Summary
Selective enzymatic debridement is increasingly being used in cases of burn wounds. However, until now the use of Nexobrid has been limited to 15% of total body surface area (TBSA) and immediate use on admission day. A 61-year-old Caucasian male suffered a severe burn injury that affected 95% TBSA. After surgical escharotomy and tracheotomy on admission day, we successfully performed a fractional enzymatic debridement of 54% of the TBSA in three different sessions within four days. This case report reveals that a delayed and fractional application of Nexobrid to more than 15% TBSA is possible
Keywords: enzymatic debridement, Nexobrid, case report, extensive burn injury
Abstract
Le débridement enzymatique sélectif des brûlures est de plus en plus utilisé. Cependant, cette technique était jusqu’ici limitée à 15% de la surface corporelle totale (SCT). Nous rapportons le cas d’un homme de 61 ans brûlé sur 95% SCT. Après une trachéotomie et des incisions de décharge le jour de son entrée, nous avons réalisé un débridement enzymatique sur 54% SCT sur 4 j en 3 séances. Cette observation montre que l’utilisation séquentielle de Nexobrid® permet de traiter plus de 15% SCT.
Introduction
Burn injuries are common and constitute a severe trauma to the affected organism. Until today, early debridement of burned tissue and wound closure with autologous skin in the form of split thickness skin graft has been the standard care in deep partial and full thickness burns, as it decreases inflammatory complications and scarring and reduces the chance of death. In most cases, debridement refers to the surgical excision of burned tissue. Depending on the depth of the burn, a tangential or fascial excision of necrotic tissue is performed until there is a well-vascularized viable wound bed suitable as a recipient site for skin grafting.1,5
The invasiveness of surgical debridement and skin grafting is one of the most relevant disadvantages, and results in loss of blood and body heat during the operation. In particular, for patients who are not in a stable cardiopulmonary condition, this can pose a severe threat or be the reason for a delay in surgery. 6,7
Rapid enzymatic debridement as a less invasive and more selective form of eliminating necrotic tissue has become more popular in burn care over the last few years, as NexoBrid, a debriding agent based on the proteolytic enzyme “bromelain” and derived from pineapple plant stems, has shown good and reproducible results. Although full thickness defects still require skin grafting, there is another advantage of using selective enzymatic debridement. In partial thickness burns, there are usually enough dermal remnants to allow spontaneous healing of the wound without the need for autografting, thus resulting in less surgery and donor site scarring. These are some of the main reasons why NexoBrid™ has become a renowned alternative to surgical debridement.7,8
Case presentation
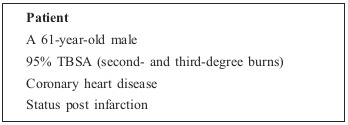
A 61-year-old Caucasian male was presented at our burn centre with second- to third-degree burns that affected 95% TBSA with inhalation trauma. He had been involved in a gas explosion at home. The known comorbidities were coronary heart disease with status post infarction and nicotine abuse. Abbreviated Burn Severity Index (ABSI) score for the patient was 17.
Upon admission and after cleaning the fresh burn and removing blisters, an escharotomy and a tracheotomy were performed. Owing to acute respiratory and cardiac failure, surgical debridement of eschars was not possible in the following few days.
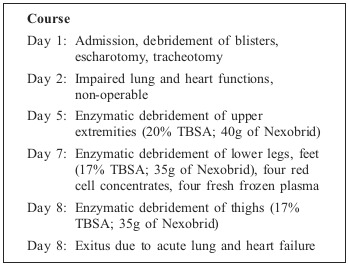
Thus, we decided to start an off-label enzymatic debridement at the bedside in the intensive care unit. Over the next few days, we performed a fractional use of enzymatic debridement with Nexobrid (Mediwound Ltd, Yavne, Israel) on 54% TBSA. On the fifth day, we performed an enzymatic debridement of the patient’s upper limbs (20% TBSA, Fig. 1); this was performed again on the seventh day on the lower legs and feet (17% TBSA, Fig. 2); and finally, the same was performed on the eighth day on the upper legs (17% TBSA, Fig. 3). After enzymatic debridement, viable dermis with small punctual bleedings or viable adipose tissue appeared and demonstrated a successful debridement of eschars.
Fig. 1.
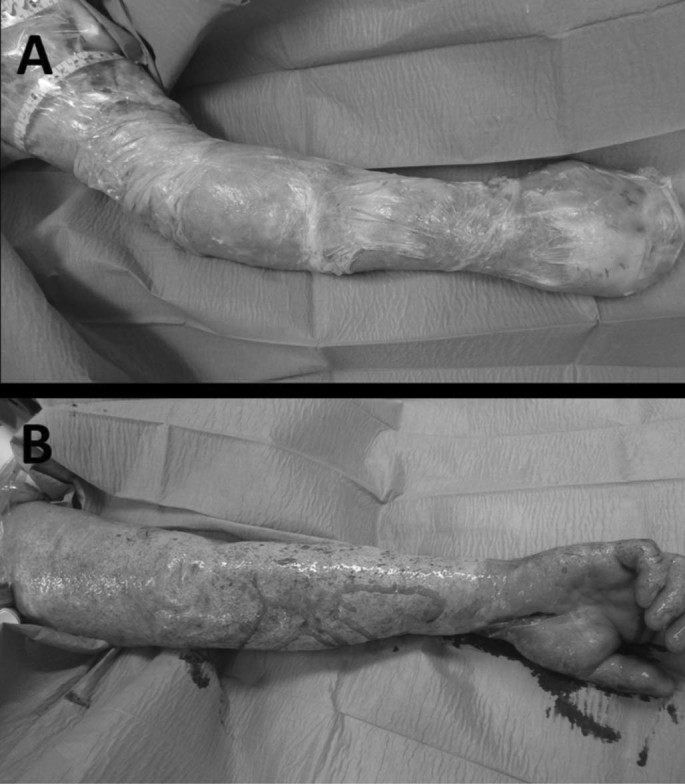
Fig. 2.

Fig. 3.

Despite successful enzymatic debridement, the patient died on the eighth day due to acute lung and heart failure.
Conclusion
Enzymatic debridement with Nexobrid is licensed for the removal of eschar in adults with deep partial- and full-thickness thermal burns. Until now, the use of Nexobrid has been limited to 15% TBSA and immediate use on admission day. In this case, we successfully performed a fractional use of enzymatic debridement with Nexobrid on 54% TBSA. In our literature review, we could find no case where such a large TBSA was treated with enzymatic debridement.
Except for bleeding during enzymatic debridement, no debridement-related side effects were noticed in the patient. As in surgical debridement, haemoglobin monitoring is necessary to avoid critical anaemia.
The Abbreviated Burn Severity Index (ABSI) score of our patient was 17 and the prognosis was infaust. Owing to the condition of our patient, no surgical intervention could be performed. Thus, on the fifth day we decided to use bedside enzymatic debridement as a last resort. Retrospectively, we could have considered using Nexobrid on admission day to avoid surgical escharotomy and accelerate the removal of necrosis.7,9
However, despite successful debridement of the burn wounds, wound coverage and lack of skin donor sites would have been challenging in this case.
This case report reveals that a delayed and fractional application of Nexobrid to more than 15% TBSA is possible.
Acknowledgments
Disclosures.Written informed consent was obtained from our patient for publication of this case report and any associated images. No conflict of financial or competing interests exist for this study.
Acknowledgements.We are grateful to our patient for giving his consent to the publication of this report.
References
- 1.Ong YS, Samuel M, Song C. Meta-analysis of early excision of burns. Burns. 2006;32(2):145–150. doi: 10.1016/j.burns.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 2.Aaronson SA. Growth factor-regulated pathways in epithelial cell proliferation. Am Rev Respir Dis. 1990;142(6 Pt 2):S7–S10. doi: 10.1164/ajrccm/142.6_Pt_2.S7. [DOI] [PubMed] [Google Scholar]
- 3.Orgill DP. Excision and skin grafting of thermal burns. N Engl J Med. 2009;360(9):983–901. doi: 10.1056/NEJMct0804451. [DOI] [PubMed] [Google Scholar]
- 4.Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10(12):1103–1108. [PubMed] [Google Scholar]
- 5.Burke JF, Bondoc CC, Quinby WC. Primary burn excision and immediate grafting: a method shortening illness. J Trauma. 1974;14(5):389–395. doi: 10.1097/00005373-197405000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Cartotto R. Minimizing blood loss in burn surgery. J Trauma. 2000;49(6):1034–1039. doi: 10.1097/00005373-200012000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg L. Minimally invasive burn care: a review of seven clinical studies of rapid and selective debridement using a bromelainbased debriding enzyme (Nexobrid). Ann Burns Fire Disasters. 2015;28(4):264–274. [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg L. A novel rapid and selective enzymatic debridement agent for burn wound management: a multi-center RCT. Burns. 2014;40(3):466–474. doi: 10.1016/j.burns.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Krieger Y. Escharotomy using an enzymatic debridement agent for treating experimental burn-induced compartment syndrome in an animal model. J Trauma. 2005;58(6):1259–1264. doi: 10.1097/01.ta.0000169867.08607.f1. [DOI] [PubMed] [Google Scholar]


