Abstract
To investigate the protective mechanism of verbenalin on cerebral ischemia-reperfusion injury. Middle cerebral artery occlusion in the left hemisphere was induced in rats by filament insertion, and rat model of focal cerebral ischemia-reperfusion was established. The high, medium and low dose of verbenalin groups were injected in the tail vein of corresponding drugs 10 min before reperfusion, and submitted for 22 h of reperfusion after the operation. Mortality rate was then calculated, and neurological deficits of rats were scored. The serum of rats was got to determine the S-100β protein level, and the brain tissue was removed to determine the levels of Bax, Bcl-2, Caspase-3 and ATPase. TTC staining was performed on the brain tissue to calculate the percentage of cerebral infarct size. Changes in brain tissue morphology were observed. Rat model of focal cerebral ischemia-reperfusion was successfully replicated. In groups that have taken different doses of verbenalin, the mortality rate, neurological deficit score and the percentage of cerebral infarction size were significantly reduced, and the levels of Bax, Caspase-3, S-100β level of the serum in the brain tissue were also significantly reduced. Increases in the levels of Bcl-2 and ATPase in brain tissue and improvement of pathological damage of hippocampus and cortex were observed. Verbenalin can inhibit the expression of apoptosis genes, promote the expression of anti-apoptosis genes, improve brain microcirculation and energy metabolism, hence reducing cerebral ischemia-reperfusion injury.
Keywords: Verbenalin, Focal cerebral ischemia-reperfusion, Apoptosis
1. Introduction
Effective ingredients in traditional Chinese medicine and a single herb medicine can be used to prevent or cure various diseases on multiple procedures and multiple targets through multiple channels. Success has been observed in reducing cerebral ischemia-reperfusion injury, indicating Chinese medicine’s advantages in the area. “Huoxue Huayu (promoting blood circulation to dispel blood stasis)” is a common method to prevent and treat cerebral ischemic injury in clinical practices, and its remarkable effect has been widely acknowledged. “Qingre Jiedu (clearing heat and detoxification)” is a new approach in traditional Chinese medicine to prevent and treat cerebral ischemic injury. Chinese medicine and modern medicine share insights and mechanisms on cerebral ischemic injury in microcirculation and clinical research. Huoxue Huayu medicine focus on improving the brain circulation, protect neurons and remove free radicals while Qingre Jiedu medicine focus on alleviating inflammation, activating self-protection mechanism of brain cells and reducing cerebral ischemic secondary reaction. The combination of Huoxue Huayu and Qingre Jiedu medicine to prevent and treat cerebral ischemia-reperfusion injury provide the best combination point for traditional Chinese medicine and modern medicine in clinical practices. Preliminary studies have proved the positive effect of traditional Chinese medicine with effects of promoting blood circulation and detoxification such as turmeric, rabdosia rubescens, Ilex pubescens, Campsis grandiflora, bidens grass, motherwort in treating cerebral ischemic injury (Gohar et al., 2017, Ishaq and Jafri, 2017).
Verbena (Verbena officinalis Linn) is a verbena plant under verbenaceae with effects of promoting blood circulation to dispel stasis, curing malaria, detoxification, relieving swelling, and it has pharmacological effects such as anti-inflammation and painkilling, immune regulation and neurological protection. Studies have shown that verbena could significantly improve the damage of hippocampal CA1 area of rats in focal cerebral ischemia-reperfusion, increase the survival rate of neurons and prolong the survival time of hypoxic rats with nitrite poisoning.
In this study, by observing the intervention role verbenalin, the effective ingredient of verbena plays in rat model of focal cerebral ischemia-reperfusion, we studied the pharmacological effects of verbenalin on cerebral ischemia-reperfusion injury. We identified the intervention mechanism and laid the experimental basis for follow-up studies, with a view to develop new drugs to mitigate cerebral ischemia-reperfusion injury.
2. Material and methods
2.1. Animal
The experiments were performed using 96 males, SPF level, male KM rats, each weighing between 25 and 30 g. Rats were provided by Shandong Lu Kang Pharmaceutical Co., Ltd., and their certificate number was 0017138 and laboratory certificate number was SYXK (Yu and Gao, 2017, Atta et al., 2017) 2010-001.
2.2. Drugs and reagents
Verbenalin, Shanghai Shengzhong Pharmaceutical and Chemical Co., Ltd., with concentration of 98.07%, batch number: 130621; Nimodipine tablets, Yabao Pharmaceutical Group Co., Ltd., batch number: 130150; B cell lymphoma factor 2 (Bcl-2) ELISA kit, R & D Company, batch number: 20131101A; Bcl-2 Related X Protein (BAX) ELISA kit, R & D Company, batch number: 20131101A; Caspase-3 ELISA kit, R & D Company, batch number: 20131101A; Coomassie brilliant blue protein quantitative test kit, Nanjing Jiancheng Bio-engineering Research Institute, batch number: 20131111; Adenosine triphosphate (ATP) enzyme test kit, Nanjing Jiancheng Bio-engineering Research Institute, batch number: 20131122; S-100β Protein ELISA kit, R & D Company, batch number: 20131101A.
2.3. Methods
Ninety six healthy male rats weighing between 25 to 30 grams, after three days of normal feeding, were weighed again and randomly divided into six groups with sixteen in each group. The six groups were the control group (sham), the experiment group, the Nimodipine group, the high, medium and low dose of verbenalin group. Gavage of 0.1 ml/10 g of Nimodipine suspension was administered (positive control drug at a dose of 30 mg/kg, which was equivalent to 15 times of the clinical dose. Final concentration of 3mg/ml with 0.5% CMC), and the control group (sham) and the experiment group were administered gavage of 0.5% CMC of the same volume, once a day for 7 days.
Starting from 8 o’clock on the sixth evening, feeding stopped one group after another, but water was given. At 8 o’clock am on the seventh day, different groups were weighed and medicine was administered. An hour later, intra-peritoneal injection of 10% chloral hydrate (0.03 ml/10 g) as anesthetic agent was administered. After the anesthesia, left common carotid artery (CCA), external carotid artery (ECA), internal carotid artery (ICA) were exposed layer by layer through an incision in the middle to left neck. Common carotid artery and external carotid artery were ligated, and an arterial clip was used to obstruct the internal carotid artery. An incision with a width of about 0.2 mm was cut at 1mm away from the common carotid artery to insert the filament into internal carotid artery through the bifurcation. The filament was advanced 8–10 mm further above the bifurcation until there was resistance, i.e., reaching and occluding the ostium of the left middle cerebral artery to ligate the incision of ICA and the filament. Two hours later, the filament was gently withdrawn to allow reperfusion and the establishment of animal model of cerebral artery occlusion-reperfusion (MCAO). Ten minutes before reperfusion, corresponding drugs were injected intravenously to the high, medium, low dose of verbenalin groups (20 mg/kg, 10 mg/kg, 5 mg/kg. Final concentrations of 4 mg/ml, 2 mg/ml, 1 mg/ml with sodium chloride). In the control group (sham), vessels on the left were exposed without inserting filament.
After 22 h of reperfusion, the neurological deficits of all rats were scored based on Longa standard. 0 point: no symptoms of neurological deficit, normal activity; 1 point: unable to fully stretch the contralateral forepaw; 2 points: circling towards the hemiplegia side when crawling; 4 points: unable to walk spontaneously, loss of consciousness; 5 points: death. Rats scored 0 and 5 were screened out. The remaining rats were put to death by cutting off their cervical spines and brains were quickly removed. The left hemisphere was cut sagittally and the right was discarded. Half of the left hemisphere was then put into the 10% formalin solution and was fixed for a week and embedded in paraffin for HE staining to observe the morphological changes of the brain tissue; the other half was washed with saline water to remove the blood stain and filter was used to absorb the saline water remained on the tissue. The weight of the half right brain was measured to determine the volume of cold saline water to be added. Saline water and brain tissue were mixed and put into a beaker containing ice cubes at a ratio of saline water (ml) to brain tissue (g) = 9:1, and the mixture was made into a 10% brain homogenate with a glass homogenizer, which was centrifuged at 3000r/min at 4 °C for 10 min and then stored at −20 °C or lower, Bax, Bcl-2 to measure the Caspase-3 and ATPase levels in the brain homogenate.
2.4. Statistical approaches
Statistical analysis was performed using statistical software SPSS 17.0. Parametric data were expressed as mean ± standard deviation ( ± s). The single factor analysis of variance was adopted to compare the differences among groups. The variance test was performed with the least significant difference (LSD) method. The variance was tested with the Games-Howell method and grade information with Radit.
3. Results
3.1. The effects on mortality rate and neurological deficit score of rats in the model of focal cerebral ischemia-reperfusion
As is seen from Table 1, the mortality rate of the experiment group was the highest, and the mortality rate of rats in the Nimodipine group, high, medium and low dose of verbenalin groups were significantly lower, indicating that the administration in each group could reduce the mortality rate of rats in the model of focal cerebral ischemia-reperfusion, reduce brain injury and protect brain tissue. Compared with the control group, the neurological deficit score of the experiment group was significantly higher (P < .01), which meant the modeling succeeded; compared with the experiment group, the neurological deficit score of the high dose of verbenalin group was much lower (P < .01), the score of medium dose of verbenalin group decreased remarkably (P < .05), and the score of the Nimodipine group and low dose of verbenalin group demonstrated a tendency of decreasing, all indicating that the administration in each group improved brain function of rats in the model of focal cerebral ischemia-reperfusion at varying degrees.
Table 1.
The effects on mortality rate and neurological deficit score of rats in the model of focal cerebral ischemia-reperfusion ().
| Group | Dose (mg/kg) | Animal number |
Mortality rate (%) | Neurological deficit score | |
|---|---|---|---|---|---|
| Before -modeling | After -modeling | ||||
| Control group | – | 16 | 16 | 0 | 0.0 ± 0.0** |
| Experiment group | – | 16 | 10 | 37.5 | 3.1 ± 0.6 |
| Nimodipine group | 30 | 16 | 11 | 31.25 | 2.2 ± 0.6 |
| High dose of verbenalin group | 20 | 16 | 12 | 25 | 1.9 ± 0.5** |
| Medium dose of verbenalin group | 10 | 16 | 11 | 31.25 | 2.0 ± 0.7* |
| Low dose of verbenalin group | 5 | 16 | 11 | 31.25 | 2.1 ± 0.8 |
Note: Compared with the experiment group.
P < .01.
P < .05.
3.2. The effects on the level of serum S-100β and the percentage of cerebral infarct size of rats in the model of focal cerebral ischemia-reperfusion
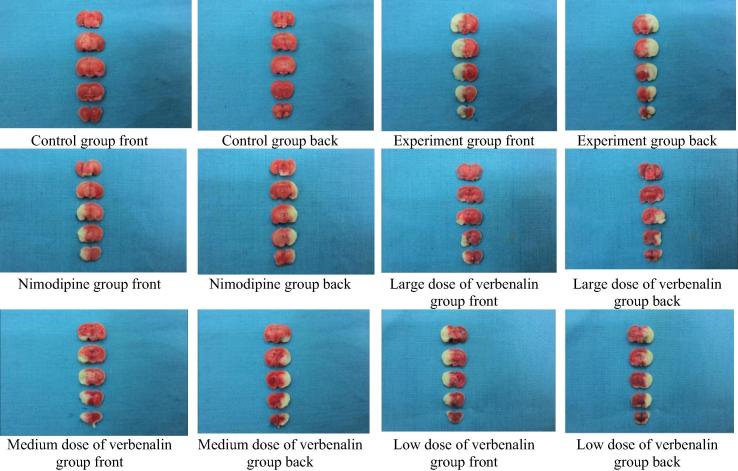
As is shown in Table 2, compared with the control group, the level of serum S-100β and the percentage of cerebral infarct size of rats in the experiment group increased significantly (P < .01), which meant the modeling succeeded. Compared with the experiment group, the level of the serum S-100β of rats in the Nimodipine group and low dose of verbenalin group decreased markedly (P < .01); the percentage of cerebral infarct size of rats in the Nimodipine group, large and medium dose of verbenalin group dropped (P < .01); the percentage of cerebral infarct size of rats in the low dose of verbenalin group demonstrated a tendency of decreasing (P > .05). The findings prove that the administration in each group protected the brain cell and neurological system of rats in the model of focal cerebral ischemia-reperfusion, reduced the level of serum S-100β and the size of cerebral infarct (see Fig. 1).
Table 2.
The effects on the level of serum S-100β and the percentage of cerebral infarct size ().
| Group | N | Dose (mg/kg) | S-100β (ng/ml) | Percentage of cerebral infarct area (%) |
|---|---|---|---|---|
| Control group | 16 | 15.147 ± 3.999** | 0.0 ± 0.0** | |
| Experiment group | 9 | 22.636 ± 3.563 | 32.477 ± 7.044 | |
| Nimodipine group | 10 | 30 | 16.751 ± 3.676** | 17.912 ± 6.216** |
| High dose of verbenalin group | 11 | 20 | 16.732 ± 4.007** | 18.825 ± 9.213** |
| Medium dose of verbenalin group | 11 | 10 | 17.188 ± 2.944** | 22.417 ± 8.917** |
| Low dose of verbenalin group | 10 | 5 | 17.860 ± 2.997** | 27.507 ± 7.884 |
Note: Compared with the experiment group.
*P < .05.
P < .01.
Fig. 1.
The size of cerebral infarct of rats in the model of focal cerebral ischemia-reperfusion.
3.3. The effects on the level of Bax, Bcl-2, Caspase-3 in the brain tissue of rats in the model of focal cerebral ischemia-reperfusion
As is shown in Table 3, compared with the control group, the level of Bax, Caspase-3 of rats in the experiment group increased significantly, which suggested pro-apoptosis factors in the brain tissue increased and the modeling succeeded. Compared with the experiment group, the levels of Bax, Caspase-3 of rats in the Nimodipine group, high, medium and low dose of verbenalin group decreased markedly (P < .01), the level of Bcl-2 in the brain tissue of rats in the Nimodipine group, large and medium dose of verbenalin group increased significantly (P < .01). The findings prove that the administration in each group increased the level of anti-apoptosis genes in the brain tissue of rats in the model of focal cerebral ischemia, reduced the level of pro-apoptosis genes and inhibit the apoptosis, so as to protect the brain tissue and alleviate cerebral ischemia.
Table 3.
The effects on the level of Bax, Bcl-2, Caspase-3 in the brain tissue of rats in the model of focal cerebral ischemia reperfusion ().
| Group | N | Dose (mg/kg) | Bax (ng/ml) | Bcl-2 (ng/ml) | Caspase-3 (pmol/l) |
|---|---|---|---|---|---|
| Control group | 16 | 2.738 ± 0.446** | 11.852 ± 1.398 | 9.675 ± 1.574** | |
| Experiment group | 10 | 4.005 ± 0.507 | 11.937 ± 1.402 | 13.434 ± 0.869 | |
| Nimodipine group | 11 | 30 | 2.838 ± 0.481** | 16.135 ± 1.334** | 9.953 ± 1.566** |
| High dose of verbenalin group | 12 | 20 | 2.805 ± 0.530** | 16.058 ± 1.220** | 9.812 ± 1.400** |
| Medium dose of verbenalin group | 11 | 10 | 2.826 ± 0.440** | 15.140 ± 1.067** | 10.609 ± 1.491** |
| Low dose of verbenalin group | 11 | 5 | 2.995 ± 0.435** | 14.816 ± 1.050** | 10.841 ± 1.572** |
Note: Compared with the experiment group.
*P < .05.
P < .01.
3.4. The effects on the activity of Na + K + -ATPase and the activity of mg ++ - ATPase of rats in the model of focal cerebral ischemia-reperfusion
As is shown in Table 4, compared with the control group, the activity of Na+-K+-ATPase and Mg++-ATPase in the brain tissue of rats in the experiment group decreased significantly(P < .01), which suggested that the modeling succeeded. Compared with the experiment group, the activity of Na+-K+-ATPase and Mg++-ATPase in the brain tissue of rats in the Nimodipine group, large dose of verbenalin group increased markedly (P < .01); the activity of Na+-K+-ATPase and Mg++-ATPase in the brain tissue of rats in the medium dose of verbenalin group increased significantly (P < .05), and the activity of Na+-K+-ATPase and Mg++-ATPase in the brain tissue of rats in the low dose of verbenalin group demonstrated a tendency of increasing (P > .05). The findings prove that the administration in each group increased the ATPase activity in the brain tissue of rats in the model of focal cerebral ischemia-reperfusion, and eased energy metabolism disorders in the brain tissue.
Table 4.
The effects on the activity of Na + K + -ATPase and the activity of Mg ++ -ATPase of rats in the model of focal cerebral ischemia-reperfusion ().
| Group | N | Dose (mg/kg) | Na+-K+-ATPase activity (μmolPi/mgprot/h) | Mg++-ATPase activity (μmolPi/mgprot/h) |
|---|---|---|---|---|
| Control group | 16 | 4.919 ± 1.507** | 5.570 ± 1.699** | |
| Experiment group | 10 | 2.818 ± 0.565 | 2.551 ± 0.558 | |
| Nimodipine group | 11 | 30 | 4.835 ± 1.608** | 5.254 ± 1.859** |
| High dose of verbenalin group | 12 | 20 | 4.885 ± 2.000** | 5.256 ± 1.638** |
| Medium dose of verbenalin group | 11 | 10 | 4.212 ± 1.136* | 4.313 ± 1.853* |
| Low dose of verbenalin group | 11 | 5 | 3.299 ± 0.717 | 3.772 ± 1.487 |
Note: Compared with the experiment group.
P < .01.
P < .05.
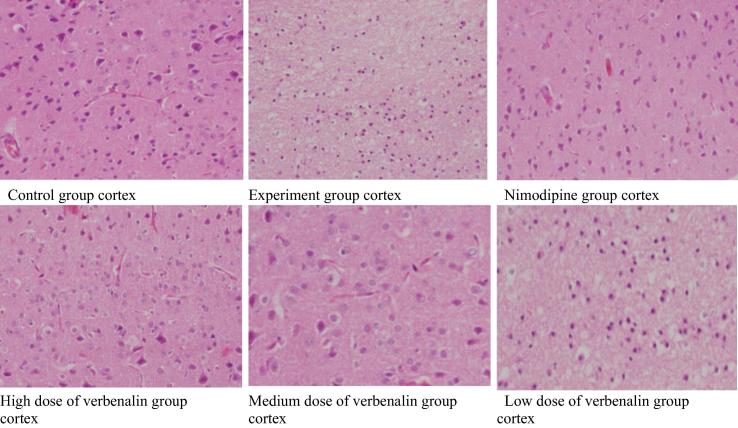
3.5. The effects on the pathological changes of cerebral cortex of rats in the model of focal cerebral ischemia-reperfusion
As is shown in see Fig. 2, for the control group, no cerebral cortex edema was observed, and the neurons were normal; for the experiment group, there was edema of cerebral cortex neurons, large neuronal necrosis and the size of infarct accounted for more than two thirds of the left cortex total; for the Nimodipine group, there was partial edema of cerebral cortex neurons, few neuronal necrosis and the size of infarct accounted for more than one third of the left cortex total; for the large dose of verbenalin group, there was edema of cerebral cortex neurons, few neuronal necrosis and the size of infarct accounted for less than one third of the left cortex total; for the medium dose of verbenalin group, there was edema of cerebral cortex neurons, few neuronal necrosis and the size of infarct accounted for between one third and two thirds of the left cortex total; for the low dose of verbenalin group, there was edema of cerebral cortex neurons, tracts of neuronal necrosis and the size of infarct accounted for between one third and two thirds of the left cortex total.
Fig. 2.
Pictures of pathological changes in the cerebral cortex of rats in the model of focal cerebral ischemia-reperfusion (HE × 400).
“—” stands for no cortex edema and normal neurons; “+” stands for cortex edema, few neuron necrosis and infarct size below one third of the left cortex total; “++” stands for cortex edema, tracts of neuron necrosis and the infarct size between one third and two thirds of the left cortex total; “+++” stands for cortex edema, large number of neuron necrosis and the infarct size more than two thirds of the left cortex total.
By Ridit test, compared with the control group, results of the experiment group showed greater statistical significance (P < .01), which suggested that there were obvious pathological changes in the cortex of rats in the experiment group, and the modeling succeeded; compared with the experiment group, results of the Nimodipine group, large and medium dose of verbenalin group showed more statistical significance (P < .01) and the results of the low dose of verbenalin group showed greater statistical significance (P < .05). The findings suggested that the administration in each group improved the pathological damage of cortex of rats in the model of focal cerebral ischemia-reperfusion at varying degrees, and protected brain tissue (see Table 5).
Table 5.
The effects on the pathological changes of cerebral cortex of rats in the model of focal cerebral ischemia-reperfusion.
| Group | N | Dose (mg/kg) | — | + | ++ | +++ | P |
|---|---|---|---|---|---|---|---|
| Control group | 16 | – | 16 | 0 | 0 | 0 | ** |
| Experiment group | 10 | – | 0 | 0 | 5 | 5 | |
| Nimodipine group | 11 | 30 | 3 | 5 | 2 | 1 | ** |
| High dose of verbenalin group | 12 | 20 | 3 | 6 | 2 | 1 | ** |
| Medium dose of verbenalin group | 11 | 10 | 2 | 6 | 2 | 1 | ** |
| Low dose of verbenalin group | 11 | 5 | 1 | 4 | 4 | 2 | * |
Note: Compared with the experiment group.
P < .01.
P < .05.
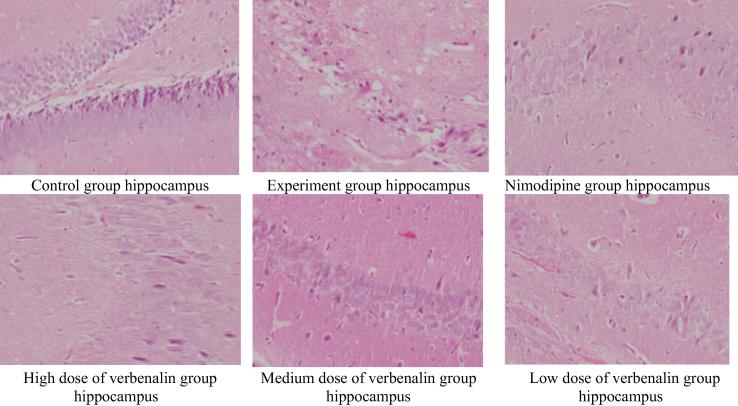
3.6. The effects on the pathological changes of hippocampus of rats in the model of focal cerebral ischemia-reperfusion
Observations are as follows (see Fig. 3): for the control group, there was no hippocampus edema, and the nerve cells were normal; for experiment group, there was hippocampus edema, large number of neuronal necrosis and the size of infarct accounted for more than two thirds of the left hippocampus total; for the Nimodipine group, there was partial edema of hippocampus, few neuronal necrosis and the size of infarct accounted for less than one third of the left hippocampus total; for the high dose of verbenalin group, there was hippocampus edema, few neuronal necrosis and the size of infarct accounted for less than one third of the left hippocampus total; for the medium dose of verbenalin group, there was hippocampus edema, few neuronal necrosis and the size of infarct accounted for between one third and two thirds of the left hippocampus total; for the low dose of verbenalin group, there was hippocampus edema, tracts of neuronal necrosis and the size of infarct accounted for between one third and two thirds of the left hippocampus total.
Fig. 3.
Pictures of pathological changes in the hippocampus of rats in the model of focal cerebral ischemia-reperfusion (HE × 400).
“—” stands for no hippocampus edema and normal neurons; “+” stands for hippocampus edema, few neuron necrosis and infarct size below one third of the left hippocampus total; “++” stands for hippocampus edema, tracts of neuron necrosis and the infarct size between one third and two thirds of the left hippocampus total; “+++” stands for hippocampus edema, large number of neuron necrosis and the infarct size more than two thirds of the left hippocampus total.
By Ridit test, compared with the control group, results of experiment group showed greater statistical significance (P < .01), which suggested that there were obvious pathological changes in the hippocampus of rats in the experiment group, and the modeling succeeded; compared with the experiment group, results of the Nimodipine group, high and medium dose of verbenalin group showed more statistical significance (P < .01) and the results of low dose of Bverbenalin group showed greater statistical significance (P < .05). The findings suggested that the administration in each group improved the pathological damage of hippocampus of rats in the model of focal cerebral ischemia-reperfusion at varying degrees, and protected brain tissue (see Table 6).
Table 6.
The effects on the pathological changes of hippocampus of rats in the model of focal cerebral ischemia-reperfusion.
| Group | N | Dose (mg/kg) | — | + | ++ | +++ | P |
|---|---|---|---|---|---|---|---|
| Control group | 16 | – | 16 | 0 | 0 | 0 | ** |
| Experiment group | 10 | – | 0 | 0 | 4 | 6 | |
| Nimodipine group | 11 | 30 | 3 | 6 | 1 | 1 | ** |
| High dose of verbenalin group | 12 | 20 | 4 | 5 | 3 | 0 | ** |
| Medium dose of verbenalin group | 11 | 10 | 3 | 5 | 2 | 1 | ** |
| Low dose of verbenalin group | 11 | 5 | 1 | 4 | 4 | 2 | * |
Note: Compared with the experiment group.
P < .01.
P < .05.
4. Discussion
Cerebral ischemia is a common disease among the elderly, and the main risk factors are obesity, hypertension, hyperlipidemia, diabetes, heart disease, hyperuricemia, high platelet aggregation. The disease led to high mortality and morbidity, posing serious threat to human health. Cerebral ischemia-reperfusion injury refers to injury of the brain cells caused by cerebral ischemia. When blood is restored after reperfusion, the ischemic injury aggravated. The most obvious changes are brain edema and neuronal injury. Ischemic cerebrovascular diseases, especially reperfusion injuries after cerebral ischemia, pose great harm to human health.
Mechanisms of cerebral ischemia-reperfusion injury are complex. In response to these mechanisms, traditional Chinese medicine and its effective ingredients have achieved some research progress on the prevention and treatment of cerebral ischemia-reperfusion injury (Zhang et al., 2016, Yang et al., 2016). At present, the research on drugs to prevent and treat cerebral ischemia focuses on studying the active sites or extracts of traditional Chinese medicine, and the research on compound prescription is mere research on single traditional Chinese medicine (Xue et al., 2016, Duan et al., 2017). The study on single active ingredients of traditional Chinese medicine is lacked, leading to the situation that the mechanism of preventing and treating cerebral ischemia-reperfusion injury with traditional Chinese medicine remains unknown and the research is not aligned with actual needs (Muhammad et al., 2017). Targeted research on the single active ingredients of traditional Chinese medicine to Huoxue Huayu and Qingre Jiedu would enable us to identify its mechanism of preventing and treating cerebral ischemia-reperfusion injury and understand how the medicine intervenes at the molecule level. This offers a new approach in studying the prevention and treatment of cerebral ischemia with traditional Chinese medicine and presents broad prospect for research. Studies have found that Verbena decoction can inhibit the expression of β-amyloid protein in rats in the Alzheimer's disease (AD) model, thus effectively avoiding the neurotoxicity injury and enabling the learning ability and memory of rats in the AD model to improve significantly (Tan and Wang, 2011, Duzer et al., 2017).
Changes in animal neurological function are macroscopic indicators of cerebral ischemia-reperfusion model, and the neurological deficit score of animals in the model can reflect the abnormalities of the nervous system. In this study, the model of cerebral ischemia-reperfusion injury was established by inserting filaments into rats, creating a two hour ischemia, and a 22 h reperfusion was carried out before the neurological deficit was scored. All groups in the model demonstrated varying degrees of neurological deficits, with manifestations such as being unable to fully stretch the right front paw; circling towards or falling to the right while walking, loss of consciousness or even the ability to walk. Cerebral ischemia-reperfusion leads to serious damage to or even death of animals, as proved by varying degrees of mortality rate in the group in the model.
S-100β protein is mainly distributed in the glial cells of the central nervous system, unique to nerve cells. Cerebral ischemia is sometimes due to damages to neurons and glial cells. When a large number of cytoplasmic proteins are released from the damaged cells and enter into intercellular fluid, soluble S-100β proteins enter cerebrospinal fluid through the intercellular fluid, and then break the damaged brain blood barrier to enter blood circulation. Therefore, the determination of serum S-100β protein level can reflect to which extent the nerve cells in the central nervous system are injured and killed, and play an important role in the cerebral ischemia-reperfusion experiment (Sarfraz et al., 2017).
Results of the experiment show that the level of S-100β protein in experiment group was significantly higher than that of the control group (P < .01). The fact that verbenalin could decrease the level of S-100β protein shows that verbenalin could protect the brain neurons of animals in the model of cerebral ischemia-reperfusion, reduce the degree of brain damage. The effect was proved best in the high dose of verbenalin group.
Pro-apoptosis gene Bax and anti-apoptosis gene Bcl-2 are considered to be the most important genes that promote and inhibit apoptosis. When Bax level increases, cell apoptosis is promoted; and when Bc1-2 level increases, cell apoptosis is inhibited. Caspase-3 is the key enzyme in the implementation of apoptosis (Zhang et al., 2013, Coballase-Urrutia et al., 2017), and under normal circumstances, Caspase-3 is in dormant state. But in the case of cerebral ischemia or cerebral ischemia-reperfusion (Sun et al., 2008, Gao et al., 2017), inflammatory factors released by brain tissue can activate Caspase-3, leading to apoptosis. Pro-apoptotic genes such as Bax in Bcl-2 family can also activate Caspase-3, leading to apoptosis (Kenneth, 2012). Downgrading the expression of Bax, Caspase-3 and upgrading the expression of Bcl-2 can both inhibit neuronal apoptosis induced by cerebral ischemia (Luna-Vargas et al., 2016, Kenneth, 2012, Yaidikar and Thakur, 2015).
Results of the experiment show that the level of Bax as well as Caspase-3 in experiment group was significantly higher than that of the control group (P < .01). The fact that verbenalin could decrease the level of Bax and Caspase-3, and increase the level of Bcl-2 shows that verbenalin could reduce the level of pro-apoptosis genes, increase the level of anti-apoptosis genes, thereby inhibiting apoptosis and protecting brain tissue. The effect was proved best in the high dose of verbelanin group.
Cerebral function is closely related to brain energy metabolism, and energy metabolism disorder is the basis of cerebral ischemic injury. Mitochondria as a place for intracellular energy synthesis, is extremely sensitive to ischemia (Yu and Gao, 2017). When there is cerebral ischemia, cell energy metabolism decreases, respiratory chain, mitochondrial enzyme activity change, and mitochondrial DNA expression will be damaged. What’s more, in the case of cerebral ischemia-reperfusion, a large number of free radicals are produced, causing stress response of mitochondria, which affects mitochondrial function. As the intracellular ATP level decreases, Na+, K+ -ATPase that rely on ATP to provide free energy are inactivated, Na+ level increases and Na+ Ca2+ exchange enhances, which then leads to intracellular Ca2+ overload. As a result, a large number of Ca2+ influent activate membrane protease and phospholipase, destroy cell membrane, and result in free fatty acids and phospholipids, which then promote the release of arachidonic acid, resulting in more oxygen free radicals. The process forms a vicious circle, leading to brain tissue swelling and necrosis. Regulation of ATP and ATPase activity in rat’s hippocampus can reduce cerebral ischemia-reperfusion injury.
5. Conclusions
Results of the experiment show that the activity of Na+-K+-ATPase and Mg2+-ATPase in the experiment group were significantly higher than those in the control group (P < .01). The fact that verbenalin could increase the activity of Na+-K+-ATPase and Mg2+-ATPase shows that verbenalin could improve the energy metabolism disorder of brain tissue caused by cerebral ischemia and hypoxia. The effect was proved best in the high dose of verbenalin group.
By observing the effects of verbenalin on the mortality, neurological deficit score, percentage of cerebral infarct size, pathological changes of brain tissue, serum S-100β protein level, Bax and Bcl-2, Caspase-3 and ATPase levels in brain tissue of rats in the model of focal cerebral ischemia-reperfusion, it was found that verbanalin could decrease the mortality rate, neurological deficit score, percentage of cerebral infarct area, improve brain tissue injury, increase Bcl-2 level and decrease Bax, Caspase-3, serum S-100β protein levels. It is suggested that verbenalin can improve brain microcirculation and energy metabolism, inhibit the expression of apoptosis genes, promote the expression of anti-apoptosis genes, protect the brain tissue and neurons, and reduce the cerebral ischemia-reperfusion injury. The effect was proved best in the high dose of verbenalin group.
Acknowledgements
National Key Scientific and Technological Innovation Project (2009ZX09103-324), Henan Province Excellent Science and Technology Innovation Team (TCJ2014-391), Henan International Cooperation Project (144300510015).
Footnotes
Peer review under responsibility of King Saud University.
References
- Atta A., Mustafac G., Sheikh M.A., Shahid M., Xiao H. The biochemical significances of the proximate, mineral and phytochemical composition of selected vegetables from Pakistan. Matrix Sci. Pharma. 2017;1(1):06–09. [Google Scholar]
- Coballase-Urrutia E., Cardenas-Rodriguez N. Biochemical and molecular modulation of CCl4-induced peripheral and central damage by Tilia americana var. mexicana extracts. Saudi Pharm. J. 2017;25(3):319–331. doi: 10.1016/j.jsps.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan S., Wang T., Zhang J., Li M., Lu C., Wang L., Zou Y., Fu F. Huatuo Zaizao pill promotes functional recovery and neurogenesis after cerebral ischemia-reperfusion in rats. BMC Compl. Altern. Med. 2017;17:19. doi: 10.1186/s12906-016-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duzer S., Aydemir Y. Significance of paranasal sinus aplasia. Acta Med. Mediterranea. 2017;33(4):637–640. [Google Scholar]
- Gao W. Characteristics studies of molecular structures in drugs. Saudi Pharm. J. 2017;25(4):580–586. doi: 10.1016/j.jsps.2017.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gohar S., Abbas G., Sajid S., Sarfraz M., Ali S., Ashraf M., Aslam R., Yaseen K. Prevalence and antimicrobial resistance of Listeria monocytogenes isolated from raw milk and dairy products. Matrix Sci. Medica. 2017;1(1):10–14. [Google Scholar]
- Ishaq S., Jafri L. Biomedical importance of cocoa (Theobroma cacao): significance and potential for the maintenance of human health. Matrix Sci. Pharma. 2017;1(1):01–05. [Google Scholar]
- Kenneth, M., 2012. Editors Perspective (Throwing Caution to the Wnts). Curr. Neurovascular Res., vol. 9, pp. i–ii. [DOI] [PubMed]
- Luna-Vargas, Mark P.A., Chipuk, Jerry E. The deadly landscape of pro-apoptotic BCL-2 proteins in the outer mitochondrial membrane. FEBS J. 2016;283:2676–2689. doi: 10.1111/febs.13624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad G., Rashid I., Firyal S., Saqib M. Successful treatment of idiopathic generalized subcutaneous emphysema in kajli a ram by large bore injection needle. Matrix Sci. Medica. 2017;1(1):01–02. [Google Scholar]
- Sarfraz M., Ashraf Y., Ashraf S. A Review: Prevalence and antimicrobial susceptibility profile of listeria species in milk products. Matrix Sci. Medica. 2017;1(1):03–09. [Google Scholar]
- Sun M., Zhao Y.M., Xu Ch. Cross-talk between calpain and caspase-3 in penumbra and core during focal cerebral ischemia-reperfusion. Cell. Mol. Neurobiol. 2008;28:71–85. doi: 10.1007/s10571-007-9250-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan W.B., Wang Z.F. Effect of Verbena Water Decoction on Learning and Memory of Alzheimer's mice. Chin. J. Ethnomed. Ethnopharm. 2011;20:36–37. [Google Scholar]
- Xue J., Zhang X.J., Cong Z., Kang N., Liu X.X., Yu J.J., Zhang N., Wang H., Zhang L., Chen R., Cui L.L., Wang L.N., Wang X.L. Protective effect of Naoxintong against cerebral ischemia reperfusion injury in mice. J Ethnopharmacol. 2016;182:181–189. doi: 10.1016/j.jep.2016.02.022. [DOI] [PubMed] [Google Scholar]
- Yaidikar L., Thakur S. Punicalagin attenuated cerebral ischemia-reper.sion insult via inhibition of proinflammatory cytokines, up-regulation of Bcl-2, down-regulation of Bax, and caspase-3. Mol. Cell. Biochem. 2015;402:141–148. doi: 10.1007/s11010-014-2321-y. [DOI] [PubMed] [Google Scholar]
- Yang S., Ning F.B., Li J., Guo D.M., Zhang L., Cui R.T., Liu Y.L. Therapeutic effect analysis of sinomenine on rat cerebral ischemia-reperfusion injury. J. Stroke Cerebrovasc. Dis. 2016;25:1263–1269. doi: 10.1016/j.jstrokecerebrovasdis.2016.02.023. [DOI] [PubMed] [Google Scholar]
- Yu D.J., Gao H.Y. Effect of propofol on mitochondrial ATP content and ATPase activity in hippocampus of rats with cerebral ischemia-reperfusion injury. Saudi J. Biol. Sci. 2017;24:246–250. doi: 10.1016/j.sjbs.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen W.A., Huang S.S., Wang H.M. Protective effects of mangiferin on cerebral ischemia–reperfusion injury and its mechanisms. Eur. J. Pharmacol. 2016;771:145–151. doi: 10.1016/j.ejphar.2015.12.003. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Liu W., Zhu D., Jin Y.H. Activation of caspase-activated deoxyribonuclease and neuroprotective effect of caspase-3 inhibitor after focal cerebral ischemia-reperfusion injury. Afr. J. Pharm. Pharmacol. 2013;7:157–164. [Google Scholar]