Abstract
Objectives
The impact of malpractice concerns on pathologists’ use of defensive medicine and interpretations of melanocytic skin lesions (MSLs) is unknown.
Methods
A total of 207 pathologists interpreting MSLs responded to a survey about past involvement in malpractice litigation, influence of malpractice concerns on diagnosis, and use of assurance behaviors (defensive medicine) to alleviate malpractice concerns. Assurance behaviors included requesting second opinions, additional slides, additional sampling, and ordering specialized tests.
Results
Of the pathologists, 27.5% reported that malpractice concerns influenced them toward a more severe MSL diagnosis. Nearly all (95.2%) pathologists reported practicing at least one assurance behavior due to malpractice concerns, and this practice was associated with being influenced toward a more severe MSL diagnosis (odds ratio, 2.72; 95% confidence interval, 1.41-5.26).
Conclusions
One of four US skin pathologists upgrade MSL diagnosis due to malpractice concerns, and nearly all practice assurance behaviors. Assurance behaviors are associated with rendering a more severe MSL diagnosis.
Keywords: Medical malpractice, Defensive medicine, Assurance behaviors, Skin pathology, Diagnosis, Melanoma, Melanocytic skin lesions
The incidence of melanoma in US whites has risen steadily over the past few decades.1 The American Cancer Society estimated 91,270 new cases of melanoma will be diagnosed in the United States in 2018, and 9,320 individuals will die of the disease.2
At present, complete surgical removal of an early melanoma offers the best chance of curing this disease, underscoring the importance of timely removal and an accurate histopathology diagnosis. Unfortunately, the pathologic interpretation of melanoma is difficult, particularly for melanoma in situ and early invasive melanoma.3,4 Given these challenges, it is not surprising that a missed diagnosis of melanoma has been cited as the most common cause of medical malpractice claims against a pathologist.5 Dermatopathologists rank second highest among all medical specialties for the number of malpractice verdicts exceeding $1,000,000.6 The risk of malpractice for those who interpret melanocytic lesions has been attributed to a variety of factors, including lesion complexity and the difficulty of distinguishing between benign and invasive melanocytic lesions with currently available histopathologic criteria, even among highly skilled dermatopathologists.3,7
To allay concerns about medical malpractice litigation, many physicians practice defensive medicine. Defensive medicine includes the use of assurance behaviors (eg, ordering additional tests, requesting second opinions) that are intended to reduce exposure to malpractice litigation but may not clinically benefit the patient.8 The use of assurance behaviors is thought to be widespread in the United States and appears to be increasing.9 National surveys indicate that 88% to 91% of physicians practice defensive medicine or assurance behaviors to reduce their risk of malpractice litigation.10-12 In addition, in a recent survey, 41% of medical students and 53% of medical residents reported being taught assurance behaviors by an attending physician.13
We previously reported that a third of participating pathologists who regularly interpret melanocytic skin lesions (MSLs) had past experience with malpractice litigation and that this experience was not associated with the use of assurance behaviors.14 The present report expands our past investigation in two important areas. First, we examine whether pathologists’ concerns about medical malpractice influence the direction of their diagnosis when interpreting MSLs and, specifically, whether medical malpractice concerns result in upgrading an MSL diagnosis. Second, we evaluate an array of pathologist characteristics, including past malpractice experience and the use of assurance behaviors in relation to the influence of malpractice concerns on the direction of MSL diagnosis.
Materials and Methods
Study Design and Procedures
The present analysis uses data from the Melanoma Pathology Study (M-Path), a study of pathologists who interpret MSLs, including benign nevi, dysplastic nevi, and melanoma. The M-Path study methods have been detailed elsewhere.4 Briefly, we invited participants from 10 states (California, Connecticut, Hawaii, Iowa, Kentucky, Louisiana, New Jersey, New Mexico, Utah, and Washington). Eligibility criteria included completion of residency training and/or fellowship training, interpretation of MSLs within the previous year, expected continuation of interpreting MSLs for at least the following 2 years, and verifiable address of practice location. Of 450 pathologists contacted to participate in the survey, 110 were not eligible, 39 declined without determination of their eligibility status, and 301 confirmed they were eligible to participate, of whom 207 (68.8%) actively enrolled in the study.
Consenting pathologists completed an online survey that elicited general demographic and professional information, including clinical training, perceptions, and experience, including past involvement in medical malpractice litigation. Pathologists were asked to agree/disagree with the following statements regarding how medical malpractice concerns affect their own practice: “I request additional slides cut from the block,” “I recommend additional surgical sampling,” “I request second opinions,” and “I order additional tests such as IHC or molecular tests” (ie, assurance behaviors). Survey response options for the assurance behaviors were formatted using a 6-point Likert scale (slightly disagree, disagree, strongly disagree, strongly agree, agree, slightly agree). We also asked pathologists to report whether the direction of their diagnosis of MSLs was influenced by concerns about medical malpractice. Three response options were available: influence toward a less severe diagnosis, no influence on diagnosis, and influence toward a more severe diagnosis. A full copy of the M-Path survey has been published previously.14
Institutional review board approval for all study procedures was obtained from the University of Washington, Fred Hutchinson Cancer Research Center, Oregon Health & Sciences University, Rhode Island Hospital, and Dartmouth College.
Statistical Analysis
Pathologists’ responses to individual survey questions on use of assurance behaviors were classified as yes (slightly agree, agree, strongly agree), indicating use of the assurance behavior, vs no (slightly disagree, disagree, strongly disagree), indicating nonuse of the assurance behavior. Due to small cell sizes, which precluded multivariable modeling, we created a composite variable representing use of at least one of the four assurance behaviors; however, applying the same “yes” and “no” categories used for the individual assurance behaviors proved infeasible due to a zero cell. After exploring possible options, we constructed a composite variable in which “yes” corresponded to “strongly agree” and “no” represented all other response categories combined. This approach, which was included in the multivariable model, produced the most stable (narrowest confidence intervals) and the most conservative results (smallest odds ratio).
With regard to the outcome variable (ie, the direction of influence of MSL diagnosis due to concerns about medical malpractice), most pathologists reported either no influence on diagnosis or being influenced toward a more severe diagnosis; only three pathologists indicated influence toward a less severe diagnosis. Consequently, the primary outcome was dichotomized as “influence toward a more severe diagnosis” vs “no influence”; the latter category included the three pathologists who reported being influenced toward a less severe diagnosis.
We used frequency distributions to display the percentage of pathologists reporting that concerns about medical malpractice had no influence on their MSL diagnosis or influenced them toward a more severe diagnosis (the outcome). Simple (unadjusted) logistic regression models explored pathologist characteristics, including past personal involvement in MSL-related malpractice litigation and the use of assurance behaviors, in relation to the outcome. Variables associated with the outcome at P ≤ .10 in the unadjusted logistic models were included in a multivariable logistic regression model that controlled for potential confounding, thereby identifying variables that were independently associated with the outcome. Correlation matrices were used to identify correlated variables. Firth’s bias reduction penalized-likelihood approach was used to obtain estimates of regression parameters, confidence intervals, and P values.15 All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC).
Results
As shown in Table 1 , of the 207 participating pathologists, 57 (27.5%) reported they were influenced toward a more severe MSL diagnosis by concerns about medical malpractice, and 150 (72.5%) were not influenced toward a more severe diagnosis.
Table 1.
Unadjusted ORs and 95% CIs for the Associations Between Pathologist Demographics, Training, and Clinical Experience and Influence Toward a More Severe MSL Diagnosis Due to Concerns About Medical Malpractice (n = 207)a
| Pathologist Characteristic | All Pathologists, No. (%) | Influence Toward a More Severe Diagnosis, No. (%) | No Influence on Diagnosis, No. (%) | OR (95% CI)b | P Value |
|---|---|---|---|---|---|
| Total | 207 (100.0) | 57 (27.5) | 150 (72.5) | ||
| Demographics | |||||
| Age, y | .007 | ||||
| <50 | 95 (45.9) | 35 (36.8) | 60 (63.2) | Reference | |
| ≥50 | 112 (54.1) | 22 (19.6) | 90 (80.4) | 0.42 (0.23-0.79) | |
| Sex | .13 | ||||
| Male | 123 (59.4) | 29 (23.6) | 94 (76.4) | Reference | |
| Female | 84 (40.6) | 28 (33.3) | 56 (66.7) | 1.62 (0.87-2.99) | |
| Training and clinical experience | |||||
| Residency training | .10 | ||||
| Anatomic/clinical pathology | 186 (89.9) | 48 (25.8) | 138 (74.2) | Reference | |
| Dermatology | 21 (10.1) | 9 (42.9) | 12 (57.1) | 2.17 (0.86-5.47) | |
| Fellowship training/board certification | .81 | ||||
| Otherc | 126 (60.9) | 34 (27.0) | 92 (73.0) | Reference | |
| Dermatopathologyd | 81 (39.1) | 23 (28.4) | 58 (71.6) | 1.08 (0.58-2.00) | |
| Years interpreting MSLs | <.001 | ||||
| <20 | 143 (69.1) | 50 (35.0) | 93 (65.0) | Reference | |
| ≥20 | 64 (30.9) | 7 (10.9) | 57 (89.1) | 0.24 (0.10-0.56) | |
| MSL volumee | .32 | ||||
| <35 | 76 (36.7) | 24 (31.6) | 52 (68.4) | Reference | |
| ≥35 | 131 (63.3) | 33 (25.2) | 98 (74.8) | 0.73 (0.39-1.36) | |
| Total number of MSLs (per month)e | |||||
| Mean (SD) | 125 (178.0) | 111 (131.5) | 131 (192.9) | 1.00 (0.99-1.01)f | .58 |
| For what percentage of MSLs is your final assessment that the diagnosis is borderline or uncertain? | .28 | ||||
| None | 21 (10.1) | 3 (14.3) | 18 (85.7) | Reference | |
| 1%-4% | 93 (44.9) | 24 (25.8) | 69 (74.2) | 1.86 (0.53-6.55) | |
| ≥5% | 93 (44.9) | 30 (32.3) | 63 (67.7) | 2.54 (0.73-8.84) | |
| Have you ever been named in a medical malpractice suit | .70 | ||||
| Never been sued | 139 (67.1) | 41 (29.5) | 98 (70.5) | Reference | |
| Yes, related to MSL | 12 (5.8) | 3 (25.0) | 9 (75.0) | 0.87 (0.23-3.30) | |
| Yes, not related to MSL | 56 (27.1) | 13 (23.2) | 43 (76.8) | 0.74 (0.36-1.51) | |
CI, confidence interval; MSL, melanocytic skin lesion; OR, odds ratio; SD, standard deviation.
aPercentages may not total 100 due to rounding.
bFirth’s bias reduction method based on penalized likelihood (addresses issues of separability, small sample sizes, and bias of the parameter estimates). Wald χ2 statistics were used to test the effect each independent coefficient had on the direction of influence.
cIncludes fellowships or board certifications in surgical pathology, cytopathology, or hematopathology.
dPathologists in this category have single or multiple certifications/fellowship training, including dermatopathology.
eSum of number of melanomas + benign MSLs interpreted per month.
fOdds ratio for every 5-unit increment in number of MSLs per month.
Results of Unadjusted Logistic Regression Models
Pathologists’ demographic and clinical characteristics are shown in Table 1. Most pathologists (54.1%) were at least 50 years of age and male (59.4%). Most had residency training in anatomic or clinical pathology (89.9%). Fewer than half were fellowship trained or board certified in dermatopathology (39.1%) or had 20 or more years of experience interpreting MSL (30.9%). Most reported reviewing 35 or more MSLs per month (63.3%), and nearly all assessed some of their MSL caseload as borderline (89.8%). A minority (5.8%) had been named in an MSL-related malpractice lawsuit.
The results of unadjusted logistic regression models suggested that pathologists with dermatology residency training, compared with pathology residency, were more likely to render a more severe MSL diagnosis due to concern about medical malpractice (odds ratio [OR], 2.17; 95% confidence interval [CI], 0.86-5.47). Two variables, older age and more years of experience interpreting MSL, strongly reduced the likelihood of rendering a more severe diagnosis due to malpractice concerns; the unadjusted ORs were 0.42 (95% CI, 0.23-0.79) for age 50 years or older, compared with a younger age, and 0.24 (95% CI, 0.10-0.56) for at least 20 years of MSL experience, compared with fewer years. Age and years of MSL interpretative experience were highly correlated (r = 0.72; P < .001), precluding simultaneous multivariable assessment; we elected years of experience for inclusion in the multivariable model due to its greater clinical relevance. The remaining pathologist characteristics, including sex, two variables representing the volume of MSL caseload, assessing lesions as borderline, dermatopathology fellowship training and/or board certification, and having been named previously in an MSL-related lawsuit, were not associated (P > .10) with rendering a more severe diagnosis due to malpractice concerns.
Survey items assessing pathologists’ perceptions about interpreting MSL are summarized in Table 2 . Most pathologists (69.6%) found interpreting MSLs enjoyable, and nearly all (96.1%) found MSL lesions challenging. Most pathologists reported being more nervous interpreting MSLs than other pathology (70.5%), were concerned about patient safety and potential harm to patients resulting from their MSL assessments (74.9%), and were confident in their MSL assessments (86%). Fewer than half (40.6%) believed too many MSL were biopsied, and slightly more than half (52.7%) thought pathologists were overcalling some benign lesions as melanoma. Most pathologists agreed that obtaining a second opinion protected them from lawsuits (86.0%).
Table 2.
Unadjusted ORs and 95% CIs for the Associations Between Pathologist Perceptions and Influence Toward a More Severe MSL Diagnosis Due to Concerns About Medical Malpractice (n = 207)a
| Perceptions: What Are Your Thoughts on Interpreting MSLs?b | All Pathologists, No. (%) | Influence Toward a More Severe Diagnosis, No. (%) | No Influence on Diagnosis, No. (%) | OR (95% CI)c | P Value |
|---|---|---|---|---|---|
| Total | 207 (100.0) | 57 (27.5) | 150 (72.5) | ||
| Interpreting melanocytic skin lesions is enjoyable | .56 | ||||
| No | 63 (30.4) | 19 (30.2) | 44 (69.8) | Reference | |
| Yes | 144 (69.6) | 38 (26.4) | 106 (73.6) | 0.83 (0.43-1.58) | |
| In general, melanocytic skin lesions are challenging to interpret | .48 | ||||
| No | 8 (3.9) | 1 (12.5) | 7 (87.5) | Reference | |
| Yes | 199 (96.1) | 56 (28.1) | 143 (71.9) | 1.97 (0.30-12.96) | |
| Interpreting melanocytic skin lesions makes me more nervous than other types of pathology | .058 | ||||
| No | 61 (29.5) | 11 (18.0) | 50 (82.0) | Reference | |
| Yes | 146 (70.5) | 46 (31.5) | 100 (68.5) | 2.03 (0.98-4.23) | |
| I am concerned about patient safety and potential harm to patients that may result from my assessment of melanocytic skin lesions | .07 | ||||
| No | 52 (25.1) | 9 (17.3) | 43 (82.7) | Reference | |
| Yes | 155 (74.9) | 48 (31.0) | 107 (69.0) | 2.07 (0.94-4.53) | |
| In general, too many melanocytic skin lesions are being biopsied | .066 | ||||
| No | 123 (59.4) | 28 (22.8) | 95 (77.2) | Reference | |
| Yes | 84 (40.6) | 29 (34.5) | 55 (65.5) | 1.78 (0.96-3.29) | |
| In general, pathologists are overcalling some benign lesions as melanoma | >.99 | ||||
| No | 98 (47.3) | 27 (27.6) | 71 (72.4) | Reference | |
| Yes | 109 (52.7) | 30 (27.5) | 79 (72.5) | 1.00 (0.54-1.83) | |
| In general, I am confident in my assessments of melanocytic skin lesionsd | .94 | ||||
| No | 29 (14.0) | 8 (27.6) | 21 (72.4) | Reference | |
| Yes | 178 (86.0) | 49 (27.5) | 129 (72.5) | 0.97 (0.40-2.31) | |
| Requesting second opinions protects me from malpractice suits | .43 | ||||
| No | 29 (14.0) | 6 (20.7) | 23 (79.3) | Reference | |
| Yes | 178 (86.0) | 51 (28.7) | 127 (71.3) | 1.46 (0.57-3.74) | |
CI, confidence interval; MSL, melanocytic skin lesion; OR, odds ratio.
aPercentages may not total 100 due to rounding.
b“No” is defined by Likert scale responses disagree (slightly disagree, disagree, strongly disagree) and “yes” is defined by agree (slightly agree, agree, strongly agree). Pathologists reported how challenging they found melanocytic skin lesions to interpret based on a 6-point Likert scale ranging from 1 (“very easy”) to 6 (“very challenging”). When pathologists were asked if they felt melanocytic skin lesions were challenging to interpret, a “No” response is defined by Likert scale responses 1, 2, 3 and “Yes” is defined by Likert scale responses 4, 5, 6. Pathologists also reported how confident they were in their assessments of melanocytic skin lesions based on a 6-point Likert scale ranging from 1 (“very confident”) to 6 (“not at all confident”). When pathologists were asked if they were confident in their assessments of melanocytic skin lesions, a “No” response is defined by Likert scale responses 4, 5, 6 and “Yes” is defined by Likert scale responses 1, 2, 3. For all other responses, “No” is defined by Likert scale responses disagree (slightly disagree, disagree, strongly disagree) and “Yes” is defined by agree (slightly agree, agree, strongly agree).
cFirth’s bias reduction method based on penalized likelihood (addresses issues of separability, small sample sizes, and bias of the parameter estimates). Wald χ2 statistics were used to test the effect each independent coefficient had on the direction of influence.
dReference reversed to be consistent with questions in which disagree is the reference for a positive response.
The results of unadjusted logistic regression models suggested that being more nervous about interpreting MSLs (OR, 2.03; 95% CI, 0.98-4.23), concern about patient safety and harm (OR, 2.07; 95% CI, 0.94-4.53), and agreeing that too many skin lesions are biopsied (OR, 1.78; 95% CI, 0.96-3.29) were positively associated with being influenced toward a more severe MSL diagnosis by malpractice concerns at P ≤ .10. Due to a strong correlation between being more nervous about interpreting MSLs and concern about patient safety/harm (r = 0.38; P < .001), precluding simultaneous assessment of these variables, we elected concern about patient safety/harm for inclusion in the multivariable model due to its greater clinical significance and relevance to medical malpractice. The remaining variables, including pathologists’ perceptions that interpreting MSLs is enjoyable and challenging, overcalling benign lesions as melanoma, pathologists’ confidence when assessing MSLs, and perceiving second opinions as protecting against malpractice lawsuits, were not associated (P > .10) with the outcome.
Assurance behaviors practiced to reduce concerns about malpractice when interpreting MSL are summarized in Table 3 . Due to concerns about malpractice, 87.0% of pathologists reported they requested additional slides, 66.2% requested additional surgical sampling, 92.3% requested a second opinion, and 62.3% ordered additional molecular testing. Nearly all, 95.2%, of pathologists reported practicing at least one of the four measured assurance behaviors.
Table 3.
Unadjusted ORs and 95% CIs for the Associations Between Pathologist Practice of Assurance Behaviors and Influence Toward a More Severe MSL Diagnosis Due to Concerns About Medical Malpractice (n = 207)a
| How Do Medical Malpractice Concerns Affect Your Own Practice When Interpreting MSLs? | All Pathologists, No. (%) | Influence Toward a More Severe Diagnosis, No. (%) | No Influence on Diagnosis, No. (%) | OR (95% CI)b | P Value |
|---|---|---|---|---|---|
| Total | 207 (100.0) | 57 (27.5) | 150 (72.5) | ||
| 1. I request additional slides cut from the block | .017 | ||||
| No | 27 (13.0) | 1 (3.7) | 26 (96.3) | Reference | |
| Yes | 180 (87.0) | 56 (31.1) | 124 (68.9) | 8.02 (1.46-44.11) | |
| 2. I recommend additional surgical sampling | .047 | ||||
| No | 70 (33.8) | 13 (18.6) | 57 (81.4) | Reference | |
| Yes | 137 (66.2) | 44 (32.1) | 93 (67.9) | 2.03 (1.01-4.07) | |
| 3. I request second opinions | .10 | ||||
| No | 16 (7.7) | 1 (6.3) | 15 (93.8) | Reference | |
| Yes | 191 (92.3) | 56 (29.3) | 135 (70.7) | 4.31 (0.74-24.92) | |
| 4. I order additional tests such as IHC and or molecular tests | .16 | ||||
| No | 78 (37.7) | 17 (21.8) | 61 (78.2) | Reference | |
| Yes | 129 (62.3) | 40 (31.0) | 89 (69.0) | 1.59 (0.83-3.05) | |
| Composite variable for assurance behaviors | |||||
| Practiced at least one of four assurance behaviors (strongly agree vs all other responses) | .002 | ||||
| No (disagree/slightly disagree, agree/slightly agree) | 131 (63.3) | 26 (19.8) | 105 (80.2) | Reference | |
| Yes (strongly agree) | 76 (36.7) | 31 (40.8) | 45 (59.2) | 2.76 (1.47-5.15) | |
CI, confidence interval; IHC, immunohistochemistry; MSL, melanocytic skin lesion; OR, odds ratio.
aPercentages may not total 100 due to rounding. Except where noted, “no” is defined by Likert scale responses disagree (slightly disagree, disagree, strongly disagree) and “yes” is defined by agree (slightly agree, agree, strongly agree).
bFirth’s bias reduction method based on penalized likelihood (addresses issues of separability, small sample sizes, and bias of the parameter estimates). Wald χ2 statistics were used to test the effect each independent coefficient had on the direction of influence.
In unadjusted logistic regression models, three of the four assurance practices were associated (P ≤ .10) with rendering a more severe MSL diagnosis due to malpractice concerns; the ORs were 8.02 (95% CI, 1.46-44.11) for requesting additional slides cut from the block, 2.03 (95% CI, 1.01-4.07) for recommending additional surgical sampling, and 4.31 (95% CI, 0.74-24.92) for requesting second opinions. Ordering additional tests was not associated (P > .10) with the outcome. The composite assurance variable in which “strongly agree” was compared with all other response categories was significantly associated with being influenced toward a more severe MSL diagnosis by malpractice concerns (OR, 2.76; 95% CI, 1.47-5.15).
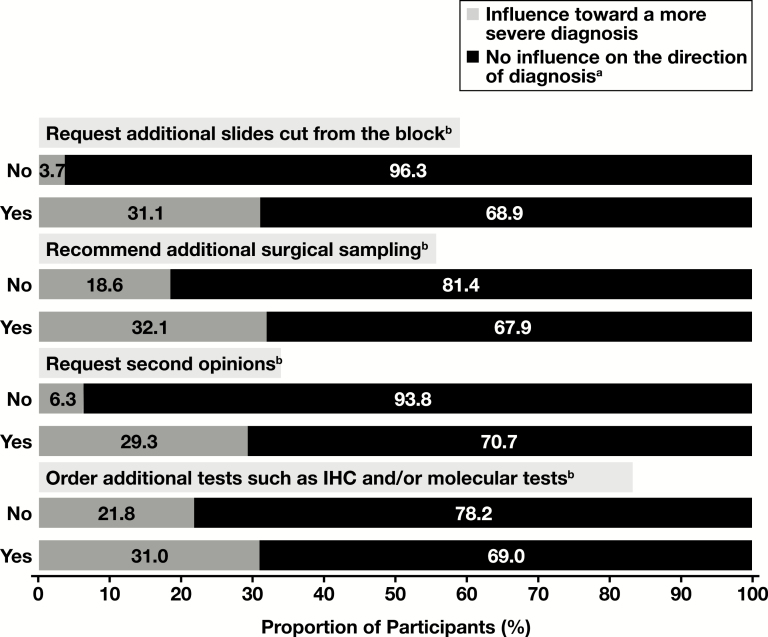
Figure 1 displays the proportion of pathologists whose MSL diagnoses were influenced (or not) by malpractice concerns according to their use (yes) or nonuse (no) of assurance behaviors. As shown, for each of the four individual assurance behaviors, the proportion of pathologists reporting that their MSL diagnoses were influenced toward a more severe diagnosis was consistently higher among those who practice the assurance behavior than among those who do not. The difference in proportions was greatest for requesting additional slides from the tissue block; influence toward a more severe MSL diagnosis due to medical malpractice concerns was reported by 3.7% of those who do not request additional slides due to concerns about medical malpractice and by 31.1% of those who do request additional slides.
Figure 1.
Pathologists’ use of assurance behaviors (no/yes) due to malpractice concerns and the influence of malpractice concerns on the direction of their melanocytic skin lesion diagnosis, based on self-report (n = 207). aIncludes three pathologists who reported influence toward a less severe diagnosis. b“No” is defined by Likert responses “slightly disagree,” “disagree,” and “strongly disagree.” “Yes” is defined by Likert responses “strongly agree,” “agree,” and “slightly agree.”
Results of the Multivariable Logistic Regression Model
To control for possible confounding and identify pathologist characteristics that were independently related to rendering a more severe diagnosis, variables associated with the outcome at P ≤ .10 in simple, unadjusted logistic models were entered into a multivariable model Table 4 . These variables included dermatology residency training, years of experience interpreting MSLs (≥20 vs <20), concern about patient safety/harm that might result from their assessment of MSLs, being of the opinion that too many MSLs are biopsied, and the composite variable representing the use of at least one assurance behavior.
Table 4.
Adjusted ORs and 95% CIs for the Associations Between Pathologist Characteristics and Influence Toward a More Severe MSL Diagnosis Due to Concerns About Medical Malpracticea
| Pathologist Characteristic | OR (95% CI) | P Value |
|---|---|---|
| Residency training | ||
| Anatomic/clinical pathology | Reference | |
| Dermatology | 1.65 (0.61-4.43) | .32 |
| Years interpreting MSL | ||
| <20 | Reference | |
| ≥20 | 0.29 (0.12-0.69) | .005 |
| I am concerned about patient safety and potential harm to patients that may result from my assessment of melanocytic skin lesions | ||
| Disagree | Reference | |
| Agree | 1.74 (0.76-3.98) | .19 |
| In general, too many melanocytic skin lesions are being biopsied | ||
| Disagree | Reference | |
| Agree | 1.58 (0.81-3.08) | .18 |
| Composite assurance variableb | ||
| None | Reference | |
| Strongly agrees with practicing at least one of four assurance behaviors | 2.72 (1.41-5.26) | .003 |
CI, confidence interval; MSL, melanocytic skin lesion; OR, odds ratio.
aResults based on a multivariable logistic regression model containing the terms shown in the model. Variables chosen for multivariable modeling were those associated with influence toward a more severe diagnosis at P ≤ .10 in simple logistic models. The OR for each variable is adjusted for all other terms in the table.
bAssurance behaviors include requesting additional slides from the block, recommending additional surgical sampling, requesting second opinions, and ordering additional tests such as immunohistochemistty and other molecular tests.
The results of the multivariable model indicated that pathologists with at least 20 years of experience interpreting MSLs, compared to those with less than 20 years’ experience, were substantially less likely to report rendering a more severe MSL diagnosis due to concerns about medical malpractice (OR, 0.29; 95% CI, 0.12-0.69; P = .005) (Table 4). In addition, pathologists who strongly agreed that they practiced at least one of four assurance behaviors, compared with those who did not, were nearly three times as likely to report being influenced toward a more severe MSL diagnosis (OR, 2.72; 95% CI, 1.41-5.26; P = .003). Other factors that were associated with rendering a more severe MSL diagnosis due to malpractice concerns in the simple, unadjusted models were not associated with the outcome when mutually adjusted.
Finally, due to our special interest in malpractice, we conducted a separate multivariable analysis to assess past experience with MSL malpractice litigation in relation to upgrading to a more severe diagnosis due to malpractice concerns. In this analysis, experience with MSL-related malpractice litigation was compared with a reference group containing those without malpractice experience or with malpractice experience unrelated to MSL. After adjustment for the same variables described above, excluding years of MSL experience, with which malpractice involvement was correlated (r = 0.19; P = .006), the OR was 0.82 (95% CI, 0.21-3.25) for the association between past malpractice experience and upgrading to a more severe MSL diagnosis.
Discussion
Although national rates of medical malpractice lawsuits and paid claims have decreased since the early 1990s, indemnity payments have increased,16,17 and physicians’ malpractice concerns remain widespread.18 In pathology, the temporal increase of average indemnity payments from 1992 to 2014 is greater than in any other specialty.16 Despite the fact that melanoma misdiagnosis is a leading cause of pathology malpractice litigation,19-21 previous studies have not addressed the influence of malpractice concerns on pathologists’ interpretation of MSLs.
In our study of pathologists from 10 US states, roughly one (28%) of four pathologists reported being influenced toward a more severe MSL diagnosis due to concern about medical malpractice litigation. In addition, nearly all pathologists (95%) self-reported practicing at least one assurance behavior due to malpractice concerns. A juxtaposition of these two findings suggests the practice of assurance behaviors is a more common strategy for alleviating malpractice concerns than rendering a more severe MSL diagnosis.
Our data indicated an association between using assurance behaviors and rendering a more severe MSL diagnosis due to malpractice concerns. This association was expected, as upgrading a diagnosis can be viewed as a form of assurance behavior. We also found that pathologists with at least 20 years of experience interpreting MSLs were less likely to report having their diagnoses influenced by malpractice concerns, possibly reflecting greater confidence due to longer term experience. Although our data showed no association between actual malpractice experience and upgrading MSL diagnoses due to malpractice concerns, this result should be interpreted cautiously due to the small number of pathologists with malpractice experience and limited statistical power for that analysis.
The questions used in our analysis specifically asked pathologists about the influence of malpractice concerns on their use of assurance behaviors and the direction of diagnostic interpretation. It is highly likely that these behaviors are also motivated by concerns about patient safety, but we did not assess whether patient safety concerns directly influenced the use of assurance behaviors or the direction of MSL diagnosis, topics that merit future study. Other limitations of this study include the use of self-reported data on diagnostic practices, as opposed to actual practice data. In addition, it is outside the scope of this study to determine the extent to which these practices might inflate health care costs, bring benefit to patients by reducing underdiagnosis, or cause harm to patients due to unnecessary treatment. Similarly, it is outside the scope of this study to assess the possible impact of malpractice concerns on possible melanoma overdiagnosis. Strengths of our study include the large number of pathologists in the study and the spectrum of pathologists surveyed, both in terms of the nature of their clinical training and practices and in geographic location. Nevertheless, our data may not be generalizable to all US pathologists or to those outside of the United States.
Conclusions
In summary, we found that one in four pathologists reported that their interpretation of MSLs was influenced toward a more severe MSL diagnosis by malpractice concerns. Pathologists with more years of MSL experience were less likely to report the influence of malpractice concerns on their diagnoses. More than 95% of pathologists reported practicing at least one of four assurance behaviors, and those who did were more likely to be influenced toward a more severe MSL diagnosis by malpractice concerns. Past personal experience with an MSL-related malpractice lawsuit was not associated with self-reported upgrading of MSL diagnoses due to concerns about malpractice, although numbers were limited for this analysis.
This work was supported by the National Cancer Institute (R01 CA151306 and R01 CA201376). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
David E. Elder reports consulting for Myriad Genetics and SciBase.
References
- 1. Welch HG, Woloshin S, Schwartz LM. Skin biopsy rates and incidence of melanoma: population based ecological study. BMJ. 2005;331:481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Cancer Society. Key statistics for melanoma skin cancer 2017. https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html. Accessed January 15, 2018. [Google Scholar]
- 3. Lott J, Boudreau D, Barnhill R, et al. Population-based analysis of histologically confirmed melanocytic proliferations using natural language processing. JAMA Dermatol. 2018;154:24-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Elmore JG, Barnhill RL, Elder DE, et al. Pathologists’ diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study. BMJ. 2017;357:j2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Troxel DB. Trends in pathology malpractice claims. Am J Surg Pathol. 2012;36:e1-e5. [DOI] [PubMed] [Google Scholar]
- 6. Krader CG. Technical acumen, interpersonal skills influence medicolegal risk. Dermatology Times [Internet]. May 8, 2012. [Google Scholar]
- 7. Marsch A, High WA. Medicolegal issues with regard to melanoma and pigmented lesions in dermatopathology. Dermatol Clin. 2012;30:593-615, v. [DOI] [PubMed] [Google Scholar]
- 8. Hermer LD, Brody H. Defensive medicine, cost containment, and reform. J Gen Intern Med. 2010;25:470-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Summerton N. Trends in negative defensive medicine within general practice. Br J Gen Pract. 2000;50:565-566. [PMC free article] [PubMed] [Google Scholar]
- 10. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170:1081-1083. [DOI] [PubMed] [Google Scholar]
- 11. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609-2617. [DOI] [PubMed] [Google Scholar]
- 12. Reisch LM, Carney PA, Oster NV, et al. Medical malpractice concerns and defensive medicine: a nationwide survey of breast pathologists. Am J Clin Pathol. 2015;144:916-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O’Leary KJ, Choi J, Watson K, et al. Medical students’ and residents’ clinical and educational experiences with defensive medicine. Acad Med. 2012;87:142-148. [DOI] [PubMed] [Google Scholar]
- 14. Carney PA, Frederick PD, Reisch LM, et al. How concerns and experiences with medical malpractice affect dermatopathologists’ perceptions of their diagnostic practices when interpreting cutaneous melanocytic lesions. J Am Acad Dermatol. 2016;74:317-24; quiz 324.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Firth D. Bias reduction of maximum-likelihood-estimates. Biometrika. 1993;80:27-38. [Google Scholar]
- 16. Schaffer AC, Jena AB, Seabury SA, et al. Rates and characteristics of paid malpractice claims among US physicians by specialty, 1992-2014. JAMA Intern Med. 2017;177:710-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paik M, Black B, Hyman DA. The receding tide of medical malpractice litigation: part I—national trends. J Empirical Legal Stud. 2013;10:612-638. [Google Scholar]
- 18. Carrier ER, Reschovsky JD, Mello MM, et al. Physicians’ fears of malpractice lawsuits are not assuaged by tort reforms. Health Aff (Millwood). 2010;29:1585-1592. [DOI] [PubMed] [Google Scholar]
- 19. Marsch A, High WA. Medicolegal issues with regard to melanoma and pigmented lesions in dermatopathology. Dermatol Clin. 2012;30:593-615, v. [DOI] [PubMed] [Google Scholar]
- 20. Troxel DB. Medicolegal aspects of error in pathology. Arch Pathol Lab Med. 2006;130:617-619. [DOI] [PubMed] [Google Scholar]
- 21. Kornstein MJ, Byrne SP. The medicolegal aspect of error in pathology: a search of jury verdicts and settlements. Arch Pathol Lab Med. 2007;131:615-618. [DOI] [PubMed] [Google Scholar]