Abstract
Patients with prehypertension suffer endothelial dysfunction and are at increased cardiovascular risk. Ankle-brachial index (ABI) constitutes an efficient tool for diagnosing peripheral arterial disease; but also an ABI < 0.9 is an independent and positive predictor of endothelial dysfunction and is associated with increased cardiovascular risk and mortality.
The aim
of this study was testing whether ABI was decreased in prehypertensive patients when compared with normotensive subjects.
Methods
We included 70 prehypertensive patients older than 19 years, in whom the ABI was registered with a 5 megahertz Doppler (Summit Doppler L250, Life Dop., USA). The highest ankle systolic pressure was divided by the highest brachial systolic pressure. We also included 70 normotensive subjects in whom the ABI was registered in the same way. The measurements were performed by the same physician who was blinded about the study.
Statistical analysis was performed with odds ratio and student t-test.
Results
The ABI values in normotensive subjects were 1.023 ± 0.21, whereas prehypertensive patients significantly had lower ABI (0.90 ± 0.14p = 0.00012).
We found ABI <0.9 in 30 prehypertensive patients (42.85%) and 13 normotensive patients (18.5%). The odds ratio of ABI <0.90 in prehypertensive patients was 3.288 (IC95 1.5–7.0, p = 0.0023).
A regression analysis failed to show any independent association between ABI values and any other clinical parameter.
Conclusions
Prehypertensive patients had lower ABI and higher prevalence of peripheral artery disease when compared with normotensive subjects; this fact increases their cardiovascular risk. ABI must be included in global evaluation of prehypertensive subjects.
Keywords: Prehypertension, Ankle-brachial index, Peripheral artery disease, Atherosclerosis, Cardiovascular risk
1. Introduction
Prehypertension, which was defined as the presence of systolic blood pressure (BP) between 120 mmHg to 139 mmHg and/or a diastolic BP between 80 mmHg and 89 mmHg by “the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)”; has a prevalence of 26.5% in Mexico.1, 2
Usually being asymptomatic, peripheral arterial disease (PAD) is an underdiagnosed disease that affects 23.8% of Mexicans over 55 years old.3 Moreover, PAD is rarely an isolated condition; it is also an indicator of generalized atherosclerosis. Indeed patients with PAD have an increased risk of coronary artery disease and/or cerebrovascular disease.4
Ankle-brachial index (ABI) is the ratio of the ankle and brachial systolic pressure; it is a non-invasive, low-cost, quick, office measurement method for diagnosing PAD. In fact, an ABI < 0.9 has high sensibility (91%–95%) and specificity (85%–100%) to diagnose lower extremity atherosclerosis.3, 4
Furthermore, a low ABI could be considered as a marker of end organ damage and a predictor of cardiovascular and cerebrovascular disease. Patients with an ABI < 0.9 significantly have a reduced survival compared with those with normal ABI. According to the evidence, there is an increase of 10.2% in the relative risk of cardiovascular events and mortality by every 0.1 of reduction in the ABI.5 A very high ABI (>1.40) is related to stiffness of arteries, and also is associated with increases in mortality.6
The aim of this study was to test whether ABI was decreased in prehypertensive patients when compared with normotensive subjects.
2. Methods
We evaluated 70 prehypertensive patients older than 19 years, statin-naive and without previous antihypertensive drug therapy. Blood pressure was recorded in triplicate with a mercurial sphygmomanometer (Tycos, Rochester, New York, USA), in the sitting position after a 5-min rest and at 5-min intervals; an average of the three measurements was recorded, the personnel measuring each patient’s BP was blinded to the study.
In all of them, the ABI was registered with a 5 megahertz Doppler (Summit doppler L250, Life Dop., USA). We also included 70 normotensive subjects in whom the ABI was registered in the same way. The measurements were performed by the same physician who was blinded about the study.
Measurement of ABI was performed by placing the patient in the supine position, with the arms and legs at the same level as the heart, for a minimum of 10 min before register. The systolic blood pressures was registered in right and left posterior tibial arteries and right and left brachial arteries respectively. The register was done by using a standard mercury sphygmomanometer and a hand-held validated Doppler instrument (5 MHz, Summit Doppler L250, Life Dop., EUA). The higher ankle systolic pressure was divided by the higher brachial systolic pressure.4, 7 All registers were performed in the morning, between 8:00 and 10:00 h, on fast, by personnel blinded to the study. Readings were taken only one day per patient.
Additionally, there were measured serum glucose (glucose oxidase, Beckman Coulter, Brea. CA, USA), creatinine (JAFFE, Beckman Coulter, Brea. CA, USA), lipid profile (CHOD-PAP, Beckman Coulter, Brea. CA, USA) and triglycerides (triglyceride-pap, Beckman Coulter, Brea. CA, USA) using a UniCel Dace 600 Synchron Clinical Systems (Beckman Coulter, Brea. CA, USA) automatic equipment, in all subjects. All venous samples were collected in the morning, after 12 h overnight fast.
Patients with any of the following diagnoses were excluded from the study: decompensated diabetes mellitus (glucose ≥ 250 mg/ml), heart, hepatic, or renal failure, evidence of valvular heart disease, heart block or cardiac arrhythmia, acute coronary syndrome or cerebrovascular disease six months before the baseline of the study. There also were excluded subjects with autoimmune disease, pregnancy and alcohol or psychotropic drugs abuse.
The study was conducted with the approval of the Research and Ethics Committee of our hospital, in accordance with the Helsinki declaration. The register number is 208/010/017/16. Participants gave written informed consent before their inclusion in the study protocol.
Statistical analysis was performed with odds ratio and student-t test. A p < 0.05 was considered as statistically significant.
A regression analysis was performed to asses if the difference in ABI values is independent of variables that have a significantly difference between groups.
3. Results
The basal characteristics of the patients and controls are shown in Table 1; briefly, prehypertensive patients were older than normotensive subjects.
Table 1.
Basal characteristics of the patients.
| Prehypertensive | Normotensive | P | |
|---|---|---|---|
| Gender (M/F) | 21/49 | 20/50 | NS |
| Age (years) | 35.9 ± 6.3 | 32.1 ± 5.3 | 0.01 |
| Body Mass Index | 30.2 ± 6 | 29.5 ± 4 | 0.12 |
| Blood Pressure (mm Hg) | 128 ± 5.3 /80 ± 4.8 |
102 ± 5.3 /66 ± 4 |
0.0001 |
| Glucose (mmol/L) | 5 ± 0.51 | 5.16 ± 0.39 | 0.33 |
| Creatinine (μmol/L) | 90.17 ± 8.3 | 83.3 ± 9.72 | 0.20 |
| Low density lipoprotein (mmol/L) |
2.80 ± 0.19 | 2.72 ± 0.10 | 0.92 |
| High density lipoprotein (mmol/L) | 0.88 ± 0.20 | 0.91 ± 0.20 | 0.45 |
| Triglycerides (mmol/L) | 2.8 ± 0.72 | 2.83 ± 1.1 | 0.19 |
The difference between groups was calculated with student t-test
The blood pressure range (minimum and maximum) observed for prehypertensive group was 122/82–138/88 mmHg, and for subjects with normal blood pressure was 92/56 to 112/80 mmHg.
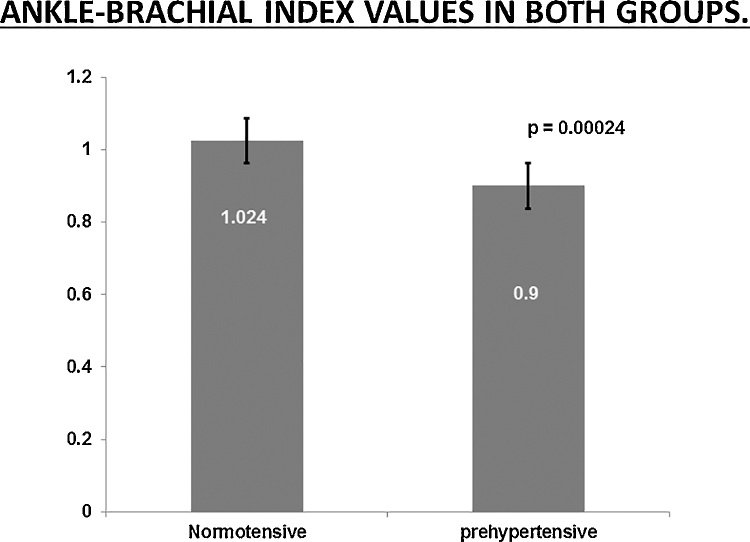
The ABI values in normotensive subjects was 1.024 ± 0.21, whereas in prehypertensive patients was 0.90 ± 0.14. When both groups were compared with student-t test, the prehypertension group had a significantly lower ABI than normotensive subjects (p = 0.00012, Fig. 1).
Fig. 1.
Ankle-brachial index values in both groups.
We found PAD (defined as an ABI < 0.9), in 30 prehypertensive patients (42.85%), and 13 normotensive subjects (18.5%). However, no patient complains of associated symptoms.
The odds ratio for an ABI < 0.90 in prehypertensive patients was 3.28 (IC95 1.5–7.0, p = 0.0023).
A regression analysis failed to show any independent association between ABI values and any other clinical parameter.
4. Discusion
A higher prevalence of PAD in prehypertensive subjects was found in this study. At the same time it was observed a lower ABI when compared with normotensive subjects. It is important to underline the fact that the ABI was measured by the same physician who was unaware of the study. Observer variation was taken into account when statistical analysis was performed. Unexpectedly, the prevalence of peripheral artery disease was higher in prehypertensive patients in our study than previous reports of Mexican people >55 years.3 Al this time we do not have an explanation for that, this item requires further research.
None of our patients complains of associated symptoms; This is an expected finding since patients with PAD are usually asymptomatic.3, 8
Previously, Korhonen et al demonstrated that hypertensive patients had lower ABI than normotensive patients9; and that those patients with resistant or uncontrolled hypertension had lower ABI values than hypertensive patients with controlled hypertension.10 Hypertensive patients have higher prevalence of PAD too, which is not only a disease of peripheral arteries, but also a marker of systemic atherosclerosis.4 Our results are in accordance with those results, with lower ABI values in patients with prehypertension when compared with normotensive subjects.
The ABI is a useful diagnostic tool for PAD, but also is a marker of generalized atherosclerosis and arterial stiffness.4, 8
A low ABI is an independent predictor of future cardiovascular events, and the risk increases with the reduction of ABI values even in absence of other cardiovascular risk factors, and in patients without PAD; then, the ABI measurement provides additional information for the stratification of cardiovascular risk. A low ABI leads to a high cardiovascular risk with a different therapeutic approach.8, 11
Thus, the measurement of ABI should be performed when an evaluation of global cardiovascular risk and detection of organ damage is required.
Patients with prehypertension have increased carotid intima-media thickness, greater left ventricle hypertrophy and more development of diastolic dysfunction when compared with normotensive subjects,12, 13 those patients also have greater incidence of myocardial infarction, stroke and cardiovascular death.11 Since a low ABI predicts high cardiovascular risk, our results supports the evidence that prehypertensive patients are a high cardiovascular risk group. Our results differ of those from Nikolov et al, they did not found difference in ABI measurement between 103 prehypertensive and 45 normotensive subjects14; whereas we found a significantly lower ABI in prehypertensive patients when compared with those with normal blood pressure.
Although in our study the prehypertensive patients shown significantly higher mean age than normotensive subjects, the regression analysis did not show an independent association between ABI values and age, perhaps, the 3 years difference was not enough for the development of PAD.
Chronic hypertension and prehypertension both lead to remodeling of large arteries and arterial stiffness, which is a contributing factor for myocardial infarction and cardiovascular mortality,15 this fact, explains why prehypertensive patients have more cardiovascular risk and mortality than normotensive subjects, and explain our findings. Indeed, the prevalence of PAD in normotensive subjects in our study is higher than the prevalence described in other reports8; an explication may be the low HDL and high body mass index and triglycerides found in those subjects, all those facts may lead to arterial damage.
The 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension16 identify as high-risk subjects with blood pressure values in the prehypertensive range and organ damage, these guidelines identify a low ABI as a marker of organ damage.
Although there is no evidence that antihypertensive drug treatment of prehypertensive patients reduces cardiovascular mortality,12 and prehypertension was not addressed in the Eighth Report of the Joint National Committee (JNC 8), our findings have therapeutic implications regarding global cardiovascular risk management17; antihypertensive treatment in prehypertensive patients with CVD (or evidence of atherosclerosis in any territory) significantly reduces the incidence of stroke, myocardial infarction, heart failure, and cardiovascular and all-cause mortality.17 Then, patients with prehypertension and a low ABI should receive antihypertensive medication.
Both, the ESC Guidelines on the diagnosis and treatment of peripheral artery diseases,8 and the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults,18 recommend the use of statins in subjects with peripheral arterial disease presumed to be of atherosclerotic origin. Those recommendations lead to consider statin treatment in prehypertensive patients with a low ABI.
According with the two paragraphs above, prehypertensive subjects with a low ABI require drug interventions to reduce their cardiovascular risk.
The main limitation of this work is that our sample is small, and we performed an observational and transversal study, and no follow-up was made.
5. Conclusions
Prehypertensive patients have a lower ABI than normotensive patients in Mexico, and a higher prevalence of PAD.
The measurement of the ABI must be part of the evaluation of prehypertensive patients.
Conflict-of-interest statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors
Author contributions
AFRG, JJLN, MBDS contributed equally to this work; AKGA, KCAP, HML participated in the acquisition, analysis, and interpretation of the data, and drafted the initial manuscript; All authors revised the article critically for important intellectual content, and approved this final version.
References
- 1.The seventh report of the joint national committee on detection, evaluation, and treatment of high blood pressure. JNC 7. Complete version. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.Guzmán-Guzmán I.P., Salgado-Goytia L., Muñoz-Valle J.F. Prehypertension in a Mexican population: influence of age, gender, and body fat. Clin Exp Hypertens. 2013;35:67–73. doi: 10.3109/10641963.2012.690470. [DOI] [PubMed] [Google Scholar]
- 3.Cantú-Brito C., Chiquete E., Duarte-Vega M. Ankle-brachial index assessed in a Mexican population with vascular risk. The INDAGA study. Rev Med Inst Mex Seguro Soc. 2011;49(3):239–246. [PubMed] [Google Scholar]
- 4.Paraskevas K.I., Mukherjee D., Whayne T.F., Jr. Peripheral arterial disease: implications beyond the peripheral circulation. Angiology. 2013;64:569–571. doi: 10.1177/0003319712466730. [DOI] [PubMed] [Google Scholar]
- 5.Rubio-Guerra A.F. Clinical forum: hypertension in patients with peripheral arterial disease. Rev Invest Clin. 2013;65:263–368. [PubMed] [Google Scholar]
- 6.Ko S.H., Bandyk D.F. Interpretation and significance of ankle-brachial systolic pressure index. Semin Vasc Surg. 2013;26(June-September (2–3)):86–94. doi: 10.1053/j.semvascsurg.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Greenland P., Abrams J., Aurigemma G.P. Prevention Conference V. Beyond secondary prevention: identifying the high-risk patient for primary prevention. Noninvasive tests of atherosclerotic burden. Circulation. 2000;101(1):E16–E22. doi: 10.1161/01.cir.101.1.e16. [DOI] [PubMed] [Google Scholar]
- 8.Aboyans V., Ricco J.B., Bartelink M.E.L. ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Endorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2017;(Aug 26) doi: 10.1093/eurheartj/ehx095. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Korhonen P.E., Syvänen K.T., Vesalainen R.K. Ankle-brachial index is lower in hypertensive than in normotensive individuals in a cardiovascular risk population. J Hypertens. 2009;27:2036–2043. doi: 10.1097/HJH.0b013e32832f4f54. [DOI] [PubMed] [Google Scholar]
- 10.Korhonen P.E., Kautiainen H., Kantola I. Patients with resistant hypertension have more peripheral arterial disease than other uncontrolled hypertensives. J Hum Hypertens. 2015;29:46–49. doi: 10.1038/jhh.2014.65. [DOI] [PubMed] [Google Scholar]
- 11.Giugliano G., Sannino A., Brevetti L. Ankle/brachial index to everyone. BMC Surg. 2012;12(Suppl. 1):S18. doi: 10.1186/1471-2482-12-S1-S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pimenta E., Oparil S. Prehypertension: epidemiology, consequences and treatment. Nat Rev Nephrol. 2010;6:21–30. doi: 10.1038/nrneph.2009.191. [DOI] [PubMed] [Google Scholar]
- 13.Ueda H., Kiyosaki M., Hiraoka H. High-normal blood pressure is associated with new-onset electrocardiographic left ventricular hypertrophy. J Hum Hypertens. 2015;29:9–13. doi: 10.1038/jhh.2014.21. [DOI] [PubMed] [Google Scholar]
- 14.Nikolov P., Nikolov J., Deneva T., Nikolov F. Changes in intima-media thickness, ankle-brachial index and flow mediated dilation in pre-hypertensive individuals. Scripta Scientifica Medica. 2015;47:15–20. [Google Scholar]
- 15.Laurent S., Boutouyrie P., Asmar R. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236–1241. doi: 10.1161/01.hyp.37.5.1236. [DOI] [PubMed] [Google Scholar]
- 16.Task Force for the management of arterial hypertension of the European Society of Hypertension; Task Force for the management of arterial hypertension of the European Society of Cardiology. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension. Blood Press. 2013;22:193–278. doi: 10.3109/08037051.2013.812549. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs F.D., de Mello R.B., Fuchs S.C. Preventing the progression of prehypertension to hypertension: role of antihypertensives. Curr Hypertens Rep. 2015;17:505. doi: 10.1007/s11906-014-0505-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]