Abstract
Human papillomavirus (HPV) is the most common sexually transmitted virus in males and females worldwide; yet its impact upon male fertility remains unclear. The objective of this study was to evaluate the potential impact of HPV infection in semen on male fertility abnormality. A systematic literature search was performed in PubMed, Medline, Embase, Web of Science, and the Cochrane Library database for relevant publications up to May 6, 2017. The odds ratio (OR), and its corresponding 95% confidence interval (CI), was selected to represent the effect size. Statistical analysis was conducted using STATA 12.0. In total, eight articles, providing data on 1955 participants, were included in this meta-analysis. Collectively, the data suggested that HPV infection of semen was a risk factor for male fertility abnormality with an OR of 3.02 (95% CI: 2.11–4.32; I2 = 6.9%). Sensitivity analysis revealed that the results of this study were robust. In conclusion, HPV infection of semen represents a risk factor for male fertility abnormality.
Keywords: human papillomavirus, male infertility, meta-analysis, semen infection
INTRODUCTION
Infertility is a global problem, affecting approximately one-fifth of couples trying to conceive.1,2 Various factors may contribute to the infertility of males and females, including several types of microorganism, e.g., bacteria, fungi, viruses, and parasites.3 Human papillomavirus (HPV), one of the most prevalent sexually transmitted infections among humans,4 represents a well-established cause of cervical cancer in females. Besides the etiological role in cancer, the association between HPV infection in females and adverse pregnancy outcomes, such as spontaneous abortion and spontaneous preterm birth, has been extensively reported.5,6,7,8 However, the impact of HPV infection upon male fertility abnormality has received far less attention.
Previous studies have reported the detection of HPV DNA in semen/sperm cells and in different sites within the male reproductive tract, such as the penile shaft, glans penis, and scrotum.9,10,11,12 Earlier studies also showed that HPV DNA can be detected in the semen of 2%–31% of the general male population and in 10%–35% of men undergoing assisted reproductive technology (ART) for infertility.13,14 In 2014, Laprise et al.15 conducted a systematic review and meta-analysis to evaluate the prevalence of HPV in semen and revealed that the pooled prevalence of HPV DNA in semen was 16% (95% confidence interval [CI]: 10%–23%) in the infertile population and 10% (95% CI: 7%–14%) in the general population. The prevalence of HPV in the semen of infertile males therefore appeared to be higher than that in the general population. In addition, it has been reported that HPV infections in semen can reduce sperm motility, increase sperm DNA fragmentation, and induce changes in semen pH.16,17,18
Recent evidence also suggests that HPV infection may affect male fertility,8 however, whether HPV infection represents a significant risk factor for male fertility abnormality remains uncertain. Therefore, we conducted this meta-analysis, and summarized the relevant published literature, to evaluate the implication of HPV infection in semen on male fertility abnormality.
MATERIALS AND METHODS
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.19
Literature search
A systematic literature search was performed in PubMed, Medline, Embase, Web of Science, and the Cochrane Library database for articles published from the earliest date available up to May 6, 2017. Searches were restricted to human studies and there was no language restriction. The following search terms were used in combination for search strategies: “human papillomavirus,” “HPV,” “sterility,” “infertility,” “sperm,” and “semen.” We also conducted manual searches of the reference lists of the review articles identified by our searches for additional reference material.
Inclusion and exclusion criteria
Studies were eligible for screening if they met the following criteria: (1) they reported the risk of HPV infection in semen for male infertility or fertility abnormality when compared to fertile males or reported sufficient data for calculation; (2) they represented a cohort study, case-control study, or cross-sectional study with a control group; and (3) HPV infection was defined as HPV DNA detected in semen samples by polymerase chain reaction (PCR) or other methods. Studies were excluded if they were (1) case reports, editorials, review articles, or opinions or (2) were without effective control groups to calculate effect estimates.
Data selection and extraction
Two authors independently evaluated all retrieved articles by title, abstract, and full text according to the above inclusion criteria. Any disagreement was resolved by consensus. Data were independently extracted from each eligible study, including first author, publication year, country of origin, study design, HPV detection method, HPV genotype, number of HPV-infected participants in the infertile or fertile male group, corresponding relative risks (RRs) or odds ratios (ORs), and 95% CI values. When data were reported from overlapping study samples (e.g., multiple publications from the same study), the most recent and comprehensive report was considered.
Quality assessment
The quality of case-control studies was assessed using the Newcastle–Ottawa Scale (NOS).20,21 In this scale, studies were scored across three categories: selection of subjects, comparability of study groups, and the assessment of outcome/exposure. This rating system was used to indicate the quality of a study, with a maximum score of nine. Studies were graded on an ordinal scoring scale, with higher scores representing studies of higher quality. The quality of cross-sectional studies was assessed using the Agency for Healthcare Research and Quality (AHRQ) statement.22
Statistical analysis
ORs, with their corresponding 95% CIs, were selected to represent the effect size to assess the risk of HPV infection for male fertility abnormality. Inter-study heterogeneity was estimated using the I2 statistic. Significant heterogeneity was defined when I2 ≥ 50%. Pooled results were calculated with a fixed-effects model (the Mantel and Haenszel method) when heterogeneity was not significant (I2 < 50%); otherwise, a random-effects model (the DerSimonian and Laird method) was applied. Sensitivity analysis was also used to evaluate whether any single study dominated the results of the meta-analyses by sequentially removing individual eligible studies. Finally, publication bias was assessed by visual inspection of funnel plots and Egger's linear regression.23 All statistical analyses were conducted using STATA 12.0 (Stata Corp LP, College Station, TX, USA).
RESULTS
Description of the studies identified by literature searches
The initial literature search yielded 937 potentially relevant studies. Most ineligible studies were excluded based on information in the title or abstract and the remaining 50 studies were reviewed in detail, which included 49 full-text journal articles and one conference abstract article. Scanning of the reference lists of these articles did not identify any additional material. The selection process is shown in Figure 1. As a result, eight articles were included in the final meta-analysis, providing data on 1955 participants.24,25,26,27,28,29,30,31 The main characteristics of the studies included in our meta-analysis are described in Table 1. Most of these studies were of high quality; only two were of low quality.27,31 In five studies, the authors detected both high-risk HPV (HR-HPV) and low-risk HPV (LR-HPV) genotypes in semen.24,26,28,30 In another two studies, the authors only investigated HR genotypes.25,27 In four studies, the authors excluded males from groups of infertile males because of an infertility factor associated with their spouse.24,25,29,30 In one study, males were defined as infertile when their sperm concentration was <20 × 106 ml−1 or when sperm motility was <50%,26 while in another study, all participants in the infertile male groups were additionally affected by infection of the male accessory gland.28 Two studies did not report a detailed definition of male infertility.27,31
Figure 1.
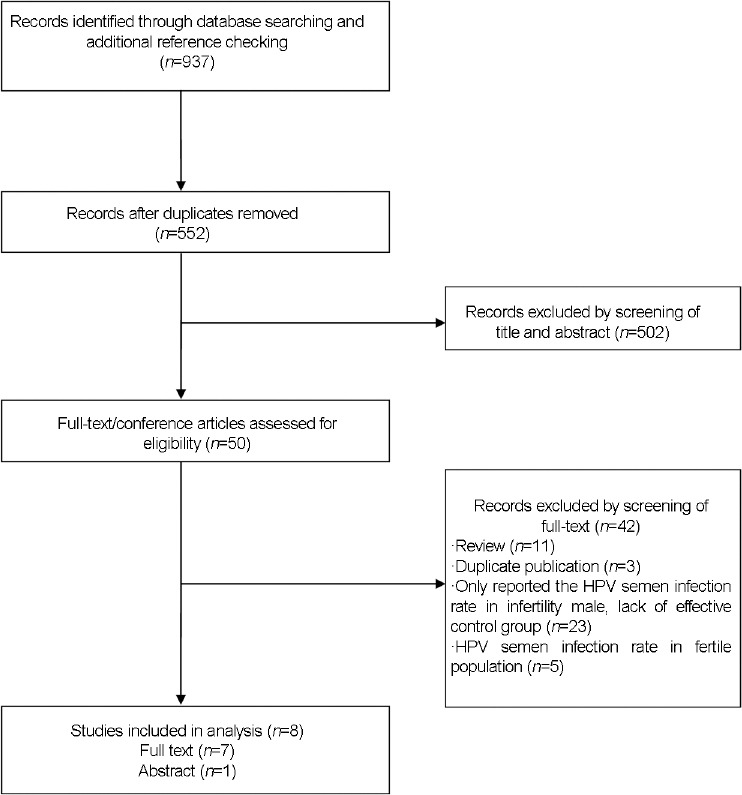
Flow diagram of the studies identified in the meta-analysis. CI: confidence interval; OR: odds ratio; HPV: Human papillomavirus.
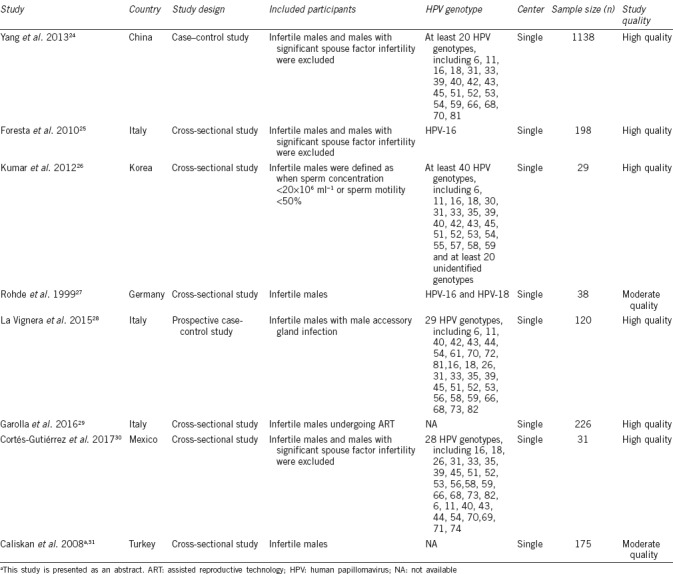
Table 1.
Basic characteristics of the eligible studies included in the present meta-analysis
Risk of HPV infection for male fertility abnormality
Due to the lack of a detailed definition of male infertility, two studies27,31 were removed from the pooled analysis of the risk of HPV infection upon male fertility abnormality. The results of six studies,24,25,26,28,29,30 with a total of 1756 participants, indicated that the infection of semen with HPV was a risk factor for male fertility abnormality, with a pooled OR of 3.02 (95% CI: 2.11–4.32; I2 = 6.9%; Figure 2).
Figure 2.
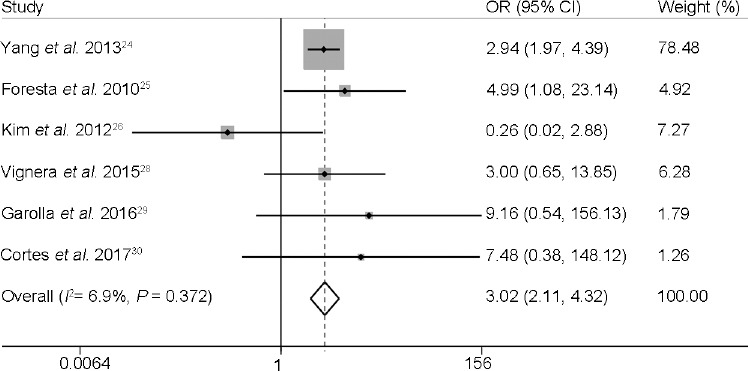
The risk of human papillomavirus semen infection for male fertility abnormality. CI: confidence interval; OR: odds ratio.
In subgroup analysis, involving studies where the authors had excluded males with an infertility factor associated with their spouse,24,25,27,29,30,31 the pooled OR was 3.25 (95% CI: 2.22–4.75; I2 = 0.0%).
Sensitivity analysis
In the sensitivity analysis, we observed that no individual study altered the overall significance of the ORs in the analyses relating to the impact of HPV semen infection on male fertility abnormality (Figure 3). Additionally, we added the two studies which did not define male infertility, into the pooled analysis of the risk of HPV infection for male fertility.27,31 The pooled OR of a total of eight studies24,25,26,27,28,29,30,31 with a total of 1969 participants was 2.93 (95% CI: 2.06–4.15; I2 = 0.0%), which still suggested that the infection of semen with HPV was a risk factor for male fertility abnormality.
Figure 3.
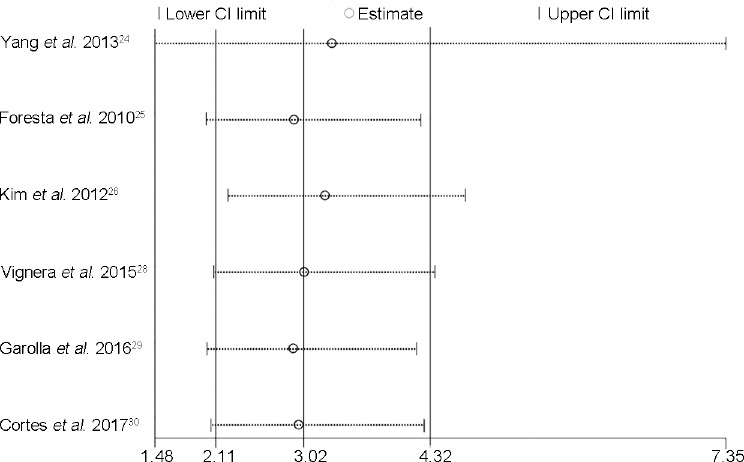
Sensitivity analysis of the risk of human papillomavirus semen infection for male infertility. CI: confidence interval.
Published bias
No significant asymmetry was found in our analyses of the impact of HPV semen infection on male fertility abnormality (P = 0.98).
DISCUSSION
To the best of our knowledge, this is the first meta-analysis to evaluate the effect of HPV infection in semen upon male fertility abnormality. Our results suggest that the infection of semen by HPV represents a risk factor for male fertility abnormality with a pooled OR of 3.02 (95% CI: 2.11–4.32). No significant inter-study heterogeneity or publication bias was identified in this meta-analysis. In addition, subgroup analyses and sensitivity analysis both indicated that HPV semen infection is a risk factor for male fertility abnormality.
Although the results of our study suggest that HPV semen infection is a risk factor for male fertility abnormality, the specific mechanisms underlying this association still remain unclear. One possibility is that HPV infection causes changes in key sperm parameters. Several studies have investigated sperm parameters in semen from HPV-positive and HPV-negative patients in the infertile and fertile population; the majority of these studies concluded that HPV infection might cause the impairment of critical sperm parameters, for example, by reducing progressive sperm motility or causing changes in sperm morphology.24,25,28,32,33,34
HPV is the most common sexually transmitted virus worldwide and more than 180 HPV genotypes have been reported.35 According to its association with different neoplasms, HPV can be divided into two different groups: HR-HPV and LR-HPV.13 Yang et al.24 investigated HPV semen infection in 615 infertile and 523 fertile males. These authors showed that HPV-45, HPV-16, HPV-52, HPV-18/59, and HPV-33, in decreasing order, were the most common genotypes in the infertile group and that the most common genotypes in the fertile group were HPV-68/81, HPV-33, and HPV-39. In addition, only five HR-HPV genotypes in the infertile group (HPV-16, HPV-18, HPV-45, HPV-52, and HPV-59) were significantly higher than those in the fertile group with ORs of 6.5, 11.3, 13.9, 12.2, and 11.3, respectively. Similarly, Foresta et al.25 showed that the HPV-16 semen infection rate was 10.2% in 108 infertile males and just 2.2% in 90 fertile males, with an OR of 5.0. HR-HPV and LR-HPV genotypes may need to be recognized separately to determine the relative risk for male fertility abnormality. Whether the impact of male fertility abnormality with HR-HPV and LR-HPV infection can be distinguished, or whether only HR-HPV infection has an impact upon infertility, requires further investigation.
Previous studies have reported that HPV cervical infection in females might reduce pregnancy rate and increase the risk of spontaneous abortion in infertile couples undergoing ART.36,37,38,39,40 Similarly, HPV semen infection might also alter the pregnancy rate and risk of spontaneous abortion in infertile couples undergoing ART. In a cross-sectional clinical study, cumulative pregnancy rates of 38.4% and 14.2% were observed in infertile couples undergoing ART in which semen was either infected or not infected with HPV, respectively.29 During the follow-up of these pregnancies, a higher miscarriage rate was observed in those cases involving HPV-infected semen (62.5% versus 16.7%). When considering the high prevalence rate of HPV semen infection in the infertile population,15 the potential risk of impaired fertility, and the persistently long duration of semen infection (approximately 15.3 months),41 it is clear that caution should be recommended for couples in which the male has HPV-infected semen.
In addition to HPV, there are many sexually transmitted diseases which may result in pregnancy complications and infertility,42,43,44 such as Chlamydia trachomatis, genital mycoplasmas, Neisseria gonorrhoeae, Hepatitis, and human immunodeficiency virus. Some sexually transmitted diseases, and other infections, may increase the risk of pregnancy complications, including miscarriage, spontaneous preterm birth, and low birth weight, which have been described in detail in previous systematic reviews and meta-analyses.43,45,46 Fode et al.42 conducted a systematic review to evaluate the possible association between sexually transmitted diseases and male fertility abnormality. The authors collated information from existing articles involving Chlamydia trachomatis, Neisseria gonorrhoeae, Trichomonas vaginalis, genital mycoplasmas, Epstein–Barr virus, Hepatitis virus and human immunodeficiency virus. However, limited by contradictory results and the limited quality of the original studies involved, these authors concluded that they could not be certain that there was an association between sexually transmitted diseases and male infertility. Consequently, further studies are now needed, involving a larger number of subjects.
It has been reported that approximately half of infertile couples are associated with a defect in male reproductive function.1,47 A number of factors may affect male infertility, including anti-sperm antibodies, azoospermia, chromosome abnormalities, mumps orchitis, and sexually transmitted infections.47 In fact, since there are no definitive male infertility diagnostic criteria, male infertility is not easy to diagnose clinically. In the studies included in our analysis, some of the authors defined the infertile male as those subjects with altered sperm parameters, at least 1 year (or 2 years) of unprotected sexual intercourse without conception, and with a healthy normal female partner (in which tubal, uterine, cervical abnormalities, and ovarian disorders were excluded).24,25,26,29,30 Subjects with a history of cryptorchidism, testicular trauma, or postmumps orchitis were also excluded. However, two of the studies included in our meta-analysis did not present a detailed definition for the infertile males involved in their research.27,31 There is a clear need for published articles to include a precise definition of male infertility, along with detailed inclusion and exclusion criteria.
At present, three vaccines are available against HPV (bivalent, quadrivalent, and 9-valent). HPV vaccination programs have been implemented across many countries worldwide to prevent the high mortality arising from cervical cancer and to reduce the incidence of dysplasia and genital warts.48 However, the impact of HPV vaccination on HPV semen infection and male infertility is relatively unexplored. Foresta et al.32 investigated the impact of prophylactic vaccination against HPV on virus clearance in infertile male patients with HPV semen infection. These authors concluded that prophylactic HPV vaccination in infertile males can improve healing from viral semen infection by reducing clearance time.32 However, due to insufficient evidence, it is currently unclear whether HPV vaccination has any significant benefit in terms of reducing the risk of male infertility and therefore requires further investigation.
The present meta-analysis was associated with some limitations which should be considered when interpreting our results. First, coinfection with other pathogens (e.g., Chlamydia trachomatis), genetic factors, and environmental exposures may have confounding effects on the association between HPV semen infection and male fertility abnormality. Since most of the original articles included in our present study lacked adjustment for such confounding factors, it is possible that factors other than HPV semen infection were not considered but could also have caused influence on fertility. Second, most of the articles included in the present study were not prospectively designed and may therefore reduce the reliability of our results.
CONCLUSIONS
The infection of semen with HPV was identified to represent a risk factor for male fertility abnormality. Further prospective studies, which include adjustment for confounding factors, are now needed to confirm the association between HPV semen infection and male fertility abnormality.
AUTHOR CONTRIBUTIONS
YQX carried out the design of this study and drafted the manuscript. YXC carried out the statistical analysis. MJC and WQH carried out the data search, selection, and study quality assessment. QC conceived of the study, participated in coordination and helped to draft the manuscript. All authors have read and approved the final version of the manuscript and agreed with the order of presentation of the authors.
COMPETING INTERESTS
All authors declared no competing interests.
REFERENCES
- 1.Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99:1324–31.e1. doi: 10.1016/j.fertnstert.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Szkodziak P, Wozniak S, Czuczwar P, Wozniakowska E, Milart P, et al. Infertility in the light of new scientific reports – Focus on male factor. Ann Agric Environ Med. 2016;23:227–30. doi: 10.5604/12321966.1203881. [DOI] [PubMed] [Google Scholar]
- 3.Pellati D, Mylonakis I, Bertoloni G, Fiore C, Andrisani A, et al. Genital tract infections and infertility. Eur J Obstet Gynecol Reprod Biol. 2008;140:3–11. doi: 10.1016/j.ejogrb.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Bezold G, Politch JA, Kiviat NB, Kuypers JM, Wolff H, et al. Prevalence of sexually transmissible pathogens in semen from asymptomatic male infertility patients with and without leukocytospermia. Fertil Steril. 2007;87:1087–97. doi: 10.1016/j.fertnstert.2006.08.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Conde-Ferraez L, Chan May Ade A, Carrillo-Martinez JR, Ayora-Talavera G, Gonzalez-Losa Mdel R. Human papillomavirus infection and spontaneous abortion: a case-control study performed in Mexico. Eur J Obstet Gynecol Reprod Biol. 2013;170:468–73. doi: 10.1016/j.ejogrb.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Skoczynski M, Gozdzicka-Jozefiak A, Kwasniewska A. Prevalence of human papillomavirus in spontaneously aborted products of conception. Acta Obstet Gynecol Scand. 2011;90:1402–5. doi: 10.1111/j.1600-0412.2011.01189.x. [DOI] [PubMed] [Google Scholar]
- 7.Ticconi C, Pietropolli A, Fabbri G, Capogna MV, Perno CF, et al. Recurrent miscarriage and cervical human papillomavirus infection. Am J Reprod Immunol. 2013;70:343–6. doi: 10.1111/aji.12156. [DOI] [PubMed] [Google Scholar]
- 8.Souho T, Benlemlih M, Bennani B. Human papillomavirus infection and fertility alteration: a systematic review. PloS One. 2015;10:e0126936. doi: 10.1371/journal.pone.0126936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giuliano AR, Nielson CM, Flores R, Dunne EF, Abrahamsen M, et al. The optimal anatomic sites for sampling heterosexual men for human papillomavirus (HPV) detection: the HPV detection in men study. J Infect Dis. 2007;196:1146–52. doi: 10.1086/521629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garolla A, Pizzol D, Foresta C. The role of human papillomavirus on sperm function. Curr Opin Obstet Gynecol. 2011;23:232–7. doi: 10.1097/GCO.0b013e328348a3a4. [DOI] [PubMed] [Google Scholar]
- 11.Rintala MA, Pollanen PP, Nikkanen VP, Grenman SE, Syrjanen SM. Human papillomavirus DNA is found in the vas deferens. J Infect Dis. 2002;185:1664–7. doi: 10.1086/340421. [DOI] [PubMed] [Google Scholar]
- 12.Giovannelli L, Migliore MC, Capra G, Caleca MP, Bellavia C, et al. Penile, urethral, and seminal sampling for diagnosis of human papillomavirus infection in men. J Clin Microbiol. 2007;45:248–51. doi: 10.1128/JCM.01576-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foresta C, Noventa M, De Toni L, Gizzo S, Garolla A. HPV-DNA sperm infection and infertility: from a systematic literature review to a possible clinical management proposal. Andrology. 2015;3:163–73. doi: 10.1111/andr.284. [DOI] [PubMed] [Google Scholar]
- 14.Schillaci R, Capra G, Bellavia C, Ruvolo G, Scazzone C, et al. Detection of oncogenic human papillomavirus genotypes on spermatozoa from male partners of infertile couples. Fertil Steril. 2013;100:1236–40. doi: 10.1016/j.fertnstert.2013.06.042. [DOI] [PubMed] [Google Scholar]
- 15.Laprise C, Trottier H, Monnier P, Coutlee F, Mayrand MH. Prevalence of human papillomaviruses in semen: a systematic review and meta-analysis. Hum Reprod. 2014;29:640–51. doi: 10.1093/humrep/det453. [DOI] [PubMed] [Google Scholar]
- 16.Garolla A, Lenzi A, Palu G, Pizzol D, Bertoldo A, et al. Human papillomavirus sperm infection and assisted reproduction: a dangerous hazard with a possible safe solution. Hum Reprod. 2012;27:967–73. doi: 10.1093/humrep/des009. [DOI] [PubMed] [Google Scholar]
- 17.Rintala MA, Grenman SE, Pollanen PP, Suominen JJ, Syrjanen SM. Detection of high-risk HPV DNA in semen and its association with the quality of semen. Int J STD AIDS. 2004;15:740–3. doi: 10.1258/0956462042395122. [DOI] [PubMed] [Google Scholar]
- 18.Lee CA, Huang CT, King A, Chan PJ. Differential effects of human papillomavirus DNA types on p53 tumor-suppressor gene apoptosis in sperm. Gynecol Oncol. 2002;85:511–6. doi: 10.1006/gyno.2002.6662. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 21.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, et al. The Newcastle. Ottawa Scale (NOS) for Assessing the Quality if Nonrandomized Studies in Meta. Analyses. 2009. [Last accessed on 2018 Jan 21]. Available from: http://www.ohrica/programs/clinical_epidemiology/oxford.htm .
- 22.Rostom A, Dube C, Cranney A, Saloojee N, Richmond Sy, et al. Celiac Disease. Rockville (MD): Agency for Healthcare Research and Quality (US), (Evidence Reports/Technology Assessments, No. 104.) 2004. [Last accessed on 2018 Jan 21]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK35156 .
- 23.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang Y, Jia CW, Ma YM, Zhou LY, Wang SY. Correlation between HPV sperm infection and male infertility. Asian J Androl. 2013;15:529–32. doi: 10.1038/aja.2013.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foresta C, Pizzol D, Moretti A, Barzon L, Palu G, et al. Clinical and prognostic significance of human papillomavirus DNA in the sperm or exfoliated cells of infertile patients and subjects with risk factors. Fertil Steril. 2010;94:1723–7. doi: 10.1016/j.fertnstert.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Kumar K, Deka D, Singh A, Chattopadhyay P, Dada R. Expression pattern of PRM2, HSP90 and WNT5A in male partners of couples experiencing idiopathic recurrent miscarriages. J Genet. 2012;91:363–6. doi: 10.1007/s12041-012-0200-4. [DOI] [PubMed] [Google Scholar]
- 27.Rohde V, Erles K, Sattler HP, Derouet H, Wullich B, et al. Detection of adeno-associated virus in human semen: does viral infection play a role in the pathogenesis of male infertility? Fertil Steril. 1999;72:814–6. doi: 10.1016/s0015-0282(99)00363-5. [DOI] [PubMed] [Google Scholar]
- 28.La Vignera S, Vicari E, Condorelli RA, Franchina C, Scalia G, et al. Prevalence of human papilloma virus infection in patients with male accessory gland infection. Reprod Biomed Online. 2015;30:385–91. doi: 10.1016/j.rbmo.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Garolla A, Engl B, Pizzol D, Ghezzi M, Bertoldo A, et al. Spontaneous fertility and in vitro fertilization outcome: new evidence of human papillomavirus sperm infection. Fertil Steril. 2016;105:65–72.e1. doi: 10.1016/j.fertnstert.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 30.Cortés-Gutiérrez EI, Dávila-Rodríguez MI, Fernández JL, de la O-Pérez LO, Garza-Flores ME, et al. The presence of human papillomavirus in semen does not affect the integrity of sperm DNA. Andrologia. 2017;49:e12774. doi: 10.1111/and.12774. [DOI] [PubMed] [Google Scholar]
- 31.Caliskan T, Kocak I, Kirdar S, Serter M, Okyay P, et al. Human papilloma virus and Chlamydia trochomatis in asymptomatic Turkish men: prevalence and relation among semen parameters and IL-18 levels. Eur Urol Suppl. 2008;7:156. [Google Scholar]
- 32.Foresta C, Garolla A, Parisi S, Ghezzi M, Bertoldo A, et al. HPV prophylactic vaccination in males improves the clearance of semen infection. EBioMedicine. 2015;2:1487–93. doi: 10.1016/j.ebiom.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garolla A, Pizzol D, Bertoldo A, De Toni L, Barzon L, et al. Association, prevalence, and clearance of human papillomavirus and antisperm antibodies in infected semen samples from infertile patients. Fertil Steril. 2013;99:125–31. doi: 10.1016/j.fertnstert.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Garolla A, Pizzol D, Ghezzi M, Selice R, Bertoldo A, et al. Prevalence and clearance of human papillomavirus in semen samples of infertile patients and role on sperm parameters. Hum Reprod. 2013;28:32. [Google Scholar]
- 35.Bernard HU, Burk RD, Chen Z, van Doorslaer K, zur Hausen H, et al. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology. 2010;401:70–9. doi: 10.1016/j.virol.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oborna I, Ondryasova H, Zborilova B, Brezinova J, Vrbkova J. Does presence of human papillomavirus (HPV) infection influence the results of in vitro fertilization (IVF) treatment? Fertil Steril. 2016;106:e335–6. [Google Scholar]
- 37.Tanaka H, Karube A, Kodama H, Fukuda J, Tanaka T. Mass screening for human papillomavirus type 16 infection in infertile couples. J Reprod Med. 2000;45:907–11. [PubMed] [Google Scholar]
- 38.Yang R, Wang Y, Qiao J, Liu P, Geng L, et al. Does human papillomavirus infection do harm to in vitro fertilization outcomes and subsequent pregnancy outcomes? Chin Med J (Engl) 2013;126:683–7. [PubMed] [Google Scholar]
- 39.Comar M, Monasta L, Zanotta N, Vecchi Brumatti L, Ricci G, et al. Human papillomavirus infection is associated with decreased levels of GM-CSF in cervico-vaginal fluid of infected women. J Clin Virol. 2013;58:479–81. doi: 10.1016/j.jcv.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Perino A, Giovannelli L, Schillaci R, Ruvolo G, Fiorentino FP, et al. Human papillomavirus infection in couples undergoing in vitro fertilization procedures: impact on reproductive outcomes. Fertil Steril. 2011;95:1845–8. doi: 10.1016/j.fertnstert.2010.11.047. [DOI] [PubMed] [Google Scholar]
- 41.Capra G, Nyitray AG, Lu B, Perino A, Marci R, et al. Analysis of persistence of human papillomavirus infection in men evaluated by sampling multiple genital sites. Eur Rev Med Pharmacol Sci. 2015;19:4153–63. [PubMed] [Google Scholar]
- 42.Fode M, Fusco F, Lipshultz L, Weidner W. Sexually transmitted disease and male infertility: a systematic review. Eur Urol Focus. 2016;2:383–93. doi: 10.1016/j.euf.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Giakoumelou S, Wheelhouse N, Cuschieri K, Entrican G, Howie SE, et al. The role of infection in miscarriage. Hum Reprod Update. 2016;22:116–33. doi: 10.1093/humupd/dmv041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rompalo A. Preventing sexually transmitted infections: back to basics. J Clin Invest. 2011;121:4580–3. doi: 10.1172/JCI61592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang QT, Zhong M, Gao YF, Huang LP, Huang Q, et al. Can HPV vaccine have other health benefits more than cancer prevention?. A systematic review of association between cervical HPV infection and preterm birth. J Clin Virol. 2014;61:321–8. doi: 10.1016/j.jcv.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 46.Paixao ES, Teixeira MG, Costa Mda C, Rodrigues LC. Dengue during pregnancy and adverse fetal outcomes: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16:857–65. doi: 10.1016/S1473-3099(16)00088-8. [DOI] [PubMed] [Google Scholar]
- 47.WHO Manual for the Standardized Investigation, Diagnosis and Management of the Infertile Male. WHO. 2000 [Google Scholar]
- 48.Bonde U, Joergensen JS, Mogensen O, Lamont RF. The potential role of HPV vaccination in the prevention of infectious complications of pregnancy. Expert Rev Vaccines. 2014;13:1307–16. doi: 10.1586/14760584.2014.944164. [DOI] [PubMed] [Google Scholar]


