Abstract
Objectives
This study determined whether greater 2-year declines in Walking Impairment Questionnaire (WIQ) stair climbing, distance, or speed scores were associated with higher all-cause and cardiovascular disease (CVD) mortality among men and women with lower extremity peripheral artery disease (PAD).
Background
Associations of decline in the WIQ with mortality among people with PAD are unknown.
Methods
Participants were 442 men and women with PAD identified from Chicago area medical centers. The WIQ was completed at baseline and at 2-year follow-up. Cox proportional hazard models were used to assess associations across categories of 2-year changes in WIQ stair climbing, WIQ distance, and WIQ speed scores with subsequent all-cause and CVD mortality, adjusting for age, sex, race, ankle-brachial index, body mass index, smoking, comorbidities, and other covariates.
Results
One hundred twenty-three participants (27.8%) died during a median follow-up of 4.7 years after the 2-year change in WIQ score measurements. Forty-five participants died from CVD. Adjusting for covariates, participants with WIQ score declines ≥20.0 points had higher all-cause mortality (hazard ratio [HR]: 1.93, 95% confidence interval [CI]: 1.01 to 3.68 for WIQ stair climbing; HR: 2.34, 95% CI: 1.15 to 4.75 for WIQ distance; and HR: 3.55, 95% CI: 1.57 to 8.04 for WIQ speed, respectively) compared with participants with ≥20.0 point improvement in each of the corresponding WIQ categories. Participants with ≥20.0 point declines in the WIQ distance score had higher CVD mortality (HR: 4.56, 95% CI: 1.30 to 16.01) compared with those with ≥20.0 point improvement in the WIQ distance score.
Conclusions
Patients with PAD who experienced ≥20.0 point declines in the WIQ stair climbing, distance, and speed scores had a higher rate of all-cause mortality compared with those with less declines in each WIQ score. (J Am Coll Cardiol 2013;61:1820–9) © 2013 by the American College of Cardiology Foundation
Keywords: functional limitation, intermittent claudication, mortality, peripheral artery disease
Lower extremity peripheral artery disease (PAD) affects more than 8 million Americans (1). Compared with those without PAD, people with PAD are at higher risk for all-cause and cardiovascular mortality (2). The Walking Impairment Questionnaire (WIQ) is a PAD-specific, self-administered questionnaire that measures patient-perceived difficulty climbing stairs and walking specific distances and speeds (3). We previously reported that lower baseline values for the WIQ stair climbing scores were associated with higher all-cause and cardiovascular disease (CVD) mortality in PAD (4). In the present study, we assessed whether greater declines in WIQ stair climbing, distance, and speed scores are associated with higher all-cause and CVD mortality among patients with PAD. We measured 2-year change in the WIQ scores because assessing change over 2 years allowed greater opportunity to identify a significant decline in the WIQ, and because patients with PAD are commonly followed longitudinally in clinical practice for 2 years or more. We hypothesized that greater declines in each WIQ score would be associated with higher all-cause and CVD mortality. In exploratory analyses, we assessed whether significant associations of decline in WIQ scores with higher mortality were attenuated by adjustment for progression of PAD and other CVD.
Methods
Participant identification.
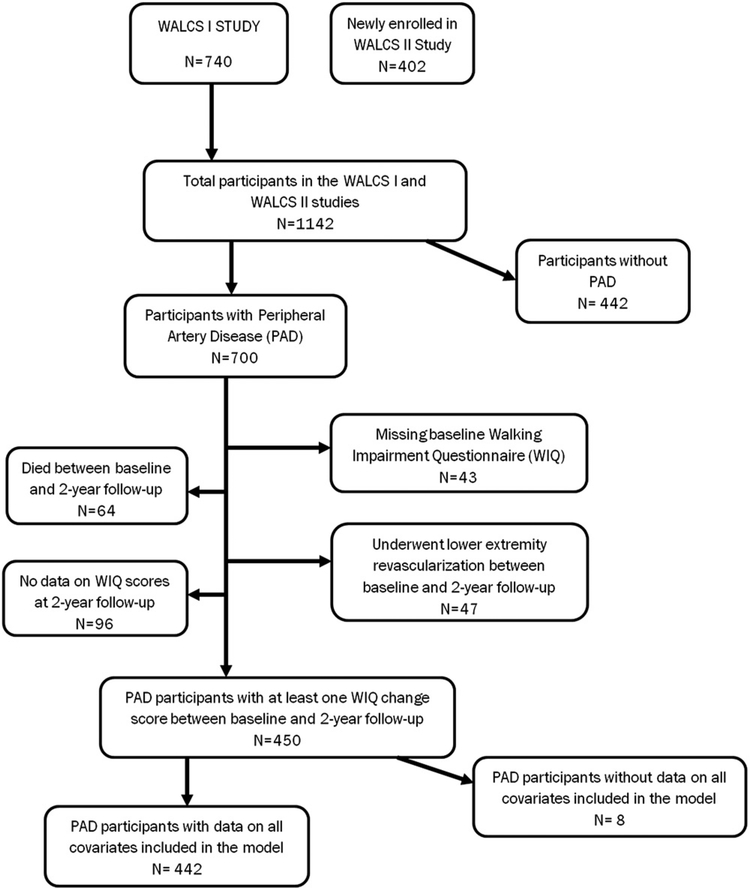
Participants for this analysis were identified from the WALCS (Walking and Leg Circulation Study) and WALCS II studies (Fig. 1). The WALCS and WALCS II are prospective, observational studies designed to identify clinical characteristics associated with functional impairment, functional decline, and mortality in PAD (5,6). The WALCS cohort of 460 participants was assembled from October 1998 to March 2000. The WALCS II cohort of 489 participants with PAD was assembled from November 2002 to April 2004. WALCS II included WALCS participants who consented to participation in WALCS II as well as newly identified participants (Fig. 1). WALCS participants were followed for up to 8 years, whereas newly identified participants for WALCS II were followed for up to 4 years. WALCS participants were ages 55 years and older at the time of enrollment. PAD participants newly identified for WALCS II 4 years later were ages 59 years and older at enrollment. For both WALCS and WALCS II, PAD participants were identified consecutively from among patients diagnosed with PAD in 3 Chicago area noninvasive vascular laboratories. This method ensured a systematic method of enrollment and minimized bias. We did not collect data on the duration of the PAD diagnosis. Onset of PAD is difficult to ascertain accurately because PAD is frequently asymptomatic (5). The institutional review boards of Northwestern University and collaborating sites approved the study protocol. Written informed consent was obtained from all participants.
Figure 1. PAD Participants Eligible for Analyses.
The cohort composition based on eligibility and data availability for peripheral arterial disease (PAD) participants in the Walking and Leg Circulation Study (WALCS) and WALCS II studies. WIQ = Walking Impairment Questionnaire.
Exclusion criteria.
We excluded participants with an ankle-brachial index (ABI) >0.90 at baseline because they either did not have PAD or because they had noncompressible arteries, which did not allow accurate assessment of PAD severity. At enrollment for WALCS and WALCS II, participants with above- or below-knee amputations or ulcers, nursing home residents, and wheelchair-bound patients were excluded due to severely limited functional capacity at baseline. We did not systematically exclude participants with critical limb ischemia. Non-English-speaking participants were excluded because data collection forms, including the WIQs, were prepared only in English. At baseline, participants with recent major surgery and self-identified or physician-identified dementia, as well as those unlikely to return for 12-month follow-up because of medical illness or logistical issues were excluded.
Walking Impairment Questionnaire.
Participants completed the WIQ at baseline and at 2-year follow-up. In the WIQ distance score, the participant records the degree of difficulty walking specific distances (ranging from walking indoors to 1,500 feet or 5 blocks) on a graded scale from 0 to 4 (3). A score of 0 represents the inability to walk the distance in question and a score of 4 represents no difficulty. In the WIQ speed score, the participant is asked to assess the degree of difficulty walking 1 block at specific speeds ranging from walking slowly to jogging on a graded scale ranging from 0 to 4 (3). In the WIQ stair climbing score, the participant reports the degree of difficulty climbing 1, 2, and 3 flights of stairs. This graded score is multiplied by a pre-specified weight for each distance, speed, or number of stair flights. The products are summed and divided by the maximum possible score to obtain a percent score, ranging from 0 (representing the inability to perform any of the tasks) to 100 (representing no difficult with any of the tasks) (7). The WIQ scores have been shown to improve in response to lower extremity revascularization (8) and supervised exercise therapy (9).
Ankle-brachial index measurement.
Using a handheld Doppler probe (Nicolet Vascular Pocket Dop II, Nicolet Biomedical, Golden, Colorado), systolic pressures were measured in the right and left brachial, posterior tibial, and dorsalis pedis arteries, and then again in reverse order. The ABI was calculated by dividing the mean of the posterior tibial and dorsalis pedis pressures in each leg by the mean of the 4 brachial pressures (10). Average brachial pressures in the arm with highest pressure were used when 1 brachial pressure was higher than the opposite brachial pressure in both measurement sets and the 2 brachial pressures differed by 10 mm Hg or more in at least 1 measurement set, because subclavian stenosis was possible in such cases (11). The lowest leg ABI was used in analyses.
Comorbidities.
At baseline, we measured presence of comorbidities that could potentially influence both the WIQ scores and mortality: history of congestive heart failure, angina, myocardial infarction (MI), stroke, diabetes, cancer, and chronic pulmonary disease. Verification of comorbidities was performed using algorithms developed for the Women’s Health and Aging Study (12), which combines data from medical record review, medications, patient self-report, selected laboratory values, and a questionnaire completed by the participant’s primary care provider. We used similar methods to identify new stroke, MI, and angina that were diagnosed after baseline.
Physical activity.
At baseline, participant-reported physical activity was measured with a questionnaire derived from the Harvard Alumni Activity Study that has been validated in participants with PAD (13). Participants were asked the following question: “During the last week, how many city blocks or their equivalent did you walk? Let 12 city blocks equal 1 mile.”
Other measures.
At baseline, height and weight were measured, and body mass index (BMI) was calculated. Cigarette smoking history was self-reported. Participants brought in their medication bottles or a list of medications to their baseline study visit. A study investigator (M.M.M.), blinded to other patient characteristics, identified use of angiotensin-converting enzyme (ACE) inhibitor medications or statins from the list of participant medications.
Death.
Information on deaths was obtained from proxies, the Social Security Administration death database, and primary care providers. Death certificate information from the state in which the death occurred, family members, or from the participants’ medical records was also obtained. Deaths from CVD were those with International Classification of Diseases-10th Revision codes in the range I00.0 through I99. This included deaths due to stroke, peripheral vascular disease, coronary heart disease, heart failure, and sudden cardiac death. A certified nosologist, blinded to participant characteristics, adjudicated cause of death based on the death certificate.
Statistical analyses.
Change in each WIQ score (stair climbing, distance, and speed score) was calculated as the difference between the 2-year follow-up WIQ score and the corresponding baseline WIQ domain score. Participants were excluded from analyses if they died or underwent lower extremity arterial revascularization before 2-year follow-up, or if their WIQ score data were missing at either visit (Fig. 1).
For each WIQ score domain, baseline characteristics of participants across 5 categories of WIQ score change were compared using linear models for continuous variables and logistic models for categorical variables. We defined 5 categories of WIQ score change in an a priori fashion after examining the distribution of change in each WIQ score between baseline and 2-year follow-up. We aimed to define categories that resulted in relatively similar numbers of participants in each category and also represented increments of 5-point change that could be more easily remembered by clinicians. In addition, the 5 categories were defined because they resulted in a nearly symmetric distribution of WIQ change scores. Category 1 consisted of participants whose WIQ score declined by ≥20.0 points (worst). Category 2 consisted of participants whose WIQ score declined by <20.0 points and >5.0 points. Category 3 included participants whose WIQ score declined by ≤5.0 points, but did not increase by >5.0 points. Category 4 included participants whose WIQ score increased by >5.0 points and <20.0 points, and Category 5 included participants whose WIQ score increased by >20.0 points (best). Cox proportional hazards analyses were used to compare differences in all-cause and CVD mortality across categories of 2-year WIQ score change, with Category 5 (best) for each WIQ domain used as the reference. Pairwise p values were calculated between the lower 4 (worst) categories and highest (best) category. Overall p for trend was also calculated. Analyses adjusted for baseline age, sex, race, ABI, BMI, current smoking, comorbidities, ACE inhibitor use, study cohort (WALCS vs. WALCS II), statin use, baseline WIQ score, and physical activity. We also assessed the association of the mean change in all 3 WIQ scores combined with all-cause and CVD mortality.
To assess whether the progression of systemic CVD mediated associations of 2-year decline in WIQ domain scores with mortality, additional exploratory analyses were performed, which added adjustment for change in ABI, incident stroke, incident MI, and incident angina from baseline to 2-year follow-up.
In additional analyses, we used Cox proportional hazards analyses to determine whether greater 2-year decline in WIQ scores was associated with greater 2-year decline in the ABI, adjusting for age, sex, race, BMI, baseline ABI, smoking, physical activity, comorbidities, medication use, baseline WIQ score, and study cohort. We also performed multivariable logistic regression analyses to identify clinical characteristics associated with Category 1 (i.e., decline in WIQ of >20 points). Finally, we calculated the degree to which the addition of each WIQ change score to a statistical model of traditional mortality risk factors in PAD improved the model’s predictive ability for mortality.
Results
Baseline characteristics.
Of 1,142 participants who completed baseline testing for WALCS and WALCS II, 700 had PAD (Fig. 1). Of these, 64 who died and 43 who underwent lower extremity revascularization between baseline and 2-year follow-up were excluded. Ninety-six PAD participants missing WIQ score data at 2-year follow-up and 8 participants missing covariate data were excluded, leaving 442 participants available for analyses. Of 442 participants included in the analyses, 123 (27.8%) participants died during a median follow-up of 56.5 months (interquartile range: 27.1 to 74.9 months) after the 2-year change in WIQ scores was assessed. Of these, 45 deaths (36.6%) were attributed to CVD. The cause of death was unknown in 11 decedents. Median follow-up for CVD mortality was 44.7 months (interquartile range: 24.9 to 73.0 months).
Table 1 lists the baseline characteristics of participants according to the degree of change in each WIQ domain score. The lowest (worst) category for 2-year change in WIQ stair climbing score was associated with older age. The lowest (worst) category for 2-year change in WIQ distance score was associated with higher physical activity at baseline. Mean 2-year changes in WIQ stair climbing, distance, and speed scores were —0.79, —1.78, and —1.55, respectively.
Table 1.
Baseline characteristics of Peripheral Arterial Disease Participants According to 2-Year Change in WIQ Score by Categories of Change (n = 442)
|
Change in WIQ Stair Climbing Score | ||||||
| Category1 Decline ≥20.0 Points (n = 84) | Category 2 Decline 20.0–5.0 Points (n = 78) | Category 3 Decline <5.0 and Increase <5.0 Points (n = 130) | Category 4 Increase 5.0–20.0 Points (n = 66) | Category 5 Increase ≥20.0 Points (n = 80) | p for Trend | |
| Age, yrs | 74.74 ± 8.04 | 71.37 ± 8.75 | 73.48 ± 8.07 | 71.91 ± 8.82 | 71.54 ± 7.80 | 0.04 |
| Male, % | 66.67 | 51.28 | 44.62 | 68.18 | 61.25 | 0.36 |
| Black race, % | 10.71 | 24.36 | 12.31 | 13.64 | 17.50 | 0.21 |
| ABI | 0.64 ± 0.14 | 0.64 ± 0.14 | 0.65 ± 0.15 | 0.67 ± 0.15 | 0.67 ± 0.15 | 0.24 |
| BMI, kg/m2 | 28.34 ± 4.90 | 27.76 ± 5.72 | 28.24 ± 5.15 | 27.11 ± 3.93 | 27.33 ± 4.76 | 0.59 |
| Current smoker, % | 16.67 | 17.95 | 15.38 | 16.67 | 20.00 | 0.81 |
| Angina, % | 39.29 | 20.51 | 32.31 | 42.42 | 21.25 | 0.31 |
| CHF, % | 22.62 | 14.10 | 24.62 | 25.76 | 13.75 | 0.97 |
| MI, % | 28.57 | 15.38 | 24.62 | 22.73 | 27.50 | 0.22 |
| Stroke, % | 10.71 | 12.82 | 13.08 | 7.58 | 16.25 | 0.55 |
| Pulmonary disease, % | 30.95 | 32.05 | 37.69 | 36.36 | 27.50 | 0.87 |
| Cancer, % | 14.29 | 16.67 | 15.38 | 10.61 | 21.25 | 0.40 |
| Diabetes, % | 39.29 | 30.77 | 27.69 | 31.82 | 28.75 | 0.51 |
| Blocks walked in the past week, n | 33.11 ± 36.33 | 35.81 ± 69.35 | 17.93 ± 40.75 | 37.58 ± 47.31 | 39.48 ± 58.44 | 0.65 |
| Statin use, % | 55.95 | 46.15 | 43.08 | 40.91 | 36.25 | 0.08 |
| ACE inhibitor use, % | 36.90 | 19.23 | 28.46 | 27.27 | 22.50 | 0.06 |
| Change in WIQ Distance Score | ||||||
| Category1 Decline ≥20.0 Points (n = 88) | Category 2 Decline 20.0–5.0 Points (n = 69) | Category 3 Decline <5.0 and Increase <5.0 Points (n = 129) | Category 4 Increase 5.0–20.0 Points (n = 77) | Category 5 Increase ≥20.0 Points (n = 68) | p for Trend | |
| Age, yrs | 72.19 ± 8.09 | 73.75 ± 7.12 | 73.31 ± 8.59 | 72.34 ± 8.09 | 71.15 ± 8.85 | 0.38 |
| Male, % | 65.91 | 43.48 | 56.59 | 62.34 | 54.41 | 0.52 |
| Black race, % | 13.64 | 17.39 | 13.18 | 11.69 | 20.59 | 0.54 |
| ABI | 0.69 ± 0.12 | 0.64 ± 0.15 | 0.64 ± 0.14 | 0.65 ± 0.17 | 0.66 ± 0.16 | 0.26 |
| BMI, kg/m2 | 27.96 ± 4.38 | 27.70 ± 5.03 | 28.09 ± 5.24 | 27.76 ± 4.36 | 27.86 ± 5.86 | 0.88 |
| Current smoker, % | 17.05 | 24.64 | 13.18 | 12.99 | 22.06 | 0.68 |
| Angina, % | 39.77 | 31.88 | 31.01 | 24.68 | 25.00 | 0.05 |
| CHF, % | 25.00 | 18.84 | 19.38 | 20.78 | 16.18 | 0.10 |
| MI, % | 26.14 | 23.19 | 22.48 | 24.68 | 22.06 | 0.88 |
| Stroke, % | 13.64 | 8.70 | 10.85 | 10.39 | 16.18 | 0.73 |
| Pulmonary disease, % | 30.68 | 39.13 | 37.98 | 25.97 | 30.88 | 0.76 |
| Cancer, % | 12.50 | 10.14 | 17.83 | 20.78 | 14.71 | 0.75 |
| Diabetes, % | 35.23 | 33.33 | 27.91 | 28.57 | 35.29 | 0.87 |
| Blocks walked in the past week, n | 52.41 ± 76.50 | 30.71 ± 37.31 | 25.94 ± 39.59 | 33.00 ± 35.10 | 31.99 ± 51.67 | 0.01 |
| Statin use, % | 52.27 | 46.38 | 44.19 | 41.56 | 35.29 | 0.08 |
| ACE inhibitor use, % | 34.09 | 24.64 | 25.58 | 28.57 | 20.59 | 0.06 |
| Change in WIQ Speed Score | ||||||
| Category 1 Decline ≥20.0 Points (n = 77) | Category 2 Decline 20.0–5.0 Points (n = 121) | Category 3 Decline <5.0 and Increase <5.0 Points (n = 60) | Category 4 Increase 5.0–20.0 Points (n = 125) | Category 5 Increase ≥20.0 Points (n = 52) | p for Trend | |
| Age, yrs | 71.79 ± 9.05 | 72.76 ± 8.45 | 73.19 ± 7.82 | 73.26 ± 8.18 | 72.06 ± 8.57 | 0.54 |
| Male, % | 66.23 | 51.61 | 46.02 | 67.00 | 53.85 | 0.80 |
| Black race, % | 16.88 | 12.90 | 14.16 | 11.00 | 28.85 | 0.14 |
| ABI | 0.67 ± 0.12 | 0.66 ± 0.14 | 0.65 ± 0.15 | 0.66 ± 0.16 | 0.64 ± 0.16 | 0.23 |
| BMI, kg/m2 | 27.32 ± 4.49 | 28.52 ± 5.55 | 27.88 ± 5.40 | 27.94 ± 4.69 | 27.26 ± 4.31 | 0.57 |
| Current smoker, % | 16.88 | 17.20 | 16.81 | 21.00 | 11.54 | 0.99 |
| Angina, % | 31.17 | 38.71 | 30.97 | 34.00 | 13.46 | 0.19 |
| CHF, % | 16.88 | 21.51 | 23.89 | 21.00 | 17.31 | 0.84 |
| MI, % | 23.38 | 22.58 | 20.35 | 25.00 | 32.69 | 0.16 |
| Stroke,% | 7.79 | 17.20 | 11.50 | 12.00 | 13.46 | 0.21 |
| Pulmonary disease, % | 32.47 | 44.09 | 33.63 | 30.00 | 21.15 | 0.28 |
| Cancer, % | 20.78 | 16.13 | 8.85 | 17.00 | 19.23 | 0.43 |
| Diabetes,% | 31.17 | 29.03 | 34.51 | 30.00 | 32.69 | 0.83 |
| Blocks walked in the past | 51.92 ± 75.48 | 30.08 ± 43.85 | 28.08 ± 35.26 | 30.61 ± 48.80 | 32.40 ± 43.51 | 0.06 |
| week, n | ||||||
| Statin use, % | 45.45 | 56.99 | 45.13 | 34.00 | 42.31 | 0.19 |
| ACE inhibitor use, % | 27.27 | 30.11 | 26.55 | 29.00 | 25.00 | 0.52 |
Values shown are mean ± SE, unless otherwise indicated. Where applicable, values are the means ± SDs across the categories. Two-year WIQ domain score change was calculated by subtracting the 2-year WIQ domain score from the baseline respective WIQ domain score. ABI = ankle brachial index; ACE = angiotensin-converting enzyme; BMI = body mass index; CHF = congestive heart failure; MI = myocardial infarction; PAD = peripheral arterial disease; WIQ = Walking Impairment Questionnaire.
In multivariable logistic regression, higher baseline physical activity, measured by blocks walked in the past week, was associated with greater decline in the WIQ distance and speed scores, respectively (data not shown). History of cancer was also associated with greater decline in the WIQ speed score, and older age and history of hip arthritis were associated with greater declines in the WIQ stair climbing score (data not shown).
Associations of 2-year change in WIQ scores with all-cause and CVD mortality.
Tables 2 to 4 show associations of 2-year change in each WIQ score with all-cause and CVD mortality, adjusting for baseline age, sex, race, ABI, BMI, smoking status, comorbidities, statin use, ACE inhibitor use, study cohort, physical activity, and baseline WIQ domain score.
Table 2.
Adjusted Associations of Categories of 2-Year Change in WIQ Stair Climbing Score With All-Cause and CVD Mortality Among PAD Participants (n = 438)
| Category | All-Cause Mortality |
CVD Mortality |
||||||
|---|---|---|---|---|---|---|---|---|
| Events | HR (95% CI) | Pairwise Value | p Trend | Events | HR (95% CI) | Pairwise p Value | p Trend | |
| Model I | ||||||||
| Category 1(decline ≥20.0 points) | 34 | 1.93 (1.01–3.68) | 0.05 | 0.004 | 15 | 1.61 (0.59–4.36) | 0.350 | 0.229 |
| Category 2 (decline 20.0–5.0 points) | 20 | 1.05 (0.54–2.06) | 0.88 | 7 | 0.65 (0.22–1.89) | 0.430 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 35 | 0.90 (0.50–1.62) | 0.72 | 11 | 0.43 (0.16–1.18) | 0.100 | ||
| Category 4 (increase 5.0–20.0 points) | 11 | 0.59 (0.28–1.27) | 0.18 | 3 | 0.22 (0.06–0.90) | 0.035 | ||
| Category 5 (increase ≥20.0 points) | 22 | 1.00 (referent) | NA | 10 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Change in ABI | ||||||||
| Category 1 (decline ≥20.0 points) | 31 | 1.82 (0.94–3.52) | 0.07 | 0.019 | 15 | 1.68 (0.62–4.60) | 0.310 | 0.150 |
| Category 2 (decline 20.0–5.0 points) | 20 | 1.00 (0.51–1.96) | 0.99 | 7 | 0.64 (0.22–1.86) | 0.411 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 33 | 0.81 (0.44–1.47) | 0.48 | 11 | 0.41 (0.15–1.13) | 0.084 | ||
| Category 4 (increase 5.0–20.0 points) | 11 | 0.58 (0.27–1.25) | 0.16 | 3 | 0.22 (0.05–0.90) | 0.035 | ||
| Category 5 (increase ≥20.0 points) | 22 | 1.00 (referent) | NA | 10 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Stroke | ||||||||
| Category 1 (decline ≥20.0 points) | 28 | 1.62 (0.80–3.30) | 0.18 | 0.072 | 12 | 1.00 (0.33–2.98) | 0.998 | 0.796 |
| Category 2 (decline 20.0–5.0 points) | 18 | 0.95 (0.45–2.02) | 0.90 | 6 | 0.53 (0.16–1.74) | 0.296 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 26 | 0.78 (0.40–1.53) | 0.46 | 7 | 0.32 (0.10–1.00) | 0.050 | ||
| Category 4 (increase 5.0–20.0 points) | 11 | 0.78 (0.35–1.75) | 0.55 | 3 | 0.29 (0.07–1.27) | 0.102 | ||
| Category 5 (increase ≥20.0 points) | 17 | 1.00 (referent) | NA | 8 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident MI | ||||||||
| Category 1 (decline ≥20.0 points) | 28 | 1.53 (0.75–3.10) | 0.24 | 0.098 | 12 | 0.98 (0.34–2.84) | 0.973 | 0.872 |
| Category 2 (decline 20.0–5.0 points) | 18 | 0.94 (0.45–1.98) | 0.87 | 6 | 0.56 (0.17–1.83) | 0.337 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 26 | 0.78 (0.40–1.53) | 0.47 | 7 | 0.31 (0.10–0.96) | 0.043 | ||
| Category 4 (increase 5.0–20.0 points) | 11 | 0.72 (0.32–1.62) | 0.43 | 3 | 0.23 (0.05–0.97) | 0.045 | ||
| Category 5 (increase ≥20.0 points) | 17 | 1.00 (referent) | NA | 8 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Angina | ||||||||
| Category 1 (decline ≥20.0 points) | 27 | 1.46 (0.72–2.98) | 0.30 | 0.133 | 12 | 0.96 (0.33–2.80) | 0.940 | 0.834 |
| Category 2 (decline 20.0–5.0 points) | 18 | 0.93 (0.44–1.96) | 0.85 | 6 | 0.53 (0.17–1.73) | 0.295 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 26 | 0.78 (0.40–1.53) | 0.47 | 7 | 0.30 (0.09–0.95) | 0.040 | ||
| Category 4 (increase 5.0–20.0 points) | 11 | 0.72 (0.32–1.61) | 0.42 | 3 | 0.23 (0.05–0.99) | 0.048 | ||
| Category 5 (increase ≥20.0 points) | 17 | 1.00 (referent) | NA | 8 | 1.00 (referent) | NA | ||
Model I is adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use, ACE inhibitor use, study cohort, and baseline WIQ stair climbing score. Pair-wise p value shows statistical significance relative to Category 5. Categories for WIQ stair climbing score change were calculated by subtracting the 2-year WIQ stair climbing score from the baseline respective WIQ stair climbing score. CI = confidence interval; CVD = cardiovascular disease; HR = hazard ratio; other abbreviations as in Table 1.
Table 4.
Adjusted Associations of Categories of 2-Year Change in WIQ Speed Score With All-Cause and CVD Mortality Among PAD Participants (n = 435)
| Category | All-Cause mortality |
CVD Mortality |
||||||
|---|---|---|---|---|---|---|---|---|
| Events | HR (95% CI) | Pairwise p Value | p Trend | Events | HR (95% CI) | Pairwise p Value | p Trend | |
| Model I | ||||||||
| Category 1(decline ≥20.0 points) | 26 | 3.55 (1.57–8.04) | 0.002 | 0.019 | 11 | 2.55 (0.78–8.38) | 0.122 | 0.174 |
| Category 2 (decline 20.0–5.0 points) | 34 | 2.53 (1.20–5.34) | 0.014 | 14 | 1.35 (0.46–3.97) | 0.585 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 27 | 1.23(0.60–2.54) | 0.575 | 10 | 0.67 (0.22–2.00) | 0.473 | ||
| Category 4 (increase 5.0–20.0 points) | 22 | 1.28 (0.61–2.71) | 0.517 | 5 | 0.45 (0.13–1.55) | 0.205 | ||
| Category 5 (increase ≥20.0 points) | 12 | 1.00 (referent) | NA | 6 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Change in ABI | ||||||||
| Category 1(decline ≥20.0 points) | 23 | 2.90(1.26–6.69) | 0.013 | 0.063 | 11 | 2.43 (0.74–7.92) | 0.141 | 0.168 |
| Category 2 (decline 20.0–5.0 points) | 34 | 2.39(1.13–5.05) | 0.023 | 14 | 1.27 (0.43–3.76) | 0.661 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 26 | 1.20(0.58–2.49) | 0.628 | 10 | 0.71 (0.24–2.13) | 0.543 | ||
| Category 4 (increase 5.0–20.0 points) | 22 | 1.26 (0.59–2.66) | 0.550 | 5 | 0.44 (0.13–1.54) | 0.198 | ||
| Category 5 (increase ≥20.0 points) | 12 | 1.00 (referent) | NA | 6 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Stroke | ||||||||
| Category 1 (decline ≥20.0 points) | 21 | 2.22 (0.89–5.54) | 0.087 | 0.253 | 9 | 0.93 (0.23–3.70) | 0.916 | 0.778 |
| Category 2 (decline 20.0–5.0 points) | 28 | 1.91 (0.85–4.26) | 0.116 | 10 | 0.63 (0.18–2.19) | 0.471 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 22 | 1.09 (0.50–2.38) | 0.830 | 9 | 0.57 (0.17–1.91) | 0.359 | ||
| Category 4 (increase 5.0–20.0 points) | 18 | 1.10 (0.49–2.50) | 0.816 | 3 | 0.25 (0.05–1.14) | 0.074 | ||
| Category 5 (increase ≥20.0 points) | 11 | 1.00 (referent) | NA | 5 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident MI | ||||||||
| Category 1 (decline ≥20.0 points) | 21 | 2.31 (0.93–5.76) | 0.073 | 0.212 | 9 | 1.31 (0.34–5.01) | 0.692 | 0.776 |
| Category 2 (decline 20.0–5.0 points) | 28 | 1.94 (0.87–4.34) | 0.105 | 10 | 0.72 (0.21–2.44) | 0.593 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 22 | 1.11(0.51–2.42) | 0.799 | 9 | 0.67 (0.20–2.27) | 0.525 | ||
| Category 4 (increase 5.0–20.0 points) | 18 | 1.13 (0.50–2.57) | 0.767 | 3 | 0.28 (0.06–1.27) | 0.098 | ||
| Category 5 (increase ≥20.0 points) | 11 | 1.00 (referent) | NA | 5 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Angina | ||||||||
| Category 1 (decline ≥20.0 points) | 20 | 2.14 (0.85–5.41) | 0.108 | 0.256 | 9 | 1.41 (0.36–5.51) | 0.618 | 0.763 |
| Category 2 (decline 20.0–5.0 points) | 28 | 1.92 (0.86–4.30) | 0.113 | 10 | 0.75 (0.22–2.53) | 0.642 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 22 | 1.12 (0.51–2.45) | 0.776 | 9 | 0.66 (0.19–2.22) | 0.500 | ||
| Category 4 (increase 5.0–20.0 points) | 18 | 1.14 (0.50–2.58) | 0.760 | 3 | 0.27 (0.06–1.24) | 0.093 | ||
| Category 5 (increase ≥20.0 points) | 11 | 1.00 (referent) | NA | 5 | 1.00 (referent) | NA | ||
Model I is adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use, ACE inhibitor use, study cohort, and baseline WIQ speed score. Pair-wise p value shows statistical significance relative to Category 5. Categories for WIQ speed score change were calculated by subtracting the 2-year WIQ speed score from the baseline respective WIQ speed score. Abbreviations as in Tables 1 and 2.
Greater 2-year decline in WIQ stair climbing score was associated with higher all-cause mortality (p for trend = 0.004) (Table 2). After additional adjustment for any newly diagnosed stroke, MI, or angina, or progression in the ABI, the association of greater 2-year decline in WIQ stair climbing score with higher all-cause mortality was attenuated and remained statistically significant only in the model that additionally adjusted for change in ABI. No significant association was observed between greater 2-year decline in WIQ stair climbing score and higher CVD mortality.
Greater 2-year decline in WIQ distance score was associated with higher all-cause mortality (p for trend = 0.006) (Table 3). After additional adjustment for any newly diagnosed stroke, MI, or angina, or progression in the ABI, the association of greater 2-year decline in WIQ distance score with higher all-cause mortality was attenuated and no longer statistically significant. Overall, no significant associations were observed between greater 2-year decline in WIQ distance score and higher CVD mortality. However, participants in Category 1 (worst) and Category 2 for 2-year change in WIQ distance score had a higher incidence of CVD mortality compared with participants in Category 5 (best) for 2-year change in WIQ distance score (hazard ratio [HR]: 4.56, 95% confidence interval [CI]: 1.30 to 16.01; and HR: 4.31, 95% CI: 1.26 to 14.80, respectively). After adjustment for 2-year change in ABI, participants in Category 1 (worst) for 2-year change in WIQ distance score were at greater risk for CVD mortality compared with participants in Category 5 (best) for 2-year change in WIQ distance score (p = 0.036).
Table 3.
Adjusted Associations of Categories of 2-Year Change in WIQ Distance Score With All-Cause and CVD Mortality Among PAD Participants (n = 431)
| Category | All-Cause Mortality |
CVD Mortality |
||||||
|---|---|---|---|---|---|---|---|---|
| Events | HR (95% CI) | Pairwise p Value | p Trend | Events | HR (95% CI) | Pairwise p Value | p Trend | |
| Model I | ||||||||
| Category 1(decline ≥20.0 points) | 36 | 2.34 (1.15–4.75) | 0.018 | 0.006 | 13 | 4.56 (1.30–16.01) | 0.018 | 0.069 |
| Category 2 (decline 20.0–5.0 points) | 21 | 1.68 (0.82–3.43) | 0.158 | 11 | 4.31 (1.26–14.80) | 0.020 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 29 | 1.10 (0.57–2.12) | 0.775 | 11 | 1.32 (0.39–4.50) | 0.658 | ||
| Category 4 (increase 5.0–20.0 points) | 18 | 1.28 (0.62–2.62) | 0.507 | 5 | 1.73 (0.44–6.76) | 0.429 | ||
| Category 5 (increase ≥20.0 points) | 15 | 1.00 (referent) | NA | 4 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Change in ABI | ||||||||
| Category 1(decline ≥20.0 points) | 32 | 1.91 (0.92–3.96) | 0.081 | 0.060 | 13 | 3.80 (1.09–13.28) | 0.036 | 0.087 |
| Category 2 (decline 20.0–5.0 points) | 21 | 1.52 (0.73–3.13) | 0.261 | 11 | 3.46 (1.00–11.94) | 0.050 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 28 | 0.99 (0.50–1.94) | 0.968 | 11 | 1.09 (0.32–3.73) | 0.892 | ||
| Category 4 (increase 5.0–20.0 points) | 18 | 1.21 (0.59–2.51) | 0.605 | 5 | 1.42 (0.36–5.61) | 0.615 | ||
| Category 5 (increase ≥20.0 points) | 15 | 1.00 (referent) | NA | 4 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Stroke | ||||||||
| Category 1 (decline ≥20.0 points) | 30 | 1.42 (0.64–3.18) | 0.391 | 0.45 | 12 | 1.25 (0.35–4.52) | 0.734 | 0.972 |
| Category 2 (decline 20.0–5.0 points) | 17 | 1.26 (0.56–2.84) | 0.571 | 8 | 1.53 (0.41–5.66) | 0.527 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 25 | 1.17 (0.55–2.52) | 0.679 | 8 | 0.65 (0.16–2.60) | 0.540 | ||
| Category 4 (increase 5.0–20.0 points) | 14 | 1.12 (0.50–2.54) | 0.779 | 3 | 0.62 (0.13–3.06) | 0.561 | ||
| Category 5 (increase ≥20.0 points) | 12 | 1.00 (referent) | NA | 4 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident MI | ||||||||
| Category 1 (decline ≥20.0 points) | 30 | 1.57 (0.70–3.48) | 0.271 | 0.293 | 12 | 1.83 (0.51–6.59) | 0.355 | 0.564 |
| Category 2 (decline 20.0–5.0 points) | 17 | 1.22 (0.54–2.74) | 0.635 | 8 | 1.43 (0.38–5.40) | 0.594 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 25 | 1.10 (0.52–2.36) | 0.802 | 8 | 0.59 (0.15–2.31) | 0.445 | ||
| Category 4 (increase 5.0–20.0 points) | 15 | 1.15 (0.51–2.60) | 0.743 | 3 | 0.70 (0.14–3.40) | 0.656 | ||
| Category 5 (increase ≥20.0 points) | 12 | 1.00 (referent) | NA | 4 | 1.00 (referent) | NA | ||
| Model I + 2-Yr Incident Angina | ||||||||
| Category 1 (decline ≥20.0 points) | 29 | 1.49 (0.67–3.31) | 0.332 | 0.360 | 12 | 1.82 (0.50–6.67) | 0.363 | 0.564 |
| Category 2 (decline 20.0–5.0 points) | 17 | 1.21 (0.54–2.72) | 0.645 | 8 | 1.41 (0.38–5.26) | 0.612 | ||
| Category 3 (decline ≤5.0 and increase ≤5.0 points) | 25 | 1.13 (0.53–2.42) | 0.746 | 8 | 0.53 (0.13–2.09) | 0.362 | ||
| Category 4 (increase 5.0–20.0 points) | 14 | 1.15 (0.51–2.63) | 0.736 | 3 | 0.67 (0.14–3.25) | 0.618 | ||
| Category 5 (increase ≥20.0 points) | 12 | 1.00 (referent) | NA | 4 | 1.00 (referent) | NA | ||
Model I is adjusted for age, sex, race, body mass index, smoking status, ankle brachial index, comorbidities, physical activity, statin use, ACE inhibitor use, study cohort, and baseline WIQ distance score. Pair-wise p value shows statistical significance relative to Category 5. Categories for WIQ distance score change were calculated by subtracting the 2-year WIQ distance score from the baseline respective WIQ distance score. Abbreviations as in Tables 1 and 2.
Greater decline in the WIQ speed score was associated with higher all-cause mortality (p for trend = 0.019) (Table 4). After additional adjustment for any newly diagnosed stroke, MI, or angina, or progression in the ABI, the association of greater 2-year decline in WIQ speed score with higher all-cause mortality was attenuated and no longer statistically significant. However, participants in Category 1 (worst) and Category 2 for 2-year change in WIQ speed score remained at higher risk for all-cause mortality compared with participants in Category 5 (best) after adjusting for change in the ABI (p = 0.013). No association was observed between greater 2-year decline in WIQ speed score and higher CVD mortality.
When each WIQ change score was added to a traditional risk model predicting all-cause and cardiovascular mortality, the change score generally modestly improved the predictive ability of the overall model. Specifically, for all-cause mortality, the improvements in prediction were + 0.02, +0.075, and +0.046 for the WIQ distance, speed, and stair climbing scores, respectively, on a scale of —2.0 to +2.0 scale, where + 2.0 represents the greatest possible gain in prediction and —2.0 represents the greatest possible loss of prediction ability. For CVD mortality, the improvements in prediction were +0.080, +0.071, and +0.005 for the WIQ distance, speed, and stair climbing scores, respectively, on the scale of —2.0 to +2.0.
Greater decline in the average of the 3 WIQ score domains was associated with increased mortality, adjusting for age, sex, race, ABI, BMI, smoking status, comorbidities, statin use, ACE inhibitor use, study cohort, physical activity, and baseline WIQ domain score (p trend = 0.004). Associations of each category of average WIQ score decline with all-cause mortality were: Category I, HR: 3.91 (95% CI: 1.75 to 8.78); Category 2, HR: 1.88 (95% CI: 0.93 to 3.81); Category 3, HR: 1.25 (95% CI: 0.62 to 2.54); and Category 4, HR: 1.42 (95% CI: 0.65 to 3.12) relative to the reference of Category 5. Greater decline in the averaged WIQ score was not associated with increased CVD mortality (p trend = 0.0545).
Greater declines in WIQ score were not associated with greater ABI declines, adjusting for age, sex, race, comorbidities, BMI, baseline ABI, baseline WIQ score, physical activity, or medications (data not shown).
Discussion
Among 442 men and women with PAD, greater 2-year declines in WIQ stair climbing, distance, and speed scores were associated with higher all-cause mortality, after adjusting for baseline ABI, baseline WIQ score, comorbidities, age, and other potential confounders. Participants with ≥20.0 point declines in WIQ stair climbing, WIQ distance, and WIQ speed scores had approximately 2- to 3-fold increases in all-cause mortality compared with those with ≥20.0 point increases in these scores. In addition, participants with a >20.0 point decline in WIQ distance score were nearly 4 times more likely to die from CVD compared with those with a ≥20.0 point increase in the WIQ distance score. Because our analyses adjusted for baseline WIQ score, these results demonstrated meaningful associations of change in each WIQ domain score, even after taking into account the baseline WIQ score.
We did not observe a significant association between greater 2-year declines in WIQ stair climbing, distance, and speed scores with higher CVD mortality. Given the relatively low number of deaths due to CVD, statistical power was limited for the association of change in each WIQ score with CVD mortality. For example, we had only 44% power to observe a statistically significant association of 2-year change in WIQ distance score with CVD mortality.
In exploratory analyses that included additional adjustment for newly diagnosed stroke, MI, or angina, or progression of the ABI, the observed associations of greater 2-year declines in WIQ domain scores with higher all-cause mortality were attenuated. These findings suggested that progression of systemic CVD might explain associations of change in WIQ domain scores with all-cause mortality.
Relatively little is known regarding the association of decline in patient-perceived walking ability with mortality risk in either the PAD population or the general population. In a population of 7,700 Veterans Administration outpatients, Fan et al. (14) found that a 1-year decrease in the physical component summary (PCS) score from the Short Form 36 Health Survey, a global measure of health-related quality of life that also assesses patient-perceived walking ability, was associated with an increased risk of death (odds ratio: 2.3, 95% CI: 1.6 to 3.4). Similar findings were observed by Otero-Rodriguez et al. (15) in a smaller study of approximately 2,400 Spanish subjects >60 years of age; a 2-year decline in the PCS score predicted all-cause mortality in the subsequent 4 years of follow-up. Participants with the greatest decline in PCS score had an HR of 2.12 (95% CI: 1.39 to 3.24) for mortality. Although the prevalences of PAD in these study populations were not reported, the observed associations of declines in patient-perceived walking ability with mortality are relevant in the PAD population. To our knowledge, this is the first study that assessed the association between decline in patient-perceived walking ability and all-cause and CVD mortality specifically in subjects with PAD, who are at higher risk of CVD events and mortality than subjects without PAD (16).
We previously reported that among participants with PAD in our WALCS cohort, greater 2-year declines in 6-min walking distance and 4-m walking velocity (fast-paced) were associated with higher all-cause mortality. Greater 2-year decline in 6-min walking distance was associated with higher CVD mortality (16). Although both the 6-min walking distance and 4-m walking velocity are useful in mortality risk prediction, they are objective measures that require dedicated time and space in the clinical setting, whereas the WIQ can be self-administered by PAD patients and is not time or labor intensive. However, applying our results to clinical practice would require that physicians be prompted to re-administer the WIQ score 2 years after a baseline measure. Further study is needed to determine whether implementing measurement of 2-year change in WIQ scores in clinical practice is associated with improved outcomes.
Study limitations.
First, although we adjusted for confounders including comorbidities and baseline WIQ scores, we could not rule out the possibility that unidentified characteristics among participants with greater 2-year decline in WIQ domain scores contributed to the observed associations with mortality risk. Second, although measuring 2-year change in the WIQ allowed us to maximize identification of patients with meaningful changes in the WIQ score, further study is needed to determine whether changes in the WIQ score at shorter follow-up intervals are associated with similar outcomes to those reported here. However, it is likely that the magnitude of change in the WIQ score, rather than the length of time between a baseline and WIQ score, is most important with regard to subsequent outcomes. Third, because we ex-cluded persons who were not fluent in English, who died before 2-year follow-up, or who underwent lower extremity revascularization before 2-year follow-up, these findings might not be generalizable to all PAD patients. Fourth, because of the relatively small absolute number of events and relatively large variance in WIQ score changes, 95% CIs were wide. Fifth, we did not record information about recruitment site. Thus, we were unable to adjust for recruitment site in our analyses. However, recruiting consecutive PAD patients from several noninvasive vascula laboratories in the Chicago area is likely to increase the generalizability of our findings. There is no reason to believe that relationships between change in the WIQ score and mortality would differ between recruitment sites.
Conclusions
Men and women with PAD with greater decline in WIQ stair climbing, WIQ distance, or WIQ speed scores are at higher all-cause mortality risk compared with those with greater improvement in WIQ domain scores. The progression of systemic CVD is a potential mechanism for increased all-cause mortality risk.
Acknowledgments
This study was supported by grants from the National Heart, Lung, and Blood Institute (K12-HL083790, R01- HL083064, R01-HL64739, and R01-HL71223) and by a grant from the National Center for Research Resources, National Institutes of Health (RR-00048). This study was also supported by the National Institute on Aging. The authors have no relationships relevant to the contents of this paper to disclose. William Hiatt, MD, acted as Guest Editor for this paper.
Abbreviations and Acronyms
- ABI
ankle-brachial index
- ACE
angiotensin-converting enzyme
- BMI
body mass index
- CVD
cardiovascular disease
- MI
myocardial infarction
- PAD
peripheral arterial disease
- PCS
physical component summary
- WIQ
Walking Impairment Questionnaire
REFERENCES
- 1.Allison MA, Ho E, Denenberg JO, et al. Ethnic-specific prevalence of peripheral arterial disease in the United States. Am J Prev Med 2007;32:328–33. [DOI] [PubMed] [Google Scholar]
- 2.Heald CL, Fowkes FGR, Murray GD, Price JF, Collaborat ABI. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis 2006;189:61–9. [DOI] [PubMed] [Google Scholar]
- 3.Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. J Vasc Surg 1996;23:104–15. [DOI] [PubMed] [Google Scholar]
- 4.Jain A, Liu K, Ferrucci L, Criqui MH, et al. The Walking Impairment Questionnaire stair-climbing score predicts mortality in men and women with peripheral arterial disease. J Vasc Surg 2012;55:1662–73 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDermott MM, Greenland P, Liu K, et al. The ankle brachial index is associated with leg function and physical activity: the Walking and Leg Circulation Study. Ann Intern Med 2002;136:873–83. [DOI] [PubMed] [Google Scholar]
- 6.McDermott MM, Hoff F, Ferrucci L, et al. Lower extremity ischemia, calf skeletal muscle characteristics, and functional impairment in peripheral arterial disease. J Am Geriatr Soc 2007;55:400–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Regensteiner J, Steiner JF, Panzer RJ, Hiatt WR. Evaluation of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol 1990;2:142–52. [Google Scholar]
- 8.Nicolai SP, Kruidenier LM, Rouwet EV, Graffius K, Prins MH, Teijink JA. The Walking Impairment Questionnaire: an effective tool to assess the effect of treatment in patients with intermittent claudication. J Vasc Surg 2009;50:89–94. [DOI] [PubMed] [Google Scholar]
- 9.McDermott MM, Ades P, Guralnik JM, et al. Treadmill exercise and resistance training in patients with peripheral arterial disease with and without intermittent claudication: a randomized controlled trial. JAMA 2009;301:165–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDermott MM, Criqui MH, Liu K, et al. Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease. J Vasc Surg 2000;32:1164–71. [DOI] [PubMed] [Google Scholar]
- 11.Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol 2004;44:618–23. [DOI] [PubMed] [Google Scholar]
- 12.Guralnik J The Women’s Health and Aging Study: Health and Social Characteristics of Older Women with Disability. Bethesda, MD: National Institute on Aging, National Institutes of Health; 1995: Appendix E. [Google Scholar]
- 13.Garg PK, Liu K, Tian L, Guralnik JM, et al. Physical activity during daily life and functional decline in peripheral arterial disease. Circulation 2009;119:251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan VS, Au DH, McDonell MB, Fihn SD. Intraindividual change in SF-36 in ambulatory clinic primary care patients predicted mortality and hospitalizations. J Clin Epidemiol 2004;57:277–83. [DOI] [PubMed] [Google Scholar]
- 15.Otero-Rodriguez A, Leon-Munoz LM, Balboa-Castillo T, Banegas JR, Rodriguez-Artalejo F, Guallar-Castillon P. Change in health-related quality of life as a predictor of mortality in the older adults. Qual Life Res 2010;19:15–23. [DOI] [PubMed] [Google Scholar]
- 16.McDermott MM, Liu K, Ferrucci L, et al. Decline in functional performance predicts later increased mobility loss and mortality in peripheral arterial disease. J Am Coll Cardiol 2011;57:962–70. [DOI] [PMC free article] [PubMed] [Google Scholar]