula (DAVF) of the lesser sphenoid wing. (a) Dural arteriovenous shunts fed by recurrent meningeal branch from the ophthalmic artery and branches from the inferolateral trunk of the internal carotid artery. (b) DAVF fed by branches arising from the left middle meningeal artery. Drainage into the superficial cortical veins with varix. (c) DAVF fed by branches arising from the left middle meningeal artery. Drainage into the superficial cortical veins with varix. (d) Venous drainage through superficial cerebral veins into SSS, paracavernous and superior petrosal sinuses. Retrograde filling into deep cerebral veins with reflux into the basal vein of Rosenthal via mesencephalic and peduncular veins, absence of the left of Rosenthal. (e) Venous drainage through superficial cerebral veins into SSS, paracavernous and superior petrosal sinuses. Retrograde filling into deep cerebral veins with reflux into the right basal vein of Rosenthal via mesencephalic and peduncular veins into the right vein of Rosenthal, absence of the left vein of Rosenthal.
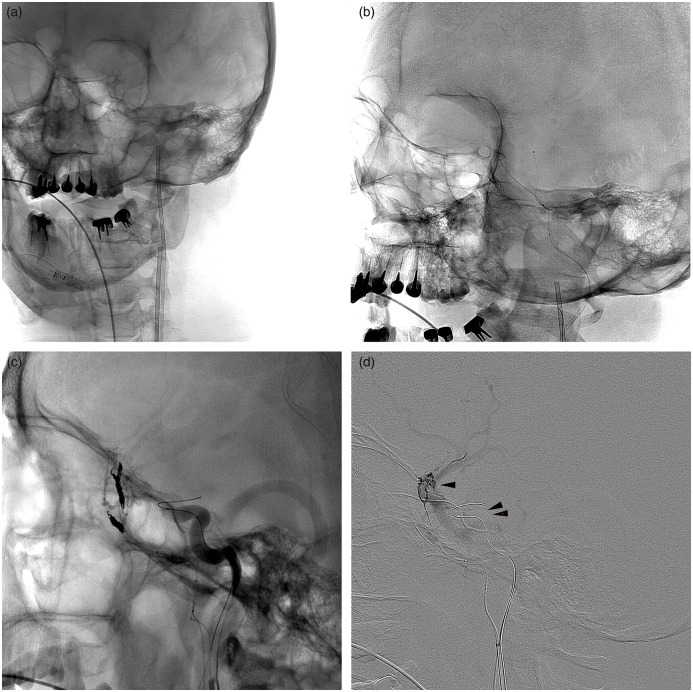
The procedure was performed under general anesthesia. The bilateral femoral approach was used and 6F guide catheters were sequentially placed in the left ICA and external carotid artery (ECA). Microcatheter Apollo 1.5 F-5.0 (ev3, Irvine, USA) was advanced over 0.007 inch microguidewire (Hybrid, Balt Extrusion, France) in the left frontal branch of the middle meningeal artery up to the fistulous zone.
To eliminate concurrent blood flow, the parietal branch of the middle meningeal artery was occluded with coils (Target, Stryker Neurovascular, Fermont, USA) through an Excelsior SL-10 microcatheter (Stryker Neurovascular, Fermont, USA). The coils were then placed distally from the detachment point of the Apollo microcatheter tip to isolate the DAVF from the ECA and ‘lock’ the working microcatheter: the pressure cooker technique. To eliminate concurrent blood flow and avoid inadvertent reflux of Onyx into the ICA lumen via dural arterial branches, a 4 × 30 mm Hyperglide balloon (ev3, Irvine, USA) was navigated into the left ICA and temporarily inflated at the level of the cavernous segment and ophthalmic artery origin.
In total, 4 ml of a non-adhesive liquid embolic agent Onyx 18 (ev3, Irvine, USA) was injected within the DAVF. An immediate control angiogram showed complete DAVF obliteration with preservation of the patency of the ophthalmic artery. The Apollo microcatheter was removed by detachment at the nominal separation point (Figure 3).
Figure 3.
Introduction of microcatheter Apollo 1.5F-5.0 into the frontal branch of the middle meningeal artery and Excelsior SL-10 microcatheter into the parietal branch. (a) Placing of two guider catheters into the external carotid artery (ECA) and internal carotid artery (ICA). (b and c) Embolization of frontal branches of the middle meningeal artery distally from the detachment point of the Apollo microcatheter. (d) Superselective angiography. The superficial middle cerebral vein is enhanced. (e) Embolization of the fistula with non-adhesive liquid embolic agent Onyx 18 in a temporary balloon occlusion of the ICA, which was temporarily inflated at the level of the cavernous segment and ophthalmic artery origin to eliminate concurrent blood flow and avoid inadvertent reflux of Onyx into the ICA. (f, g, h) A radical occlusion of DAVF, preserving the patency of the ophthalmic artery. (i) No filling of DAVF from the ECA.
The postoperative course was uneventful. No visual impairment was detected. The patient was discharged on the second day after the operation.
Discussion
Currently, there are fewer than 20 case reports of a DAVF in the sphenoid bone lesser wing area.1–14 The fistula is fed by branches of the ECA (middle and accessory meningeal arteries) and by the ICA (branches of the inferolateral trunk, recurrent meningeal branch of the ophthalmic artery). The location and anatomical relationship between the two venous systems (superficial middle cerebral vein and sphenoparietal sinus) determine the characteristics of venous drainage.
The sphenoparietal sinus was first mentioned by Gilbert Breschet in the early 19th century. He considered it a single venous channel running from the superior sagittal sinus to the sphenoid bone lesser region.15 However, San Millan Ruız et al. considered this description inaccurate. According to anatomical studies, the sphenoparietal sinus is not a single venous cavity between the layers of the dura mater located between the SSS and the cavernous sinus.5 It would be more correct to describe it as two connected parts with different structures: the parietal part, represented by the anterior (frontal) portion of the middle meningeal vein, and the true dural sinus, located on the lesser wing of the sphenoid bone. The dural sinus of the sphenoid bone lesser wing connects laterally to the anterior branch of the middle meningeal vein and runs medially into the anterior-superior part of the cavernous sinus. The orbital and diploic veins of the orbital roof run into the dural sinus of the lesser wing. In fact, the sphenoparietal sinus is a restricted venous cavity located only on the lesser wing of the sphenoid bone. Therefore, it would be more appropriate to refer to it as a sinus of the sphenoid bone lesser wing.5,9 Trolard also gives a similar description of the sinus.16
It is generally believed that the superficial middle cerebral vein runs into the sinus of the sphenoid bone lesser wing.17 But, according to San Millan Ruiz et al., this vein is essentially a separate venous collector, with drainage into the cavernous, paracavernous or laterocavernous sinuses.18–20 Thus, blood flow of the sphenoparietal sinus and the superficial middle cerebral vein do not mix. However, Tanoue and Suzuki noted the possibility that the superficial middle cerebral vein and sinus of the sphenoid bone lesser wing merge just before they enter the cavernous sinus.17, 18 It should be taken into account that the authors assessed the anatomical variations in the structure using the data of the magnetic resonance angiography or Computer Tomography Angiography (CTA), which may have had an impact on the findings.
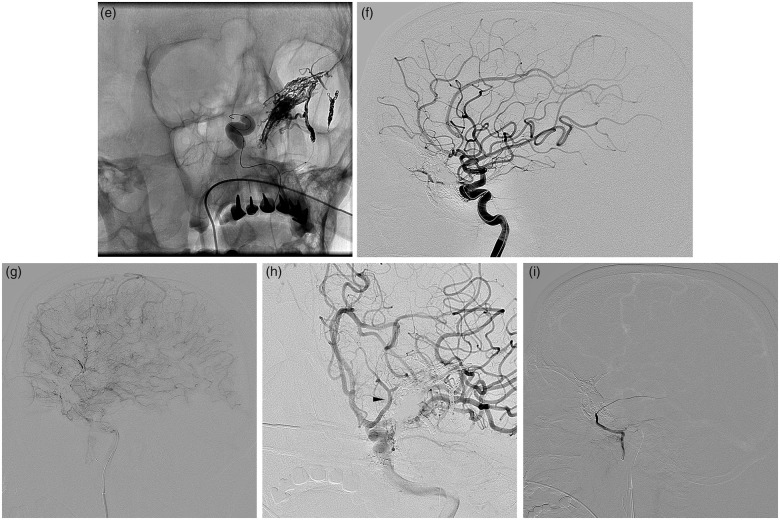
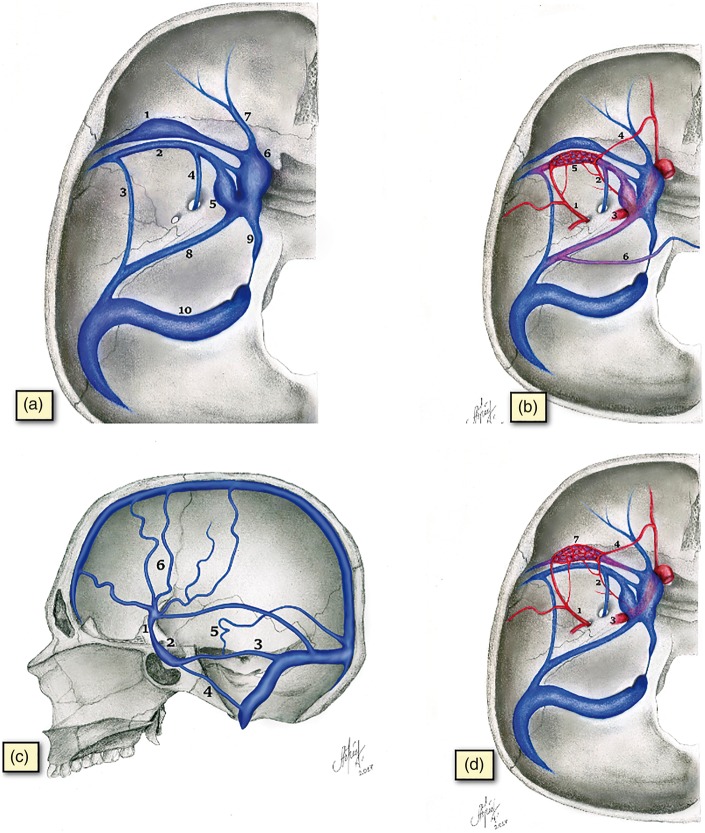
Knowledge of the topographical peculiarities of these venous reservoirs is of fundamental importance both for estimating the exact location of the dural fistula in the sphenoid bone lesser region and for determining the natural course. The fistula of а superficial middle cerebral vein drains into the cortical (superficial and deep) veins of the brain, thereby causing a disturbance in the venous outflow with a high risk of hemorrhage.1,6 DAVF of the sphenoparietal sinus are characterized by an asymptomatic course or manifestation, typical of fistulas of the cavernous sinus area.5–7 Figure 4 shows the topography of venous collectors in the sphenoid bone lesser wing area and the venous drainage pathways, as well as a schematic representation of the fistula in the sphenoid bone lesser wing area and the superficial middle cerebral vein.
Figure 4.
Topographical and anatomical relationships between venous structures in the lesser sphenoid wing region. Normal venous drainage vs. in presence of an arteriovenous fistula (AV-fistula). (a) The anatomy of the venous system in the lesser sphenoid wing region and normal venous drainage pathways. (1) Dural sinus of the lesser sphenoid wing. (2) Superficial middle cerebral vein. (3) An example of SMCV drainage into the superior petrosal sinus (sphenopetrosal sinus). (4) An example of SMCV drainage into the pterygopalatine plexus through the foramen rotundum. (5) Paracavernous sinus. (6) Cavernous sinus. (7) Superior orbital vein. (8) Superior petrosal sinus. (9) Inferior petrosal sinus. (10) Sigmoid sinus. (b) AV-fistula of the superficial middle cerebral vein. (1) Middle meningeal artery. (2) Branches of the inferolateral trunk of the internal carotid artery (ICA). (3) The ICA. (4) Recurrent meningeal branch of the ophthalmic artery. (5) AV-fistula of superficial middle cerebral vein. (6) Venous drainage into the basal veins via the lateral mesencephalic and peduncular veins to the opposite vein of Rosenthal. (7) AV-fistula in the sinus region of the lesser sphenoid wing. (c) Venous drainage pathways of arteriovenous fistula of the superficial middle cerebral vein. (1) Superficial middle cerebral vein. (2) Cavernous sinus. (3) Superior petrosal sinus. (4) Inferior petrosal sinus. (5) Venous drainage into the deep veins of the brain. (6) Drainage into the superficial cortical veins. (d) AV-fistula of the lesser sphenoid wing. (1) Middle meningeal artery. (2) Branches of the inferolateral trunk of the ICA. (3) The ICA. (4) Recurrent meningeal branch of the ophthalmic artery. (5) AV-fistula of superficial middle cerebral vein. (6) Venous drainage into the basal veins via the lateral mesencephalic and peduncular veins to the opposite vein of Rosenthal. (7) AV-fistula in the sinus region of the lesser sphenoid wing.
We also should mention the ways of retrograde filling into the deep veins in our case report. According to previously published reports, reflux into the basal vein on the side of the fistula was conducted via retrograde flow through the lateral mesencephalic vein or anterior pontomesencephalic vein, whereas reflux through the peduncular veins was conducted into the opposite basal vein.5–7 In our case, the fistula was draining into the opposite vein, which is due to the absence of the second and third segment of the left vein of Rosenthal.
DAVF treatments include microsurgical and endovascular intervention and stereotactic radiosurgery. Introduction of a non-adhesive liquid embolic agent has significantly increased the efficiency of endovascular treatment. However, poliafferent fistulas decrease the possibility of complete occlusion due to the presence of a concurrent blood flow that prevents the embolic agent penetrating into the arteriovenous shunt. In this case, the described strategy achieved deep penetration of the liquid implant into the DAVF, at the same time eliminating the risk of embolic agent reflux into the ICA.
The search for publications on DAVF in the sphenoid bone lesser wing region was performed using the PubMed database. We were able to find 13 publications, reporting a total 18 cases of DAVF in the given location.1–14 The analysis of published cases allowed us to divide these clinical observations into fistulas of the sphenoid bone lesser wing sinus and the superficial middle cerebral vein (Table 1), based on the pattern of venous drainage. In two cases, direct drainage to the basal vein was noted. These cases can be regarded as the equivalent of fistulas of the superficial middle cerebral vein, as according to Watabe et al. (2015) occlusion of the proximal segment of the basal vein can lead to reflux into the superficial medial cerebral vein.11
Table 1.
Published cases of the lesser sphenoid wing region DAVF.
| No. | Author, year | Gender/ age, y | Clinical features | Location | Drainage | Presence of varix | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Bitoh S et al., 19802 | M, 14 | Exophthalmos, ophthalmoparese | Lesser sphenoid wing sinus | Cavernous sinus, superior orbital vein, pterygopalatine plexus | No | Ligation of external carotid artery + surgical disconnection |
| 2 | Tsutsumi et al., 19903 | F, 35 | Postoperative AV-fistula | Lesser sphenoid wing sinus | Cavernous sinus | No | Spontaneous thrombosis |
| 3 | Ezura et al., 19964 | M, 45 | Transient global amnesia | Superficial middle cerebral vein | Superficial and deep middle cerebral vein, basal veins | Yes | Embolization + surgical disconnection |
| 4 | San Millan Ruiz et al., 20045 | M, 47 | Headache | Superficial middle cerebral vein | Superficial and deep middle cerebral vein, basal veins | Yes | Embolization + surgical disconnection |
| 5 | Rezende, 20066 | M, 45 | Headache | Superficial middle cerebral vein | Superficial and deep middle cerebral vein, basal veins | Yes | Embolization |
| 6 | Khadavi et al., 20097 | M, 54 | Visual deterioration, glaucoma | Lesser sphenoid wing sinus | Cavernous sinus, superior orbital vein | No | Embolization |
| 7 | Shi et al., 20139 | Unknown | Unknown | Superficial middle cerebral vein | Lateral and superior sagittal sinus | Yes | Unknown |
| 8 | Shi et al., 20139 | Unknown | Unknown | Lesser sphenoid wing sinuses. | Cavernous sinus and superior orbital vein | No | Unknown |
| 9 | Shi et al., 20139 | Unknown | Unknown | Lesser sphenoid wing sinuses. | Cavernous sinus and superior orbital vein | No | Unknown |
| 10 | Shi et al., 20139 | Unknown | Unknown | Lesser sphenoid wing sinuses. | Pterygopalatine plexus | No | Unknown |
| 11 | Shi et al., 20139 | Unknown | Unknown | Lesser sphenoid wing sinuses. | Middle meningeal vein | No | Unknown |
| 12 | Tanaka et al., 20128 | M, 61 | Loss of visual field (infarction of the occipital lobe) | Superficial middle cerebral vein | Superficial middle cerebral vein, basal vein | Yes | Surgical disconnection |
| 13 | Osbun et al., 201314 | M, 55 | Right-sided homonymous hemianopsia | Basal vein* | Basal vein. | Yes | Embolization |
| 14 | Fukuda et al., 201410 | M, 44 | Headache | Superficial middle cerebral vein | Superficial middle cerebral vein, lateral sinus | Yes | Embolization |
| 15 | Fukuda et al., 201410 | M, 58 | Dizziness | Superficial middle cerebral vein | Superficial middle cerebral vein, basal vein | Yes | Embolization |
| 16 | Watanabe et al., 201511 | M, 69 | Asymptomatic progression | Basal vein* | Basal vein. | Yes | Surgical disconnection |
| 17 | Murakami et al., 201712 | M, 68 | Headache | Superficial middle cerebral vein | Superficial and middle cerebral vein, basal veins | Yes | Embolization |
| 18 | Nakajima et al., 201713 | M, 71 | Haemorrhage | Superficial middle cerebral vein | Superficial and deep middle cerebral vein, basal veins | Yes | Surgical disconnection |
| 19 | This case report | M, 24 | Headache | Superficial middle cerebral vein | Superficial middle cerebral vein, right basal vein | Yes | Embolization |
Two case reports of AV-fistulas in the lesser sphenoid wing region with drainage exclusively into the basal vein can be considered equivalent to the AV-fistula of the superficial middle cerebral vein. For example, according to Watanabe et al. (2015) an exclusion of the bridging vein, which was draining into the basal vein, in direct proximity to the confluence led to a change in the blood flow, redirecting the reflux into the superficial medial cerebral vein.11
F: female; M: male.
Conclusion
DAVF in the sphenoid bone lesser wing region are formed in the setting of a complex relationship between a number of adjacent large venous reservoirs and arterial trunks. A thorough evaluation of venous drainage allows the identification of precise fistula anatomy and thus determination of the optimal treatment options. Drainage into the superficial and deep veins of the brain and the presence of varicosity are typical for fistulas of the superficial middle cerebral vein. Clinical presentation of the sphenoparietal sinus DAVF is similar to that of the cavernous sinus fistula. An intravascular intervention using a non-adhesive liquid embolic agent allows the achievement of complete occlusion of the fistula.
Author contributorship
KVD, BKN, SDV conceived and designed the work. BKN, SDV and SAV acquired data. All authors analysed and interpreted data. BKN approved the final version of the manuscript on behalf of all authors. All authors critically revised the article and provided administrative, technical and material support.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Cognard C, Gobin YP, Pierot L, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology 1995; 194: 671–680. [DOI] [PubMed] [Google Scholar]
- 2.Bitoh S, Arita N, Fujiwara M, et al. Dural arteriovenous malformation near the left sphenoparietal sinus. Surg Neurol 1980; 13: 345–349. [PubMed] [Google Scholar]
- 3.Tsutsumi K, Shiokawa Y, Kubota M, et al. Postoperative arteriovenous fistula between the middle meningeal artery and sphenoparietal sinus. Neurosurgery 1990; 26: 869–870. [DOI] [PubMed] [Google Scholar]
- 4.Ezura M, Takahashi A, Mizoi K. Dural arteriovenous shunts involving the sphenoparietal sinus. A case report. Interv Neuroradiol 1996; 2: 223–228. [DOI] [PubMed] [Google Scholar]
- 5.San Millán Ruíz D, Ruíz D, Fasel JH, et al. The sphenoparietal sinus of breschet: Does it exist? An anatomic study. AJNR Am J Neuroradiol 2004; 25: 112–120. [PMC free article] [PubMed] [Google Scholar]
- 6.Rezende MT, Piotin M, Mounayer C, et al. Dural arteriovenous fistula of the lesser sphenoid wing region treated with Onyx: Technical note. Neuroradiology 2006; 48: 130–134. [DOI] [PubMed] [Google Scholar]
- 7.Khadavi NM, Mancini R, Nakra T, et al. Rare dural arteriovenous fistula of the lesser sphenoid wing sinus. Ophthal Plast Reconstr Surg 2009; 25: 404–406. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka T, Kato N, Arai T, et al. Surgical treatment of a sylvian-middle fossa dural arteriovenous fistula draining into the basal vein of Rosenthal with frontotemporal craniotomy. J Stroke Cerebrovasc Dis 2012; 21: 333–337. [DOI] [PubMed] [Google Scholar]
- 9.Shi ZS, Ziegler J, Feng L, et al. Middle cranial fossa sphenoidal region dural arteriovenous fistulas: Anatomic and treatment considerations. AJNR Am J Neuroradiol 2013; 34: 373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fukuda H, Miyake K, Kunieda T, et al. Endovascular treatment of sphenoid wing dural arteriovenous fistula with pure cortical venous drainage. J Stroke Cerebrovasc Dis 2014; 23: 1730–1735. [DOI] [PubMed] [Google Scholar]
- 11.Watanabe J, Maruya J, Nishimaki K. Surgical treatment of a dural arteriovenous fistula in the sphenoid wing with unique drainage pattern through the basal vein of Rosenthal. NMC Case Rep J 2015; 2: 88–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murakami T, Nakamura H, Nishida T, et al. Transarterial sinus embolization for a dural arteriovenous fistula in a sinus of the lesser sphenoid wing: A case report. NMC Case Rep J 2017; 4: 47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakajima H, Ishiguro T, Terada A, et al. Dural arteriovenous fistula of the sinus of the lesser sphenoid wing presenting with pontine hemorrhage. World Neurosurg 2017; 98: 871.e17–871.e21. [DOI] [PubMed] [Google Scholar]
- 14.Osbun JW, Kim LJ, Spetzler RF, et al. Aberrant venous drainage pattern in a medial sphenoid wing dural arteriovenous fistula: A case report and review of the literature. World Neurosurg 2013; 80: e381–6. [DOI] [PubMed] [Google Scholar]
- 15.Breschet G (1892) Recherches anatomiques, physiologiques sur le systeme veineux et specialement sur les canaux veineux des os. Villeret et Rouen, Paris, p. 1–42.
- 16.Trolard P. Les veines meninges moyennes. Rev Sci Biol 1890, pp. 485–499. [Google Scholar]
- 17.Suzuki Y, Matsumoto K. Variations of the superficial middle cerebral vein: Classification using three-dimensional CT angiography. AJNR Am J Neuroradiol 2000; 21: 932–938. [PMC free article] [PubMed] [Google Scholar]
- 18.Tanoue S, Kiyosue H, Okahara M, et al. Para-cavernous sinus venous structures: Anatomic variations and pathologic conditions evaluated on fat-suppressed 3D fast gradient-echo MR images. AJNR Am J Neuroradiol 2006; 27: 1083–1089. [PMC free article] [PubMed] [Google Scholar]
- 19.Lv X, Jiang C, Li Y, et al. The laterocavernous sinus system: Venous inflows, venous outflows, and clinical significance. World Neurosurg 2011; 75: 90–93; discussion 34–35. [DOI] [PubMed] [Google Scholar]
- 20.Gailloud P, San Millán Ruíz D, Muster M, et al. Angiographic anatomy of the laterocavernous sinus. AJNR Am J Neuroradiol 2000; 21: 1923–1929. [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki Y, Ikeda H, Shimadu M, et al. Variations of the basal vein: Identification using three-dimensional CT angiography. AJNR Am J Neuroradiol 2001; 22: 670–676. [PMC free article] [PubMed] [Google Scholar]
- 22.Chapot R, Stracke P, Velasco A, et al. The pressure cooker technique for the treatment of brain AVMs. J. Neuroradiol 2014; 41: 87–91. [DOI] [PubMed] [Google Scholar]