ABSTRACT
A 49-year-old man, who presented with new onset dyspnea on exertion and fatigue without clear history of a typical erythema migrans rash, was found to have complete atrioventricular (AV) heart block with positive serology for Lyme disease. A complete stepwise reversal of the AV block was achieved shortly after the initiation of intravenous antibiotic treatment.
KEYWORDS: Lyme carditis, atrioventricular heart block, lyme disease, lyme borreliosis, heart block
1. Introduction
Lyme disease is a multisystem illness caused by a tick-borne spirochetal infection, Borrelia Burgdorferi, that is acquired through the Ixodes tick bite that it is known to be the most common tick-borne infection in the northern hemisphere with clusters in endemic areas (i.e. northeast and north-central USA) [1,2]. Although Lyme carditis (LC) is an uncommon manifestation of the early disseminated phase (weeks to months after a tick bite), it can present with various degrees of atrioventricular (AV) blocks, and if not promptly treated can be fatal [3]. We hereby present a case of completely reversed third-degree AV block due to Lyme disease.
2. Case report
2.1. Presentation
A 49-year-old man, avid jogger from Northern Maryland, with history of asthma and attention deficit disorder, presented with new onset worsening fatigue and dyspnea on exertion during his typical routine jogging activities. He normally runs 6–8 miles in the woods near his home, 4 days a week. Just recently, in the last 7–10 days, he noticed progressive worsening in his performance, due to dyspnea, fatigue, and intermittent chest tightness, forcing him to have several breaks during his practice. Thus, he sought the attention of his primary care physician, who performed a 12-lead EKG that showed third-degree AV block. The patient was then sent to the hospital for further management after consulting an outpatient cardiologist.
In the Emergency Department, upon further questioning, the patient did recall an unspecific rash on his right leg about 4 weeks prior, but he denied noticing any insect bites. He also denied fever, chills, arthralgia, or sick contact. Of note, his cardiac history was unremarkable and his EKG done 5 months earlier for routine check-up was completely normal (Figure 1). The patient was asymptomatic and his physical exam was largely unremarkable, except for bradycardia and irregular rhythm. His initial laboratory work-up was remarkable for negative troponin levels, normal CBC and CMP, and positive Lyme serology (The Lyme IgG/IgM total antibody titer was 2.57 (0.00–0.90). Quantitative IgM was 3.27 (0.00–0.79.) The Western Blot was positive for 10 of 10 IgG bands and 3 of 3 IgM bands). Serial EKG’s were obtained during his stay (Figure 1). Additionally, an Echocardiogram and a chest radiogram were obtained and were normal.
Figure 1.
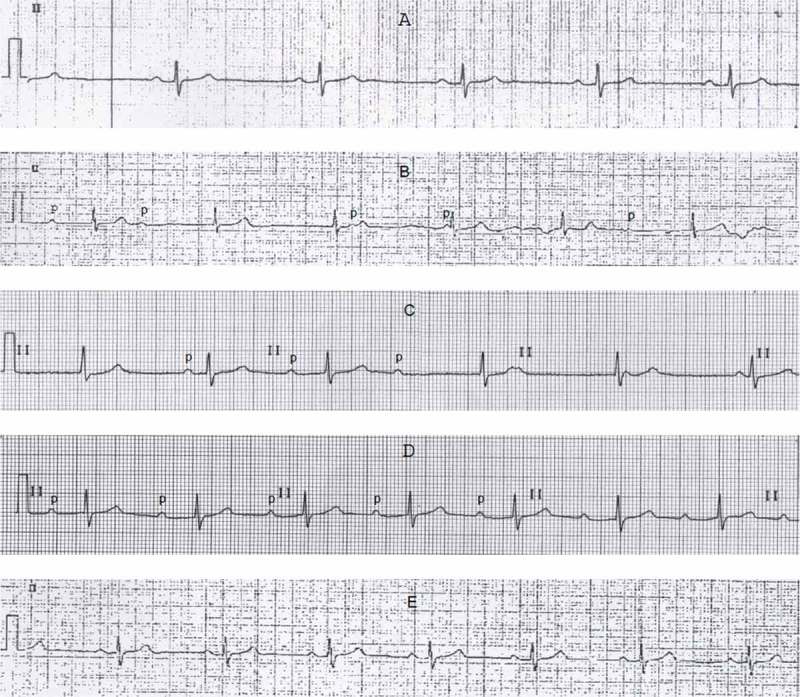
Serial electrocardiograms, lead II strips. (a): normal, 5 months prior to admission. (b): Complete third-degree atrioventricular (AV) block, at primary office 12 h before admission. (c): Type I second-degree AV block, 2 h after admission and antibiotic therapy. (d): first-degree AV block, 12 h after admission and antibiotic therapy. (e): normal, at discharge.
2.2. Management and progression
The patient was promptly admitted to the telemetry unit, and in addition to his home medications (budesonide-formoterol, montelukast, albuterol, and methylphenidate), he was started empirically on IV 2 g Ceftriaxone daily (given the high suspicion of LC in an endemic area like Maryland). During the first 24 h, although asymptomatic, patient showed multiple episodes of bradycardia on telemetry. On his second day, and just after only 2 doses of Ceftriaxone, patient’s cardiac rhythm was progressively shifting from third-degree AV block to second-degree, then first-degree before being back to normal regular and sinus within 48 h from admission. The patient was then discharged home to complete a total of 21 days of IV Ceftriaxone, to treat a presumed LC.
2.3. Follow-up
On his 2 weeks follow-up appointment with his cardiologist, he was asymptomatic, and he had already resumed his jogging practice without notable limitations. His repeat EKG was normal.
3. Discussion
LC was first described in 1980 [4], and can present in up to 10% of patients who encounter Lyme disease, especially if not appropriately treated [5]. In this report, we presented a case of LC with complete AV block that quickly reversed to regular sinus rhythm after the prompt initiation of antibiotic. Our suspicion of Lyme disease and hence LC in our patient was based on a history of exposure and geographic risk and presentation with conduction disturbance in absence of baseline cardiac history. Unsurprising was the lack of documented tick bite and erythema migrans in our patient, knowing that only one-third of patients diagnosed with Lyme can recall having a tick bite and only 75–90% of them can recall or have erythema migrans [6]. Conduction disturbances are the most common manifestations of LC, presumably due to endocardium inflammatory infiltrates of the conduction system, and it can present with multiple levels of AV blocks with higher prevalence of third-degree then second-degree and first-degree, which are 49%, 16%, and 12%, respectively [7]. In a systematic review, Forrester et al. reviewed a total of 45 cases of complete AV block due to LC, 40% of these cases required transvenous pacing, and in all other cases the median time to achieve complete resolution to normal sinus rhythm or improvement to first-degree block was 6 days (range 1–42) [8]. Although the stepwise complete reversal of the complete AV block in LC has been shown in several case reports [9–11], only few reports have shown a quick reversal to normal sinus rhythm within days. We don’t know whether our patient developed fluctuating AV block particularly Mobitz type II which is the more common presentation, prior to complete block, the remarkable AV block regression from third- to second- and first-degree before a complete resolution shortly after the initiation of adequate antibiotic treatment, suggests anatomic healing of inflamed endocardium.
4. Conclusion
LC is a serious complication of Lyme disease that should always be considered in endemic areas, especially in absence of pre-existing cardiac disease even in the absence of typical presentation. It, therefore, requires early recognition and prompt antibiotic treatment, and complete resolution with benign outcome is generally achieved.
Disclosure statement
No potential conflict of interest was reported by the authors.
Patient consent
Written informed consent was obtained from the patient for the publication of this case.
References
- [1].Centers for Disease, C. and Prevention Notice to readers: final 2012 reports of nationally notifiable infectious diseases. MMWR Morb Mortal Wkly Rep. 2013;62(33):669–682. [PMC free article] [PubMed] [Google Scholar]
- [2].Schwartz A.M., Hinckley A. F., Mead P. S, et al. Surveillance for Lyme disease – USA, 2008-2015. MMWR Surveill Summ. 2017;66(22):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lelovas P., Dontas I., Bassiakou E, et al. Cardiac implications of Lyme disease, diagnosis and therapeutic approach. Int J Cardiol. 2008;129(1):15–21. [DOI] [PubMed] [Google Scholar]
- [4].Steere A.C., Batsford W.P., Weinberg M, et al. Lyme carditis: cardiac abnormalities of Lyme disease. Ann Intern Med. 1980;93(1):8–16. [DOI] [PubMed] [Google Scholar]
- [5].Krause PJ, Bockenstedt LK.. Cardiology patient pages. Lyme disease and the heart. Circulation. 2013;127(7):e451–4. [DOI] [PubMed] [Google Scholar]
- [6].Bateman H, Sigal L. Update on Lyme carditis. Curr Infect Dis Rep. 2000;2(4):299–301. [DOI] [PubMed] [Google Scholar]
- [7].Van der Linde MR. Lyme carditis: clinical characteristics of 105 cases. Scand J Infect Dis Suppl. 1991;77:81–84. [PubMed] [Google Scholar]
- [8].Afari M.E., Marmoush F, Rehman MU, et al. Lyme carditis: an interesting trip to third-degree heart block and back. Case Rep Cardiol. 2016;2016:5454160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Forrester JD, Mead P. Third-degree heart block associated with Lyme carditis: review of published cases. Clin Infect Dis. 2014;59(7):996–1000. [DOI] [PubMed] [Google Scholar]
- [10].Timmer S.A., Boswijk DJ, Kimman GP, et al. A case of reversible third-degree AV block due to Lyme carditis. J Electrocardiol. 2016;49(4):519–521. [DOI] [PubMed] [Google Scholar]
- [11].Fuster LS, Gul EE, Baranchuk A. Electrocardiographic progression of acute Lyme disease. Am J Emerg Med. 2017;35(7):1040 e5–1040 e6. [DOI] [PubMed] [Google Scholar]


