Summary
Hand burns are present in >60% of all burn cases and in fire mass casualty incidents even up to 100%. Most trauma and especially burns may be detrimental to the complex and delicate structures of the hand by direct injury, indirect BICS (Burn Induced Compartment Syndrome and interstitial high pressure) or by delayed or faulty treatment. BICS represents a special threat as the increasing swelling and oedema of the small diameter hand and forearm will exert pressure on the capillary/venous system, eventually ending in irreversible damage to the skin, nerves, muscle and vascular bed. Immediate release of constricting skin by incisional escharotomy and sometimes fasciotomy may arrest this vicious cycle: escharotomy is simple for experienced hand or burn surgeons, but they are not always present at the primary treatment site. The diagnosis of BICS is not simple either, as the direct measurement of interstitial/compartment pressure is rarely done. Burns caused by hot rollers such as industrial linen ironing machines are especially traumatic as besides the “simple” thermal burn, the hot rollers exert immense crushing pressure to the hand caught between the rollers. Over the last few years, several publications have described the role of a newly approved Bromelain derived enzymatic debriding agent (NexoBrid) for burns in general and hand burns in particular, and its ability to resolve or prevent BICS. We present a rare severe thermal/crush hand injury case where we were able to successfully treat the patient with NexoBrid enzymatic debridement-escharotomy.
Keywords: hand burns, crush burns, enzymatic debridement, thermal-crush injuries
Abstract
Une atteinte des mains est observée dans plus de 60% des brûlures, et dans quasiment tous les cas de catastrophes. La plupart des traumaitismes, en particulier les brûlures, peuvent être délétères pour les structures complexes et délicates de la main. Ceci peut être dû à la brûlure elle même, à un syndrome compartimental (SC), à un traitement tardif ou mal conduit. Le SC est particulièrement dangereux dans les espaces ténus de l’avant bras et de la main. L’augmentation de pression consécutive à l’oedème obère la microcirculation, entraînant au bout du compte des lésions cutanées, nerveuses, vasculaires et musculaires irréversibles. La libération immédiate des tissus ainsi comprimés par incision de décharge cutanée voire aponévrotomie peut interrompre le cercle vicieux. Il s’agit d’un geste simple pour des chirurgiens spécialisés, malheureusement pas toujours disponibles sur le site du traitement initial. Le diagnostic de SC n’est pas toujours aisé si la mesure directe des pressions tissulaires n’est pas réalisée. Les brûlures dues à des rouleaux chauffés comme ceux des presses à repasser industrielles car, outre le dégagement de chaleur, les rouleaux exercent une pression intense sur la main coincée entre eux. Depuis quelques années, plusieurs articles on décrit le rôle d’un nouvel agent de débridement enzymatique à base de bromélaïne (Nexobrid) pour le traitement des brûlures dont celles des mains ainsi que ses capacité à prévenir et traiter les SC. Nous présentons ici un cas de main de presse avec utilisation, couronnée de succès, de Nexobrid
Introduction
Burns on the hand are common as the hand is used in activities that expose it to trauma, and it is also used, automatically, to protect the face in any accident. In some series, hand burns are present in >60% of all burn cases, and in fire mass casualty incidents even up to 100%. The hand, with its functional and cosmetic importance and the complexity of important structures such as nerves, blood vessels, tendons, muscles and numerous delicate joints all tightly packed in a crowded space, is an evolutionary wonder. Most trauma and especially burns may be detrimental to these delicate structures by direct injury, indirect BICS (Burn Induced Compartment Syndrome and interstitial high pressure) or by delayed or faulty treatment. Thus, care of the injured and burned hand is often given by specialized, highly trained professionals who are rarely present in the initial admission process.
BICS represents a special threat as the increasing swelling and oedema of the small diameter hand and forearm will exert pressure on the capillary/venous system increasing extravasation and pressure on the surroundings, including deeper structures, as well as stretching the already traumatized skin, occluding more capillary and venous components while the arteries continue to pump blood in. Thus, the swelling and pressure continue to increase, eventually ending in irreversible damage to the skin, nerves, muscle and vascular bed. Immediate release of the constricting skin by incisional escharotomy and sometimes fasciotomy may arrest this vicious cycle if executed early enough, within hours, before the damage is irreversible. Escharotomy is simple for experienced, skilled hands or burn surgeons, but they are not always present at the primary treatment site, and escharotomy in unskilled hands may be more destructive than curative. The diagnosis of BICS is not simple either, as the direct measurement of interstitial/compartment pressure is rarely done and the clinical signs of the 5 “Ps” (Pallor, Paresthesia, Pain on extension, reduced Pulse and Paralysis) as well as reduction of laser Doppler, ultrasound and pulse oximetry signs appear rather late when much of the damage is already done.1-3 Burns caused by hot rollers such as industrial linen ironing machines are especially traumatic as besides the “simple” thermal burn, the hot rollers exert immense crushing pressure as well as shearing forces that cause crushing injuries and shearing/degloving/avulsion injuries to the hand caught between the rollers. Such crush-burns are considered a formidable challenge to any hand or burn surgeon, even more so than “simple” hand burns with or without BICS.4-6
In the last few years, several publications have described the role of a newly approved Bromelain derived enzymatic debriding agent (NexoBrid) for burns in general and hand burns in particular, and its ability to resolve or prevent BICS.7-11 In our burn centre we have had previous experience with this enzymatic debridement agent where we witnessed its efficacy in removing burn eschars of varying thickness, without causing harm to unburned tissues. We present a rare severe thermal/crush hand injury case where we were able to successfully treat the patient with NexoBrid enzymatic debridement-escharotomy.
Case report
A 36-year-old woman was transferred to our regional burn centre after suffering an industrial injury. Her right hand was caught between hot industrial ironing rollers, one of them heated to 160°C. The rollers pulled on the hand until the midforearm was wedged between them. Emergency services took several minutes to free her hand, then they transported her to a local emergency department where she received initial treatment including analgesia (IV Fentanyl 0.1 mg/2ml and PO Paracetamol 1g.) and the burns were cleaned with chlorhexidine solution. An X-ray showed avulsion of the ulna’s styloid process and fractures of the distal radius epiphysis. The right forearm and hand were dressed with chlorhexidine solution and the patient was transferred to our regional burn centre, arriving two and a half hours post injury. On arrival the hand was grossly swollen, the skin was hard and tight with the fingers in a claw position and with clinically assessed full thickness burns on the palmar side of the hand and forearm. The fingers were insensate and the patient could not move the hand or any of the fingers. The ulnar pulse was not palpable and the radial pulse barely palpable (Fig. 1). Due to the condition described above, and our previous experience with NexoBrid, we chose to use rapid enzymatic debridement/escharotomy in this case. Six hours post injury and less than an hour post admission to our centre, after administration of IV Ketoprofen 100 mg, Nexo-Brid® was applied. During the 4-hour treatment the patient was closely monitored. Two hours after treatment she reported a tingling sensation in her fingers and she could start to move the fingers and hand. After the removal of NexoBrid (4 hours post application) the burns were judged to be completely debrided down to the subcutaneous palmar fat of the hand and muscle fascia on the forearm with preservation of viable dermis on the fingers and palmar creases. A substantial decrease of the swelling was seen, with complete return of normal ulnar and radial pulses (Fig. 2). The patient could move her hand and fingers, and reported return of sensation. Local treatment was continued with chlorhexidine soakings for the next 4 days (Fig. 3). On post injury day 5 the patient was operated on under general anaesthesia, all burns were refreshed by scraping and split thickness autografts harvested from the right thigh were applied on all full thickness defects, and Aquacel®Ag was applied on the areas of exposed dermis (Fig. 4). A transient thrombocytopenia of 60,000-80,000 platelets was seen after surgery (on days 6-8 post-injury), with normalization of the platelet count afterwards. We believe this may have been the result of the surgical intervention on day 5 leading to transient procedural bacteraemia and influx of catabolites and debris from the injured extremity. On the eighth day post injury a Doppler of the extremities revealed no vein thrombosis of the right forearm. On the contralateral uninjured upper extremity, superficial vein thrombosis of the left forearm was seen.
Fig. 1A. Palmar side of right hand with deep swollen and tight crushed and burned soft tissues. The paresthetic fingers are in typical flexion contraction.

Fig. 1B. The dorsal skin harmed only by the non heated roller is only abraded and swollen.
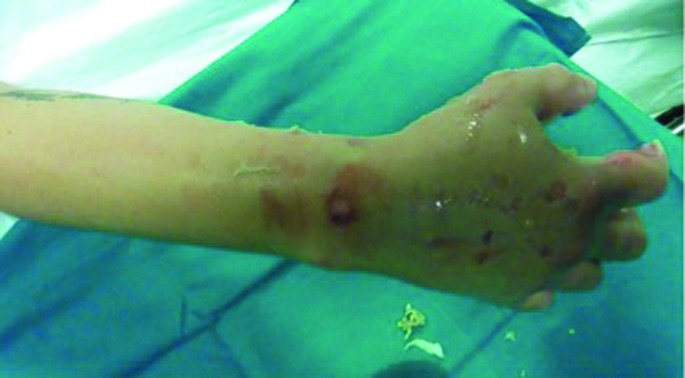
Fig. 2A. Application of NexoBrid gel.

Fig. 2B. The hand 4 hours after Nexobrid application: the dissolved eschar was wiped away revealing the clean, bleeding bed showing subcutaneous fat, fascia and dermis.

Fig. 3. Exposed tissues following 4 days of soaking.

Fig. 4. Thin split thickness applied over the full thickness defects.

Twelve days post injury, minor graft separation over some areas of exposed fascia appeared (Fig. 5). At day 15, negative pressure wound therapy was applied for 10 days to create a vascular bed over the exposed fascia. The pain at the forearm was controlled at day 19 post injury by an axillary regional block. On day 29, the open areas were closed by autografting. Throughout the entire period and during the following weeks the patient underwent occupational and physical therapy. At present, 6 months post injury, the hand is functional with a linear scar. The scar quality as assessed by MVSS (Modified Vancouver Scar Scale) was 7/18 (the linear scar over the grafted tendon was assessed as 4, severely affecting the final result that otherwise would have been 3/18). The POSAS (Patient & Observer Scar Assessment Scale) patient’s assessment was 28/60 and the observer’s was 31/60 with general assessment of both being the same, 5/10 (Fig. 6). The patient performed physical therapy, restoring nearly full upper extremity function for the entire period of six months before returning recently to her country of origin (Romania).
Fig. 5. Seven days post grafting (12 days post injury) with sloughing of the graft, especially over tendons and fascia.
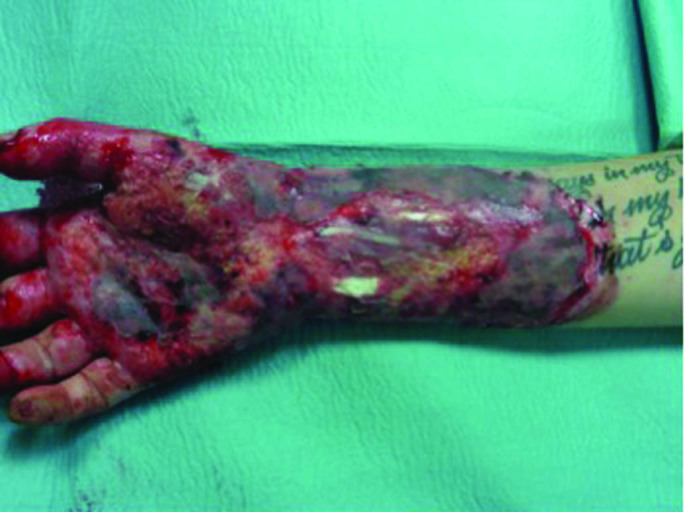
Fig. 6A. Six months post injury the wounds are completely healed with good scarring; B) a fibrotic band where the thin autograft adheres to the flexor tendon can be seen.
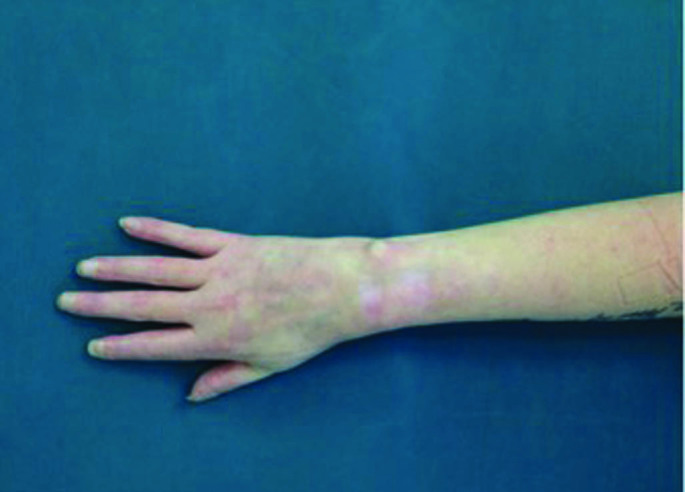
Fig. 6B. A fibrotic band where the thin autograft adheres to the flexor tendon can be seen.

Discussion
Though relatively rare, crush burns are an entity encountered by most burn centres, especially in industrial areas. Crush burns combined with degloving injury are the worst-case scenario, especially in anatomical areas such as extremities. Crushing and shearing forces and mounting interstitial and compartment pressures add another dimension to the deep thermal burn-related pathophysiology. The findings of the fractured styloid process and radial epiphysis on admission in this case reflect the severity of the crushing forces that shattered bones. The immense crushing and heat, aside from extending the thermal damage,4 contributed to the massive extravasation and swelling resulting not only in BICS but also in direct injury to the muscles. The first treatment of cleaning the injured hand and then infusing a litre of crystalloids solution may even have added to the swelling process and BICS during the hours until enzymatic escharotomy was performed. As we did not measure interstitial and compartment pressure before and after treatment, relying like most centres on clinical evaluation, we consider the clinical findings following the rapid and effective eschar dissolution sufficient. The patient’s report of a return of sensation and motion within the treatment period itself is a measure of the speed and efficacy of BICS resolution. We speculate that had this treatment been executed sooner after injury, the results could have been even better. All the 5 Ps were present before treatment and none after it, thus enzymatic debridement can also be considered as an effective means to resolving BICS, and may be termed “enzymatic escharotomy” corroborating previous human and animal studies.7-11 Considering the severe crush injury and bone fractures, deeper damage to muscles, like in cases of explosion/blast injuries, should be expected, and because enzymatic debridement dissolves only thermally denatured tissues, it is not expected to have an effect on the subfascial mechanically damaged structures. The fact the patient underwent an uneventful continuous monitoring during and after debridement gave a measure of safety, but we wonder whether the intractable pain that necessitated an axillary block was not only due to the fractures and physical therapy but also to a certain degree of muscular damage/ischemia. Due to the roller’s shearing forces, the skin avulsion/degloving typically reached the fascial plan. However, it does not seem to add much to the severity of the trauma as it involved the already thermally injured tissues that were entirely debrided enzymatically (Fig. 3). The presence of this denuded fascia and flexor tendon also explains the areas where the autografts did not take and required regrafting later. Autografting of such hostile wound beds can be facilitated by initial use of biological covers such as cryo-preserved allografts or xenografts to be replaced after several days by autografts or by negative pressure wound therapy that “prepares” the recipient bed.
Conclusion
This is the first report of a thermal-crush-avulsion hand injury successfully treated by enzymatic debridement.
Our lessons learned from this case are:
The importance of very early effective treatment of combined thermal and crush injuries such as the one presented here should be stressed, especially to emergency department personnel.
Rapid enzymatic debridement with NexoBrid in severe thermal-crush injuries can be a first line therapy in emergency departments to be applied as early as possible after admission. Such an immediate preventive/curative enzymatic debridement/ escharotomy can alleviate the weight of diagnosis and decision for surgical escharotomy (as not all emergency department personnel are skilled in surgical escharotomy, especially in cases such as this), thus allowing a safe course of treatment or transfer to another, specialized centre. We recommend continuous monitoring of the patient, especially the condition of the extremity, and readiness to intervene if adverse events happen.
In the case of suspected deeper, subfascia injury it is important to measure and monitor subfascial pressure to ensure that a fasciotomy is not needed.
References
- 1.Saffle J. Practice guidelines for burn care, Preface and Acknowledgements. BCR, 2001. 2001;i-xii and 1S:69S. [Google Scholar]
- 2.Orgill DP, Piccolo N. Escharotomy and decompressive therapies in burns. J Burn Care Res. 2009;30(5):759–768. doi: 10.1097/BCR.0b013e3181b47cd3. [DOI] [PubMed] [Google Scholar]
- 3.Smith MA, Munster AM, Spence RJ. Burns of the hand and upper limb - a review. Burns. 1998;24(6):493–505. doi: 10.1016/s0305-4179(98)00063-1. [DOI] [PubMed] [Google Scholar]
- 4.Sagi A. Combined thermal and crush injury to the hand and fingers. Burns. 1997;23(2):176–181. doi: 10.1016/s0305-4179(96)00116-7. [DOI] [PubMed] [Google Scholar]
- 5.Wang X-W. Thermal-crush injuries of the hands and forearms: an analysis of 60 cases. Burns. 1985;11:264–268. doi: 10.1016/0305-4179(85)90121-4. [DOI] [PubMed] [Google Scholar]
- 6.Sever C. Thermal crush injury of the hand caused by roller type ironing press machine. Acta Orthop Traumatol Turc. 2010;44(6):496–499. doi: 10.3944/AOTT.2010.2350. [DOI] [PubMed] [Google Scholar]
- 7.Krieger Y. Escharotomy using an enzymatic debridement agent for treating experimental burn-induced compartment syndrome in an animal model. J Trauma. 2005;58(6):1259–1264. doi: 10.1097/01.ta.0000169867.08607.f1. [DOI] [PubMed] [Google Scholar]
- 8.Krieger Y. Efficacy of enzymatic debridement of deeply burned hands. Burns. 2012;38(1):108–112. doi: 10.1016/j.burns.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Rosenberg L. A novel rapid and selective enzymatic debridement agent for burn wound management: a multi-center RCT. Burns. 2014;40(3):466–474. doi: 10.1016/j.burns.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg L. Safety and efficacy of a proteolytic enzyme for enzymatic burn debridement: a preliminary report. Burns. 2004;30(8):843–850. doi: 10.1016/j.burns.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 11.Rosenberg L. Enzymatic debridement. Herndon D (ed): “Total Burn Care”, Chapter 11. 2012 [Google Scholar]


