Abstract
Health 360x is a mobile health application and social platform that integrates self-monitoring and decision support for preventive health. We studied 240 diabetic patients in primary care practices and a church community in metropolitan Atlanta. Health coaches were trained on the Health 360x curriculum, which was adapted from the American Association of Diabetes Educators. Participants worked with the health coaches to set goals for diabetes self-management. The intervention included weekly coaching for 12 weeks and online peer networking. Outcome variables included blood pressure, physical activity, and blood glucose that showed significant improvement at 12 weeks and 12 months compared to baseline. Focus group testing revealed that references for empowerment and engagement were associated with positive clinical outcomes. Barriers to adoption and use of the technology were inability to use the internet and concern about privacy and security of health data. Future efforts will integrate a multidisciplinary training dashboard with considerable attention to education on security features including data encryption and sign-on verification.
INTRODUCTION
Chronic conditions such as diabetes and high blood pressure increase with age; a 2017 RAND report estimate that nearly 150 million Americans are living with at least one chronic condition; approximately 100 million of them have more than one, and nearly 30 million are living with five or more chronic conditions (1). Individuals with five or more chronic conditions, represent about 12% of the US adult population, but account for more than 1 trillion dollars (40%) of US health spending. People who are 65 years of age and older are most likely to have chronic health problems, which is a significant burden to the health care system. However, the personal and long-term economic costs due to lost productivity impact 50% of Americans in their mid-40s to mid-60s who are living with multiple health conditions. Social determinants such as poor access to diagnosis and preventive health services further exacerbate health disparities among Americans living with chronic conditions (2,3).
In its 2012 report titled “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America” (4), the National Academy of Medicine proposed a vision that integrates science and informatics with real-time access to knowledge, digital capture of the care experience, and patient-clinician partnerships driven by engaged and empowered patients. In this model, the learning health care system is centered on patient needs and perspectives and promotes the inclusion of patients, families, and other caregivers as vital members of the continuously learning care team. Such patient-centered and community-engaged intervention is especially relevant to communities and populations with high disease burden and health disparities (5). Advances in mobile health technology and health information offer new opportunities to innovate chronic care delivery (6-9). We describe our research with a technology-enabled health coaching model for diabetes self-management that is grounded in behavior change theory.
MATERIALS AND METHODS
System and Method for Chronic Illness Care
The technology is based on the patent, “System and Method for Chronic Illness Care” (10). The patent was issued to Morehouse School of Medicine in 2012, and assignment was transferred to AccuHealth Technologies, a faculty start-up company. The invention relates to a computerized system programmed for providing care support to patients with chronic illness. The system includes a medical professional module adapted for receiving, storing, and providing data in communication with medical professional(s) at the point of care; a health-coach module adapted for receiving, storing, and providing data in communication with patient(s) and other health coach(es); a patient module adapted for receiving, storing, and providing data in communication with patient(s); and a public-health module adapted for receiving, storing, and providing data in communication with a research professional(s). Each module is operatively associated with the others through a network.
The AccuHealth Technologies development team partners with clinicians and informaticians at Morehouse School of Medicine for research and development, funded in part by the National Institutes of Health and the American Heart Association.
Health 360x Mobile and Web-Based Application
AccuHealth Technologies team has been developing, deploying and supporting a multi-faceted technology for Health 360x (H360x) (previously known as e-HealthyStrides) that includes web, mobile android, and iOS applications; community networking and social software; database synchronization; web services; onboard database caches; et cetera, for more than 4 years. Web device connectivity and database synchronization with Microsoft HealthVault (Microsoft, Redmond, Washington) have been features of H360x focused on diabetes and cardiovascular self-monitoring and management for more than 5 years. The development of the mobile technologies began in 2012, and testing for mobile applications began in 2013. The multifaceted nature of the technology supported by a broad patent presents a unique opportunity to develop application program interfaces to wearable devices, other applications, and the electronic medical records (EMR).
What are barriers to adoption and sustained use of H360x (e-HealthyStrides) technology in care settings, in ways that bring value to patients and clinicians?
Gap Analysis (Preliminary Data)
The objective of the gap analysis is to determine: 1) acceptability of H360x (an interactive, internet-based, patient-driven, diabetes self-management support and social networking program) among Morehouse Community Physicians’ Network (CPN) patients with diabetics; 2) evaluate efficacy for diabetes self-management (DSM) behavior change; and 3) determine success factors for use of e-HealthyStrides technology. The gap analysis was published by Pemu et al. (11). A total of 146 patients diagnosed with diabetes, as classified by the International Classification of Diseases, 10th revision (ICD-10) (12) were enrolled from three primary care practices and evaluated using the following survey tools: Diabetes Empowerment Scale (13,14); Diabetes Knowledge Test (DKT) (15,16); Patient Assessment of Chronic Illness Care (17); Consumer Health Information Technology survey, a locally developed instrument; and the American Association of Diabetes Educators seven self-care behaviors (AADE7) (18). All survey questions were scored on a scale of 1 to 5, with 1 being the lowest score and 5 the highest. Eighty-two percent of participants were female, 95% self-identified as black or African American, and the average age was 58 years old. Although a majority (70%) owned or had easy access to a computer, only 25% had used the internet to help in managing their overall health and 18% reported using the internet for information about diabetes. Whereas 35% had no prior experience with the computer/internet, they were enthusiastic to learn. Seventeen percent had high school education or less; 46% had college, graduate, or professional degrees; and 37% had some college or technical school. The number of years since diagnosis of diabetes varied widely: 37% reported being diabetic for 6 to 10 years, 8% for less than 1 year, 28% for 1 to 5 years, and 11% for 11 to 20 years. Six (6%) of the group had been diabetic more than 20 years. Seventy-one percent completed some diabetes self-management training previously. Diabetes knowledge was low to average based on mean DKT score: 13.3 ± 3.88 of 23. The patient activation scores were significantly higher than scores for problem solving/contextual counseling (chi-square = 40.36; P = 0.001); goal setting (chi-square = 51.45; P = 0.0001). The scores from the Patient Assessment of Chronic Illness Care suggest a need for more assistance/support for problem solving/contextual counseling, follow-up/care coordination, and delivery system design/decision support.
H360x will empower and engage patients in sustained DSM, health coaching, and peer support.
Participant Group
Study participants were recruited based on a convenience sampling from three primary care practices and a community church:
Three CPN member practices all in metropolitan Atlanta. CPN is designated by the Agency for Healthcare Research and Quality as a practice-based research network (19). CPN member practices include 100 practices in metropolitan Atlanta, Macon, and Columbus, Georgia. CPN practices are small independent practices (one to four clinicians), and the majority provide primary care services. The CPN is organized as an academic–community research collaboration: practices sign a business associate agreement with Morehouse School of Medicine (MSM) to share clinical data, and to participate as co-investigators in MSM-sponsored, and institutional review board–approved research studies (20,21).
Big Bethel African Methodist Episcopal (BBAME) Church is a 3,000-member historic church in downtown Atlanta with an average weekly church attendance of approximately 880 adults. BBAME is a Connectional Church and has 47 ministries, including a very active Health Ministry.
Theoretical Framework for Behavior Change Intervention
The conceptual framework (22) for H360x uses the cognitive behavior change theory, known as COM-B, which is a behavior system that frames behavior as changeable and adaptable in a bidirectional manner based on capability, opportunity, motivation. Capability is the psychological and physical capacity to engage in the activity concerned, including the necessary knowledge and skills. Motivation is largely governed by the brain processes that energize and direct behavior, including goal-directed conscious decision-making, habitual processes, emotional response, as well as analytical decision-making. Opportunity includes factors that lie outside the individual and facilitate or prompt the behavior (22).
H360x Ecosystem: Enabling Patient-Centered Health
The H360x ecosystem design incorporates constructs from the model of supportive accountability and the COM-B system (22) to create a social support that enables and sustains behavior change. In Figure 1, the concentric circles reference spheres of influence on behavior change.
Fig. 1.
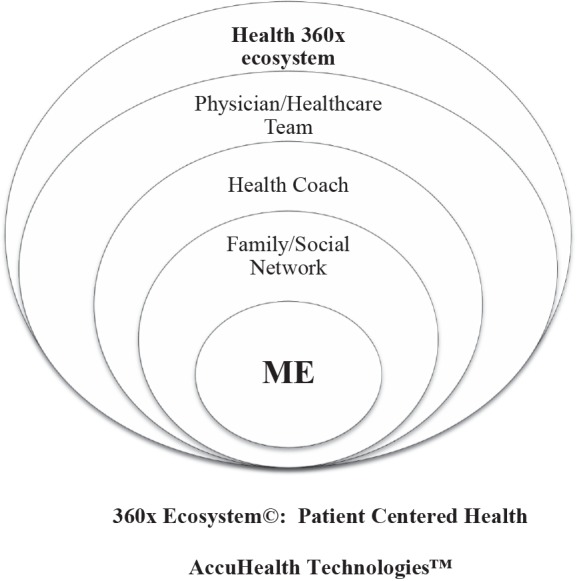
The Health 360x ecosystem mediates patient-centered behavior intervention, with spheres of influence beginning with the patient, family and social networks, health coaching, and the health system.
The H360x ecosystem also integrates the patient-centered theme of the Institute of Medicine Vision of Best Care at Lower Cost, the Path to Continuously Learning Health Care in America (4). The patient-clinician pillar begins with the engaged and empowered patient; according to the Institute of Medicine vision, “a learning health care system is anchored on patient needs and perspectives and promotes the inclusion of patients, families, and other caregivers as vital members of the continuously learning care team” (4).
At the core of the patient-centered H360x ecosystem is “ME” which references self-monitored and data-driven decision support. Concentric circles surrounding ME begin with family, friends, and social network; these individuals are physically and/or emotionally closest to the patient and likely to exert long-term influence on behavior change. The next concentric circle is the Health Coach: H360x integrates curriculum-based and disease-specific coaching support. The Physician/Healthcare Team is the outermost circle of the H360x ecosystem and is designed to enable bidirectional sharing of data between H360x and the practice/health system EMR patient portal.
H360x Behavior Intervention elements are education, monitoring with tailored-in-the-moment feedback, persuasion, modeling, enablement, and incentives (Table 1). These elements directly affect an individual’s capability, opportunity and motivation for behavior change. Health coaches’ involvement is designed to sustain engagement by engendering accountability, bond, and legitimacy (22).
TABLE 1.
How COM-B Conceptual Framework Aligns With Health 360x Elements and Potential Mechanistic Link to Behavior Change
| Health 360x Elements | Mechanistic Linkage | Intervention Elements | COM-B Behavioral Constructs | Outcome |
| Curriculum Monitoring | Engagement | Education Persuasion | Capability: physical or psychological | Behavior change |
| Tailored in-the moment feedback | Training | Opportunity: social or physical | ||
| Social networks | Modeling | |||
| Videos/skill building | Incentive | |||
| I-stories | Enablement | Motivation: automatic and reflective | ||
| Competitions/prizes | ||||
| Personal profiles and illness biographies |
Abbreviations: COM-B, behavior guided by capability, opportunity, motivation; I-stories, multimedia story that is designed to help the listener or observer learn about the story teller’s journey with their health condition. It is typically a brief heartfelt and enthusiastic description of the following: their life before the condition, how their life has changed, what has made them feel most empowered, what their goals are, and what they’re looking forward to now.
Diabetes Health Coaching Intervention
The H360x application is accessible at www.health360.com or https://www.ehealthystrides.org. It consists of an integrated diabetes curriculum and pages for uploading and viewing self-monitored graphic and color-coded displays for parameters such as blood pressure, body mass index, number of steps walked, and blood glucose (11,23-26). The application also includes a structured instrument used by the patient to identify and set self-management goals based on the AADE7. (18) In consultation with the health coach, steps required to attain and track these goals are regularly monitored by the patient and shared with the health coach during monthly scheduled calls. The discussion forum was accessible from the H360x sign-on page for conversations among participants from each practice and their health coach and physician. All access was password-protected. Data entered through the H360x application was stored on the Microsoft HealthVault and all participants in the study received free Microsoft HealthVault accounts as part of the study. HealthVault (http://www.HealthVault.com) (27) interfaces with hundreds of medical and consumer devices including blood pressure, blood glucose, and physical activity monitors. H360x has an application programming interface with Microsoft HealthVault which allows H360x users to retrieve self-monitored data from their medical devices to the H360x application. H360x returns data that is color coded for decision support (Figure 2).
Fig. 2.
Health 360x features. Sample screen shots display color-coded systolic and diastolic blood pressure. Graph displays self-monitored blood pressure measurements over 3 months. This data can be shared with the clinician and/or health coach at the point of care.
Inclusion of Physician Champions, Health Coaches, and Participants With Diabetes From CPN Primary Care Practices
Independent physician practice members of the MSM CPN who had implemented EMRs were invited to join the study. Each practice identified a physician champion and a health coach; typically, the health coach is the practice’s medical assistant.
Computers with privacy screens were provided in a suitable location at each practice to facilitate use and access of H360x for self--monitoring by patients who did not have access to a home computer.
Inclusion of Champions, Health Coaches, and Study Participants With Diabetes From Big BBAME Church
The Senior Pastor and a Master Coach (who is also a member of the Health Ministry at BBAME) served as Champions and helped to generate church-wide engagement and commitment to join the research study as health coaches or study participants. BBAME members diagnosed with diabetes were eligible to join as study participants. Members of the Health Ministry were eligible to join as coaches for the BBAME implementation. Computer kiosks with privacy screens were provided in a suitable location at BBAME to facilitate participants’ access and use of H360x for study participant self-monitoring and for health coaching sessions.
Recruitment of Study Participants With Diabetes
All diabetic patients in each practice were identified using the ICD-10 codes for diabetes mellitus (6). Letters of invitation were sent to all identified patients. Patients who called to opt out did not receive any further contact.
BBAME participants were approached by, or reached out directly to the health coaches. Included were participants with diagnosed diabetes who were older than 21 years and willing and able to use the internet for the duration of the study. Excluded were participants who were precluded from doing so by any insurmountable physical impairment.
Eligible participants were mailed a packet with study protocol and informed consent before attending a training and orientation day at MSM. Participants were enrolled at the training/enrollment day after they reviewed and signed the inform consent, which was approved by the MSM institutional review board.
Training of Physicians and Health Coaches
Health coach training was standardized for customized delivery at the CPN practice or BBAME community setting. CPN physicians and health coaches were trained together, and BBAME Health Ministry coaches were trained together. All the training was conducted at the MSM computer laboratory.
Health coaches and physicians were oriented to the study processes and the H360x web application and discussion forum. The health coaches were trained and certified using a program designed by the AADE for staff at the point of care of diabetes. Additional training was provided for the coaches on the use of the structured goal setting and counseling tool, and technical training for web access to assist study participants. Each coach was provided with a laptop computer for the duration of the study.
Training of Study Participants From CPN Practices and BBAME
The participant orientation was a 4- to 5-hour hands-on activity that took place in the computer laboratory on the main campus of MSM. Training was conducted by co-authors (P.I.P. and F.O.) and by health coaches from each practice and BBAME. Once enrolled, all participants (with or without assistance) created email accounts, usernames, and passwords specific to the H360x application. They were guided through the access and use of H360x including how to create updated medication lists; how to access their personal H360x webpage from home; how to use their monitors, such as sphygmomanometer, glucometers, and pedometers to record and upload information to the HealthVault database; and how to view the data. They were oriented to the curriculum and associated quizzes, use of the discussion forum, and how to keep the usernames and passwords safe. All participants completed surveys at enrollment to determine their readiness for behavior change (see section on gap analysis above). At the end of the orientation visit, each participant was provided with a sphygmomanometer, glucometer, and pedometer, all of which were universal serial bus–port enabled to directly interface with e-HealthyStrides and upload all monitored data onto each participant’s HealthVault account. Participants were encouraged to access H360x as often as they could. Incentives were provided for completion of quizzes at the end of each chapter of the curriculum. Participants were encouraged to upload their data at least once a week for those with home access to a computer and once every 3 weeks for those who needed to go to the physicians’ office or BBMAME to upload data. All participants were required to set a self-management behavioral goal at baseline, using the structured goal-setting tool.
Health Coaching Sessions
Each health coach had 15 to 20 study participants and conducted structured coaching sessions over 12 weeks: each participant met with their respective health coach once each week for the first 2 months, then every other week for the final month of coaching. Structured coaching sessions concluded at 12 weeks. Participants were encouraged to continue to log onto the website and join informal peer support groups.
Project staff conducted virtual individual or peer group coaching sessions as needed to provide support after completion of structured sessions. Final study data collection was completed at 52 weeks.
Blood pressure, fasting blood glucose, and physical activity data were collected at baseline, after the 12-week intervention, and at 52 weeks.
Focus Group Sessions
We conducted focus groups to explore participants’ perspectives on the program. A qualitative descriptive design used semistructured focus group and conference call discussions among study participants. All tape-recorded discussions were transcribed verbatim and read line-by-line to extract meaningful codes and categories using NVivo 10 software (QSR International, Melbourne, Australia) (2) through a thematic analysis approach. Categories were then clustered into meaningful themes and references for awareness, access, empowerment, and engagement (22).
Statistical Analysis
We conducted univariate descriptive analyses. Quantitative variables are summarized using the means and standard deviations or medians where appropriate, whereas categorical variables are summarized using percentages. Differences between pre- and post-training/-intervention assessments for quantitative variables are examined using the paired Student t test or Wilcoxon signed-rank test, and McNemar chi-square test for categorical variables. The statistical test is two-sided and the level of significance is set at P ≤ 0.05.
RESULTS
Participant Characteristics
Two hundred eighty-seven participants completed 12 months (52 weeks) of follow-up. Ninety-seven percent of study participants are black or African American; the average age was 62.1 ± 13.81 years; 44% were ≥65 years old; 70% were female. Mean body mass index was 33.76 ± 8.13 kg/m2; 64% were obese; and 30% were overweight.
Duration of diabetes for 19.8% of participants was less than 2 years, for 14% it was 2 to 5 years, and for 66% it was more than 5 years from the diagnosis.
Clinical Outcomes of H360x Technology-Assisted Coaching Intervention
Overall systolic blood pressure, fasting blood glucose, and daily physical activity improved from baseline to 12 weeks. Systolic blood pressure at baseline was 134 mm Hg versus 128 mm Hg after 12 weeks of technology-assisted coaching intervention (P < 0.01). Similarly, blood glucose showed significant improvement from baseline: 137 mg/dl versus 122 mg/dl, P < 0.001; as did physical activity: 1.4 miles/day versus 1.96 miles/day, P < 0.001.
Per protocol, structured coaching was discontinued after 12 weeks. Systolic blood pressure, fasting blood glucose, and physical activity data remained optimized at 52 weeks and statistically improved compared to baseline: 130 mm Hg, 112 mg/dl, and 2.05 miles, respectively (P < 0.01)
Site-Specific Clinical Outcomes at 12 and 52 Weeks
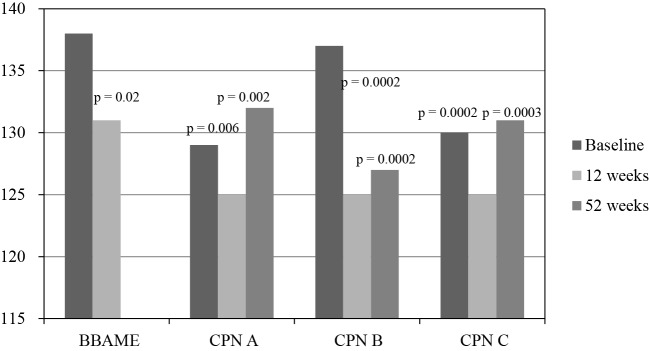
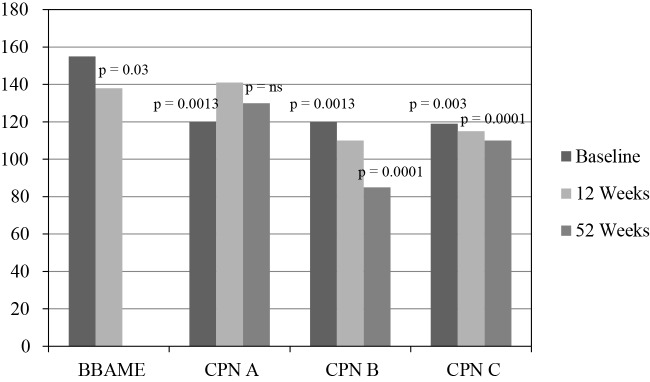
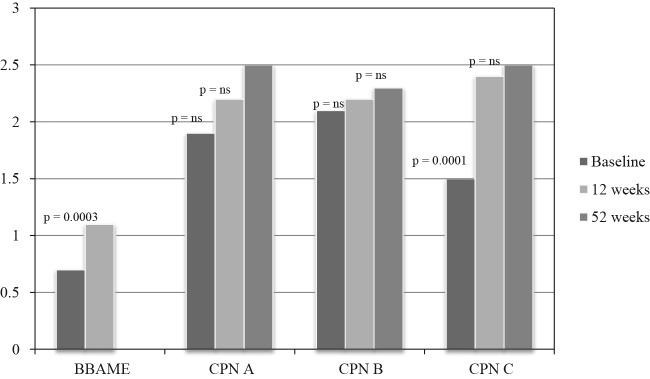
CPN practices and BBAME showed significant improvement in systolic blood pressure, fasting blood glucose, and physical activity at 12 weeks (Figures 3, 4, and 5) Fifty-two–week data was only available for CPN practices. There was variable systolic blood pressure response at 52 weeks; however, blood pressure remained in normal range for clinic sites that tracked the data.
Fig. 3.
Systolic blood pressure (mm Hg) at baseline, and after 12 weeks of intervention. Data at 52 weeks show long-term follow-up without interval health coaching.
P values vs. baseline.
Abbreviations: BBAME, Big Bethel AME Church; CPN, Community Physicians Network; CPN A, Practice A; CPN B, Practice B; CPN C, Practice C.
Fig. 4.
Fasting blood glucose (mg/dl) at baseline, and after 12 weeks of intervention. Data at 52 weeks show long-term follow-up without interval health coaching.
P value vs. baseline.
Abbreviations: BBAME, Big Bethel AME Church; CPN, Community Physicians Network; CPN A, Practice A; CPN B, Practice B; CPN C, Practice C; ns, not significant.
Fig. 5.
Physical activity (miles/day walked) at baseline, and after 12 weeks of intervention. Data at 52 weeks show long-term follow-up without interval health coaching.
P value vs. baseline.
Abbreviations: BBAME, Big Bethel AME Church; CPN, Community Physicians Network; CPN A, Practice A; CPN B, Practice B;CPN C, Practice C; ns, not significant.
Focus Group Results and References for Behavior Change
Using Word Cloud Analysis, two main themes and four categories were strongly associated with behavior change. The theme of Empowerment showed strong reference for Awareness and Access to curriculum, whereas the theme of Engagement with other diabetics and with health coaches also showed strong references.
Barriers to Engagement and Use of H360x Technology
Engagement with H360x was measured by usage minutes online when working with the H360x mobile or website. Based on usage, less than 25th percentile versus greater than 25th percentile, the following variables were not a barrier to usage: age (30 to 49 years vs. 50 to 64 years vs. >65 years) (P = 0.64); race/ethnicity (P = 0.96) (Table 2); self-rated ability to use a computer (P = 0.92); and ability to see clearly (P = 0.85) (Table 3). Participants’ anxiety about use of the internet (P < 0.01) and discomfort with putting health information on the internet (P < 0.006) significantly reduced engagement and use of the technology to self-monitor and manage health (Table 4).
TABLE 2.
Age and Race/Ethnicity as Potential Barriers to Use
| Age (Years) × Usage (Minutes Online) (n = 138) | |||
| Age, years | <25th percentile (%) | 25+percentile (%) | Total (%) |
| 30 to 49 | 8 (5.8) | 18 (13.0) | 26 (19) |
| 50 to 64 | 20 (14.5) | 60 (43.5) | 80 (57.9) |
| 65+ | 8 (5.8) | 24 (17.4) | 32 (23.2) |
| P = 0.64 | |||
| Race/Ethnicity × Usage (n = 138) | |||
| Black | 35 (25.4) | 99 (71.7) | 134 (97) |
| Other | 1 (0.72) | 3 (2.17) | 4 (2.9) |
| P = 0.96 | |||
TABLE 3.
Self-Rated Ability and Ability to See Clearly as Potential Barriers to Use
| Self-Rated Ability to Use the Computer × Usage (Minutes Online) (n = 131) | |||
| Score | <25th percentile (%) | 25+percentile (%) | Total (%) |
| Unable 0,1,2 | 7 (5.3) | 21 (15.9) | 28 (21.2) |
| Able 3,4,5 | 25 (18.9) | 79 (59.9) | 104 (78.8) |
| P = 0.92 | |||
| Ability to See Clearly × Usage (n = 135) | |||
| Agree/strongly agree | 30 (23.6) | 80 (63) | 110 (86.6) |
| Disagree/strongly Disagree/neutral | 5 (5.9) | 12 (9.5) | 17 (13.4) |
| P = 0.85 | |||
TABLE 4.
Internet Ability Anxiety and Internet Comfort as Barriers to Use
| I Feel Anxious about my Ability to Use the Internet × Usage (minutes online) (n = 133) | |||
| <25th percentile (%) | 25+percentile (%) | Total (%) | |
| No | 17 (12.8) | 72 (54.1) | 89 (66.9) |
| Yes | 17 (12.8) | 27 (20.3) | 44 (33.1) |
| P = 0.015 | |||
| I Feel Comfortable About Putting My Health Information on the Internet × Usage (n = 134) | |||
| Agree/strongly agree | 26 (19.7) | 46 (63) | 72 (54.6) |
| Disagree/strongly Disagree/neutral | 9 (6.8) | 51 (38.6) | 60 (45.5) |
| P = 0.006 | |||
DISCUSSION
The following findings from our study have clinical relevance and applicability for medicine:
Our study participants identified awareness of and access to a structured, evidence-based curriculum as key references for empowerment in self-management of diabetes.
Engagement with other diabetics and health coaches were also highly referenced by study participants.
H360x technology-assisted coaching with embedded curriculum and social network features supports behavior change and clinically relevant outcomes in patients with diabetes. Empowerment and engagement are references to the COM-B behavior change framework.
Although study participants had low average baseline DKT scores and less than 25% acknowledged use of the internet to manage their health, structured health coaching with the H360x mobile application and online peer support empowered and engaged participants to self-monitor and act on the data to manage their diabetes.
H360x technology-assisted health coach training was effective in community primary care practice setting, as well as a community church setting.
Statistically significant clinical outcomes for blood pressure, blood glucose, and physical activity were evident at 12 weeks.
The 52-week data showed improvement in blood pressure, blood glucose, and physical activity even after the structured coaching was discontinued at 12 weeks.
We identified significant barriers to use of H360x mobile technology for DSM among study participants who were anxious about use of the internet and those who were not comfortable putting their health information on the internet.
Clinical Implications of This Study and Relevance to the National Academy of Medicine’s Vision Imperative on the Learning Health Care System
There is an abundance of mobile applications that help consumers track various health indices. There are also sensors and monitoring devices that support health. Most of these devices and applications generally target healthy and technology savvy individuals.
H360x focuses on individuals who are living with one or more chronic health conditions because they consume significant health care resources. In our study, even when African Americans have access to computers and other technologies, they are not using these resources to manage their health. To our knowledge, our study is unique because we integrate science and informatics with real-time access to knowledge by engaging and empowering patients with our technology-assisted health-coaching model.
African American patients, who were the majority of our study participants, are medically underserved and traditionally underrepresented in most clinical studies. Our study should serve as a model for future studies in underserved patient populations, especially with regard to the use of technology and health coaching intervention.
The COM-B behavior change theory framework is integrated into H360x design and functionality. As the technology evolves, we expect to improve future efforts with decision support including integration of artificial intelligence. This is an important differentiation for H360x because most consumer application designs are not grounded in behavior change theory.
Future development will integrate the care experience and patient-clinician interaction. Current development efforts with specific, measurable, achievable, realistic, and time-bound applications that interface with electronic health records Fast Healthcare Interoperability Resources is an important next step for the H360x ecosystem. The opportunity to scale and generalize the H360x user base and experience aligns with the National Academy of Medicine’s vision imperative of a learning health care system.
Study Limitations
The study was not randomized; it was a convenience sample, and each patient served as their own control for evaluating the health coaching intervention.
The study was launched with the web-based e-HealthyStrides application, which synchronized with many devices on the HealthVault platform, including blood pressure monitors, blood glucose monitors, and accelerometers; this enabled study participants to use the automated feature on the application to directly upload monitored data from the device monitors. This HealthVault functionality helped to minimize errors with data entry. However, practice-site physician co-investigators found it very time consuming to access the HealthVault during clinic visits. The physician co-investigator from Practice B painstakingly downloaded patient monitored data from HealthVault to inform clinical decision-making during clinic visits. We observed that this practice showed the most consistent and long-term improvement in clinical outcomes through 52 weeks. Clinical outcomes data at 52 weeks was not consistently available from BBAME due to technical challenges. The e-HealthyStrides application has since successfully migrated to the H360x mobile application on Android and iPhones for current and ongoing studies.
Future Directions
Mobile application technologies such as the H360x seeking to transform the health care system of the future must address the following:
Effectively “scale up” and consistently engage individuals with chronic health conditions.
Increase our understanding of mechanisms of behavior change.
Integrate patient-reported outcomes so that self-reporting is as efficient and precise as possible. For example, ecological momentary assessments, which are self-reports in real time, minimize recall bias, increase ecological validity, and allow for longitudinal analysis of the processes that influence behavior over time.
Data security and privacy.
Integrate with cloud-based and US Food and Drug Administration – cleared devices or physiologic sensors.
Address patient-clinician interactions by interfacing with electronic health records Fast Healthcare Interoperability Resources technology (28,29) and supporting enhanced security and interoperability with national standards for sharing data between EMRs and mobile applications (29).
Big data analytics, pattern recognition, and machine learning are additional future advances.
ACKNOWLEDGMENTS
Supported by Grants from Microsoft HealthVault Be Well fund; National Institutes of Health (NIH) — National Center for Research Resources (NCRR): 3U54RR026137-S3, 2R25RR017694-06A1, 5U54RR022814, and 5P20RR11104; National Institute on Minority Health and Health Disparities (NIMHD): U54MD008149, 8U54MD007588, and U54MD008173; National Center for Advancing Translational Science (NCATS): UL1TR000454; National Institute of General Medicine: U54GM119023. From the Community Physicians’ Network (CPN) physicians: Dr. Janet Bivens, Dr. Kingsley Agbeyegbe, and Dr. Patricia Glenn, and all CPN patients.
The authors thank Mr. Rondereo Sidney for help with manuscript preparation; Ms. Debra Teague for outreach to the Community Physicians Network; Ms. Pamela Cooper and Ms. Geannene Trevillion for outreach to Big Bethel AME Church; Big Bethel AME Church, Atlanta, Georgia, including Pastor Gregory Eason, Senior Pastor, and Mr. William Petty of the Health Ministry; our Health Coaches Mrs. Frankie Akins, Mrs. Alicia Oden, and Mr. William Davis; the staff and medical assistants from participating CPN practices; and the following physician champions: Janet Bivens, MD, Kingsley Agbeyegbe, MD, and Patricia Glenn, MD; as well as the faculty and staff of the Clinical Research Center at Morehouse School of Medicine.
Footnotes
Potential Conflicts of Interest: Dr. Ofili is the lead Inventor of the patented technology that supports Health 360x. She is also the Founder and Chief Scientific Officer of AccuHealth Technologies Inc., a Morehouse School of Medicine Technology Transfer Faculty Start Up.
Contributor Information
ELIZABETH O. OFILI, ATLANTA, GEORGIA.
PRISCILLA E. PEMU, ATLANTA, GEORGIA.
ALEXANDER QUARSHIE, ATLANTA, GEORGIA.
ERNEST ALEMA MENSAH, ATLANTA, GEORGIA.
LATRICE ROLLINS, ATLANTA, GEORGIA.
FOLAKE OJUTALAYO, ATLANTA, GEORGIA.
ATUARRA MCCASLIN, ATLANTA, GEORGIA.
BETHANY SAINT CLAIR, ATLANTA, GEORGIA.
DISCUSSION
Golden, Baltimore: Really important work! So, I’m a diabetologist, and we know that these kinds of technologies definitely support behavior change. One of the challenges that we’ve had with some of the mobile technology companies which have approached us with apps is that at least in the John’s Hopkins health system, we use Epic. And so then, when you try to collaborate with them to have this kind of technology integrate with the EMR, it is very difficult. They want to develop something similar themselves or they want to invite the company to work with them, but then they want one-third equity in the company. I’m trying to figure out how we can work with some of these very large EMR companies because I think it’s a bit of a hindrance that we can’t as clinicians get that information directly into Epic.
Ofili, Atlanta: This is very good question. There are some national efforts on electronic medical record (EMR) integration that should help. For example, the 21st Century’s Cures Act that was just approved by Congress will mandate EMR systems to provide an application programming interface so that mobile apps can interface with EMRs. The Fast Healthcare Interoperability Resources (FHIR) is also a technology that will support enhanced security and interoperability, with national standards, for sharing data between EMRs and Mobile “apps.”
REFERENCES
- 1.Chronic Conditions in America: Price and Prevalence. Available at: https://www.rand.org/blog/rand-review/2017/07/chronic-conditions-in-america-price-and-prevalence.html .
- 2.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:130389. doi: 10.5888/pcd11.130389. http://dx.doi.org/10.5888/pcd11.130389 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Satcher D, Okafor M, Nottingham J. Twenty-First Century Global Mental Health. Burlington, Massachusetts: Jones & Bartlett Learning; The social determinants of mental health. In: Sorel E editor. 2012 71–91. [Google Scholar]
- 4.Best Care at Lower Cost-The Path to Continuously Learning Health Care in America. Institute of Medicine, National Academy of Medicine. Available at: www.iom.edu/bestcare . [PubMed]
- 5.Mensah GA, Cooper RS, Siega-Riz AM, et al. Reducing cardiovascular disparities through community-engaged implementation research: a National Heart, Lung, and Blood Institute workshop report. Circ Res. 2018;122 doi: 10.1161/CIRCRESAHA.117.312243. 213-10.1161/CIRCRESAHA.117.312243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Internetlivestats.com. PewResearch Center. Available at: pewinternet.org.
- 7.AccuHealth – Helping to Manage Chronic Illness. Available at: StockNewsNow.com. Accessed: July 2, 2014.
- 8.SNNLive spoke with Elizabeth Ofili, M.D. CSO of AccuHealth Technologies at SEMDA 2014 Annual Conference in Atlanta, GA. Published on May 27, 2014.
- 9.Award: Technology Association of Georgia Southeastern Software Association (SSA), Where Georgia Leads: Healthcare IT, and Emerging Megatrend. The finalists in the Where Georgia Leads: HealthIT — Accuhealth Technologies. [Google Scholar]
- 10.Ofili E, Pemu PI, Quarshie A, et al. United States Patent No: US 8,234,131 B2. Date of Patent: July 31, 2012. Filed: July 14, 2009. Prior Publication Data US 2010/0017229 Al on January 21, 2010. Provisional application No. 61/080,593 filed on July 14, 2008.
- 11.Pemu PE, Quarshie A, Ofili EO, et al. Socio-demographic psychosocial and clinical characteristics of participants in e-HealthyStrides©: an interactive ehealth program to improve diabetes self-management skills. J Health Care Poor Underserved. 2011;22((Suppl 4)):146–64. doi: 10.1353/hpu.2011.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) International Classification of Diseases (ICD) 10th revision, clinical modification ICD-10 CM. Geneva, Switzerland: WHO; 2011. Available at: http://www.who.int/classifications/icd/en/ [Google Scholar]
- 13.Anderson RM, Funnell MM, Fitzgerald JT, et al. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000;23((6)):739–43. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- 14.Anderson RM, Funnell MM, Butler PM, et al. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995;18((7)):943–9. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald JT, Funnell MM, Hess GE, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998;21((5)):706–10. doi: 10.2337/diacare.21.5.706. [DOI] [PubMed] [Google Scholar]
- 16.University of Michigan Health System. Diabetes research and training center: Michigan diabetes research training center materials for health professionals. Ann Arbor, Michigan: University of Michigan Health System; 2000. [Google Scholar]
- 17.Glasgow RE, Wagner EH, Schaefer J, et al. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43((5)):436–44. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 18.AADE. AADE7 self-care behaviors. Diabetes Educ. 2008;34((3)):445–9. doi: 10.1177/0145721708316625. [DOI] [PubMed] [Google Scholar]
- 19.Practice Based Research Network, Agency for Healthcare Quality and Research. Available at: https://www.ahrq.gov/topics/practice-based-research-network-pbrn.html .
- 20.Ofili E, Igho-Pemu P, Lapu-Bula R, et al. The Community Physicians Network (CPN): an academic community partnership to eliminate healthcare disparities. Ethn Dis. 2005;15((4 Suppl 5)) S5-124–7. [PubMed] [Google Scholar]
- 21.Igho-Pemu P, Quarshie A, Oduwole A, et al. Morehouse Community Physicians Network (CPN) hypertension registry: patterns of care and opportunities for targeted medical education. Ethn Dis. 2005;15((4 Suppl 5)):S5-120–3. [PubMed] [Google Scholar]
- 22.Michie S, van Stralen MM, West R. The behavior change wheel: a new method for characterizing and designing behavior change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.“Morehouse School of Medicine offers health coaching program for Diabetics.”. Available at: http://www.myfoxatlanta.com/video?clipId=8674166&autostart=true .
- 24.Atlanta Fox affiliate station (Fox 5 Atlanta) about the eHealtyStrides program and its expansion to the city of Atlanta. Available at: https://www.youtube.com/channel/UCjhAhn2BM_78tE74OPJliwg/feed . [Google Scholar]
- 25.Atlanta Journal Atlanta Journal-Constitution. Available at: http://www.ajc.com/news/news/atlanta-workers-team-up-with-morehouse-medical-to-/nWq3Y/ [Google Scholar]
- 26.Pemu P. Health 360x: A Technology Application to Improve Self-Management Skills. Selected to Present during Health Literacy Month on Expanding Health Literacy in the Technology Age at the National Coordinating Center Quality Improvement Network supporting the Centers for Medicare and Medicaid Innovation’s healthcare quality improvement contract, Quality Improvement Organizations assisting providers in hospitals, nursing homes, home health, and primary care settings to improve quality safety and lower long term health care costs. October 5, 2016.
- 27.Microsoft HealthVault. Available at: www.HealthVault.com . [Google Scholar]
- 28.Mandl KD, Mandel JC, Murphy SN, et al. The SMART Platform: early experience enabling substitutable applications for electronic health records. J Am Med Inform Assoc. 2012;19:597e603. doi: 10.1136/amiajnl-2011-000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mandel JC, Kreda DA, Mandl KD, Kohane IS, Ramoni RB. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc. 2016;0:1–10. doi: 10.1093/jamia/ocv189. [DOI] [PMC free article] [PubMed] [Google Scholar]