Abstract
Non-communicable diseases are important causes of mortality and morbidity in India. Data from the Registrar General of India, World Health Organization and Global Burden of Disease (GBD) Study have reported that cardiovascular diseases (CVD) are the most important causes of death and disability. Age-adjusted mortality from these conditions has increased by 31% in last 25 years. Case-control studies have reported that hypertension is most important risk factor for CVD in India. GBD Study has estimated that hypertension led to 1.6 million deaths and 33.9 million disability-adjusted life years in 2015 and is most important cause of disease burden in India. Intensive public health effort is required to increase its awareness, treatment and control. UN Sustainable Development Goals highlight the importance of high rates of hypertension control for achieving target of 1/3 reduction in non-communicable disease mortality by 2030. It is estimated that better hypertension control can prevent 400–500,000 premature deaths in India.
Keywords: Hypertension, India, Cardiovascular disease, Global burden of disease study, Non-Communicable disease
1. Introduction
Morbidity and mortality data in India have always highlighted primacy of communicable diseases and maternal and childhood conditions as leading causes.1, 2 Indeed, up to end of the last century acute and chronic infections, e.g., neonatal and childhood gastrointestinal infections, viral and bacterial lower respiratory infections, poliomyelitis, malaria and tuberculosis along with neonatal sepsis, childhood malnutrition and maternal mortality were important causes.1 Public health measures focused on these conditions, along with overall socioeconomic change have led to a remarkable decline in death rates from these conditions.3 This has been due to focus on preventive measures directed towards these conditions- better hygiene, immunization, improved maternal and childhood nutrition and health systems focused on health during pregnancy and management of acute and chronic infections.3
Chronic non-communicable diseases have emerged as leading causes of mortality and morbidity only at the turn of the present century in India.4 Registrar General of India first reported this transition while enumerating causes of deaths in the country for years 2001–2003.5 Non-communicable diseases (NCD’s), also known as chronic diseases and better as socially transmitted diseases, caused more than 50% of deaths in these years and cardiovascular diseases (CVDs) emerged as the most important cause. Increasing proportion of NCD’s as cause of deaths has been reported in the latest Registrar General of India report also.6 Serial data from the Census of India have also reported increasing proportionate mortality from CVD in India.7
The present article summarizes trends in major CVD’s (ischemic heart disease-IHD and stroke) in terms of absolute numbers and age-adjusted rates in India using the World Health Organization (WHO) and Global Burden of Diseases (GBD) Study data. We used previous studies to identify CVD risk factors of importance in Indians.8, 9 We then summarized the trends in CVD risk factors in India using previous reviews.7, 10, 11, 12, 13, 14, 15 Using GBD study data along with risk factor prevalence trends have highlighted the observation that hypertension is the most important risk factor for CVD, non-communicable diseases as well as overall diseases in India. Public health, health systems based as well as clinic-based interventions are needed to increase awareness, treatment and control of hypertension.16 It is well known that up to a third of cardiovascular deaths can be avoided by proper treatment and control of hypertension17 and by addressing this risk factor we can significantly prevent premature CVD mortality in India.
2. Methods
Data for this narrative review have been obtained from multiple sources. Mortality data for India were obtained from the Government of India and Registrar General of India using previous publications and websites of the Census of India and Registrar General of India.5, 6 These data were also used to determine the proportionate mortality from various disease conditions in India. We used electronic databases of WHO18, 19 and GBD Study 201520 to identify absolute number of deaths from CVD in India. In the GBD study, annual data on absolute numbers of CVD deaths including deaths from major CVD types- IHD, stroke (hemorrhagic and ischemic), rheumatic heart disease and others are available. We retrieved data of major CVD causes at 5-year time points (1990, 1995, 2000, 2005, 2010 and 2015) to simplify evaluation of the trends.20 We also obtained age-adjusted death rates per 100,000 persons for CVD and its subtypes from the GBD Study. Finally, data on the top ten Category 2 (broad category of risk factors) and Category 3 (specific risk factors) factors responsible for disease burden in India were obtained from GBD study and tabulated according to absolute mortality as well as disability adjusted life years (DALY’s).20 Data regarding hypertension prevalence, awareness, treatment and control have been obtained from previously published reviews.7, 10, 11, 12, 21, 22 Trends in other CVD risk factors have been obtained from previous publications7, 10, 11, 13, 14, 15 and GBD 2015 study.20 The data are presented as a narrative review and not as a systematic review, both are equally important as discussed recently.23 Descriptive statistics are presented.
3. Cardiovascular mortality in india
3.1. Registrar General of India
Mortality data has been collected by Registrar General of India based on hospital records at limited urban and rural sites in the country. There has also been a vast schism between actual causes of deaths in India and those reported by various agencies. These data are reported as proportionate mortality from various causes.6 Accordingly CVD caused about 12–15% of all deaths in India in 1980s to 1990′s.24 As the number of deaths has been increasing in each year, these proportions would result in escalating absolute number of deaths from CVD in the country. Since 2001–2003 the Registrar General of India has developed a verbal autopsy based system to assess causes of deaths in the country within the Indian Sample Registration System.25 Between 2001–2003 trained census enumerators obtained details of events leading to death (verbal autopsy narrative) at more than 600,000 households spread across all the districts in the country. Ascertainment of causes of deaths was performed independently by two trained physicians for each narrative and cross-checked for consensus. Validation protocol was used to ensure agreement and International Classification of Diseases (ICD)-10 codes were used. Cardiovascular diseases were diagnosed with codes G45, G46, G81-83, 100–128, 131,134-184, 186–199 and R00-R01, R03, R55 and R96.5, 6, 26 Proportionate mortality from cardiovascular diseases was calculated for different age-groups and has been reported.5, 6
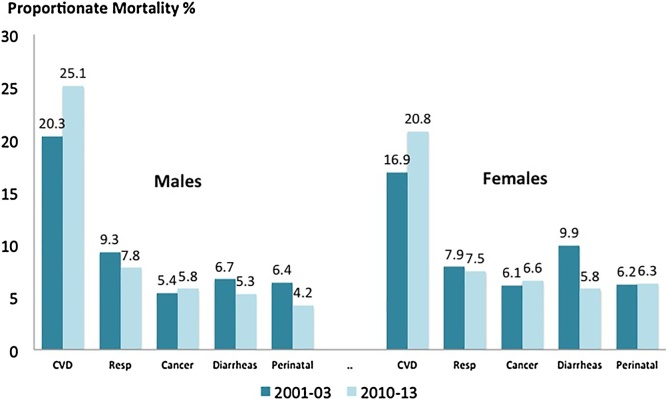
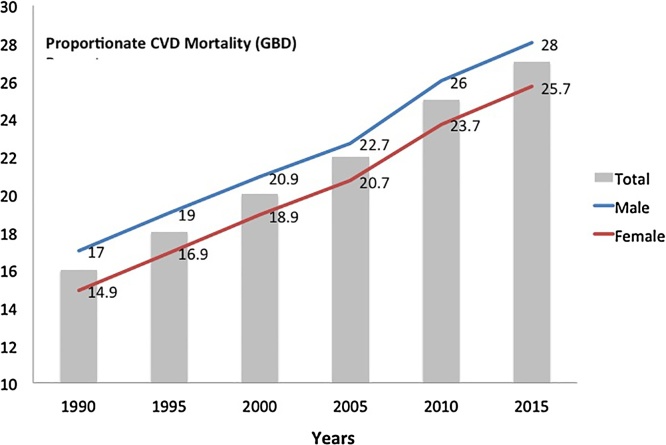
In 2001–2003 the top five causes of deaths, as percent of total mortality were CVS’s (males 20.3, females 16.9), respiratory diseases (males 9.3, females 8.0), diarrheal diseases (males 6.7, females 9.9), perinatal problems (males 6.4, females 6.2), and chest infections (males 5.4, females 7.1).5 This exercise has been periodically repeated at various sample registration system sites and the latest data are available for the years 2010–2013.6 At this time-period the top five causes of deaths were cardiovascular diseases (males 25.1, females 20.8), respiratory diseases (males 7.8, females 7.5), cancer (males 5.8, females 6.6), diarrheal diseases (males 5.3, females 5.8) and perinatal problems (males 4.2, females 6.3). CVD’s retain the top position while cancer related mortality has increased. On the other hand, proportionate mortality from respiratory diseases, perinatal causes and diarrheal diseases has shown a significant decline (Fig. 1). Increasing proportionate mortality (% of all deaths) from CVD’s in India has also been reported by the GBD Study (Fig. 2). There are large regional variations in CVD’s in India10, 11 and a major limitation of these mortality data is lack of state-level statistics. The Indian Burden of Diseases Investigators have recently published state level mortality data.27 The study has reported that CVD’s are among the most important causes of deaths in all the regions and states of India.27 These data are important because in India health is a state subject and lack of state-level data hampers policy-led focus on prevention and treatment these conditions.3, 4
Fig. 1.
Change in proportionate mortality form the top 5 causes of deaths in India according to Registrar General of India reports in years 2001–03 and 2010–13.
Fig. 2.
Increasing proportionate mortality from cardiovascular diseases in India. Data are from Global Burden of Disease (GBD) Study 2015.
3.2. World Health Organization
WHO has been tabulating mortality statistics for various member nations for the past many years. Recently the focus has shifted to global burden of NCD’s following the WHO Framework and UN General Assembly declaration on NCDs.26 The WHO data are available at their website- http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Mortality statistics are provided as absolute number of deaths from various causes. In India, for the year 2014, CVDs were reported as the most important causes of deaths and led to 2.48 million deaths/year comprising deaths from IHD (1.45 million/y), stroke (0.69 million/y), rheumatic heart disease (0.11 million/y) and other CVDs.19 Other leading causes of deaths include respiratory infections, diarrheal diseases, perinatal causes, tuberculosis and cancers, and are similar to the Registrar General of India report.5
WHO has also provided absolute number of CVD related deaths at various time points.19 Accordingly individuals dying from CVDs in the year 2000 were 1.93 million, 1.96 million in 2005, 2.25 million in 2010 and 2.48 million in 2015. Deaths from IHD increased and in the years 2000, 2005, 2010 and 2015 were 0.91, 1.06, 1.28 and 1.45 million, respectively while stroke deaths have increased at a lower rate and were 0.61, 0.64, 0.66 and 0.69 million, respectively.
3.3. Global Burden of Disease Study
GBD has been periodically estimating mortality and morbidity burden from various diseases and risk factors in almost all countries of the world for the last 20 years.28 The initial GBD effort was jointly led by investigators from WHO in collaboration with many academic centers around the globe and was modeled on the World Development Report 1993.29 The initial report was published in 1997.30 Recent emergence of big-data analytics using greater computer processing speeds have led to data being upgraded and published every 1–2 years. In recent years data have been published for GBD 2010, 2013 and 2015 with an upcoming series of reports for GBD 2016.31, 32, 33, 34 GBD uses DisMod-MR 2.1, a Bayesian meta-regression tool, as the main method of estimation ensuring consistency between disease incidence, prevalence, remission, and cause of death rates for more than 300 conditions. Recent versions of GBD comply with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).33, 34
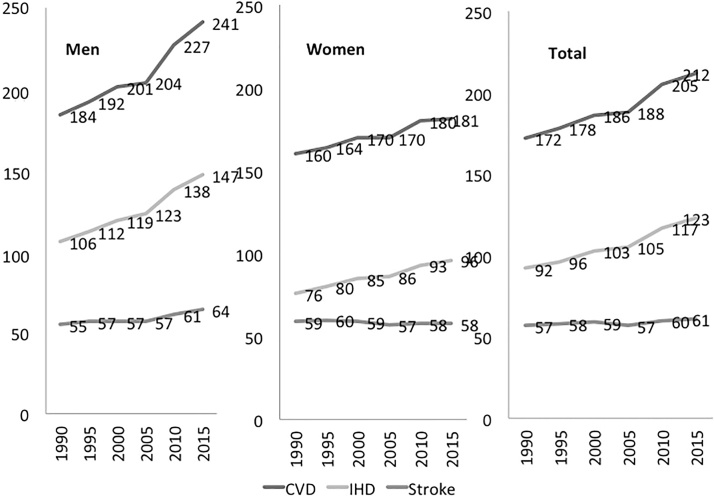
Data for India have been obtained from GBD website based on GBD 2015 study.20 In terms of absolute numbers there has been a steady increase in persons dying from cardiovascular diseases (Table 1). The increase is due to increasing mortality from IHD and strokes. Data from other diseases such as rheumatic heart disease are also available but not included in this article due to focus on hypertension related conditions. Age adjusted mortality statistics are shown in Table 2. There is significant increase in absolute as well as age-adjusted mortality rates from CVD and IHD while stroke mortality rates have stabilized and, indeed, decreased in women (Fig. 3). The increase in CVD and IHD mortality in India is in contrast to developed countries and most middle-income countries, including China, where there has been a 30–70% decline in CVD mortality in the past 50 years.35, 36
Table 1.
Global Burden of Diseases Study data on absolute number of mortality due to cardiovascular disease, ischemic heart disease and stroke (in thousands) in males, females and overall from 1990 to 2015 in India (Available at: www.ghdx.healthdata.org/gbd-results-tool).
| Cardiovascular disease |
Ischemic heart disease |
Stroke |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| 1990 | 828.9 | 673.1 | 1501.9 | 476.2 | 321.0 | 797.2 | 247.4 | 248.9 | 496.3 |
| 1995 | 953.5 | 760.1 | 1713.5 | 555.5 | 370.4 | 925.9 | 283.0 | 278.1 | 561.1 |
| 2000 | 1095.8 | 863.2 | 1959.0 | 651.2 | 429.8 | 1081.0 | 317.2 | 302.4 | 619.6 |
| 2005 | 1211.0 | 936.7 | 2148.5 | 729.2 | 474.0 | 1203.2 | 337.7 | 314.5 | 652.2 |
| 2010 | 1451.0 | 1065.8 | 2516.8 | 881.4 | 553.3 | 1434.7 | 371.3 | 343.3 | 734.6 |
| 2015 | 1634.9 | 1146.0 | 2780.9 | 1001.8 | 608.3 | 1601.1 | 438.0 | 364.0 | 802.0 |
Numbers are in thousands.
Table 2.
Global Burden of Diseases Study data on age-adjusted mortality rates/100,000 due to cardiovascular disease, ischemic heart disease and stroke in males, females and overall from 1990 to 2015 in India (Available at: www.ghdx.healthdata.org/gbd-results-tool).
| Cardiovascular disease |
Ischemic heart disease |
Stroke |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| 1990 | 183.9 | 160.3 | 172.5 | 105.6 | 76.4 | 91.6 | 54.9 | 59.2 | 57.0 |
| 1995 | 191.5 | 164.0 | 178.2 | 111.6 | 79.9 | 96.3 | 56.8 | 60.0 | 58.4 |
| 2000 | 200.8 | 169.9 | 185.9 | 119.3 | 84.6 | 102.6 | 58.1 | 59.4 | 58.8 |
| 2005 | 204.4 | 169.9 | 187.8 | 123.0 | 86.0 | 105.2 | 57.0 | 57.0 | 57.0 |
| 2010 | 227.5 | 179.9 | 204.6 | 138.2 | 93.4 | 116.6 | 61.3 | 58.0 | 59.7 |
| 2015 | 240.5 | 181.4 | 212.0 | 147.4 | 96.3 | 122.8 | 64.4 | 57.6 | 61.2 |
Death rates are in numbers per 100,000
Fig. 3.
Trends in age-adjusted mortality rates/100,000 from cardiovascular disease, ischemic heart disease and stroke in men, women and overall from 1990 to 2015 in India. Global Burden of Disease Study.
4. Risk factors
Globally, the cardiovascular disease epidemic has followed socioeconomic development and industrialization. The first phase of industrial revolution in the developed countries was characterized with replacement of human effort in creating industrial goods by machines. These machines led to a decline in human effort and resulted in less physical activity and affluence which translated into consumption of unhealthy foods.37 Creation of industrial cities also led to a profound socioeconomic change and environmental pollution.37 Although it also led to better maternal nutrition and gain in average height of population, in the long-term, the adverse consequences of physical inactivity led to obesity and an exponential increase in multiple cardiovascular risk factors.38 Similar epidemiological transition is now happening in India.1, 39
Cardiovascular risk factors can be broadly divided into four groups- social determinants, lifestyle factors, biochemical factors and genetic factors (Table 3). Hundreds of risk factors within these four classes have been identified. There are no prospective epidemiological studies from India that have evaluated relative importance of various CVD risk factors in cardiovascular diseases. Determinants of ischemic coronary heart disease and stroke have been evaluated in large case-control studies in India. Global studies such as INTERHEART8 and INTERSTROKE9 have reported substantial contribution of standard cardiovascular risk factors in their pathogenesis. Accordingly eight common risk factors are responsible for incident acute coronary disease in South Asians: high apolipoprotein B/apolipoprotein A1 ratio, hypertension, diabetes, abdominal obesity, smoking, sedentary lifestyle, low fruit and vegetable intake and psychosocial stress.8 Hypertension was not the most important risk factor and its population attributable risk was lower than lipid abnormalities and smoking.8 However, the diagnosis of hypertension in INTERHEART study was made according to presence of known hypertension and not measured blood pressure and would have underestimated its prevalence in the South Asian population with low awareness of this condition.12, 22 INTERSTROKE study diagnosed hypertension based on measured blood pressure as well as known hypertension and reported that it is the most important risk factor for stroke (both hemorrhagic and ischemic) in India as well as globally.9 Thus, hypertension is the most important stroke risk factor and among top-3 of coronary risk factors in India and given its high prevalence and high contribution of stroke to CVD mortality in India (40–45%), it is the most important CVD risk factor in India.40
Table 3.
General classification of cardiovascular risk factors.
| Group 1: Social determinants | Group 2: Lifestyle factors | Group 3: Biological factors | Group 4: Genetic factors |
|---|---|---|---|
|
|
|
|
5. Recent hypertension epidemiology studies in India
Recent epidemiological studies have reported that hypertension is present in 25–30% urban and 10–20% rural subjects in India.12, 22 This translates into 100–110 million persons with this condition in the country. However, there are large regional variations in its prevalence and these prevalence rates may be not truly representative. Multisite studies that evaluated hypertension prevalence using similar tools in various regions of the country are few.40 Recently, a few large studies have been conducted but are limited to either male industrial workers,41 lower socioeconomic status women,42 middle class urban men and women,43 urban and rural men and women at a few locations in the country,44, 45, 46 or rural men and women,47 with poor national representativeness.
Fourth National Family Health Survey (NFHS-4) has reported significant regional variations in hypertension prevalence in the country. This survey was implemented in both urban and rural areas.48 A uniform sample design was adopted in all the districts. The primary sampling units for rural areas were Villages and Census Enumeration Blocks for urban locations. The field agencies were given a list of selected sampling units for each state or union territories that were selected for the fieldwork. NFHS-4 was designed to provide information on various demographic parameters and other family welfare and health indicators by background characteristics at the national and state level and, for the first time, at the district level also. Because of need to report health indicators at the district level, the NFHS-4 sample size was increased to 571,660 households, as compared with 109,041 households in NFHS-3. NFHS-4 adopted a two-stage sampling design in rural and urban areas of each district of India. Survey ultimately interviewed 601,509 households, 699,686 women and 103,525 men from 28,583 primary sampling units composed of villages in rural areas and census enumeration blocks in urban areas in 640 districts of the country.48 The domain of clinical, anthropometric and biochemical testing in NFHS-4 included random blood glucose and BP measurements with estimates to be reported at the district level for women aged 15–49 and men aged 15–54. All these components in the field were evaluated using portable equipment. An automatic and battery operated BP instrument was used. Only medical or other personnel with specific training on the procedures were involved. NFHS-4 was conducted in two phases, and each phase covered almost an equal number of states/groups of states and union territories.49
Hypertension data have been obtained from the NFHS-4 website50 and prevalence in various states among men and women is reported in Table 4. The sample sizes are population proportionate and the data shows that there are significant differences in prevalence of hypertension in different states of the country. Accordingly, the prevalence is much greater in the Southern, North Eastern and North Western states of the country and is significantly greater in men as compared to women (Table 4). Of the 33 states that are represented in Table 4, hypertension prevalence of >15% is observed in 8/33 (24.2%) states and low prevalence (<5%) is observed in 6/33 (18.2%) states. Other states have a medium prevalence 5–15%. A major shortcoming of the NFHS-4 program is the exclusion of middle and older aged adults. It is well known that hypertension prevalence increases with age. Exclusion of this high prevalence group has led to lower prevalence in this study.
Table 4.
Hypertension prevalence in young men (15–54y) and women (15–49y) in India in National Family Health Survey-4.
| State (alphabetic) | Sample size | Hypertension (known or BP ≥ 140/90 mmHg) |
||
|---|---|---|---|---|
| Men | Women | Total | ||
| Andaman & Nicobar | 3219 | 27.9 | 9.0 | 18.5 |
| Andhra Pradesh | 11826 | 16.2 | 10.0 | 13.1 |
| Arunachal Pradesh | 16224 | 21.6 | 15.0 | 18.3 |
| Assam | 32307 | 19.6 | 16.0 | 17.8 |
| Bihar | 51243 | 9.4 | 5.9 | 7.7 |
| Chandigarh | 866 | 13.5 | 9.3 | 11.4 |
| Chhattisgarh | 28701 | 12.7 | 8.8 | 10.8 |
| Delhi | 6586 | 4.2 | 7.6 | 5.9 |
| Goa | 2457 | 13.2 | 8.5 | 10.9 |
| Gujarat | 28506 | 13.0 | 9.7 | 11.4 |
| Haryana | 25032 | 16.8 | 9.2 | 13.0 |
| Himachal Pradesh | 12114 | 21.9 | 12.1 | 17.5 |
| Jammu & Kashmir | 29384 | 13.7 | 11.6 | 12.7 |
| Jharkhand | 32866 | 12.2 | 7.8 | 10.0 |
| Karnataka | 30034 | 15.4 | 9.7 | 12.6 |
| Kerala | 12897 | 9.5 | 6.8 | 8.2 |
| Madhya Pradesh | 72313 | 10.9 | 7.9 | 9.4 |
| Maharashtra | 33957 | 15.9 | 9.1 | 12.5 |
| Manipur | 15342 | 20.4 | 11.4 | 15.9 |
| Meghalaya | 10347 | 10.4 | 9.9 | 10.2 |
| Mizoram | 13896 | 17.9 | 9.8 | 13.9 |
| Nagaland | 12230 | 23.1 | 16.0 | 19.6 |
| Odisha | 37930 | 12.5 | 9.0 | 10.8 |
| Punjab | 22511 | 21.8 | 13.2 | 17.5 |
| Pondicherry | 4618 | 15.1 | 9.1 | 12.1 |
| Rajasthan | 47857 | 12.4 | 6.9 | 9.7 |
| Sikkim | 6096 | 27.3 | 16.5 | 21.9 |
| Tamilnadu | 33614 | 15.5 | 8.3 | 11.9 |
| Telangana | 8625 | 18.2 | 10.1 | 14.2 |
| Tripura | 5623 | 13.6 | 12.6 | 13.1 |
| Uttarakhand | 19290 | 17.2 | 9.6 | 13.4 |
| Uttar Pradesh | 110600 | 10.1 | 7.6 | 8.9 |
| West Bengal | 20057 | 12.4 | 10.3 | 11.4 |
6. Hypertension as the most important risk factor
The GBD studies have estimated importance of various risk factors for disease incidence in India.51 Estimates in the GBD 2015 study reports that the following risk factors as important for disease burden and mortality (Table 5). Category 2 risk factors include groups of risk factors and shows that air pollution (ambient air pollution and indoor air pollution) and dietary risks (multiple dietary factors) are important. However, when we further sub-classify the risk factors into Category 3 or specific risk factors, elevated blood pressure is by far the most important risk factor.
Table 5.
Top ten Category 2 (broad categories) and Category 3 (specific factors) risk factors for disease burden (disability adjusted life years) and mortality in India: Global Burden of Disease Study 2015.
| Ranking | Category 2 risk factors | Category 3 risk factors |
|---|---|---|
| 1 | Air pollution | High blood pressure |
| 2 | Dietary risks | High fasting blood glucose |
| 3 | Child and maternal malnutrition | Ambient particulate matter |
| 4 | High systolic blood pressure | Household air pollution |
| 5 | High fasting blood glucose | Smoking |
| 6 | Unsafe water, sanitation | High total cholesterol |
| 7 | Tobacco smoke | Low whole grains intake |
| 8 | High total cholesterol | Low glomerular filtration |
| 9 | Alcohol and drug use | Unsafe water |
| 10 | High body mass index | Low fruit intake |
The study also shows that of the top ten Category 2 and 3 risk factors 7 are related to cardiovascular diseases. These risk factors are dietary risks (low whole grain, low fruit intake), high blood pressure, air pollution (ambient and household), high total cholesterol, high fasting glucose, tobacco, high body mass index, low glomerular filtration rate and low physical activity.
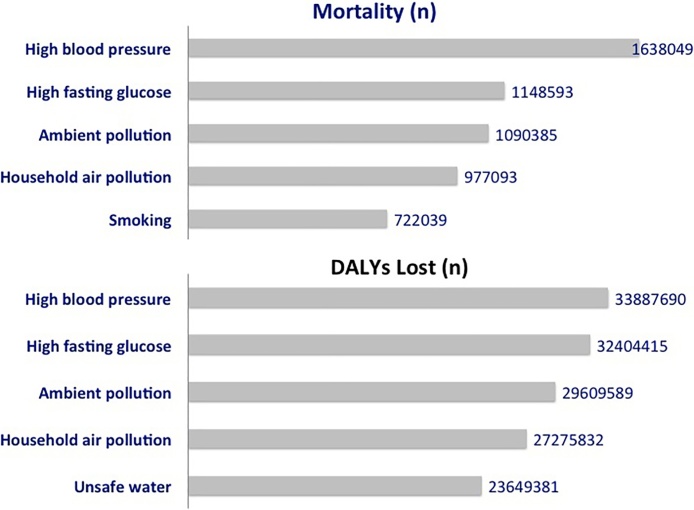
Association of top five Category 3 risk factors with total mortality and DALY’s is shown in Fig. 4. GBD Study estimates that high blood pressure caused 1,638,049 deaths and led to 33,887,690 DALY’s lost in India in 2015. These are more than any other risk factor including high fasting blood glucose, ambient particulate matter pollution, household air pollution and smoking (Fig. 4). Clearly, hypertension is not only the most important risk factor for non-communicable diseases but also from all disease conditions in India. Hypertension leads to mortality via its effects on cardiovascular mortality (1,428,819 deaths) as well as deaths related to diabetes, kidney failure and other endocrine diseases (209,230 deaths). On the other hand, high fasting glucose has been implicated in 529,568 cardiovascular deaths, 568,931 renal and endocrine deaths and 50,094 deaths due to chronic infections including tuberculosis and HIV/AIDS. Ambient air pollution, household pollution and smoking lead to deaths from respiratory, cardiovascular and acute and chronic infections.
Fig. 4.
Global Burden of Disease Study 2015 estimates for risk factors causing largest burden in India in terms of mortality (absolute numbers) and disability adjusted life years (DALYs) (numbers).
7. Promoting hypertension control in India
Hypertension is highly prevalent and endemic in India. Unfortunately, despite the high prevalence its awareness, treatment and control status is low in Indian urban as well as rural populations.12, 22 Poor awareness, treatment and control of high blood pressure has been attributed to a variety of socioeconomic factors- low educational status, poverty, rural residence, as well as physiological factors- obesity. Awareness status of hypertension has increased in the last 30 years in India but remains very low especially in rural populations.12 Hypertension awareness has increased from less than 30% in 1980′s among urban populations to about 60% presently and from less than 10% in rural areas in 1980′s to 30% presently, however, its treatment and control status remain low at less than 30% in urban and 10–15% in rural areas.22 The Jaipur Heart Watch study reported increasing hypertension awareness and treatment status over a 25-year period in urban men and women but the control status has remained poor at less than 30%.52 Similar low hypertension control rates have been reported from serial hypertension epidemiology studies at Vellore53 (South India) and Delhi54 (North India). In developed countries too, hypertension control rates have not increased substantially over the past 40 years and remain suboptimal at about 40%.55
Hypertension management and control is crucial to prevent its vascular complications.56 There is strong clinical trial and meta-analytical evidence that systolic blood pressure > 140 mmHg is harmful and prompt initiation and titration of therapy to achieve and maintain systolic blood pressure < 140 mmHg in all these patients is recommended.56 A meta-analysis reported that each 10 mmHg reduction of systolic blood pressure was associated with significantly lower risk of mortality, cardiovascular events, coronary heart disease, stroke, albuminuria and retinopathy in patients with hypertension.57 Strong evidence also exists from randomized clinical trials that systolic blood pressure < 130 mmHg and diastolic blood pressure < 90 mmHg is associated with decreased adverse vascular complications.58
Multiple strategies exist for better hypertension and control of hypertension in India as reported earlier.59 Relevant to public health are focus on social determinants of health, strengthening health systems, especially primary and secondary healthcare, empowering primary care physician for hypertension management, use of non-physician health workers in promoting adherence to therapies and evaluating control and patient empowerment.60, 61, 62 Unfortunately, little effort is directed at the health systems level and at the physician level.63, 64
There are a number of studies that are evaluating role of various healthcare innovations and technologies to improve hypertension awareness and control in India. Population level interventions for increasing awareness and control of hypertension and other cardiovascular risks have not been very successful in India.65 A study from Nepal (COBIN) reported usefulness of female community health workers in promoting adherence to anti-hypertensive therapy and reduction of systolic blood pressure in hypertension patients.66 Large studies in rural India are evaluating role of formal and informal community health workers in reducing population level BP.67, 68, 69 Technology based interventions are also in progress.70 A study from rural Tibet reported feasibility of a mobile technology-based platform and decision support system in reduction of cardiovascular risks.71
8. Conclusion
Our narrative review highlights data from Registrar General of India,5, 6 WHO,18, 19 GBD,20 and Indian GBD27 Studies showing that cardiovascular diseases are the most important causes of death and disability in the country. Age-adjusted mortality from these conditions has increased by 31% in last 25 years in contrast to declining mortality from these diseases in developed countries. Case-control studies have reported that hypertension is most important risk factor for CVD in India. GBD Study has estimated that hypertension led to 1.6 million deaths and 33.9 million disability-adjusted life years in 2015 and is most important cause of mortality as well as disease burden in India.51 Hypertension is widely prevalent in India with significant regional variations as reported by the NFHS-4 study (Table 4).50 Intensive public health effort is required to increase its awareness, treatment and control. Increasing hypertension treatment and control is important for achieving the WHO Global Monitoring Framework targets for delivering UN Sustainable Development Goals (SDG) in developing countries such as India. The SDG goal number 3 is focused on health and Section 3.4 has recommended reduction in non-communicable disease related mortality by one-third through prevention and treatment strategies.72 The Lancet Commission on Hypertension16 and World Heart Federation60 have provided a roadmap to achieve this goal. We believe that to achieve UN SDGs and WHO targets it would be important to focus on better hypertension control in India.59 Modelling studies have highlighted the importance of hypertension to achieve the 25 × 25 target of WHO.73 We estimate that proper control of hypertension in India can potentially prevent a quarter to a third of the 1.64 million hypertension attributable deaths in India thus preventing 400,000–500,000 deaths annually. This would also help the Indian policymakers achieve targets of the UN Sustainable Development Goals.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
Nil.
References
- 1.Yadav S.K., Aroikasamy P. Understanding epidemiological transition in India. Glob Health Action. 2014;7:23248. doi: 10.3402/gha.v7.23248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dreze J., Sen A. Penguin; 2012. An Uncertain Glory: India and Its Contradictions. [Google Scholar]
- 3.Reddy K.S., Patel V., Jha P., Paul V.K., Shivakumar A.K., Dandona L. for Lancet India Group for Universal Healthcare: towards achievement of universal health care in India. Lancet. 2011;377:760–768. doi: 10.1016/S0140-6736(10)61960-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel V., Chatterji S., Chisholm D. Chronic diseases and injuries in India. Lancet. 2011;377:413–428. doi: 10.1016/S0140-6736(10)61188-9. [DOI] [PubMed] [Google Scholar]
- 5.Registrar General of India . Registrar General of India, Ministry of Home Affairs; New Delhi: 2009. Report on Causes of Deaths in India 2001–2003. [Google Scholar]
- 6.Registrar General of India and Centre for Global Health Research . 2015. Causes of Death Statistics 2010–2013. [Available at: http://www.cghr.org/wordpress/wp-content/uploads/COD-India-Report-2010-2013-Dec-19-2015.pdf Accessed 31 August 2017. [Google Scholar]
- 7.Gupta R., Mohan I., Narula J. Trends in coronary heart disease epidemiology in India. Ann Glob Health. 2016;82:307–315. doi: 10.1016/j.aogh.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Joshi P., Islam S., Pais P. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 9.O’Donnell M., Chin S.L., Rangarajan S. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R., Joshi P.P., Mohan V., Reddy K.S., Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 11.Gupta R., Guptha S., Sharma K.K., Gupta A., Deedwania P.C. Regional variations in cardiovascular risk factors in India: India Heart Watch. World J Cardiol. 2012;4:112–120. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anchala R., Kannuri N.K., Pant H. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shrivastava U., Misra A., Mohan V., Unnikrishnan R., Bachani D. Obesity, diabetes and cardiovascular disease in India: public health challenges. Diabetes Res. 2017;13:65–80. doi: 10.2174/1573399812666160805153328. [DOI] [PubMed] [Google Scholar]
- 14.Unnikrishnan R., Anjana R.M., Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016;12:357–370. doi: 10.1038/nrendo.2016.53. [DOI] [PubMed] [Google Scholar]
- 15.Gupta R., Rao R.S., Misra A., Sharma S.K. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J. 2017;69:382–392. doi: 10.1016/j.ihj.2017.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olsen M.H., Angell S.Y., Asma S. A call to action and a life course strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on Hypertension. Lancet. 2016;388:2665–2712. doi: 10.1016/S0140-6736(16)31134-5. [DOI] [PubMed] [Google Scholar]
- 17.Sacco R.L., Roth G.A., Reddy K.S. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American Heart Association and World Heart Federation. Circulation. 2016;133:e674–690. doi: 10.1161/CIR.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization . World Health Organization; Geneva: 2014. Global Status Report on Non-Communicable Diseases. [Google Scholar]
- 19.World Health Organization . 2018. Country Level Mortality Data. [Available at: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed 15 July 2017] [Google Scholar]
- 20.Global Burden of Disease Study . 2015. Health Data. [Available at: http://ghdx.healthdata.org/gbd-data-tool. Accessed 15 July 2017] [Google Scholar]
- 21.Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004;18:73–78. doi: 10.1038/sj.jhh.1001633. [DOI] [PubMed] [Google Scholar]
- 22.Gupta R. Convergence in urban-rural prevalence of hypertension in India. J Hum Hypertens. 2016;30:79–82. doi: 10.1038/jhh.2015.48. [DOI] [PubMed] [Google Scholar]
- 23.Mahtani K.R., Jefferson T., Heneghan C. 2017. What Makes a Systematic Review Complex? BMJ Blogs. [Available at: http://blogs.bmj.com/bmj/2017/12/12/what-makes-a-systematic-review-complex/. Accessed 31 December 2017] [Google Scholar]
- 24.Gupta R., Misra A., Pais P., Rastogi P., Gupta V.P. Correlation of regional cardiovascular disease mortality in India with lifestyle and nutritional factors. Int J Cardiol. 2006;108:291–300. doi: 10.1016/j.ijcard.2005.05.044. [DOI] [PubMed] [Google Scholar]
- 25.Jha P., Gajalakshmi V., Gupta P.C. Prospective study of one million deaths in India: rationale, design and validation results. PLoS Med. 2006;3:e00018. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization . 2018. NCD Global Monitoring Framework. [Available at: http://www.who.int/nmh/global_monitoring_framework/en/ Accessed 14 March 2017] [Google Scholar]
- 27.India State-Level Disease Burden Collaborators Nations within a nation: variations in epidemiological transition across the states in India 1990–2016, in the Global Burden of Disease Study. Lancet. 2017;390:2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith J.N. Harper Collins; New York: 2015. Epic Measures: One Doctor Seven Billion Patients. [Google Scholar]
- 29.The World Bank . Oxford University Press & World Bank; New York: 1993. World Development Report 1993: Investing in Health. [Google Scholar]
- 30.Murray C.L., Lopez A.D. Global mortality, disability and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 31.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national levels of age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.GBD 2015 Mortality and Causes of Death Collaborators Global, regional and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis of the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.GBD 2016 Mortality and Causes of Death Collaborators Global, regional and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2016;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta R., Guptha S., Joshi R., Xavier D. Translating evidence into policy for cardiovascular disease control in India. Health Res Policy Syst. 2011;9:8. doi: 10.1186/1478-4505-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roth G.A., Johnson C., Abajobir A. Global, regional, and national cardiovascular disease prevalence, mortality, and disability-adjusted life-years for 10 causes of cardiovascular mortality, 1990 to 2015: A systematic analysis for the Global Burden of Disease Study. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrari Y.N. Harper Collins; New York: 2015. Sapiens A Brief History of Humankind. [Google Scholar]
- 38.Wells J.C.K., Nesse R.M., Sear R., Johnstone R.A., Stearns S. Evolutionary public health: introducing the concept. Lancet. 2017;390:500–509. doi: 10.1016/S0140-6736(17)30572-X. [DOI] [PubMed] [Google Scholar]
- 39.Gupta R., Gupta K.D. Coronary heart disease in low socioeconomic status subjects in India: an evolving epidemic. Indian Heart J. 2009;61:358–367. [PubMed] [Google Scholar]
- 40.Gupta R. Recent trends in hypertension epidemiology in India. In: Deb P.K., editor. CSI Textbook of Cardiology. Jaypee Brothers Medical Publishers; New Delhi: 2018. [Google Scholar]
- 41.Reddy K.S., Prabhakaran D., Chaturvedi V. Methods for establishing a system for cardiovascular diseases in Indian industrial populations. Bull WHO. 2006;84:461–469. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta R., Pandey R.M., Misra A. High prevalence and low hypertension awareness, treatment and control in Asian Indian women. J Hum Hypertens. 2012;26:585–593. doi: 10.1038/jhh.2011.79. [DOI] [PubMed] [Google Scholar]
- 43.Gupta R., Sharma K.K., Gupta B.K. Geographic epidemiology of cardiometabolic risk factors in urban middle-class residents in India: a cross sectional study. J Global Health. 2015;5:10411. doi: 10.7189/jogh.05.010411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shah B., Mathur P. Surveillance of cardiovascular risk factors in India: the need and the scope. Indian J Med Res. 2010;132:634–642. doi: 10.4103/0971-5916.73420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhansali A., Dhandhania V.K., Mohan D. Prevalence of and risk factors for hypertension in urban and rural India: the ICMR INDIAB study. J Hum Hypertens. 2015;29:204–209. doi: 10.1038/jhh.2014.57. [DOI] [PubMed] [Google Scholar]
- 46.Gupta R., Kaur M., Islam S. Association of household wealth, educational status and social capital with hypertension awareness, treatment and control in South Asia. Am J Hypertens. 2017;30:373–381. doi: 10.1093/ajh/hpw169. [DOI] [PubMed] [Google Scholar]
- 47.Kinra S., Bowen L.J., Lyngdoh T. Sociodemographic patterning of non-communicable disease risk factors in rural India: a cross sectional study. BMJ. 2010;341:c4974. doi: 10.1136/bmj.c4974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ram F., Paswan B., Singh S.K. National family health survey-4 (2015–16) Econ Pol Weekly. 2017;52(16):66–70. [Google Scholar]
- 49.Gaur K., Mohan I., Gupta R. Syndemic of obesity, hypertension and hyperglycemia among 15–49 year olds in Rajasthan: district-level data from National Family Health Survey-4. RUHS J Health Sci. 2017;2:54–64. [Google Scholar]
- 50.2017. National Family Health Survey. [Available at: http://rchiips.org/nfhs/abt.html Accessed 31 December 2017] [Google Scholar]
- 51.2015. Global Burden of Disease Study GBD Compare. [Available at: https://vizhub.healthdata.org/gbd-compare/. Accessed 2 September 2017] [Google Scholar]
- 52.Gupta R., Gupta V.P., Agrawal A., Sharma K.K., Prakash H., Deedwania P.C. 25-year trends in hypertension prevalence, awareness, treatment and control in an urban population in India. Indian Heart J. 2018 doi: 10.1016/j.ihj.2017.11.011. [EPub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oommen A.M., Abraham V.J., George K., Jose V.J. Rising trend of cardiovascular risk factors between 1991 and 1994 and 2010–2012: a repeat cross sectional survey in urban and rural Vellore. Indian Heart J. 2016;68:263–269. doi: 10.1016/j.ihj.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Praveen P.A., Amarchand R., Ramakrishnan L. Changes in hypertension prevalence, awareness, treatment and control rates over twenty years in National Capital Region of India. BMJ Open. 2017;7:e015639. doi: 10.1136/bmjopen-2016-015639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Glynn L.G., McManus R.J. Blood pressure control: missed opportunity or potential holy grail? Ann Intern Med. 2017 doi: 10.7326/M17-3036. [EPub.] [DOI] [PubMed] [Google Scholar]
- 56.WHO Expert Committee . Vol. 862. 1996. pp. 2–10. (Hypertension Control WHO Technical Report Series). [Google Scholar]
- 57.Turnbull F. Blood pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood pressure lowering regimens on major cardiovascular events: results of prospectively designed overviews of randomized trials. Lancet. 2003;362:1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 58.Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation and management of high blood pressure in adults: executive summary: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017 doi: 10.1161/HYP.0000000000000066. [EPub] [DOI] [PubMed] [Google Scholar]
- 59.Gupta R., Yusuf S. Towards better hypertension control in India. Indian J Med Res. 2014;139:657–660. [PMC free article] [PubMed] [Google Scholar]
- 60.Adler A.J., Prabhakaran D., Bovet P. Reducing cardiovascular mortality through prevention and management of raised blood pressure: a World Heart Federation roadmap. Glob Heart. 2015;10:111–122. doi: 10.1016/j.gheart.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 61.Angell S., De Cock M., Frieden T.R. A public health approach to global management of hypertension. Lancet. 2015;385:825–827. doi: 10.1016/S0140-6736(14)62256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gupta R., Khedar R.S., Panwar R.B. Strategies for better hypertension control in India and other lower-middle income countries. J Assoc Phys India. 2016;64(9):58–64. [PubMed] [Google Scholar]
- 63.Patel V., Parikh R., Nandraj S. Assuring health coverage for all in India. Lancet. 2015;389:2422–2435. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed] [Google Scholar]
- 64.Lakhanpaul M., Narula S., Patel V., Piot P., Venkatapuram S. Accounting for the future of health in India. Lancet. 2017;389:680–682. doi: 10.1016/S0140-6736(17)30324-0. [DOI] [PubMed] [Google Scholar]
- 65.Pandey R.M., Agrawal A., Misra A. Population-based intervention for cardiovascular disease related knowledge and behaviours in Asian Indian women. Indian Heart J. 2013;65:40–47. doi: 10.1016/j.ihj.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Neupane D., McLachlan C.S., Mishra S.R. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open-label, cluster-randomized trial. Lancet Glob Health. 2018;6:e66–73. doi: 10.1016/S2214-109X(17)30411-4. [DOI] [PubMed] [Google Scholar]
- 67.Fathima F.N., Joshi R., Agrawal T. Rationale and design of the primary prevention strategies at the community level to promote adherence of treatments to prevent cardiovascular diseases (PREPARE) trial. Am Heart J. 2013;166:4–12. doi: 10.1016/j.ahj.2013.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jeemon P., Narayanan G., Kondal D. Task shifting of frontline community heart workers for cardiovascular risk reduction: design and rartionale of a cluster randomized controlled trial (the DISHA study) in India. BMC Pub Health. 2016;16:264. doi: 10.1186/s12889-016-2891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jeemon P., Harikrishnan S., Sanjay G. A program of lifestyle intervention in families for cardiovascular risk reduction (PROLIFIC study): design and rationale of a family based randomized controlled trial in individuals with family history of premature coronary heart disease. BMC Pub Health. 2017;17:10. doi: 10.1186/s12889-016-3928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ajay V.S., Jindal D., Roy A. Development of a smartphone-enabled hypertension and diabetes mellitus management package to facilitate evidence-based care delivery in primary healthcare facilities in India: themPower Heart Project. J Am Heart Assoc. 2016;5:e004343. doi: 10.1161/JAHA.116.004343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tian M., Ajay V.S., Dunzhu D. A cluster-randomized controlled trial of a simplified multifaceted management program for individuals at high cardiovascular risk (SimCard Trial) in rural Tibet, China and Haryana, India. Circulation. 2015;132:815–824. doi: 10.1161/CIRCULATIONAHA.115.015373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.2017. United Nations Sustainable Development Goals. [Available at: http://www.un.org/pga/wp-content/uploads/sites/3/2015/08/120815_outcome-document-of-Summit-for-adoption-of-the-post-2015-development-agenda.pdf. Accessed 17 March 2017] [Google Scholar]
- 73.Kontis V., Mathers C.D., Rehm J. Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modeling study. Lancet. 2014;384:427–437. doi: 10.1016/S0140-6736(14)60616-4. [DOI] [PubMed] [Google Scholar]