Abstract
Depression, HIV-related stigma and low levels of social support may be particularly prevalent and adversely affect health and treatment outcomes among HIV-infected pregnant women. We examined factors associated with social support and stigma among pregnant women initiating antiretroviral therapy in the Western Cape, South Africa; and explored associations with depressive symptoms (Edinburgh Postnatal Depression Scale; EPDS) in linear regression models. Among 623 participants, 11% and 19% had elevated EPDS scores using thresholds described in the original development of the scale (scores ≥13 and ≥10, respectively). Social support and stigma were highly interrelated and were associated with depressive symptoms. Stigma was observed to moderate the association between social support and depression scores; when levels of stigma were high, no association between social support and depression scores was observed. Elevated depression scores are prevalent in this setting, and interventions to reduce stigma and to address risk factors for depressive symptoms are needed.
Keywords: Social support;, stigma;, antenatal depression;, pregnancy;, South Africa
Background
Antenatal depression is prevalent in low- and middle-income countries (LMICs) [1, 2], with documented adverse effects on both maternal and child health [3–5]. Many of the risk factors for antenatal depression are prevalent in LMIC settings where HIV is most common, including poverty, unplanned pregnancy, and traumatic life events [6]. HIV-infected pregnant women may be a particularly vulnerable group, with high rates of depressive symptoms and psychiatric morbidity reported globally [7]. Other prevalent risk factors in this population may include high levels of HIV-related stigma and low levels of social support, both of which have been shown to have negative effects on factors such as coping [8] and quality of life [9]. Of note is that depression has been shown to be associated with non-adherence to antiretroviral therapy (ART) [10] and with attrition from care [11] in general HIV populations in Africa. Each of depression, HIV-related stigma and a lack of social support have additionally been identified as barriers to accessing prevention of mother-to-child transmission (PMTCT) services [12] and to the uptake of antiretrovirals for PMTCT [13]; and HIV-related stigma is a widely reported barrier to ART initiation, adherence and retention in care among HIV-infected pregnant and postpartum women [14].
There is thus strong evidence that depression and psychosocial factors play an important role in the treatment of HIV disease, and these factors are increasingly understood as constituting barriers to HIV care in the context of both general HIV and PMTCT programmes. In addition, recent evidence suggests that psychosocial factors and depression are interrelated. Studies conducted in sub-Saharan Africa have identified associations between depressive symptoms and both low levels of social support [15] and high levels of HIV-related stigma [16, 17], and recent research conducted among HIV-infected men and women in South Africa has reported that both HIV-related stigma and social support are independently associated with depression [18]. However, the interrelationships among these constructs are poorly understood, and most previous research has not explored the potentially moderating effect of these factors on the relationships between other factors and depression. Research that simultaneously explores the independent effects of multiple psychosocial factors is needed in order to generate a more nuanced understanding of the complex interrelationships among these constructs, thereby guiding the development of much-needed interventions. Given the well-documented adverse effects of antenatal depression on both maternal and child health and development, and the fact that there are few effective treatment resources for antenatal depression in LMICs [4, 6], this understanding is urgently needed.
Although risk factors for depression have been well described in many populations, including among HIV-infected pregnant women, research into psychosocial factors in the population of women who initiate lifelong ART during pregnancy is needed, as little research has focussed on this population specifically. Although ART eligibility in pregnant women was previously based on CD4 cell count and clinical disease staging, the World Health Organization now recommends that all pregnant women initiate lifelong ART, a recommendation known as “Option B+” [19]. This recommendation substantially increases the number of ART-eligible pregnant women, and a better understanding of the psychosocial factors that have been shown to impact on HIV care in other populations is needed in this context. We thus examined the factors associated with social support and stigma among HIV-infected pregnant women who were initiating ART in the Western Cape, South Africa; and explored the interrelationships among these constructs and antenatal depressive symptoms. Our aim was (i) to explore variables associated with the perceived availability of social support and HIV-related stigma; and (ii) to explore the relationships between the perceived availability of social support and HIV-related stigma, and antenatal depressive symptoms in this sample.
Methods
This cross-sectional analysis draws on a multi-phase implementation science study evaluating strategies for delivering HIV care and treatment services during pregnancy and the postpartum period (https://clinicaltrials.gov/ct2/show/NCT01933477). The study is located at a large primary care antenatal clinic in the former township of Gugulethu in Cape Town, South Africa. This stable, low socioeconomic community is characterized by high levels of HIV and poverty, with an antenatal HIV prevalence of 29% [20] and an unemployment rate of 40% [21].
Participants
HIV-infected pregnant women were eligible to participate if they were 18 years or older and were eligible to initiate ART based on current local guidelines during the study period. Between March and June 2013, ART eligibility was determined based on CD4 cell count or clinical staging; after June 2013, all HIV-infected pregnant women were eligible to initiate lifelong ART regardless of CD4 cell count or clinical staging. All women provided written informed consent prior to participation. The study was approved by the University of Cape Town’s Faculty of Health Sciences Human Research Ethics Committee and by the Institutional Review Board of the Columbia University Medical Center.
Measures
All measures were translated into isiXhosa, the predominant local language, and were back-translated to ensure accuracy. These measures were piloted prior to the study in order to ensure that items were understood by and applicable to a sample of women recruited from the same population. Given concerns around literacy levels, all measures were administered by trained isiXhosa-speaking interviewers. Study visits were conducted in an interview space separate from the antenatal clinic at study visits which were scheduled to coincide with participants’ routine antenatal visits. Demographic characteristics, including age, marital status, gravidity, and timing of HIV diagnosis, were assessed at participants’ first study visit. For our purposes, a composite poverty score was developed in order to categorize participants into tertiles based on their relative level of disadvantage. This composite score was calculated based on current employment status and a standardized composite asset index score based on housing type and household access to a flush toilet, piped water inside the home, electricity, and a refrigerator, telephone and television. Participants were categorized from least to most disadvantaged based on this score.
Participants completed a battery of psychosocial measures at their second antenatal visit, including a 12-item measure to assess the perceived availability of social support. The original measure was constructed as part of the development of methods to identify members of individuals’ social support networks, with a view to developing procedures suitable for use in community surveys [22]. This measure was then modified and administered to a sample of HIV-infected injection drug users in the United States, and included domains of both instrumental and emotional support [23]. The measure used in the present study was based on this modified scale. Each item was assessed on a scale ranging from 1 to 5, with higher scores indicating higher levels of social support. The perceived availability of instrumental [Cronbach’s alpha (α): 0.88] and emotional support (α: 0.92) were assessed separately by calculating the mean response across items pertaining to these constructs, as widely used elsewhere [24].
HIV-related stigma was assessed using items adapted from the Social Impact Scale [25]. The original scale was developed in order to explore the differential impacts of stigma among individuals diagnosed with HIV and with cancer, respectively, and was constructed through a process of consultation with clinical experts and HIV-infected individuals as well as factor analysis to group the items into sub-scales [25]. For our purposes, five items from the original scale were included, and two items were added assessing HIV-related stigma in the context of motherhood specifically. Items were assessed on a scale ranging from 1 to 5, with higher scores indicating higher levels of stigma. Mean scores were calculated for items assessing two dimensions of stigma, namely social rejection (α: 0.75) and internalized shame (α: 0.80), as described in the original development of the scale [25].
The Edinburgh Postnatal Depression Scale (EPDS; α: 0.78) [26] was used to measure self-reported symptoms common to depressive disorders. This 10-item measure of recent depressive symptoms was originally developed for use in screening for possible depressive disorders among postnatal women, but has been validated for use in pregnancy [27]. In addition, the scale has been validated for use as a screening tool in South Africa in a sample of postnatal women [28]. Each item of the scale was assessed on a frequency scale ranging from 0 to 3, and a total score was obtained by summing individual item responses, with higher scores indicating more severe depressive symptoms. Threshold values of both ≥10 and ≥13 were explored as suggestive of elevated depressive symptoms, as recommended in the original development of the scale [26]. For our purposes, the EPDS was used as a measure of self-reported depressive symptoms, rather than as a diagnostic tool.
Data analysis
Data were analysed using Stata 12 (StataCorp Inc, College Station, Texas, USA). Variables significantly associated with higher levels of instrumental and emotional support and with higher levels of social rejection and internalized shame were identified using Wilcoxon rank sum (Mann-Whitney) and Kruskal-Wallis tests. Multivariable linear regression models were built to examine variables independently associated with these constructs. Variables significantly associated with higher depression scores were similarly identified in unadjusted analyses. The associations between social support, stigma, potential confounders, and depressive symptoms were then explored in linear regression models. In order to explore the effects of social support and stigma on depressive symptoms at different levels of the other variable, tertiles of social support and stigma scores were created corresponding to low, medium and high levels. The potentially moderating effect of each variable was then examined graphically at each level of the other variable. Continuous depression scores were used in all analyses, although the proportion of participants with elevated scores on the EPDS was calculated using the suggested threshold values described above.
Results
Demographic and clinical characteristics and antenatal depressive symptoms:
A total of 623 women [median age: 28 years; inter-quartile range (IQR): 24–32], enrolled between March 2013 and April 2014, completed psychosocial measures and were included in the analysis. Detailed demographic and clinical characteristics are presented in Table 1. Most participants had not completed secondary education and were currently unemployed, and less than half were married or cohabiting. Most participants reported a previous pregnancy, and most of the current pregnancies were unintended. Just over half of the participants were diagnosed with HIV during the current pregnancy. At the time of their second antenatal visit, 84% of participants had initiated ART, with a median duration of ART use of 16 days (IQR: 14–22). A total of 121 women (19%) had elevated EPDS scores using a threshold of ≥10, and 67 women (11%) had EPDS scores ≥13.
Table 1.
Demographic and clinical characteristics and antenatal depressive symptoms
| Variable | n (%) |
|---|---|
| Number of mothers | 623 |
| Age in years – median [IQR] | 28 [24, 32] |
| Ethnicity – Black/African | 620 (99.5) |
| Educational attainment | |
| Primary/some secondary | 457 (73) |
| Completed secondary/any tertiary | 166 (27) |
| Current employment | 386 (62) |
| Unemployed | 237 (38) |
| Employed | |
| Poverty level (assets + employment) | |
| Most disadvantaged | 226 (36) |
| Moderately disadvantaged | 205 (33) |
| Least disadvantaged | 192 (31) |
| Relationship status | |
| Single | 367 (59) |
| Married/cohabiting | 256 (41) |
| Primigravida | 111 (18) |
| Median gestation in weeks at enrolment [IQR] | 20 [16, 26] |
| Pregnancy intention | |
| Unintended | 439 (70) |
| Intended | 184 (30) |
| Time of HIV diagnosis | |
| Before this pregnancy | 280 (45) |
| During this pregnancy | 343 (55) |
| HIV viral load at start of antenatal care | |
| Median [IQR; log10 copies/mL] | 4.0 [3.4, 4.6] |
| <50 copies/mL | 23 (4) |
| 50–1,000 copies/mL | 76 (12) |
| 1,001–10,000 copies/mL | 216 (35) |
| 10,001–100,000 copies/mL | 238 (38) |
| >100,000 copies/mL | 70 (11) |
| CD4 cell count at start of antenatal care (n=607) | |
| Median [IQR; cells/μL] | 343 [235, 507] |
| ≤200 cells/μL | 110(18) |
| 201–350 cells/μL | 206 (34) |
| 351–500 cells/μL | 135 (22) |
| >500 cells/μL | 156 (26) |
| Taking antiretroviral therapy (ART) at time of second antenatal visit | 524 (84) |
| Median [IQR] time on ART in days | 16 [14, 22] |
| Antenatal depressive symptoms (EPDS) | |
| Median score [IQR] | 4 [1, 8] |
| Above threshold ≥10 | 121 (19) |
| Above threshold ≥13 | 67 (11) |
Perceived availability of social support:
Table 2 reports scale scores and item-specific responses from the measures of social support and HIV-related stigma. Although participants reported high levels of social support generally, the reported availability of instrumental support was significantly lower than that of emotional support (mean scores: 4.2 and 4.4, respectively; paired t-test: t=−6.40, p<0.001). Of note, women reported a low availability of monetary support (mean score for item assessing monetary assistance to pay rent: 3.4). Variables associated with the subscales of social support were examined separately. Higher levels of both social rejection [β: −0.1; 95% confidence interval (CI): −0.2, −0.01; p=0.031] and internalized shame (β: −0.3; 95% CI: −0.4, −0.2; p<0.001) were significantly associated with lower perceived availability of instrumental support, after adjusting for age. In addition, after adjustment for age, participants experiencing higher levels of poverty reported significantly lower availability of instrumental support (β for most vs least disadvantaged: −0.3; 95% CI: −0.4, −0.1; p<0.001), while women who were diagnosed with HIV during the current pregnancy reported higher availability of instrumental support (β: 0.2; 95% CI: 0.03, 0.3; p=0.015). Higher levels of both social rejection (β: −0.2; 95% CI: −0.3, −0.1; p=0.003) and internalized shame (β: −0.2; 95% CI: −0.3, −0.1; p<0.001) were similarly significantly associated with lower perceived availability of emotional support, independent of age and poverty.
Table 2.
Social support and HIV-related stigma – total scale scores, item-specific responses, and Cronbach’s alpha (α) coefficients
| Variable | Mean score (SD) | α |
|---|---|---|
| Perceived availability of support1 | 4.2 (0.8) | 0.92 |
| Instrumental support | 4.2 (0.9) | 0.88 |
| Is there someone who would help take care of you if you had to stay in bed for several | 0.87 | |
| weeks? | 4.4 (1.0) | |
| Is there someone you could turn to if you needed to borrow R10, get a ride to the doctor, or | 0.87 | |
| some other small immediate help? | 4.2 (1.2) | |
| Is there someone you could turn to if you needed to borrow some money to help pay your | 0.91 | |
| rent for one month? | 3.4 (1.6) | |
| Is there someone who could take care of your children if you got sick? | 4.4 (1.0) | 0.87 |
| Is there someone who would help you or be with you when you are having the baby? | 4.2 (1.2) | 0.87 |
| Is there someone who would help you take care of the baby, after the new baby is born? | 4.2 (1.2) | 0.87 |
| Is there someone who would help take care of you if you had problems with your | 4.4 (1.0) | 0.86 |
| pregnancy? Is there someone who would help when you get far along in your pregnancy? |
4.4 (1.0) | 0.86 |
| Emotional support | 4.4 (0.9) | 0.92 |
| Would someone be available to talk to you if you were upset, nervous or depressed? | 4.4 (1.0) | 0.90 |
| Is there someone you could contact if you wanted to talk about an important personal | 0.89 | |
| problem you were having? | 4.4 (1.0) | |
| Would the people in your personal life give you information, suggestions, or guidance if | 0.90 | |
| you needed it? | 4.3 (1.1) | |
| Is there someone you could turn to if you needed advice to help make a decision? | 4.4 (1.1) | 0.90 |
| HIV-related stigma2 | 2.2 (0.8) | 0.84 |
| Social rejection | 1.7 (0.8) | 0.75 |
| I feel others are concerned they could “catch” my HIV through contact like a handshake or eating food I make. | 1.8 (0.9) | |
| I feel others avoid me because of my HIV. | 1.7 (0.8) | |
| Internalized shame | 2.4 (0.9) | 0.80 |
| I do not feel I can be open with others about my HIV. | 2.6 (1.4) | 0.70 |
| I feel I need to keep my HIV a secret. | 2.6 (1.4) | 0.71 |
| Due to my HIV, I have a sense of being unequal in my relationships with others. | 1.8 (1.0) | 0.79 |
| I feel like I am a bad mother because I am HIV-positive. | 1.9 (1.0) | 0.76 |
| I worry about who will take care of my baby if I become sick. | 2.8 (1.5) | 0.82 |
Items scored between 1 and 5, with higher scores indicating greater perceived availability of support;
Items scored between 1 and 5, with higher scores indicating greater stigma
HIV-related stigma:
In terms of HIV-related stigma, reported levels of internalized shame were higher than those of social rejection (mean score: 2.4 and 1.7 respectively; paired t-test: t=−20.77, p<0.001). Women reported the highest levels of stigma on items assessing secrecy around their HIV-infection (mean scores: 2.6 for both items) and on the item assessing concern around who will take care of their baby if they become sick (mean score: 2.8). Correlates of both dimensions of HIV-related stigma were explored separately. After adjustment for age and poverty, increased availability of both instrumental (β: −0.2; 95% CI: −0.3, −0.1; p<0.001) and emotional support (β: −0.1; 95% CI: −0.2, −0.02; p=0.013) were significantly associated with lower reported levels of social rejection. Higher levels of both dimensions of social support were similarly associated with lower levels of internalized shame in unadjusted analyses. In adjusted analyses, the relationship between higher levels of the perceived availability of instrumental support remained significantly associated with lower levels of internalized shame (β: −0.3; 95% CI: −0.5, −0.2; p<0.001), independent of age, poverty, and the perceived availability of emotional support.
Variables associated with antenatal depressive symptoms:
The relationships between demographic and psychosocial constructs, and antenatal depressive symptoms were explored. In unadjusted analyses, significantly higher depression scores were observed among mothers who reported single marital status, an unintended pregnancy, and higher levels of social rejection and internalized shame. In addition, increases in age and in the perceived availability of instrumental and emotional support were significantly associated with lower depression scores (Table 3). When adjusted for age, marital status and pregnancy intention (adjusted model A), the associations between both dimensions of HIV-related stigma and depression scores persisted, as did the associations between both dimensions of social support and depression scores. In a multivariable model adjusted for all other covariates (adjusted model B), maternal age, the report of an unintended pregnancy, and higher levels of social rejection and internalized shame remained significantly associated with depression scores, with a stronger effect observed for internalized shame compared to that observed for social rejection. A one-unit increase in social rejection was associated with a 0.7 unit increase (95% CI: 0.1, 1.3; p=0.025) in depression score; compared to a 1.8 unit increase in depression score (95% CI: 1.2, 2.3; p<0.001) associated with a one-unit increase in internalized shame, independent of marital status, pregnancy intention and the perceived availability of both instrumental and emotional support.
Table 3.
Association between perceived availability of social support, HIV-related stigma, and antenatal depressive symptoms
| Variable | Mean EPDS score (SD) | Unadjusted regression coefficient [95% CI] | P-value | (A) Regression coefficient [95% CI]1 | P-value | (B) Regression coefficient [95% CI]2 | P-value |
|---|---|---|---|---|---|---|---|
| Age | −0.1 [−0.2, −0.002] | 0.044 | −0.1 [−0.1, −0.01] | 0.035 | |||
| Educational attainment | |||||||
| Completed secondary/any tertiary | |||||||
| Primary/some secondary | 5.2 (5.5) 5.3 (5.2) |
Reference 0.1 [−0.8, 1.1] |
0.757 | ||||
| Current employment | |||||||
| Employed | |||||||
| Unemployed | 4.8 (5.1) 5.6 (5.3) |
Reference 0.8 [−0.03, 1.7] |
0.060 | ||||
| Poverty level | |||||||
| Least disadvantaged | |||||||
| Moderately disadvantaged | |||||||
| Most disadvantaged | 4.8 (5.0) 5.2 (5.3) 5.7 (5.4) |
Reference 0.4 [−0.6, 1.5] 0.9 [−0.1, 2.0] |
0.405 0.066 |
||||
| Relationship status | |||||||
| Married/cohabiting | |||||||
| Single | 4.7 (4.8) 5.7 (5.5) |
Reference 1.0 [0.1, 1.8] |
0.023 | Reference 0.6 [−0.2, 1.4] |
0.136 | ||
| Pregnancy intention | |||||||
| Intended | |||||||
| Unintended | 4.3 (4.6) 5.7 (5.5) |
Reference 1.4 [0.5, 2.3] |
0.002 | Reference 1.0 [0.2, 1.9] |
0.018 | ||
| Time of HIV diagnosis | |||||||
| Before this pregnancy | |||||||
| During this pregnancy | 5.3 (5.2) 5.3 (5.3) |
Reference 0.03 [−0.8, 0.9] |
0.949 | ||||
| Perceived availability of support – instrumental | −1.1 [−1.6, −0.6] | <0.001 | −1.1 [−1.6, −0.7] | <0.001 | −0.2 [−0.8, 0.4] | 0.561 | |
| Perceived availability of support – emotional | −0.8 [−1.3, −0.4] | <0.001 | −0.9 [−1.3, −0.4] | <0.001 | −0.04 [−0.6, 0.5] | 0.900 | |
| HIV-related stigma – social rejection | 2.2 [1.7, 2.7] | <0.001 | 2.2 [1.7, 2.7] | <0.001 | 0.7 [0.1, 1.3] | 0.025 | |
| HIV-related stigma – internalized shame | 2.2 [1.8, 2.6] | <0.001 | 2.2 [1.8, 2.6] | <0.001 | 1.8 [1.2, 2.3] | <0.001 |
Regression coefficient [95% CI] adjusted for age, marital status and pregnancy intention;
Regression coefficient [95% CI] adjusted for all other covariates in model
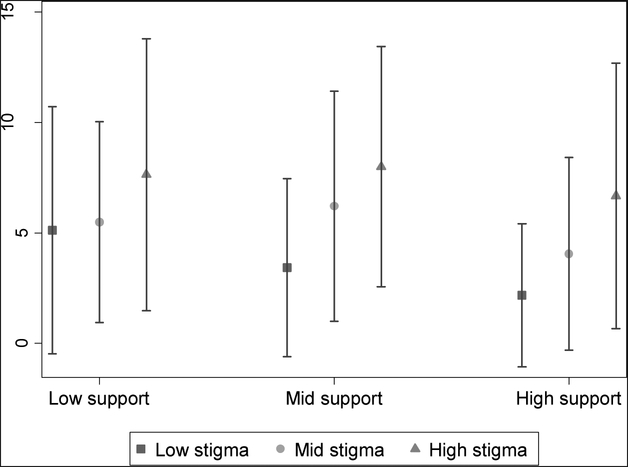
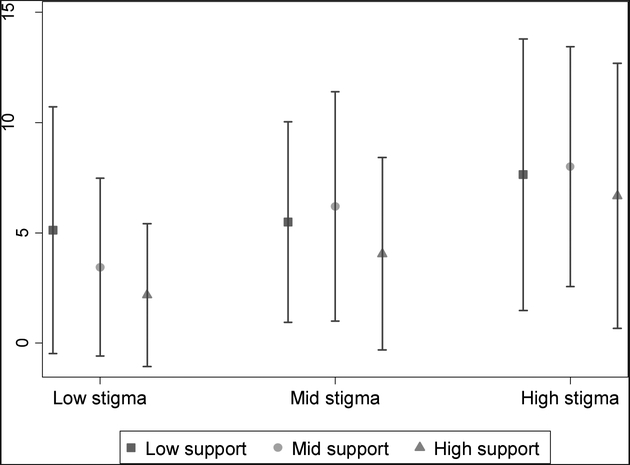
When stratified by tertiles of social support, a clear dose-response relationship was observed between tertiles of HIV-related stigma and increasing depression scores across all levels of social support (Figure 1a). In contrast, a clear dose-response relationship was observed between higher levels of perceived social support and lower depression scores only when HIV-related stigma was low (Figure 1b). At higher levels of stigma, the relationship between social support and depressive symptoms did not persist, suggesting that HIV-related stigma moderates the relationship between social support and depressive symptoms. This same moderating effect was observed when the subscales of social support and HIV-related stigma were examined. Specifically, social rejection and internalized shame were observed to moderate the effects of the perceived availability of instrumental and emotional support on depression scores.
Figure 1a.
Mean (SD) depression score across tertiles of HIV-related stigma, stratified by tertiles of social support
Figure 1b.
Mean (SD) depression score across tertiles of social support, stratified by tertiles of HIV-related stigma
Discussion
This research explored variables associated with the perceived availability of social support and HIV-related stigma in a sample of HIV-infected pregnant women in South Africa, and examined the interrelationships among these factors and antenatal depressive symptoms. Social support and HIV-related stigma were observed to be highly interrelated in this sample, with strong and persistent associations observed between these constructs, and between poverty and decreased levels of instrumental support. A high proportion of participants scored above suggested thresholds on the EPDS, with 1 in 5 women scoring ≥10, and 1 in 10 scoring ≥13. Social rejection and internalized shame were found to be strongly associated with depression scores in this sample, with stronger effects observed for internalized shame. Although associations were observed between social support and depression scores in unadjusted analyses, stigma was observed to moderate this association, with social support only associated with depression scores when low levels of stigma were reported. In contrast, an association between stigma and depression scores was observed at all levels of social support, suggesting that social support does not act as a buffer against the detrimental effects of stigma in this sample.
Although slightly lower than other recently reported estimates among pregnant women in the region [29–31], the proportion of participants with elevated depression scores observed here is concerning, given documented adverse effects on maternal and child health and on HIV-related treatment outcomes. Although much progress has been made in improving maternal physical health, this persistently high prevalence of depressive symptoms suggests that more focus is needed on mental health in this population. The variables associated with depression scores observed here are well-documented risk factors for depression during pregnancy, although here they are described among a population of women among whom a dearth of date exist. As this population grows, understanding and targeting these barriers to optimal mental health will become increasingly important to ensure long-term maternal and child health.
The finding that stigma moderates the relationship between social support and depression scores is notable, and contrasts with previous research conducted among HIV-infected men and women in the Western Cape, South Africa, where both social support and stigma were found to be independently associated with depression [18]. This novel finding highlights the urgent need for interventions to reduce stigma in this context, particularly given its adverse effects in HIV-infected pregnant women who may already be at increased risk of depression. While much progress has been made in the stigma-reduction field, many gaps and challenges remain in developing effective interventions and incorporating them into national HIV programmes [32], and the need for evidence-based interventions has been widely described. Our findings highlight the need for an increased focus on preventive interventions to reduce stigma, particularly given the well-documented adverse effects of antenatal depression and the relative lack of effective treatment resources in LMICs [4, 6]. Although many interventions to increase social support for HIV-infected individuals have been posited, our findings suggest that increasing social support may not be sufficient in contexts where stigma is prevalent, and community- and structural-level approaches to alleviate stigma, which are currently rare [32], are urgently needed.
In this low socioeconomic context, higher levels of poverty were identified as a risk factor for both higher levels of HIV-related stigma and lower levels of social support, and the relationship between poverty and instrumental support persisted in adjusted analyses. For women in adverse socioeconomic circumstances, instrumental support may be lacking if friends and family are similarly living in poverty. Alternatively, women may require additional support to request assistance from friends and family, especially in contexts where stigma is prevalent. Interestingly, the perceived availability of instrumental support had stronger effects on depression scores in unadjusted analyses than did the perceived availability of emotional support. This is consistent with the findings of previous research in KwaZulu-Natal, South Africa [24], and may indicate that structural interventions to alleviate poverty may have a greater impact than interventions to increase emotional social support in these contexts. These interventions may be particularly beneficial among pregnant women, where financial constraints may be compounded by factors such as transport costs when accessing antenatal care, as well as increased household expenses after delivery.
A particular strength of this study is the inclusion of a large sample recruited from a primary care clinic, as the results observed are likely to be generalizable to other communities in the region. In addition, the inclusion of multiple psychological constructs in one analysis and the exploration of the complex interrelationships between them is a novel aspect of the present study, given the dearth of similar data in this context. A limitation of the present analysis, however, is that all of the data included were based on self-report and may be subject to social desirability bias. Although the EPDS has been validated for use as a screening tool in a South African population [28], the use of self-reported depressive symptoms may not reflect the true prevalence of antenatal depression in this population. Since this measure is not a diagnostic assessment, it may additionally be picking up on generalized psychiatric distress, including symptoms of anxiety, even though it was developed specifically as a measure of depression. As this study was a cross-sectional analysis of baseline data, we cannot make inferences regarding causality among these variables. Recent research has demonstrated a dynamic relationship between social support and stigma [33], a finding which warrants further exploration using other longitudinal datasets. In addition, it is possible that depression causes increases in reported stigma as well as decreases in the perceived availability of social support, a hypothesis that we were unable to explore in these cross-sectional data and that has major implications for the development of interventions in this context.
Despite these limitations, the findings from the present study are notable, and add to the literature in several important ways. Few data examining psychosocial risk factors among women initiating ART in the context of Option B+ exist, and the present study is notable in that it explores these constructs in this important population. As increasing numbers of women initiate ART during pregnancy, understanding the psychosocial risk factors faced by these women will become increasingly important, given their possible impact on adherence and retention in care. The present analysis is notable in that it begins to explore these constructs, and highlights the importance of simultaneously considering the associations among multiple psychosocial risk factors and depressive symptoms in order to generate a more nuanced understanding of the complex interrelationships among these constructs. In particular, this analysis highlights the moderating role of HIV-related stigma in the relationship between social support and depressive symptoms in this population. These results suggest that research to identify ways of reducing stigma and increased efforts to alleviate stigma, particularly at the community and structural level, are urgently needed. Finally, these findings suggest that further study of the impact of psychosocial factors on HIV-related outcomes, including ART adherence and retention in care, is needed in this population.
Acknowledgements
The authors would like to thank the women who participated in this study, as well as the study staff for their support of this research. This research was supported by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the National Institute of Child Health and Human Development (NICHD), grant number 1R01HD074558. Additional funding comes from the Elizabeth Glaser Pediatric AIDS Foundation. Drs. Mellins and Remien are also supported by a grant from NIMH to the HIV Center for Clinical and Behavioral Studies (P30-MH45320).
References
- 1.Walker SP, Wachs TD, Meeks Gardner J, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet. 2007; 369(9556):145–57. [DOI] [PubMed] [Google Scholar]
- 2.Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011; 378(9799):1325–38. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization, United Nations Population Fund. Mental health aspects of women’s reproductive health: a global review of the literature. Geneva: World Health Organization; 2009. [Google Scholar]
- 4.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014; 384(9956):1800–19. [DOI] [PubMed] [Google Scholar]
- 5.Brittain K, Myer L, Koen N, et al. Risk factors for antenatal depression and associations with infant birth outcomes: results from a South African birth cohort study. Paediatr Perinat Epidemiol. 2015; 29(6):505–14. [DOI] [PubMed] [Google Scholar]
- 6.Howard LM, Molyneaux E, Dennis C-L, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014; 384(9956):1775–88. [DOI] [PubMed] [Google Scholar]
- 7.Kapetanovic S, Dass-Brailsford P, Nora D, Talisman N. Mental health of HIV-seropositive women during pregnancy and postpartum period: a comprehensive literature review. AIDS Behav. 2014; 18(6):1152–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotze M, Visser M, Makin J, Sikkema K, Forsyth B. Psychosocial variables associated with coping of HIV-positive women diagnosed during pregnancy. AIDS Behav. 2013; 17(2):498–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peltzer K, Ramlagan S. Perceived stigma among patients receiving antiretroviral therapy: a prospective study in KwaZulu-Natal, South Africa. AIDS Care. 2011; 23(1):60–8. [DOI] [PubMed] [Google Scholar]
- 10.Nel A, Kagee A. Common mental health problems and antiretroviral therapy adherence. AIDS Care. 2011; 23(11):1360–5. [DOI] [PubMed] [Google Scholar]
- 11.Krumme AA, Kaigamba F, Binagwaho A, Murray MB, Rich ML, Franke MF. Depression, adherence and attrition from care in HIV-infected adults receiving antiretroviral therapy. J Epidemiol Community Health. 2015; 69(3):284–9. [DOI] [PubMed] [Google Scholar]
- 12.O’Hiarlaithe M, Grede N, de Pee S, Bloem M. Economic and social factors are some of the most common barriers preventing women from accessing maternal and newborn child health (MNCH) and prevention of mother-to-child transmission (PMTCT) services: a literature review. AIDS Behav. 2014; 18(Suppl 5):S516–30. [DOI] [PubMed] [Google Scholar]
- 13.Gourlay A, Birdthistle I, Mburu G, Iorpenda K, Wringe A. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013; 16:18588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodgson I, Plummer ML, Konopka SN, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One. 2014; 9(11):e111421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seth P, Kidder D, Pals S, et al. Psychosocial functioning and depressive symptoms among HIV-positive persons receiving care and treatment in Kenya, Namibia, and Tanzania. Prev Sci. 2014; 15(3):318–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Endeshaw M, Walson J, Rawlins S, et al. Stigma in Ethiopia: association with depressive symptoms in people with HIV. AIDS Care. 2014; 26(8):935–9. [DOI] [PubMed] [Google Scholar]
- 17.Onyebuchi-Iwudibia O, Brown A. HIV and depression in Eastern Nigeria: the role of HIV-related stigma. AIDS Care. 2014; 26(5):653–7. [DOI] [PubMed] [Google Scholar]
- 18.Breet E, Kagee A, Seedat S. HIV-related stigma and symptoms of post-traumatic stress disorder and depression in HIV-infected individuals: does social support play a mediating or moderating role? AIDS Care. 2014; 26(8):947–51. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. Programmatic update: use of antiretroviral drugs for treating pregnant women and preventing HIV infection in infants. Available at: http://www.who.int/hiv/PMTCT_update.pdf. Acessed: September 21, 2015.
- 20.Kaplan R, Orrell C, Lawn SD, Bekker L-G, Wood R. The Hannan Crusaid Treatment Centre - early beginnings and lessons learnt. South Afr J HIV Med. 2014; 15(1):35–7. [Google Scholar]
- 21.Strategic Development Information, City of Cape Town GIS Department. City of Cape Town - Census 2011 - Gugulethu. Available at: http://www.capetown.gov.za/en/stats/2011CensusSuburbs/2011_Census_CT_Suburb_Gugulethu_Profile.pdf. Acessed: September 8, 2015.
- 22.Barrera MA. A method for assessing social support networks in community survey research. Connections. 1980; 3(3):8–13. [Google Scholar]
- 23.Arnsten JH, Li X, Mizuno Y, et al. Factors associated with antiretroviral therapy adherence and medication errors among HIV-infected injection drug users. J Acquir Immune Defic Syndr. 2007; 46(Suppl 2):S64–71. [DOI] [PubMed] [Google Scholar]
- 24.Yeji F, Klipstein-Grobusch K, Newell M-L, Hirschhorn LR, Hosegood V, Barnighausen T. Are social support and HIV coping strategies associated with lower depression in adults on antiretroviral treatment? Evidence from rural KwaZulu-Natal, South Africa. AIDS Care. 2014; 26(12):1482–9. [DOI] [PubMed] [Google Scholar]
- 25.Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000; 41(1):50–67. [PubMed] [Google Scholar]
- 26.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987; 150(6):782–6. [DOI] [PubMed] [Google Scholar]
- 27.Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression scale (EDDS). J Reprod Infant Psychol. 1990; 8(2):99–107. [Google Scholar]
- 28.Lawrie TA, Hofmeyr GJ, de Jager M, Berk M. Validation of the Edinburgh Postnatal Depression Scale on a cohort of South African women. S Afr Med J. 1998; 88(10):1340–4. [PubMed] [Google Scholar]
- 29.Tsai AC, Tomlinson M, Dewing S, et al. Antenatal depression case finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health. 2014; 17(5):423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baron E, Field S, Kafaar Z, Honikman S. Patterns of use of a maternal mental health service in a low-resource antenatal setting in South Africa . Health Soc Care Community. 2015; 23(5):502–12. [DOI] [PubMed] [Google Scholar]
- 31.Schneider M, Baron E, Davies T, Bass J, Lund C. Making assessment locally relevant: measuring functioning for maternal depression in Khayelitsha, Cape Town . Soc Psychiatry Psychiatr Epidemiol. 2015; 50:797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013; 16(3 Suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takada S, Weiser SD, Kumbakumba E, et al. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Ann Behav Med. 2014; 48(1):26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]