Abstract
Breakfast is considered by many to be the most important meal of the day. This study examined the intake of nutrients and foods at breakfast among Danes and the relation to the overall dietary quality. Data were derived from the Danish National Survey on Diet and Physical Activity 2011–2013, a cross-sectional national food consumption study. A total of 3680 participants aged 6–75 years were included in the analyses of breakfast consumption. The Nutrient Rich Food Index 9.3 method was used to examine the overall dietary quality of the diet. The intake of nutrients and foods at breakfast were compared across dietary quality score tertiles by ANCOVA adjusted for energy and socio economic status. Breakfast was eaten frequently by children and adults and contributed with 18–20% of total energy intake. Breakfast was relatively high in dietary fibre, B vitamins, calcium and magnesium and low in added sugar, total fat, sodium, vitamin A and D. A decrease in the intake of added sugar, total fat and saturated fat and an increase in the intake of dietary fibre and most micronutrients were seen across tertiles of dietary quality scores. Commonly consumed foods provided at breakfast in Denmark included bread, breakfast cereals and dairy products as well as water, coffee and juice, while intakes of fruits, vegetables, cakes and soft drinks were low.
Keywords: Breakfast, dietary intake, foods, nutrition, dietary quality, NRF 9.3, index
1. Introduction
It is often stated that breakfast is the most important meal of the day and this has been integrated into the public mindset [1,2]. Recommendations on the intake of meals, foods, and nutrients in Denmark are based on the Nordic Nutrition Recommendations and the Danish food-based dietary guidelines (FBDG). The Danish FBDG do not mention when and how much breakfast should be eaten. Previously, the Nordic Nutrition Recommendations (NNR 2004) suggested that breakfast should account for 20–25% of the total energy intake [3]. However, the latest version of the NNR does not include recommendations on the proportion of energy from breakfast [4]. Thus, there is no official Danish or Nordic recommendation for energy and macro- and micronutrient intakes at breakfast.
The Danish Veterinary and Food Administration have a few recommendations for the timing of breakfast consumption. It is emphasized that skipping breakfast can have a negative influence on cognitive capacity and children, in particular, can have difficulty in reaching an adequate intake of daily nutrients [5]. The Danish FBDG only include a minor emphasis on specific meal based recommendations. One example is through the public-private partnership with the aim of increasing the intake of whole grain in the Danish population [6]. The Danish Whole Grain Partnership emphasizes that breakfast (and dinner) presents the greatest potential for an increased intake of whole grain [6,7].
The typical meal pattern in Denmark consists of three main meals and two to three in-between-meals. Breakfast is typically based on the intake of bread or breakfast cereals and dairy products. The intake of fruits, vegetables, fish, meat, and cakes are seldom consumed at breakfast. Water, milk, coffee, and juice are typically consumed at breakfast [8,9].
Eating breakfast compared with skipping the meal is associated with improved dietary quality [10,11]. Irregular breakfast consumption compared with regular consumption has been associated with e.g., cardiovascular diseases [12], type 2 diabetes [13,14,15], and body weight [16]. Further, breakfast consumption has a positive effect on cognitive performance in children and adolescents when compared with skipping the breakfast meal [17]. The literature on breakfast consumption has been summarized in a recent systematic review concluding that there is limited evidence of breakfast consumption being an important factor in combined weight and cardiometabolic risk management, but breakfast consumption can contribute to a healthier eating pattern [18].
In Denmark, few studies have been conducted on meal regularity and health and most studies on breakfast have described the breakfast consumption patterns according to age, gender, and socioeconomic status (SES) [9,19,20,21].
A multi-site randomized controlled trial including Danish participants tested the effectiveness of a recommendation to eat or skip breakfast on weight loss in adults. The authors concluded that the consumption of breakfast had no effect on weight loss [19]. The “Diet, Smoking, Alcohol and Exercise” (KRAM) study is the largest national health study of the Danish adult population, with 18,065 adults participating in a health examination [20]. The study examined the daily meal pattern of the participants and found that 82% of respondents reported eating breakfast every day and more women than men consumed breakfast regularly. Adolescents and young adults (18–24 years) had the most irregular breakfast patterns. The higher the education, the more regular breakfast patterns were seen. Those not eating breakfast every day had a higher intake of total fat, saturated fat and added sugar than those with more regular breakfast-eating patterns [20]. The World Health Organization’s (WHO) Study on Health Behaviour in School-aged Children (HBSC) has analyzed breakfast consumption in Danish children and adolescents. The latest study from 2014 showed that eight out of ten Danish 11-year-old children consumed breakfast every weekday. This proportion decreased in 15-year-olds where 66% of girls and 74% of boys had breakfast on a daily basis during the school week [21]. The regularity of meals and the intake of energy and nutrients in children and adults have been reported previously in the Danish National Survey of Diet and Physical Activity (DANSDA), and the results are similar to the HBSC study regarding regular breakfast patterns over time [8,9]. Breakfast habits in Denmark have recently been described and confirmed to have a high regularity of breakfast consumption among adults 18–74 years, as only 7% do not eat breakfast on a given day [22]. However, the 2016 report does not include data on nutrient intakes in relation to breakfast.
In the present study, DANSDA data are used to analyze breakfast consumption and association with the intake of key food groups, energy, and macro- and micronutrients. The analyses have been carried out in the aligned approach agreed in the International Breakfast Research Initiative (IBRI). IBRI was set up to study the nutritional impact of breakfast and provide evidence-based recommendations, primarily for a nutrient-based balanced breakfast [23]. The objectives of the present study are to describe the prevalence of breakfast consumption in Denmark, describe the contribution of breakfast to the daily nutrient intake and intake from key food groups and among breakfast consumers, compare energy, nutrient and food group intakes at breakfast by tertiles of daily dietary quality using the Nutrient Rich Food (NRF 9.3) Index. The prevalence of breakfast consumption and nutrient intake at breakfast are described for children, adolescents, younger and older adults, whereas two age groups (children/adolescents and adults) are used, when describing intakes across tertiles of NRF 9.3 scores.
2. Materials and Methods
2.1. Population
This study was based on data derived from the DANSDA 2011–2013, which is a nation-wide cross-sectional survey. Data were collected all year round during the survey period. The study population comprised of a simple random sample of 4 to 75-year-old children and adults retrieved from the Danish Civil Registration System. In comparison with census data from Statistics Denmark, the distribution of gender and age of the participants could be characterized as representative for the Danish population. However, individuals with a basic education were under-represented, and men and 19 to 54-year-olds were slightly under-represented [24]. In all, 3816 participants aged 6–75 years had complete dietary data and 3680 participants had 7 days of food records and were included in the present study. A total of 23 individuals did not eat breakfast in the week of dietary recording. Within the IBRI framework, it was decided that no lower limit for the energy content of breakfasts should be applied, thus all breakfasts are included in the analysis regardless of energy contribution.
The DANSDA survey has been conducted in accordance with the guidelines laid down in the Declaration of Helsinki and has been approved by the Danish Data Protection Agency. The Danish National Committee on Health Research Ethics has decided that, according to Danish Law, DANSDA does not require approval.
2.2. Intake of Energy, Nutrients, and Foods
The dietary intake was recorded every day for seven consecutive days in food diaries with pre-coded response categories, which included open-answer options. The food record was following a typical Danish meal pattern with breakfast, a morning snack, lunch, an afternoon snack, dinner, and evening snack. The amount of foods eaten was given in predefined household measures (cups, spoons, slices, etc.) or estimated from photos of up to six portion sizes. For food items not included in the pre-coded food record, the participants wrote the type of food and portion size eaten in open-answer categories. Participants also received a food diary booklet to take to school or to other places outside of the home on the days of food recording. Details about the method and calculation of intake of food and nutrients have been described elsewhere [25].
The intake of energy, nutrients, and food items was calculated for each individual using the software system GIES (version 1.000d; developed at the National Food Institute, Technical University of Denmark, Copenhagen, Demark), and the Danish Food Composition Databank [26]. In order to allow a focus solely on food-derived micronutrients, nutrient intakes from dietary supplements were not included in the calculation of nutrient intake and the current analysis. Food groups providing the major part of food intake at breakfast were chosen to describe the food intake at breakfast. The same food groups were chosen for children and adults, although the intake of some food groups are very low or zero in children (e.g., alcoholic beverages).
In the present study, the mean intake of energy, nutrients, and foods was calculated for breakfasts, as well as for the intake of the total day. The analysis in the study followed the harmonized approach defined within the IBRI consortium [23].
2.3. The Regularity of Breakfast Consumption
The regularity of breakfast was defined as follows:
5–7 breakfasts per week: Regular consumer
2–4 breakfasts per week: Irregular consumer
Breakfast 0–1 day per week: Skipper
2.4. Calculation of Dietary Quality of the Diet by the NRF 9.3 Index
The dietary quality of the overall diet was calculated on the basis of a modified Nutrient Rich Foods (NRF) Index. The NRF Index calculates the nutrient density, defined as nutrients per calorie. The current NRF algorithms, based on 12 nutrients, can be applied to individual foods, meals or to the total diet [27]. The present version, known as NRF 9.3, was based on the sum of the percentage of daily values for nine nutrients to encourage protein, dietary fibre, vitamin A, vitamin C, vitamin E, calcium, iron, magnesium, and potassium, minus the sum of the percentage of maximum recommended values for three nutrients to limit saturated fat, total or added sugar, and sodium, with all daily values calculated per 2000 kcal and capped at 100% [28]. As used in the IBRI studies, the NRF 9.3 score reflects nutrient intakes (normalized to an intake of 2000 kcal) expressed as percentages of the national daily values for food labelling purposes. The IBRI consortium decided to replace vitamin E with vitamin D in the list of the nine nutrients to encourage, because vitamin D is a nutrient of public health concerns in many of the participating countries, including Denmark [24].
The algorithm for the NRF 9.3 Index subtracts the sum of the three nutrients to limit from the sum of the nine nutrients to encourage expressed as a multiple of 100:
| (∑ sub-scores positive × 100) − (∑ sub-scores negative × 100) | (1) |
The sub-score was calculated for each nutrient. For the nutrients to encourage, sub-scores above 100 were truncated to 100 for that nutrient. For the nutrients to limit, if the sub-score was less than 100, then 0 was assigned to the sub-score. The maximum possible score was 900 points reflecting a diet where intakes per 2000 kcal were ≥ the daily values for the nine nutrients to encourage and were ≤ the daily values for the three nutrients to limit. Similarly, 600 points reflect a diet where intakes per 2000 kcal were ≥ the daily values for the nine nutrients to encourage and were ≥ the daily values for the three nutrients to limit, but there are numerous combinations of intake to achieve, e.g., 600 points. For the European countries participating in the IBRI studies, the NRF 9.3 scores were calculated on the basis of the EU reference daily values and maximum recommended values for nutrients based on a 2000-kcal diet (Table 1) [29]. Positive and negative nutrient sub-scores were calculated for both children and adults. For added sugar, an upper limit of 10% of energy intake was used as the nutrient reference value (NRV) according to the recommendation by the WHO [30]. The daily sodium intakes were converted to salt by applying the conversion factor of 2.5 [29] and the NRV was 6 g. The NRV for dietary fibre was defined as 25 g based on the European Food Safety Authority (EFSA) recommendation [31].
Table 1.
The reference daily values and maximum recommended values for nutrients based on a 2000-kcal diet.
| Nutrient | NRV 1 | MRV 2 |
|---|---|---|
| Protein (g) | 50 | - |
| Dietary fibre (g) | 25 | - |
| Vitamin A (ug) | 800 | - |
| Vitamin C (mg) | 80 | - |
| Vitamin D (ug) | 5 | - |
| Calcium (mg) | 800 | - |
| Iron (mg) | 14 | - |
| Potassium (mg) | 2000 | - |
| Magnesium (mg) | 375 | - |
| Saturated fat (E% fat) | - | 10 |
| Added sugar (E% fat) | - | 10 |
| Sodium (g) | - | 6 |
1 NRV, nutrient reference value; 2 MRV; maximum recommended value.
2.5. Statistical Analysis
SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. The significance level was chosen as p < 0.05. Model fit was checked by histograms and QQ (quantile-quantile) plots of the residuals. In order to meet the model assumption of normally distributed residuals, all macro- and micro-nutrient intakes were square root transformed and the food intakes were transformed using log10. Intakes of energy were not transformed.
Pearson Chi-square tests were used to test the difference in the regularity of breakfast consumption between gender and age groups, respectively. Non consumers of breakfast were included in the population for the Chi-square tests, but were excluded from all other statistics presented. Descriptive statistics for energy, nutrient, and food intake are given as the mean and standard deviation (SD). Education was chosen as a measure for SES as other research has shown education to be the key social variable of dietary habits in Denmark [32,33].
One-way analysis of variance (ANOVA) was used to compare the breakfast energy intake and all day energy intake between four age groups. Analysis of covariance (ANCOVA) adjusted for energy intake at breakfast was used to compare the nutrient intake at breakfast between the four age groups, while ANCOVA adjusted for daily energy intake was used to compare the daily nutrient intake between all age groups.
Tertiles of NRF 9.3 scores were calculated separately for children/adolescents (6–17 years) and adults (18–75 years). The upper tertile (T3) was indicative of the highest level of overall dietary quality. The two age groups were chosen to form the basis of the future work of IBRI developing two sets of nutritional guidelines for breakfast: one for children/adolescents and another for adults. A one-way ANOVA, and an ANCOVA adjusted for the daily energy intake and an ANCOVA adjusted for the daily energy intake and education was used to test the effect of tertile on nutrient and food intake (eaters only) at breakfast. The model check, as described above, was used to validate these models. The Tukey–Kramer post hoc test was used for multiple comparisons.
3. Results
3.1. The Regularity of Breakfast Consumption
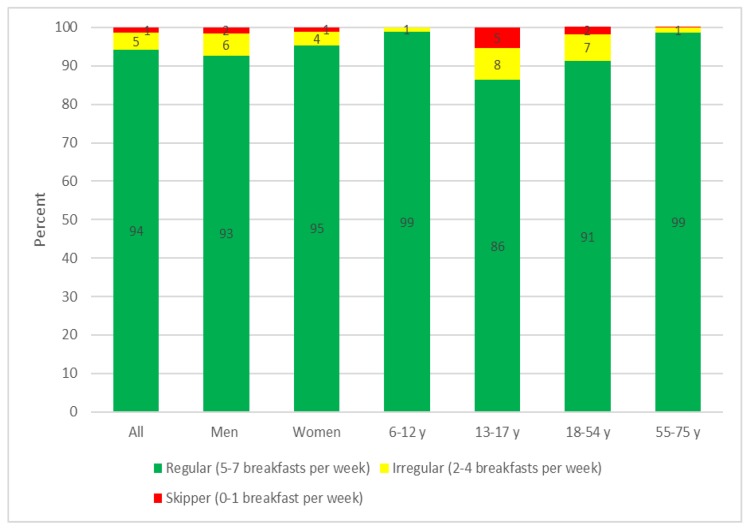
Among the sample (n = 3680), the majority of the population (94.1%) were regular breakfast consumers, while 4.6% had an irregular pattern and 1.3% were classified as skippers (Figure 1). Slightly more women than men were regular breakfast consumers (p = 0.0023). Children (6–12 years) and older adults (55–75 years) had breakfast regularly (98.9% and 98.8% respectively) while adolescents (13–17 years) had an irregular pattern with 5.4% skipping breakfast and 8.3% eating breakfast 2–4 times a week. Among the adults (18–54 years), 7% were classified as irregular breakfast consumers. The chi-square test for homogeneity showed that the pattern of breakfast consumption was significantly different between the four age groups (p < 0.0001)
Figure 1.
The proportion of skippers, irregular consumers, and regular consumers in the total Danish population according to gender and age (n = 3680).
3.2. Daily and Breakfast Intake of Energy, Nutrients and Foods
Overall, 3657 participants consumed breakfast (476 children 6–12 years, 272 adolescents 13–17 years, 1791 younger adults 18–54 years, 1118 older adults 55–75 years) and were included in the analysis of nutrient and food intake. Table 2 and 3 show the unadjusted means and SD. The mean breakfast energy intake and daily energy intake were different (p = 0.0012 and p < 001, respectively) between age groups (Table 2). Differences between age groups were also found for the mean breakfast and daily intake of macronutrients.
Table 2.
The intake of energy and macronutrients at breakfast and for the total day according to age in Danes
| Age Group | All (6–75 years) n = 3657 |
Children (6–12 years) n = 476 |
Adolescents (13–17 years) n = 272 |
Younger Adults (18–54 years) n = 1791 |
Older Adults (55–75 years) n = 1118 |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | p * | p ** | |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Breakfast Intake | Daily Intakes | |
| Energy (kJ) | 1736 | 806 | 9645 | 3066 | 1599 | 564 | 8655 | 1934 | 1759 | 820 | 9042 | 3365 | 1754 | 844 | 10029 | 3267 | 1761 | 824 | 9599 | 2932 | 0.0012 | <0.0001 |
| Carbohydrates (g) | 59 | 28 | 266 | 87 | 59 | 22 | 269 | 62 | 64 | 31 | 273 | 104 | 58 | 28 | 273 | 91 | 58 | 28 | 251 | 82 | <0.0001 | <0.0001 |
| Carbohydrates (E%) | 56 | 12 | 47 | 6 | 60 | 8 | 51 | 5 | 60 | 11 | 50 | 6 | 55 | 12 | 47 | 6 | 54 | 12 | 45 | 6 | <0.0001 | <0.0001 |
| Added sugars (g) | 8 | 9 | 51 | 38 | 9 | 7 | 56 | 28 | 9 | 8 | 62 | 42 | 7 | 8 | 53 | 41 | 9 | 11 | 42 | 32 | <0.0001 | <0.0001 |
| Added sugars (E%) | 8 | 9 | 9 | 5 | 9 | 6 | 11 | 5 | 8 | 7 | 11 | 6 | 7 | 8 | 9 | 6 | 9 | 10 | 8 | 4 | <0.0001 | <0.0001 |
| Proteins (g) | 16 | 8 | 87 | 29 | 14 | 6 | 74 | 20 | 15 | 8 | 81 | 30 | 16 | 8 | 91 | 31 | 16 | 8 | 87 | 27 | <0.0001 | <0.0001 |
| Proteins (E%) | 16 | 5 | 16 | 3 | 15 | 3 | 15 | 2 | 15 | 5 | 16 | 3 | 16 | 6 | 16 | 3 | 16 | 5 | 17 | 3 | <0.0001 | <0.0001 |
| Fat (g) | 14 | 10 | 94 | 37 | 11 | 6 | 81 | 22 | 12 | 8 | 85 | 36 | 14 | 10 | 99 | 39 | 15 | 10 | 95 | 36 | <0.0001 | <0.0001 |
| Fat (E%) | 28 | 11 | 37 | 6 | 25 | 9 | 34 | 4 | 25 | 10 | 34 | 5 | 29 | 11 | 37 | 6 | 30 | 11 | 38 | 6 | <0.0001 | <0.0001 |
| SFA (g) | 7 | 5 | 38 | 16 | 5 | 3 | 33 | 10 | 6 | 4 | 34 | 16 | 7 | 5 | 3 | 17 | 7 | 5 | 38 | 16 | <0.0001 | <0.0001 |
| SFA (E%) | 13 | 6 | 15 | 3 | 12 | 5 | 14 | 2 | 12 | 6 | 14 | 3 | 13 | 6 | 15 | 3 | 14 | 7 | 15 | 3 | <0.0001 | <0.0001 |
| Dietary fibre (g) | 5 | 3 | 22 | 8 | 4 | 2 | 20 | 6 | 4 | 3 | 19 | 8 | 5 | 4 | 23 | 8 | 5 | 3 | 23 | 8 | <0.0001 | <0.0001 |
Abbreviation: SFA: Saturated fatty acids. p * for macronutrients adjusted for energy intake at breakfast p ** for macronutrients adjusted for daily energy intake. p < 0.05 considered significant. Values for macronutrients were Square root transformed prior to analysis. Mean and SD are based on absolute values of intake.
The mean breakfast intake of micronutrients differed between the age groups (except folate and vitamin B12, both p > 0.05 (Table 3). The mean daily intake of micronutrients differed between age groups (except thiamin and riboflavin, both p > 0.10).
Table 3.
The intake of micronutrients at breakfast and for the total day according to age in Danes.
| Age Group | All (6–75 years) n = 3657 |
Children (6–12 years) n = 476 |
Adolescents (13–17 years) n = 272 |
Younger Adults (18–54 years) n = 1791 |
Older Adults (55–75 years) n = 1118 |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | Breakfast Intake | Daily Intake | p * | p ** | |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Breakfast Intake | Daily Intake | |
| Thiamin (mg) | 0.3 | 0.1 | 1.4 | 0.5 | 0.3 | 0.1 | 1.3 | 0.4 | 0.3 | 0.2 | 1.3 | 0.5 | 0.3 | 0.2 | 1.4 | 0.5 | 0.2 | 0.1 | 1.4 | 0.5 | <0.0001 | 0.4550 |
| Riboflavin (mg) | 0.4 | 0.2 | 1.8 | 0.7 | 0.4 | 0.2 | 1.6 | 0.5 | 0.5 | 0.3 | 1.7 | 0.7 | 0.4 | 0.2 | 1.8 | 0.7 | 0.4 | 0.2 | 1.8 | 0.6 | <0.0001 | 0.1042 |
| Niacin (NE) | 5.1 | 2.5 | 33.0 | 11.7 | 3.4 | 1.5 | 23.8 | 6.9 | 4.0 | 2.0 | 27.2 | 10.6 | 5.3 | 2.6 | 34.9 | 12.1 | 5.8 | 2.4 | 35.2 | 10.6 | <0.0001 | <0.0001 |
| B6 (mg) | 0.2 | 0.1 | 1.6 | 0.5 | 0.2 | 0.1 | 1.3 | 0.4 | 0.2 | 0.1 | 1.4 | 0.5 | 0.2 | 0.1 | 1.7 | 0.6 | 0.2 | 0.1 | 1.6 | 0.5 | <0.0001 | <0.0001 |
| Folate (ug) | 67 | 36 | 340 | 129 | 59 | 25 | 288 | 86 | 67 | 35 | 286 | 109 | 69 | 40 | 355 | 133 | 67 | 34 | 351 | 132 | 0.0570 | <0.0001 |
| B12 (mg) | 1.0 | 0.8 | 6.6 | 3.7 | 0.9 | 0.6 | 5.4 | 2.4 | 1.0 | 0.9 | 5.3 | 2.8 | 1.0 | 0.8 | 6.6 | 3.7 | 1.0 | 0.8 | 7.4 | 4.2 | 0.1320 | <0.0001 |
| Biotin (mg) | 9 | 6 | 36 | 15 | 8 | 5 | 34 | 11 | 9 | 7 | 32 | 15 | 9 | 6 | 38 | 17 | 8 | 6 | 35 | 146 | <0.0001 | <0.0001 |
| Vit E (alfa-TE) | 1.5 | 1.4 | 8.9 | 4.0 | 1.3 | 1.2 | 7.6 | 2.6 | 1.3 | 1.3 | 7.2 | 3.4 | 1.5 | 1.5 | 9.3 | 4.3 | 1.4 | 1.4 | 9.1 | 4.0 | 0.0001 | <0.0001 |
| Vit D (ug) | 0.3 | 0.9 | 4.4 | 4.2 | 0.2 | 0.2 | 2.7 | 2.1 | 0.3 | 0.3 | 2.9 | 2.7 | 0.4 | 0.5 | 4.4 | 3.9 | 0.4 | 1.5 | 5.7 | 5.1 | 0.0020 | <0.0001 |
| Vitamin C (mg) | 17 | 20 | 112 | 57 | 13 | 15 | 103 | 52 | 19 | 23 | 94 | 51 | 18 | 20 | 114 | 58 | 17 | 21 | 117 | 58 | 0.0010 | <0.0001 |
| Vit A (RE) | 148 | 236 | 1299 | 967 | 105 | 145 | 1189 | 706 | 139 | 211 | 973 | 737 | 155 | 244 | 1330 | 992 | 156 | 259 | 1376 | 1051 | 0.0030 | <0.0001 |
| Calcium (mg) | 331 | 183 | 1113 | 413 | 295 | 141 | 1052 | 346 | 322 | 209 | 1081 | 441 | 332 | 186 | 1161 | 426 | 348 | 185 | 1071 | 403 | 0.0004 | <0.0001 |
| Iron (mg) | 1.9 | 1.1 | 11.2 | 3.7 | 1.9 | 0.9 | 9.5 | 2.4 | 2.0 | 1.2 | 9.8 | 3.7 | 2.0 | 1.1 | 11.7 | 3.8 | 1.8 | 1.0 | 11.5 | 3.6 | <0.0001 | <0.0001 |
| Zinc (mg) | 2.2 | 1.1 | 12.0 | 4.2 | 1.8 | 0.9 | 10.1 | 2.8 | 2.0 | 1.2 | 11.2 | 4.4 | 2.2 | 1.2 | 12.6 | 4.4 | 2.3 | 1.2 | 12.1 | 3.9 | <0.0001 | <0.0001 |
| Sodium (mg) | 501 | 324 | 3726 | 127 | 413 | 206 | 3216 | 838 | 481 | 251 | 3534 | 1272 | 508 | 355 | 3941 | 1368 | 532 | 324 | 3646 | 1198 | <0.0001 | <0.0001 |
| Iodine (ug) | 42 | 26 | 247 | 142 | 47 | 24 | 233 | 119 | 49 | 32 | 235 | 128 | 42 | 26 | 259 | 157 | 40 | 24 | 236 | 129 | <0.0001 | 0.0197 |
| Potassium (mg) | 619 | 280 | 3436 | 1097 | 504 | 212 | 2750 | 784 | 575 | 307 | 2875 | 1066 | 638 | 289 | 3556 | 1099 | 647 | 272 | 3673 | 1053 | <0.0001 | <0.0001 |
| Magnesium (mg) | 89 | 52 | 370 | 118 | 77 | 46 | 300 | 83 | 82 | 63 | 314 | 121 | 93 | 53 | 391 | 123 | 90 | 48 | 380 | 1072 | <0.0001 | <0.0001 |
| Selenium (ug) | 7.4 | 4.4 | 51.5 | 20.0 | 6.5 | 3.1 | 41.5 | 13.3 | 6.9 | 3.6 | 44.7 | 18.1 | 7.8 | 5.0 | 53.5 | 21.2 | 7.2 | 4.1 | 54.1 | 19.1 | <0.0001 | <0.0001 |
p * for micronutrients adjusted for energy intake at breakfast p ** for micronutrients adjusted for daily energy intake. p < 0.05 considered significant. Values for micronutrients were square root transformed prior to analysis. Mean and SD are based on absolute values of intake.
Descriptive figures of the mean intake of solid foods and beverages at breakfast according to the age groups are shown in Figures S1 and S2. Generally, the total intake of foods and beverages increased with increasing age. The intake of vegetables, cakes, soft drinks, and cordials (sweet fruit beverages with water) were low.
3.3. The Contribution of Breakfast to Daily Energy and Nutrient Intakes
The percentage contribution to daily nutrient intakes in children (6–12 years) and adolescents (13–17 years) is shown in Figure 2 and in younger (18–54 years) and older adults (55–75 years) in Figure 3. Breakfast provided 18–20% of daily energy intake. Among children and adolescents, breakfast contributed with a higher proportion of carbohydrates, dietary fibre, and several vitamins (thiamine, riboflavin, folate, and biotin) and minerals (calcium, magnesium, iron, and iodine) than energy to the daily diet. The contribution of added sugars, total fats, saturated fats, vitamins D and A, sodium, and selenium at breakfast was lower than the contribution of energy to the daily diet.
Figure 2.
The contribution of breakfast (%) to the daily nutrient intakes in 6–12 and 13–17 year-old Danes.
Figure 3.
The contribution of breakfast (%) to the daily nutrient intakes in 18–54 and 55–75 year-old Danes.
Among younger and older adults (Figure 3), breakfast contributed to a higher proportion of carbohydrates, dietary fibre, some vitamins (riboflavin, folate, and biotin) and minerals (calcium and magnesium) than energy to the daily diet. The contribution of total fats, vitamins C, D, E and A, sodium, iodine and selenium at breakfast was lower than the contribution of energy to the daily diet. The contribution of added sugars was higher than the contribution of energy to the daily diet among older adults.
3.4. Energy, Nutrients and Food Intakes at Breakfast by Tertiles of Daily Dietary Quality
Breakfast consumers were divided into tertiles of daily dietary quality based on the NRF 9.3 score. The population was split into two age groups, children/adolescents (6–17 years) and adults (18–75 years). Sociodemographic and lifestyle characteristics are shown in Table S1. Children/adolescents, who had a higher dietary quality, were more likely to be female and not be overweight/obese. Adults, who had a higher dietary quality, were more likely to be female, have an intention to eat healthily, were less likely to smoke daily or have a sedentary lifestyle.
A decrease in energy content of breakfast was seen in both age groups across tertiles of daily dietary quality as expressed by NRF 9.3 (Table 4). Intakes of added sugar, total fat and saturated fat (expressed as % breakfast energy intake) decreased significantly from the lowest to highest tertile of NRF 9.3 in children/adolescents and adults. The intake of protein (expressed as % breakfast energy intake) and dietary fibre increased in both age groups across tertiles of NRF 9.3.
Table 4.
The mean intake at breakfast of energy and micronutrients among breakfast consumers across the tertiles of the NRF 9.3 score according to age in Danes.
| Age Group | Children/Adolescents 6–17 years (n = 748) | Adults 18–75 years (n = 2909) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary Quality T3 | Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary Quality T3 | |||||||||||||
| Mean | SD | Mean | SD | Mean | SD | p * | p ** | p *** | Mean | SD | Mean | SD | Mean | SD | p * | p ** | p *** | |
| NRF 9.3 | 538 | 66 | 644 | 20 | 729 | 41 | 571 | 66 | 685 | 30 | 774 | 95 | ||||||
| Energy (kJ) | 1720 | 750 | 1632 | 628 | 1620 | 630 | <0.0001 | <0.0001 | <0.0001 | 1861 a | 1021 | 1727 a | 741 | 1682 b | 701 | <0.0001 | <0.0001 | 0.0007 |
| Carbohydrates (g) | 60 b | 27 | 60 b | 25 | 62 a | 27 | <0.0001 | 0.0008 | 0.0003 | 56 c | 30 | 57 b | 26 | 61 a | 28 | <0.0001 | <0.0001 | <0.0001 |
| Carbohydrates (%E) | 58 c | 11 | 60 b | 9 | 63 a | 8 | <0.0001 | <0.0001 | <0.0001 | 51 c | 14 | 54 b | 11 | 58 a | 11 | <0.0001 | <0.0001 | <0.0001 |
| Added sugars (g) | 11 a | 9 | 9 b | 7 | 7 c | 7 | <0.0001 | <0.0001 | <0.0001 | 10 a | 11 | 7 b | 8 | 7 a,b | 8 | <0.0001 | 0.0049 | 0.0203 |
| Added sugars (%E) | 11 a | 8 | 9 b | 6 | 7 c | 5 | <0.0001 | <0.0001 | <0.0001 | 10 a | 12 | 7 b | 7 | 7 b | 7 | <0.0001 | <.0001 | <0.0001 |
| Proteins (g) | 14 b | 7 | 14 b | 6 | 15 a | 7 | <0.0001 | <0.0001 | <0.0001 | 16 c | 10 | 16 b | 8 | 16 a | 7 | <0.0001 | <0.0001 | <0.0001 |
| Proteins (%E) | 14 b | 4 | 14 b | 3 | 16 a | 4 | <0.0001 | <0.0001 | <0.0001 | 15 c | 7 | 16 b | 4 | 17 a | 5 | <0.0001 | <0.0001 | <0.0001 |
| Fat (g) | 13 a | 8 | 11 b | 6 | 9 c | 5 | <0.0001 | <0.0001 | <0.0001 | 18 a | 13 | 14 b | 8 | 11 a | 7 | <0.0001 | <0.0001 | <0.0001 |
| Fat (%E) | 28 a | 10 | 25 b | 9 | 21 c | 7 | <0.0001 | <0.0001 | <0.0001 | 34 a | 12 | 29 b | 10 | 25 c | 9 | <0.0001 | <0.0001 | <0.0001 |
| SFA (g) | 7 a | 4 | 5 b | 3 | 4 c | 2 | <0.0001 | <0.0001 | <0.0001 | 9 a | 7 | 7 b | 4 | 5 c | 3 | <0.0001 | <0.0001 | <0.0001 |
| SFA (%E) | 14 a | 6 | 12 b | 5 | 9 c | 4 | <0.0001 | <0.0001 | <0.0001 | 17 a | 7 | 14 b | 6 | 10 c | 5 | <0.0001 | <0.0001 | <0.0001 |
| Dietary fibre (g) | 4 c | 2 | 4 b | 2 | 5 a | 3 | <0.0001 | <0.0001 | <0.0001 | 4 c | 2 | 5 b | 3 | 6 a | 3 | <0.0001 | <0.0001 | <0.0001 |
Abbreviation: SFA: Saturated fatty acids p *. Unadjusted (ANOVA) p ** Adjusted for daily energy p *** adjusted for daily energy and education (ANCOVA). The Tukey–Kramer test for multiple comparisons was used. Different superscript letters indicate significantly different means for data adjusted for daily energy and education. p < 0.05 considered significant. Values for macronutrients were Square root transformed prior to analysis. Mean and SD are based on absolute values of intake.
The intake of most vitamins increased from the lowest to highest tertile of NRF 9.3 in children/adolescents and adults, except the intake of vitamin D adjusted for energy intake and education (both children/adolescents and adults) and vitamin E (children/adolescents) (Table 5). The intake of vitamin A decreased across the tertiles of NRF 9.3 in children/adolescents and adults.
Table 5.
The mean intake at breakfast of micronutrients among breakfast consumers across the tertiles of the NRF 9.3 score according to age in Danes.
| Age Group | Children/Adolescents 6–17 years (n = 748) | Adults 18–75 years (n = 2909) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary Quality T3 | Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary Quality T3 | |||||||||||||
| Mean | SD | Mean | SD | Mean | SD | p * | p ** | p *** | Mean | SD | Mean | SD | Mean | SD | p * | p ** | p *** | |
| Thiamin (mg) | 0.27 c | 0.13 | 0.28 b | 0.13 | 0.32 a | 0.16 | <0.0001 | <0.0001 | <0.0001 | 0.23 c | 0.14 | 0.26 b | 0.14 | 0.29 a | 0.14 | <0.0001 | <0.0001 | <0.0001 |
| Riboflavin (mg) | 0.44 a | 0.25 | 0.44 b | 0.22 | 0.49 a | 0.23 | <0.0001 | <0.0001 | <0.0001 | 0.40 c | 0.26 | 0.43 b | 0.22 | 0.45 a | 0.21 | <0.0001 | <0.0001 | <0.0001 |
| Niacin (NE) | 3.5 b | 1.8 | 3.4 a | 1.5 | 4.0 a | 1.7 | <0.0001 | <0.0001 | <0.0001 | 5.4 c | 2.9 | 5.6 b | 2.4 | 5.6 a | 2.2 | <0.0001 | <0.0001 | <0.0001 |
| B6 (mg) | 0.20 b | 0.11 | 0.21 a | 0.10 | 0.25 a | 0.10 | <0.0001 | <0.0001 | <0.0001 | 0.19 c | 0.12 | 0.23 b | 0.13 | 0.25 a | 0.13 | <0.0001 | <0.0001 | <0.0001 |
| Folate (ug) | 61.5 b | 32.6 | 60.6 a | 27.2 | 63.9 a | 27.3 | <0.0001 | 0.0036 | 0.0008 | 63.3 c | 37.1 | 68.5 b | 35.8 | 72.2 a | 39.9 | <0.0001 | <0.0001 | <0.0001 |
| B12 (mg) | 0.91 b | 0.76 | 0.89 a | 0.67 | 1.08 a | 0.66 | <0.0001 | <0.0001 | <0.0001 | 1.01 b | 0.97 | 1.03 a | 0.75 | 1.01 a | 0.64 | <0.0001 | <0.0001 | <0.0001 |
| Biotin (mg) | 6.5 c | 4.4 | 7.6 b | 4.7 | 10.6 a | 6.7 | <0.0001 | <0.0001 | <0.0001 | 7.0 c | 5.6 | 8.4 b | 5.6 | 10.1 a | 6.5 | <0.0001 | <0.0001 | <0.0001 |
| Vit E (alfa-TE) | 1.59 a | 1.66 | 1.26 b | 1.19 | 1.08 c | 0.79 | <0.0001 | 0.0058 | 0.0320 | 1.44 b | 1.33 | 1.40 c | 1.30 | 1.65 a | 1.70 | <0.0001 | <0.0001 | <0.0001 |
| Vit D (ug) | 0.28 a | 0.27 | 0.23 a,b | 0.16 | 0.25 b | 0.19 | <0.0001 | 0.1986 | 0.1432 | 0.34 b | 0.38 | 0.33 b | 0.78 | 0.41 a | 1.54 | <0.0001 | 0.0592 | 0.1035 |
| Vitamin C (mg) | 15.2 b | 21.7 | 14.9 a,b | 17.0 | 16.0 a | 15.7 | <0.0001 | 0.0253 | 0.0041 | 13.0 c | 17.0 | 17.7 b | 20.0 | 21.4 a | 23.5 | <0.0001 | <0.0001 | <0.0001 |
| Vit A (RE) | 136 | 197 | 113 | 151 | 102 | 166 | <0.0001 | 0.0100 | 0.0070 | 201 a | 296 | 154 b | 220 | 112 c | 217 | <0.0001 | <0.0001 | <0.0001 |
| Calcium (mg) | 284 c | 182 | 293 b | 152 | 339 a | 169 | <0.0001 | <0.0001 | <0.0001 | 313 c | 211 | 344 b | 178 | 358 a | 161 | <0.0001 | <0.0001 | <0.0001 |
| Iron (mg) | 1.76 c | 0.86 | 1.88 b | 0.94 | 2.19 a | 1.16 | <0.0001 | <0.0001 | <0.0001 | 1.74 c | 1.04 | 1.89 b | 1.00 | 2.18 a | 1.17 | <0.0001 | <0.0001 | <0.0001 |
| Zinc (mg) | 1.70 c | 0.92 | 1.80 b | 0.88 | 2.18 a | 1.12 | <0.0001 | <0.0001 | <0.0001 | 2.07 c | 1.29 | 2.25 b | 1.11 | 2.39 a | 1.08 | <0.0001 | <0.0001 | <0.0001 |
| Sodium (mg) | 500 a | 255 | 427 b | 203 | 386 b | 201 | <0.0001 | <0.0001 | 0.0010 | 616 a | 421 | 528 a | 313 | 409 b | 239 | <0.0001 | <0.0001 | <0.0001 |
| Iodine (ug) | 46.2 b | 29.3 | 45.7 b | 24.7 | 50.6 a | 25.7 | <0.0001 | 0.0005 | 0.0001 | 38.1 c | 27.8 | 41.4 b | 24.4 | 43.7 a | 22.3 | <0.0001 | <0.0001 | <0.0001 |
| Potassium (mg) | 482 c | 271 | 507 b | 217 | 600 a | 253 | <0.0001 | <0.0001 | <0.0001 | 556 c | 262 | 644 b | 270 | 726 a | 289 | <0.0001 | <0.0001 | <0.0001 |
| Magnesium (mg) | 63.4 c | 37.9 | 74.4 b | 44.5 | 99.0 a | 64.9 | <0.0001 | <0.0001 | <0.0001 | 74.0 c | 39.8 | 90.1 b | 47.2 | 110.7 a | 57.4 | <0.0001 | <0.0001 | <0.0001 |
| Selenium (ug) | 6.54 b | 3.72 | 6.24 b | 2.90 | 7.10 a | 3.21 | <0.0001 | <0.0001 | <0.0001 | 7.49 c | 5.37 | 7.54 b | 4.21 | 7.74 a | 4.37 | <0.0001 | <0.0001 | <0.0001 |
p * Unadjusted (ANOVA) p ** Adjusted for daily energy p *** adjusted for daily energy and education (ANCOVA). The Tukey–Kramer test for multiple comparisons was used. Different superscript letters indicate significantly different means for data adjusted for daily energy and education. p < 0.05 considered significant. Values for micronutrients were Square root transformed prior to analysis. Mean and SD are based on absolute values of intake.
The intake of calcium, iron, zinc, potassium, and magnesium increased from the lowest to highest tertile of NRF 9.3 in both age groups, whereas the intake of sodium decreased in both age groups.
In children/adolescents, the intake of breakfast cereals incl. oats and muesli and milk added to cereals was higher in the group with the highest dietary quality score (highest tertile of NRF 9.3). In contrast, the intake of fermented milk, non-whole grain wheat bread, fruits, tea and milk was higher in the lowest tertile of NRF 9.3 (Table 6). Otherwise, few significant differences across the tertiles were observed.
Table 6.
The mean intake at breakfast of selected food groups (eaters only) among breakfast consumers across the tertiles of the NRF 9.3 score among Danish children.
| Age Group | Children/Adolescents 6–17 years (n = 748) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary QualityT3 | ||||||||||
| % Consumers (n) | Mean | SD | % Consumers (n) | Mean | SD | % Consumers (n) | Mean | SD | p * | p ** | p*** | |
| Breakfast cereals incl. oats & muesli (g) | 58 (143) | 22 b | 19 | 73 (183) | 20 b | 24 | 82 (204) | 37 a | 33 | <0.0001 | <0.0001 | <0.0001 |
| Porridge (oats, rice etc.) (g) | 10 (25) | 68 | 67 | 13 (33) | 75 | 69 | 18 (42) | 84 | 75 | 0.4253 | 0.4238 | 0.3771 |
| Milk for breakfast cereals (g) | 36 (90) | 75 b | 48 | 50 (125) | 90 b | 62 | 58 (145) | 105 a | 65 | 0.0014 | 0.0010 | 0.0100 |
| Fermented dairy products (g) | 25 (63) | 84 a | 70 | 37 (92) | 72 b | 63 | 29 (72) | 63 b | 49 | 0.0722 | 0.1184 | 0.0869 |
| Non-whole grain wheat bread (g) | 80 (200) | 38 a | 31 | 68 (169) | 34 a | 27 | 60 (151) | 23 b | 20 | <0.0001 | <0.0001 | 0.0002 |
| Whole grain wheat bread (g) | 39 (98) | 28 | 23 | 46 (115) | 29 | 25 | 43 (108) | 27 | 23 | 0.7045 | 0.8552 | 0.9845 |
| Whole grain rye bread (g) | 16 (41) | 19 | 17 | 17 (42) | 16 | 16 | 24 (59) | 19 | 19 | 0.7540 | 0.6835 | 0.7101 |
| Pastry, cakes, biscuits (g) | 18 (44) | 17 | 18 | 13(33) | 13 | 11 | 12(29) | 12 | 7 | 0.5758 | 0.6673 | 0.9216 |
| Fats on bread (g) | 73 (183) | 7a | 6 | 73(182) | 6 a | 4 | 58(146) | 4 b | 4 | <0.0001 | <0.0001 | <0.0001 |
| Cold cuts, cheese, egg on bread (g) | 89 (222) | 22 | 20 | 86(214) | 17 | 14 | 81(202) | 16 | 15 | 0.0026 | 0.0326 | 0.2876 |
| Vegetables, rich in dietary fibre (g) | 1 (2) | 16 | 8 | 5(12) | 9 | 12 | 4(11) | 14 | 13 | 0.3371 | 0.4983 | 0.3407 |
| Vegetables, low in dietary fibre (g) | 3 (8) | 19 | 19 | 5(12) | 12 | 11 | 6(15) | 17 | 16 | 0.8888 | 0.9426 | 0.2989 |
| Fruits (g) | 22 (54) | 45 a | 88 | 35(87) | 33 a,b | 36 | 54(134) | 41b | 52 | 0.2760 | 0.1162 | 0.0787 |
| Beverages total (g) | 97 (242) | 226 b | 134 | 98 (245) | 199 b | 122 | 98 (246) | 219 a | 132 | 0.0560 | 0.0658 | 0.0190 |
| Coffee (g) | 4 (10) | 188 | 170 | 4 (10) | 110 | 80 | 5 (12) | 113 | 67 | 0.7356 | 0.7396 | 0.6723 |
| Tea (g) | 10 (26) | 99 a | 68 | 8 (21) | 81 b | 45 | 13 (33) | 78 b | 69 | 0.1310 | 0.1586 | 0.0819 |
| Water (g) | 38(93) | 106 | 81 | 45(111) | 109 | 103 | 48 (121) | 105 | 104 | 0.8085 | 0.6899 | 0.8720 |
| Milk (incl. milk with chocolate flavor/fruits) (g) | 71 (176) | 153 a,b | 125 | 74 (185) | 122 b | 101 | 74 (186) | 147 a | 101 | 0.0287 | 0.0263 | 0.0019 |
| Juice (g) | 41 (103) | 99 | 87 | 48 (119) | 83 | 81 | 46 (116) | 75 | 63 | 0.0914 | 0.1790 | 0.6084 |
| Cordial (g) | 8 (19) | 66 | 45 | 4 (11) | 53 | 22 | 2 (6) | 76 | 49 | 0.7231 | 0.7352 | 0.4738 |
| Cordial light (g) | 3 (8) | 80 | 84 | 3 (8) | 44 | 30 | 1 (3) | 57 | 49 | 0.3943 | 0.4086 | 0.1834 |
| Carbonated soft drinks sugar sweetened (g) | 6 (14) | 47 | 29 | 1 (2) | 32 | 15 | - | n/a | n/a | 0.7012 | 0.7326 | 0.5374 |
| Carbonated soft drinks sugar light (g) | 0 | n/a | n/a | − (1) | 29 | 0 | − (1) | 21 | n/a | <0.0001 | n/a | n/a |
| Beer (g) | 0 | n/a | n/a | 0 | n/a | n/a | 0 | n/a | n/a | n/a | n/a | n/a |
| Wine/spirits (g) | 0 | n/a | n/a | 0 | n/a | n/a | 0 | n/a | n/a | n/a | n/a | n/a |
Under 1%. n/a: not applicable. p *. Unadjusted (ANOVA) p ** Adjusted for daily energy p *** adjusted for daily energy and education (ANCOVA). The Tukey–Kramer test for multiple comparisons was used. Different superscript letters indicate significantly different means for data adjusted for daily energy and education. p < 0.05 considered significant. Values for food intake were Log (10) transformed prior to analysis. Mean and SD are based on absolute values of intake. No statistical tests were carried out for % of consumers.
Among adults, the intake of breakfast cereals incl. oats and muesli, fruits and water increased across the tertiles of NRF 9.3, while non-whole grain bread and fats on bread decreased (Table 7). The intake of fermented dairy products was higher in the group with the highest dietary quality score (highest tertile of NRF 9.3). When comparing food intake in the groups with lowest and highest dietary quality, the study shows the higher intake of breakfast cereals, vegetables, fruits, dairy products and water, and lower non-whole grain bread in the group with highest dietary quality among adults.
Table 7.
The mean intake at breakfast of selected food groups (eaters only) among breakfast consumers across the tertiles of the NRF 9.3 score among Danish adults.
| Age Group | Adults 18–75 years (n = 2909) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Dietary Quality T1 | Medium Dietary Quality T2 | High Dietary Quality T3 | ||||||||||
| % Consumers (n) | Mean | SD | % Consumers (n) | Mean | SD | % Consumers (n) | Mean | SD | p * | p ** | p *** | |
| Breakfast cereals incl. oats & muesli (g) | 38 (367) | 27 c | 23 | 57 (551) | 31 b | 25 | 71 (688) | 37 a | 29 | <0.0001 | <0.0001 | <0.0001 |
| Porridge (oats, rice etc.) (g) | 8 (75) | 81 | 67 | 11 (108) | 90 | 91 | 15 (145) | 98 | 94 | 0.6462 | 0.3394 | 0.4779 |
| Milk for breakfast cereals (g) | 22 (217) | 89 b | 50 | 32 (309) | 94 a,b | 51 | 40 (383) | 102 a | 53 | 0.0161 | 0.0009 | 0.0110 |
| Fermented dairy products (g) | 23 (220) | 96 b | 88 | 34 (331) | 100 b | 81 | 42 (406) | 115 a | 85 | 0.0019 | <0.0001 | <0.0001 |
| Non-whole grain wheat bread (g) | 73 (708) | 41a | 34 | 62 (600) | 27 b | 21 | 47 (459 | 20 c | 17 | <0.0001 | <0.0001 | <0.0001 |
| Whole grain wheat bread (g) | 35 (337) | 29 a,b | 22 | 45 (439) | 29 a,b | 22 | 46 (444) | 26b | 22 | 0.0003 | 0.0601 | 0.1251 |
| Whole grain rye bread (g) | 39 (373) | 23 | 18 | 50 (42) | 16 | 16 | 46 (59) | 19 | 19 | 0.0523 | 0.3660 | 0.6989 |
| Pastry, cakes, biscuits (g) | 14 (137) | 17 a | 16 | 11 (104) | 13 a,b | 10 | 9 (84) | 10 b | 9 | 0.0003 | 0.0042 | 0.0396 |
| Fats on bread (g) | 75 (728) | 11 a | 9 | 64 (620) | 7 b | 6 | 43 (419) | 5 c | 5 | <0.0001 | <0.0001 | <0.0001 |
| Cold cuts, cheese, egg on bread (g) | 86 (839) | 43 a | 37 | 88 (854) | 37 a,b | 32 | 82 (798) | 33 b | 32 | <0.0001 | 0.0039 | 0.0292 |
| Vegetables, rich in dietary fibre (g) | 3 (26) | 15 b | 14 | 5 (50) | 30 a | 54 | 6 (58) | 28 a | 42 | 0.1456 | 0.1462 | 0.0852 |
| Vegetables, low in dietary fibre (g) | 6 (58) | 18 | 27 | 7 (63) | 22 | 27 | 7 (65) | 21 | 21 | 0.3237 | 0.1755 | 0.4446 |
| Fruits (g) | 29 (284) | 40c | 41 | 49 (477) | 54 b | 57 | 66 (643) | 67a | 82 | <0.0001 | <0.0001 | <0.0001 |
| Beverages total (g) | 98 (954) | 439 c | 228 | 99 (960) | 475 b | 221 | 98 (963) | 497 a | 229 | <0.0001 | <0.0001 | <0.0001 |
| Coffee (g) | 70 (674) | 113c | 67 | 75 (723) | 291 a | 167 | 75 (724) | 264 b | 158 | <0.0001 | <0.0001 | <0.0001 |
| Tea (g) | 15 (141) | 175 | 144 | 22 (213) | 195 | 172 | 27 (260) | 201 | 169 | 0.4072 | 0.1432 | 0.2605 |
| Water (g) | 51 (498) | 170 c | 128 | 63 (611) | 196 b | 139 | 73 (712) | 224a | 149 | <0.0001 | <0.0001 | <0.0001 |
| Milk (incl. milk with chocolate flavor/fruits) (g) | 37 (256) | 140 | 120 | 37 (358) | 124 | 100 | 33 (322) | 118 | 95 | 0.0567 | 0.3336 | 0.5149 |
| Juice (g) | 29 (283) | 95 | 71 | 36 (348) | 98 | 73 | 36 (349) | 93 | 68 | 0.7467 | 0.9310 | 0.9168 |
| Cordial (g) | 5 (45) | 88 | 74 | 3 (31) | 68 | 49 | 2 (23) | 74 | 80 | 0.2370 | 0.2774 | 0.2553 |
| Cordial light (g) | 3(24) | 99 | 72 | 2 (21) | 80 | 63 | 1 (12) | 91 | 61 | 0.6213 | 0.6174 | 0.4768 |
| Carbonated soft drinks sugar sweetened (g) | 4 (40) | 128 a | 129 | 1 (13) | 47 b | 34 | 1 (5) | 77 a,b | 101 | 0.0037 | 0.0103 | 0.0237 |
| Carbonated soft drinks sugar light (g) | 2 (17) | 142 | 187 | 1 (11) | 55 | 27 | − (3) | 107 | 126 | 0.4415 | 0.6744 | 0.3888 |
| Beer (g) | − (2) | 79 | 44 | − (4) | 159 | 135 | 0 | n/a | n/a | 0.8205 | 0.4893 | 0.3807 |
| Wine/spirits (g) | 3 (30) | 17 | 22 | 3 (30) | 10 | 7 | 4 (42) | 7 | 4 | 0.0012 | 0.0022 | 0.0057 |
Under 1%. Abbreviations: n/a not applicable. p *. Unadjusted (ANOVA) p ** Adjusted for daily energy p *** adjusted for daily energy and education (ANCOVA). The Tukey–Kramer test for multiple comparisons was used. Different superscript letters indicate significantly different means for data adjusted for daily energy and education. p < 0.05 considered significant. Values for food intake were Log (10) transformed prior to analysis. Mean and SD are based on absolute values of intake. No statistical tests were carried out for % of consumers.
4. Discussion
This study examined the regularity of breakfast consumption, energy, macro- and micronutrient and food group intakes at breakfast in Denmark. The relationship between nutrient and food intakes at breakfast and the overall dietary quality was also assessed within the Danish population. The relationship between nutrient intakes at breakfast and overall dietary quality in Denmark by using the Nutrient Rich Food Index 9.3 (NRF 9.3) has not been published previously.
The study shows that breakfast is eaten relatively frequently by children and adults in Denmark. This is in line with other Danish studies [20,21,22]. More women than men eat breakfast regularly and adolescents eat most irregularly. This also has been found in other Danish and international studies [20,21,34]. The present study shows that breakfast provides approximately 18–20% of the daily energy in all age groups. This finding is in line with previous studies of breakfast in Denmark [8,9], thus indicating a relatively staple contribution of breakfast to the total energy intake.
The study shows that commonly consumed foods at breakfast for Danish children, adolescents and adults are bread, breakfast cereals, and dairy products. Beverages consumed at breakfast are primarily water and juice (children and adolescents), coffee, water and juice (adults). Breakfast is a good source of carbohydrates, dietary fibre, B vitamins, calcium and magnesium, and is relatively low in fat, added sugar and sodium. The contribution of riboflavin, biotin, calcium, and magnesium from breakfast is 20–30% of the daily intake. This is due to the relatively high intake of dairy products and cereals at breakfast. In the Danish diet, the intake of cereals and dairy products (incl. cheese) accounts for 52% of the intake of riboflavin and 43% of the intake of magnesium, while dairy products (incl. cheese) account for 59% of the intake of calcium [24]. No data on the contribution of biotin are available in DANSDA. Breakfast contributes with approximately 10% of the daily intake of vitamin A and D. This reflects the low intake of foods rich in these vitamins at breakfast, but also illustrates the relatively low fortification practices in Denmark. Only salt is mandatorily fortified with iodine and despite the possibility to fortify foods voluntarily, few foods are fortified with nutrients. This might be due to a negative attitude among consumers towards foods fortified with nutrients [35,36].
Previous Danish analyses on the different dimensions of socioeconomic position (income, employment status, educational level etc.) on diet, health behavior, and obesity have shown education to be the key social variable of dietary habits in Denmark [37,38,39]. Education was therefore chosen as a measure for SES in this study. However, in the present study, the characteristics of participants showed no differences in education across the tertiles of NRF 9.3 scores. In relation to the measurement of dietary quality, a Danish diet quality index (DQI) has been used previously and the studies have shown a higher dietary quality with increasing education [33,39]. The Danish DQI is based on intake of macronutrients and food groups included in the Danish FBDG (total fats, saturated fats, fruits and vegetables, fish, and added sugar) [33,40]. In contrast to the Danish DQI, the NRF 9.3 Index is based to a larger extent on micronutrient intakes. As the content of micronutrients included in the NRF 9.3 is generally adequate in the average Danish diet [24], this might be part of the explanation for the lacking relationship between dietary quality and education, when using NRF 9.3 as a measure of dietary quality in Denmark. However, more analyses are needed to examine the differences between the two indices, how they rank different dietary intakes in the Danish diet, and the relationship between intake of food and the nutrients they provide.
In this study, other factors than education show relation to dietary quality. The low dietary quality group for adults comprises a higher proportion of males, individuals with a sedentary lifestyle and daily smokers and a lower proportion of individuals with the intention to eat healthily. Overall, these data suggest that individuals in the low dietary quality group have a less healthy lifestyle compared to the medium and high-quality dietary groups. The less healthy lifestyle includes less healthy dietary and breakfast habits due to a lower intake of breakfast cereals including milk and fruits and a higher intake of non-whole grain wheat bread, fats on bread and pastry/cakes/biscuits (adults). This together with other dietary factors is reflected in a lower NRF 9.3 score. These results are in line with previous analyses of DANSDA data showing that males and individuals with no intention to eat healthily consume a less healthy diet overall and that men compared with women have more unhealthy dietary habits and a higher intake of non-whole grain bread, cheese, red meat and fats and lower intake of fruits and vegetables [24,37,41]. This is reflected in the breakfast habits as well. When comparing food intake in the groups with lowest and highest dietary quality, the study showed a higher intake of breakfast cereals, vegetables, fruits, dairy products and water, and lower non-whole grain bread in the group with highest dietary quality among adults. Many of these foods are included in the Danish FBDG and the healthier food patterns at breakfast could be examined further in order to identify key food patterns in relation to nutrient intakes. Prior to the analysis of food patterns, it could be useful to disaggregate the food intake at breakfast into single food items in order to examine the intake of high and low-fat dairy products, the intake of high and low sugary breakfast cereals as well as the intake of food low in salt. Examining the intake of specific food items, will create a basis for the future work on the recommendations for a healthy breakfast in Denmark.
This study reveals good dietary practices among breakfast consumers and forms a basis for future dietary advice in Denmark. The low consumption of foods rich in sugar and sodium should be highlighted as a healthy dietary habit in public health campaigns. Additionally, the relatively high contribution of dietary fibre could be emphasized. However, keeping in mind that the overall intake of dietary fibre and whole grain is too low in Denmark [7,24] and with the study showing a high proportion of adults and especially children and adolescents eating non-whole grain bread for breakfast, a nutritional focus could be to substitute the non-whole grain foods with whole grain foods. The high intake of non-whole grain bread at breakfast among adolescents in combination with a lower intake of daily dietary fibre than the other age groups indicates a potential for raising the daily dietary fibre and whole grain intake among adolescents by increasing the whole grain intake at breakfast. In order to qualify advice on whole grain products at breakfast, it could be useful to evaluate how much of the recommended amount of whole grain is derived from breakfast. In addition to raising attention to whole grain cereals at breakfast, a focus could be on the intake of fruits and vegetables. The current study shows that a high proportion of Danes do not eat vegetables or fruits at breakfast. As Danes eat too little fruits and vegetables [24], the intake of fruits especially could be increased at breakfast. Regarding the intake of beverages, the good practice of drinking water at breakfast could be highlighted.
It has not been the aim of the current work to analyze the dietary quality among regular and irregular consumers of breakfast and in the analysis of dietary quality, regular and irregular consumers of breakfast were treated as one group. Even if breakfast is consumed regularly by the majority of the population, a future research project could be to analyze if regular and irregular consumers of breakfast have a different overall dietary quality.
Strengths of the study include the large nationally representative sample of the Danish population, and the assessment of nutrient and food group intakes at all meals based on seven days. Weighting factors were not applied within the data set to account for non-response bias. This may be seen as a limitation as adults with low educational level are underrepresented in DANSDA [24]. Therefore, we cannot exclude the possibility of systematic differences in breakfast and dietary habits between participants and non-participants as these groups differ in health behaviour [42,43]. The consequence may be the recording of healthier Danish breakfast habits than what is actually the case because higher educated individuals eat more healthily than lower educated. Still, adjustments were made for socioeconomic status in the statistical analyses.
Misreporting occurs in dietary surveys due to self-reported food intake. Previous research has shown that subjects with a high BMI, non-smokers, and subjects who eat healthily to avoid being overweight mostly under-report energy intake [44]. However, misreporting includes both over- and under-reporting and the exclusion of those misreporting may introduce selection and unknown biases into the data [45]. Instead of excluding implausible reporters from the current study, the energy intake was controlled for in the statistical analysis.
By expressing the contribution of nutrients from breakfast to daily energy and nutrient intakes, the study highlights that breakfast is an important meal providing many key nutrients. Together with the analysis of the impact of breakfast on the overall dietary quality and information on the percentage of consumers of different food groups, the results form a solid base for the future work of nutrient-based recommendations. The results can help Danish authorities in formulating more meal-based dietary guidelines.
5. Conclusions
The present study shows that breakfast is an important meal providing many key nutrients and it is high in dietary fibre and low in added sugars, total fat, saturated fat, and sodium. The analysis on the impact of breakfast on overall dietary quality form a solid base for future work of nutrient-based recommendations. The results can help Danish authorities in formulating more meal based dietary guidelines. The use of NRF 9.3 enables the comparison of dietary quality in different countries, but future research is needed to investigate the impact of using the NRF 9.3 index on a Danish diet to examine dietary quality. Additionally, further examination of why different dietary quality indices show different results regarding the relationship between education and dietary quality needs to be carried out.
On the basis of the results from the counties participating in IBRI, a set of guiding principles to derive nutrient guidelines for breakfast will be developed. The principles will be based on the nutritional profiles of breakfast among individuals in the NRF 9.3 upper tertile, taking into account the current public health interests in specific nutrients. Two sets of nutritional guidelines for breakfast will be developed: one for children and adolescents and another for adults.
The standardized approach used in IBRI can be applied on other meals in Denmark in order to form a basis for meal-based dietary guidelines, for example, lunch and dinner. This work can serve as a more evidence-based platform for authorities for the formulation of future meal-based dietary guidelines.
Overall, the study shows interesting results on both the food and nutrient level and more analyses can be carried out in order to qualify future meal-based guidelines.
Acknowledgments
Cereal Partners Worldwide. Orbe. Switzerland funded the work of the International Breakfast Research Initiative and funded the publication of the series of papers in open access. All participants within the International Breakfast Research Initiative have contributed to fruitful discussions. The Danish National Survey of Diet and Physical Activity (DANSDA) was internally funded. The authors would like to express their gratitude to all the participants in DANSDA.
Supplementary Materials
The following are available online at http://www.mdpi.com/2072-6643/10/8/1085/s1, Table S1: Sociodemographic and lifestyle characteristics of children and adults breakfast consumers across tertiles of NRF 9.3. Figure S1: Mean intake of solid foods (g) at breakfast according to age group. Figure S2: Mean intake of beverages (g) at breakfast according to age group.
Author Contributions
S.F., J.M., and A.B.-J. conceived the study, designed the analyses of this study and were responsible for the design and collection of data from The Danish National Survey of Diet and Physical Activity. C.T., K.K. and S.F. carried out the analyses. S.F. was responsible for analyses of data and writing the manuscript. All authors participated in the discussion of the results and revision of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest. A Governing Principles document outlining rights and duties in this project was signed by all International Breakfast Research Initiative researchers or their institutions and the project sponsors. A copy of the document is included in the supplementary material. A research grant were received by S.F. on behalf of the Technical University of Denmark in order to perform the analyses within the International Breakfast Research Initiative.
References
- 1.Dye L. The Importance of Breakfast in Europe. A Review of National Policies and Health Campaigns. European Breakfast Cereal Association; 2017. [(accessed on 1 April 2018)]. Available online: http://www.breakfastisbest.eu/docs/102017/BIB_Report_Executive_Summary_Importance_of_Breakfast_in_Europe_2017.pdf. [Google Scholar]
- 2.De la Hunty A., Gibson S., Ashwell M. Does regular breakfast cereal consumption help children and adolescents stay slimmer? A systematic review and meta-analysis. Obesity Facts. 2013;6:70–85. doi: 10.1159/000348878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nordic Nutrition Recommendations 2004 . Integrating Nutrition and Physical Activity. 4th ed. Nordic Council of Ministers; Copenhagen, Denmark: 2004. [Google Scholar]
- 4.Nordic Nutrition Recommendations 2012 . Integrating Nutrition and Physical Activity. 5th ed. Nordic Council of Ministers; Copenhagen, Denmark: 2014. [Google Scholar]
- 5.Danish Veterinary and Food Administration. [(accessed on 28 May 2018)]; Available online: http://altomkost.dk/tips/til-maaltiderne/morgenmad/
- 6.Danish Whole Grain Partnership. [(accessed on 28 May 2018)]; Available online: www.fuldkorn.dk/english.
- 7.Mejborn H., Ygil K.H., Fagt S., Trolle E., Korup K., Christensen T. Danskernes Fuldkørnsindtag 2011–2013 (Intake of Whole Grain in Denmark—in Danish); National Food Institute: 2014. [(accessed on 1 June 2018)]; Available online: https://www.food.dtu.dk/-/media/Institutter/Foedevareinstituttet/Publikationer/Pub-2014/Danskernes_fuldkornsindtag_2011-2013.ashx.
- 8.Fagt S., Groth M.V., Andersen N.L. Danskernes Kostvaner 1995. Mad og Måltider (In Danish with an English Summary) Fødevaredirektoratet; København, Demark: 2000. 2000:06. [Google Scholar]
- 9.Christensen L.M., Kørup K., Trolle E., Matthiessen J., Fagt S. Børn og Unges Måltidsvaner 2005–2008 (In Danish with an English Summary) DTU Fødevareinstituttet; København, Demark: 2012. [(accessed on 28 May 2018)]. Available online: http://orbit.dtu.dk/files/54035355/rapport_m_ltidsvaner2005_2008_4_19_r_jan.pdf. [Google Scholar]
- 10.Rampersaud G.C., Pereira M.A., Girard B.L., Adams J., Metzl J.D. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J. Am. Diet. Assoc. 2005;105:743–760. doi: 10.1016/j.jada.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Priebe M.G., McMonagle J.R. Effects of ready-to-eat-cereals on key nutritional and health outcomes: A. systematic review. PLoS ONE. 2016;11:1–35. doi: 10.1371/journal.pone.0164931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cahill L.E., Chiuve S.E., Mekary R.A., Jensen M.K., Flint A.J., Hu F.B., Rimm E.B. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation. 2013;128:337–343. doi: 10.1161/CIRCULATIONAHA.113.001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uemura M., Yatsuya H., Hilawe E.H., Li Y., Wang C., Chiang C., Otsuka R., Toyoshima H., Tamakoshi K., Aoyama A. Breakfast skipping is positively associated with incidence of type 2 diabetes mellitus: Evidence from the aichi workers cohort study. J. Epidemiol. 2015;25:351–358. doi: 10.2188/jea.JE20140109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mekary R.A., Giovannucci E., Willett W.C., van Dam R.M., Hu F.B. Eating patterns and type 2 diabetes risk in men: Breakfast omission, eating frequency, and snacking. Am, J. Clin Nutr. 2012;95:1182–1189. doi: 10.3945/ajcn.111.028209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mekary R.A., Giovannucci E., Cahill L., Willett W.C., van Dam R.M., Hu F.B. Eating patterns and type 2 diabetes risk in older women: Breakfast consumption and eating frequency. Am. J. Clin. Nutr. 2013;98:436–443. doi: 10.3945/ajcn.112.057521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szajewska H., Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit. Rev. Food Sci. Nutr. 2010;50:113–119. doi: 10.1080/10408390903467514. [DOI] [PubMed] [Google Scholar]
- 17.Hoyland A., Dye L., Lawton C.L. A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr. Res. Rev. 2009;22:220–243. doi: 10.1017/S0954422409990175. [DOI] [PubMed] [Google Scholar]
- 18.St-Onge M.P., Ard J., Baskin M.L., Chiuve S.E., Johnson H.M., Kris-Etherton P., Varady K., American Heart Association Obesity Committee of the Council on Lifestyle and Cardiometabolic Health. Council on Cardiovascular Disease in the Young. Council on Clinical Cardiology et al. Meal timing and frequency: Implications for cardiovascular disease prevention: A Scientific Statement from the American Heart Association. Circulation. 2017;135:e96–e121. doi: 10.1161/CIR.0000000000000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dhurandbar E.J., Dawson J., Alcorn A., Larsen L.H., Thomas E.A., Cardel M., Bourland A.C., Astrup A., St-Onge M.-P., Hill J.O., et al. The effectiveness of breakfast recommendations on weight loss: A randomized controlled trial. Am. J. Clin. 2014;100:507–513. doi: 10.3945/ajcn.114.089573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Christensen A.I., Severin M., Holmberg T., Eriksen L., Toftager M., Zachariassen A., Ekholm O., Tolstrup J.S., Grønbaek M., Curtis T. KRAM-Undersøgelsen i tal og Billeder (In Danish) National Institute of Public Health, University of Southern Denmark; Copenhagen, Demark: 2009. [Google Scholar]
- 21.Inchley J., Currie D., Young T., Samdal O., Torsheim T., Augustson L., Mathison F., Aleman-Diaz A., Molcho M., Weber M., et al. Health Behavior in School-Aged Children (HBSC) Study: International Report from the 2013/2014 Survey. WHO Regional Office for Europe; Copenhagen, Demark: 2016. [(accessed on 20 March 2018)]. Growing up unequal: Gender and socioeconomic differences in young people’s health and well-being. Available online: http://www.euro.who.int/en/publications/abstracts/growing-up-unequal.-hbsc-2016-study-20132014-survey. [Google Scholar]
- 22.COOP . In: Danskernes Madvaner 2016. Roland T., Poulsen D., Steenberg M., Obelitz M., Falk J., editors. Coop Analyse; Albertslund, Demark: 2016. [(accessed on 30 March 2018)]. Available online: https://om.coop.dk/Upload/om.coop.dk/Publikationer/analyser/Danskernes%20Madvaner%202016_Coop%20Analyse.pdf. [Google Scholar]
- 23.Gibney M.J., Barr S.I., Bellisle F., Drewnowski A., Fagt S., Livingstone B., Masset G., Varela-Moreiras G., Moreno L., Smith J., et al. Breakfast in human nutrition: The International Breakfast Research Initiative. Nutrients. 2018;10:559. doi: 10.3390/nu10050559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedersen A.N., Christensen T., Matthiessen J., Knudsen V.K., Rosenlund-Sørensen M., Biltoft-Jensen A., Hinsch H.J., Ygil K.H., Kørup K., Saxholt E., et al. Danskernes Kostvaner 2011–2013. Høvedresultater (In Danish with an English Summary) DTU Fødevareinstituttet; Cøbenhavn, Demark: 2015. [(accessed on 20 March 2018)]. Available online: http://www.food.dtu.dk/Publikationer/Ernaering-og-kostvaner/De_nationale_kostundersoegelser. [Google Scholar]
- 25.Biltoft-Jensen A.P., Matthiessen J., Rasmussen L.B., Fagt S., Groth M.V., Hels O. Validation of the Danish 7-day pre-coded food diary among adults: Energy intake v. energy expenditure and recording length. Br. J. Nutr. 2009;102:1838–1846. doi: 10.1017/S0007114509991292. [DOI] [PubMed] [Google Scholar]
- 26.Danish Food Data. [(accessed on 26 October 2016)]; Available online: www.frida.fooddata.dk.
- 27.Drewnowski A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am. J. Clin. Nutr. 2010;91:1095S–1101S. doi: 10.3945/ajcn.2010.28450D. [DOI] [PubMed] [Google Scholar]
- 28.Fulgoni V.L., III, Keast D.R., Drewnowski A. Development and validation of the Nutrient-Rich Foods Index: A tool to measure nutritional quality of foods. J. Nutr. 2009;139:1549–1554. doi: 10.3945/jn.108.101360. [DOI] [PubMed] [Google Scholar]
- 29.European Food Safety Authority Regulation (eu) no 1169/2011 of the European parliament and of the council of 25 october 2011. Off. J. Eur. Union. 2011;1169/2011:18–63. [Google Scholar]
- 30.Guideline: Sugar Intake for Adults and Children. World Health Organisation; Geneva, Switzerland: 2015. [(accessed on 1 February 2018)]. Available online: http://apps.who.int/iris/bitstream/handle/10665/149782/9789241549028_eng.pdf;jsessionid=44345FBF70B58A25B4BB48DF36D3D5F2?sequence=1. [Google Scholar]
- 31.European Food Safety Authority Scientific opinion on dietary reference values for carbohydrates and dietary fibre. EFSA J. 2010;8:1462. [Google Scholar]
- 32.Groth M.V., Fagt S., Brøndsted L. Social determinants of dietary habits in Denmark. Eur. J. Clin. Nutr. 2001;55:959–966. doi: 10.1038/sj.ejcn.1601251. [DOI] [PubMed] [Google Scholar]
- 33.Groth M.V., Sørensen M.R., Matthiessen J., Fagt S., Landvad N., Knudsen V.K. Disparities in dietary habits and physical activity in Denmark and trends from 1995 to 2008. Scand. J. Public Health. 2014;42:611–620. doi: 10.1177/1403494814547668. [DOI] [PubMed] [Google Scholar]
- 34.Barr S.I., DiFrancesco L., Fulgoni V.L., 3rd Breakfast consumption is positively associated with nutrient adequacy in Canadian children and adolescents. Br. J. Nutr. 2014;112:1373–1383. doi: 10.1017/S0007114514002190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsalis G., Hummelshøj I., Lahteenmaki L. Undersøgelse af Forbrugernes Holdning til Produkter, der er Tilsat D-Vitamin af Sundhedsmaessige Årsager (Study of Attitudes towards Products Fortified woth Vitamin D for Health Reasons—In Danish) Aarhus University, Business and Social Sciences MAPP-Centre for Research and Customer Relations in the Food Sector; Aarhus, Demark: 2015. [(accessed on 1 June 2018)]. Available online: https://pure.au.dk/ws/files/93733978/DCArapport_d_vitamin_net.pdf. [Google Scholar]
- 36.Bech-Larsen T., Grunert K.G., Poulsen J.B. The Acceptance of Functional Foods in Denmark, Finland and the United States. The Aarhus School of Business; Aarhus, Demark: 2001. [(accessed on 1 June 2018)]. Working paper no 73. Available online: https://pure.au.dk/ws/files/32301883/0003055.pdf. [Google Scholar]
- 37.Groth M.V., Fagt S. Danskernes Kostvaner. Måltidsvaner, Holdninger, Sociale Forskelle og Sammenhaeng med Anden Livsstil. (In Danish with English summary) Fodevaredirektoratet; København, Demark: 2003. [(accessed on 25 July 2018)]. Available online: http://www.food.dtu.dk/Publikationer/Ernaering-og-kostvaner/De_nationale_køstundersoegelser. [Google Scholar]
- 38.Groth M.V., Fagt S., Stockmarr A., Matthiessen J., Biltoft-Jensen A. Dimensions of socioeconomic position related to body mass index and obesity among Danish women and men. Scand. J. Public Health. 2009;37:418–426. doi: 10.1177/1403494809105284. [DOI] [PubMed] [Google Scholar]
- 39.Groth M.V., Christensen L.M., Knudsen V.K., Sørensen M.R., Fagt S., Ege M., Matthiessen J. Sociale Forskelle. Børns Kostvaner, Fysiske Aktivitet og Overvaegt & Voksnes Kostvaner. DTU Fødevareinstituttet; København, Demark: 2013. [(accessed on 25 July 2018)]. Available online: http://www.food.dtu.dk/Publikationer/Ernaering-og-kostvaner/De_nationale_kostundersoegelser. [Google Scholar]
- 40.Knudsen V.K., Fagt S., Trolle E., Matthiessen J., Groth M.V., Biltoft-Jensen A., Sørensen M.R., Pedersen A.N. Evaluation of dietary intake in Danish adults by means of an index based on food-based dietary guidelines. [(accessed on 25 July 2018)];Food Nutr. Res. 2012 56 doi: 10.3402/fnr.v56i0.17129. Available online: https://www.tandfonline.com/doi/abs/10.3402/fnr.v56i0.17129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fagt S., Biltoft-Jensen A., Matthiessen, Groth M.V., Christensen T., Trolle E. Danskernes Kostvaner 1995–2006. Status og Udvikling med Henblik på Frugt og Grønt Samt Sukker. DTU Fødevareinstituttet; København, Demark: 2008. [(accessed on 25 July 2018)]. Available online: http://www.food.dtu.dk/Publikationer/Ernaering-og-kostvaner/De_nationale_kostundersoegelser. [Google Scholar]
- 42.Christensen A.I., Ekholm O., Gray L., Glumer C., Juel K.W. What is wrong with non-respondents? Alcohol-, drug- and smoking-related mortality and morbidity in a 12-year follow-up study of respondents and non-respondents in the Danish Health and Morbidity Survey. Addiction. 2015;110:1505–1512. doi: 10.1111/add.12939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tolonen H., Laatikainen T., Helakorpi S., Talala K., Martelin T., Prattala R. Marital status, educational level and household income explain part of the excess mortality of survey non-respondents. Eur. J. Epidemiol. 2010;25:69–76. doi: 10.1007/s10654-009-9389-9. [DOI] [PubMed] [Google Scholar]
- 44.Rasmussen L.B., Matthiessen J., Biltoft-Jensen A.P., Tetens I. Characteristics of misreporters of dietary intake and physical activity. Public Health Nutr. 2007;10:230–237. doi: 10.1017/S136898000724666X. [DOI] [PubMed] [Google Scholar]
- 45.Poslusna K., Ruprich J., de Vries J.H., Jakubikova M., van’t Veer P. Misreporting of energy and micronutrient intake estimated by food records and 24 h recalls, control and adjustment methods in practice. Br. J. Nutr. 2009;101:S73–S85. doi: 10.1017/S0007114509990602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.