Abstract
Pulmonary artery intimal sarcoma (PAS) is a rare mesenchymal tumor mostly diagnosed in middle-aged women. In a 63-year-old female, the radiological findings showed cavitation in the left upper lobe of the lung and infiltrative tumor mass around the left pulmonary artery. PAS consisted of small, round tumor cells with about 80% of mitotic activity and with myxoid background and specific immunoprofile and diagnosed as undifferentiated sarcoma with round cell features type. The final diagnosis of PAS was established according to the pathohistological, chest computed tomography scan, and surgery finding.
Keywords: Artery thrombosis, pulmonary artery intimal sarcoma, pulmonary infarction, thromboembolism
INTRODUCTION
Pulmonary artery intimal sarcoma (PAS) is a rare mesenchymal tumor that originated from pulmonary artery intima, mostly diagnosed in middle-aged women. A characteristic symptom in patients with PAS is thromboembolism.[1] Pathohistological findings vary from spindle cell proliferation with focal osteosarcoma or chondrosarcoma differentiation to round cell tumor proliferation with myxoid background. According to the literature, the majority of these tumors express vimentin, CD31, and alpha- smooth muscle actin (alpha-SMA).[2]
We, herein, present a female patient with PAS which caused left pulmonary artery thrombosis accompanied with upper left lobe cavitation.
CASE REPORT
On admission, a 63-year-old woman a ppeared neglected. She was hospitalized at Clinic for Pulmonology of Clinical Center of Serbia in Belgrade, Republic of Serbia, in November 2016 to detect the origin of fatigue, cough, sweating, malaise, weight loss, and occasional hemoptysis in the past few months. Her findings showed increased reference values of sedimentation (90 mm/h), as well as increased level of white blood cells (15.9 × 109/l). The differential white cell count showed neutrophilia (83.59%) and lymphopenia (8.45%) and increased C-reactive protein values (127 mg/ml) as well as glucose serum level (29.6 mmol/l). Bronchoscopic findings with biopsy were inconclusive. Sixteen months after surgery, the patient's condition is stable with no recurrent episodes of hemoptysis and thromboembolism of the left pulmonary artery and its branches, and antidiabetic therapy effects were monitored with the purpose to start the suggested oncological therapy. Tumorous mass in the left upper lobe had a partial response on chemotherapy, but the patient could not go under surgery.
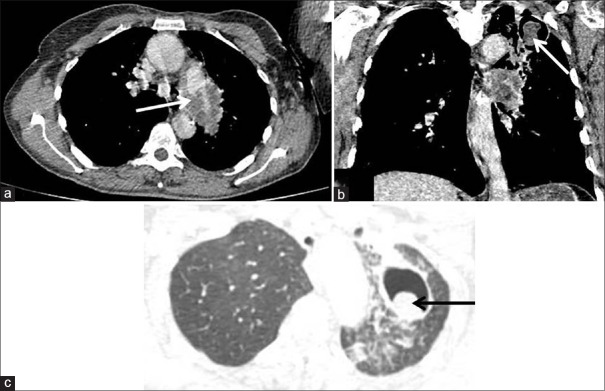
Radiography and multidector computed tomography
The chest radiograph showed cavitation in the left upper lobe of the lung, and therefore, the multidector computed tomography (MDCT) was indicated. The MDCT finding showed the existence of 55x17 mm (AP/LL) large infiltrative tumour mass around the left pulmonary artery with almost complete thrombosis of its left branch. There was another 37x15mm large soft tissue-like lesion in posterobasal area of the left hemithorax [Figure 1a]. In the anterior segment of the left upper lobe there was a 47x31 mm (AP/LL) cavitation found with a mass in the posterior wall [Figure 1b and c].
Figure 1.
Contrast-enhanced computed tomography findings: (a) axial computed tomography scan shows a large filling defect in the left pulmonary artery consistent with obliterative thrombosis (arrow) with extraluminal tumor extension. (b) Coronal and (c) apical axial computed tomography scan in the same patient revealed a soft-tissue mass with the cavity in the left upper lobe (arrows)
Intraoperative findings
Since the etiology of the cavitation of the left upper lobe was not determined by repeated bronchoscopy examinations, the diagnostic thoracotomy was indicated. The patient went under surgery at Clinic for Thoracic Surgery of Clinical Center of Serbia in Belgrade, Republic of Serbia, in November 2016. During the exploration of chest cavity for the purpose of preparation for radical surgery, the central tumor mass as well as tensed pulmonary artery which was filled with thrombotic masses was found, and therefore, it was concluded that the safe resection was not possible. Due to the central position of the tumor in the hilar region of the left lung and impossibility to safely manage the pulmonary artery without risk to patient's life, the decision was made to end the surgery. Biopsy of the tumor from the left hilar region was taken with the purpose of pathohistological examination and determination of the tumor etiology.
Pathohistology
The tumor mostly consisted of a population of small round cells with lack of pleomorphism in myxoid background. Zones of hyper- and hypocellularity zones were observed in the tumor [Figure 2a–c]. All tumor cells expressed vimentin [Figure 3a], and most of them expressed alpha-SMA [Figure 3b] and CD31 [Figure 3c]. Both hypo- and hypercellular zones were with high mitotic activity, of about 80% [Figure 3d]. Desmin, CD34, caldesmon, Fli-1, cytokeratin, S-100 protein, and mdm2 were not expressed. The tumor morphology and its immunophenotype led to a diagnosis of rare subtype of PAS which is known as “undifferentiated sarcoma with round cell features."
Figure 2.
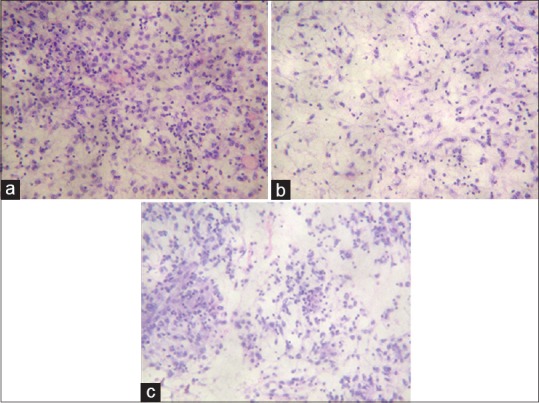
Various types of cellularity of pulmonary artery intimal sarcoma: (a) small, round tumor cells in cellular area of pulmonary artery intimal sarcoma (H and E, ×20); (b) the same cells in myxoid background of tumor with (H and E, ×20); (c) zone of pulmonary artery intimal sarcoma with mixed, hypo- and hypercellularity (H and E, ×20)
Figure 3.
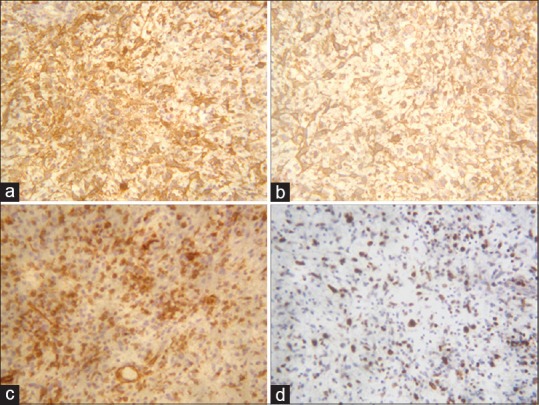
Immunohistochemistry confirmed diagnosis of pulmonary artery intimal sarcoma: (a) tumor cells expressed vimentin improving their mesenchymal origin, ×20; (b) alpha-smooth muscle actin was expressed in small, round tumor cells; (c) CD31 was expressed in tumor cells, ×20; (d) the high proliferative activity was detected by Ki-67, ×20
DISCUSSION
PAS is a rare mesenchymal tumor localized in the pulmonary artery with consequent thrombosis of its lumen with various morphological pattern, predominantly as spindle cell proliferation with or without osseous and chondromatous differentiation and characteristic immunophenotype.[1,2,3]
Our patient was diagnosed with thrombosis of left pulmonary artery and cavitation of the upper left lobe. Tumor node in the left hilar region was extirpated surgically for pathohistological diagnosis. The PAS was diagnosed on the extirpated sample. The 2015 WHO classification of the lung tumors defines this mesenchymal tumor as rare PAS subtype of “undifferentiated sarcoma with round cell features,” with characteristic immunoprofile vimentin+/CD31+/alpha-SMA+.[4] The most of PAS is spindle cell proliferation with focal osseous and chondromatous differentiation in 1/6 of these patients. All tumor cells express vimentin and the most of them alpha-SMA and CD31, but and in some cases also desmin, myogenin, and CD34.[5] According to Bode-Lesniewska et al., the most of PAS express mdm2, implicating that mdm2/p53 pathway may be involved in possible pathogenesis of this tumor.[6] However, in our case, mdm2 was not expressed in tumor cells of PAS.
Only a limited surgery was performed in our patient because of the risk to patient's life. Lee et al. observed that only 30% of their patients with PAS had complete resection. Only 55% (11/20) of them received postoperative treatment: Only 3 (15%) received chemotherapy, 5 (25%) received radiotherapy, and 3 (15%) received combined radiochemotherapy.[3]
The nature of the cavitation in the left upper lobe was not determined on biopsy. Authors’ opinion is that cavitation could be a result of previously developed rusty lung infarction as the consequence of thromboembolism or the tumorous infiltration but surrounded by tumor mass with partial response to chemotherapy.
CONCLUSION
Our patient was diagnosed with rare morphological subtype of PAS. The final diagnosis of PAS was established by multidisciplinary approach in correlation with clinicopathological, chest CT scan, and surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wong HH, Gounaris I, McCormack A, Berman M, Davidson D, Horan G, et al. Presentation and management of pulmonary artery sarcoma. Clin Sarcoma Res. 2015;5:3. doi: 10.1186/s13569-014-0019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kriz JP, Munfakh NA, King GS, Carden JO. Pulmonary artery intimal sarcoma: A case report. Case Rep Oncol. 2016;9:267–72. doi: 10.1159/000445498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee Y, Kim HJ, Yoon H, Choi CM, Oh YM, Lee SD, et al. Clinical characteristics and treatment outcomes of primary pulmonary artery sarcoma in Korea. J Korean Med Sci. 2016;31:1755–60. doi: 10.3346/jkms.2016.31.11.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Travis WD, Brambila E, Burke AP, Marx A, Nicholson AG, editors, editors. 4th ed. Lyon: IARC; 2015. WHO Classification of Tumours of Lung, Pleura, Thymus and Heart. [DOI] [PubMed] [Google Scholar]
- 5.Bandyopadhyay D, Panchabhai TS, Bajaj NS, Patil PD, Bunte MC. Primary pulmonary artery sarcoma: A close associate of pulmonary embolism-20-year observational analysis. J Thorac Dis. 2016;8:2592–601. doi: 10.21037/jtd.2016.08.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bode-Lesniewska B, Zhao J, Speel EJ, Biraima AM, Turina M, Komminoth P, et al. Gains of 12q13-14 and overexpression of mdm2 are frequent findings in intimal sarcomas of the pulmonary artery. Virchows Arch. 2001;438:57–65. doi: 10.1007/s004280000313. [DOI] [PubMed] [Google Scholar]