Abstract
The study aimed to estimate prevalence and influencing factors of overweight, general obesity, and abdominal obesity in rural areas of China. A total of 39034 participants aged 18 to 79 years were enrolled from the Henan Rural Cohort Study for the cross-sectional study. The age-standardized prevalence of overweight, general obesity, and abdominal obesity were 34.97%, 16.82%, and 43.71% in the general Chinese rural adults, respectively. Gender differences were: 36.04%, 18.98%, 35.37% for men, and 34.55%, 15.42%, 49.13% for women, respectively. The subgroup analysis showed the rates of overweight, general obesity, and abdominal obesity existed considerable disparities, but were universally high in all subgroups. Further, the study found that there were statistically significant U-shaped associations between the prevalence of overweight, general obesity, and abdominal obesity and age groups. In addition, the prevalence of participants with both abnormal BMI and WC were even at approximate forty percent. Aging, married/cohabiting, higher per capita monthly income, and unhealthy lifestyle were independent influencing factors of overweight, general obesity and abdominal obesity. In conclusion, overweight and obesity were severe in rural China. There is an increased need for closely monitoring high risk factors and promoting healthy lifestyle to curb the obesity epidemic among rural population.
Introduction
As a disorder of energy metabolism, obesity affects multiple organ systems and is associated with a variety of vascular and several nonvascular complications, such as cardiovascular diseases (CVDs, mainly heart disease and stroke), diabetes, hypertension, dyslipidemia, musculoskeletal disorders, and some cancers1–5. Although the great efforts have been made to clear grim obesity in China, the prevalence of obesity still continues to increase, especially in rural areas with limited resources6–9. Moreover, the incidence rates are increasing faster in rural areas than those in cities6,7. The summary prevalence of general obesity and overweight in rural China were reported to be 3.6% and 8.2% in 1993. Whereas, the latest published nationwide prevalence estimates from 2010 have climbed to 11.0% and 29.1% for general obesity and overweight, respectively8,9. In addition, according to the 2011 China Health and Nutrition Survey (CHNS) data, the prevalence of abdominal obesity was 44.0% in rural China10. Therefore, ongoing reliable estimations are needed to plan effective national prevention and control programs for obesity management and reducing the disease complications in areas with limited resources.
Different anthropometric measures such as body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) have been proposed to define obesity. However, BMI is related to body fat percentage and could well reflect the degree of obesity deducting the influence of different heights while WC is the most practical and simplest index to measure the magnitude of the accumulation of fat in the abdomen. Thus, BMI and WC are the commonly-used anthropometric measurements for obesity in China11–14.
The aims of the current study were to provide the recent estimates of the prevalence of overweight, general obesity, and abdominal obesity, and to investigate potential influencing factors based on a large epidemiological survey conducted in Chinese rural adults, which will help policy making for obesity management in Chinese rural population.
Results
Demographic characteristics
Table 1 summaries the demographic characteristics of the 39034 participants aged 18–79 years old. The mean (standard deviation, SD) age was 55.61 (12.16) years. Overall, a total of 15446 and 6932 subjects were diagnosed with overweight and general obesity, respectively. The mean BMI were 25.85 kg/m2 for participants with overweight and 30.30 kg/m2 for obesity (P < 0.001). Current cigarette smoking, adequate vegetable and fruit intake, and lower level of height were more common among leaner study participants, while younger age, being women, married/cohabiting, lower education level, higher per capita monthly income, current alcohol drinking, high fat diet, lack of physical activity, higher level of weight, WC, and BMI were more prevalent among overweight and general obese participants.
Table 1.
Demographic characteristics of the participants.
| Variable | Overall (N = 39034) | BMI (N = 39034) | χ2/F | P | WC (N = 39034) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| General obesity (n = 6932) | Overweight (n = 15446) | Normal weight (n = 15705) | Underweight (n = 951) | Abdominal obesity (n = 20167) | Normal (n = 18867) | χ2/t | P | ||||
| Age (years), mean ± SD | 55.61 ± 12.16 | 54.74 ± 11.42 | 55.62 ± 11.32 | 55.85 ± 12.94 | 57.73 ± 16.16 | 23.657 | <0.001 | 56.05 ± 11.19 | 55.14 ± 13.10 | 7.403 | <0.001 |
| Sex, n (%) | 117.717 | <0.001 | 2796.344 | <0.001 | |||||||
| Women, n (%) | 23615 (60.50) | 4477 (64.58) | 9541 (61.77) | 9064 (57.71) | 533 (56.05) | 14753 (73.15) | 8862 (46.97) | ||||
| Men, n(%) | 15419 (39.50) | 2455 (35.42) | 5905 (38.23) | 6641 (42.29) | 418 (43.95) | 5414 (26.85) | 10005 (53.03) | ||||
| Marital status, n (%) | 60.609 | <0.001 | 0.302 | 0.583 | |||||||
| Married/cohabiting | 25048 (91.69) | 6355 (92.84) | 14074 (92.32) | 13861 (90.80) | 758 (87.03) | 18311 (91.61) | 16737 (91.77) | ||||
| Widowed/single/divorced/separation | 3177 (8.31) | 490 (7.16) | 1170 (7.68) | 1404 (9.20) | 113 (12.97) | 1676 (8.39) | 1501 (8.23) | ||||
| Education, n (%) | 20.361 | <0.001 | 144.241 | <0.001 | |||||||
| ≤Primary school | 17469 (44.75) | 3184 (45.93) | 6784 (43.92) | 7022 (44.71) | 479 (50.37) | 9615 (47.68) | 7854 (41.63) | ||||
| ≥Junior school | 21565 (55.25) | 3748 (54.09) | 8662 (56.08) | 8683 (55.29) | 472 (49.63) | 10552 (52.32) | 11013 (58.37) | ||||
| Per capita monthly income, n (%) | 86.542 | <0.001 | 29.107 | <0.001 | |||||||
| ≤500 RMB | 13920 (35.66) | 2281 (32.91) | 5322 (34.46) | 5905 (37.60) | 412 (43.32) | 6949 (34.46) | 6971 (36.95) | ||||
| 500 RMB ~ | 12837 (32.89) | 2384 (34.39) | 5229 (33.85) | 4939 (31.45) | 285 (29.97) | 6822 (33.83) | 6015 (31.88) | ||||
| ≥1000 RMB | 12277 (31.45) | 2267 (32.72) | 4895 (31.69) | 4846 (30.95) | 254 (26.71) | 6396 (31.72) | 5881 (31.17) | ||||
| Smoking, n (%) | 216.362 | <0.001 | 1647.513 | <0.001 | |||||||
| Never | 28401 (72.76) | 5315 (76.67) | 11479 (74.32) | 10945 (69.69) | 662 (69.61) | 16435 (81.49) | 11966 (63.42) | ||||
| Ever | 3175 (8.13) | 567 (8.18) | 1283 (8.31) | 1244 (7.92) | 81 (8.52) | 1266 (6.28) | 1909 (10.12) | ||||
| Current | 7458 (19.11) | 1050 (15.15) | 2684 (17.38) | 3516 (22.39) | 208 (21.87) | 2466 (12.23) | 4992 (26.46) | ||||
| Drinking, n (%) | 58.449 | <0.001 | 546.729 | <0.001 | |||||||
| Never | 30159 (77.26) | 5334 (76.95) | 11869 (76.84) | 12170 (77.49) | 786 (82.65) | 16521 (81.92) | 13638 (72.28) | ||||
| Ever | 1820 (4.66) | 259 (3.74) | 702 (4.54) | 808 (5.14) | 51 (5.36) | 641 (3.18) | 1179 (6.25) | ||||
| Current | 7055 (18.07) | 1339 (19.32) | 2875 (18.61) | 2727 (17.36) | 114 (11.99) | 3005 (14.90) | 4050 (21.47) | ||||
| Adequate vegetable and fruit intake, n (%) | 16307 (41.78) | 2710 (39.09) | 6444 (41.72) | 6773 (43.13) | 380 (39.96) | 33.630 | <0.001 | 8081 (40.07) | 8226 (43.60) | 49.929 | <0.001 |
| High fat diet, n (%) | 7449 (19.08) | 1384 (19.97) | 3009 (19.48) | 2927 (18.64) | 129 (13.56) | 25.852 | <0.001 | 3786 (18.77) | 3663 (19.41) | 2.599 | 0.107 |
| Physical activity, n (%) | 84.917 | <0.001 | 159.083 | <0.001 | |||||||
| Low | 12584 (32.24) | 2504 (36.12) | 4928 (31.90) | 4814 (30.65) | 338 (35.54) | 6825 (33.84) | 5759 (30.52) | ||||
| Moderate | 14743 (37.77) | 2519 (36.34) | 5870 (38.00) | 5977 (38.06) | 377 (39.64) | 7860 (38.97) | 6883 (36.48) | ||||
| High | 11707 (29.99) | 1909 (27.54) | 4648 (30.09) | 4914 (31.29) | 236 (24.82) | 5482 (27.18) | 6225 (32.99) | ||||
| Height (cm), mean ± SD | 159.72 ± 8.20 | 159.46 ± 8.43 | 159.67 ± 8.18 | 159.88 ± 8.10 | 159.71 ± 8.59 | 4.560 | 0.003 | 159.04 ± 8.19 | 160.45 ± 8.15 | −17.123 | <0.001 |
| Weight (kg), mean ± SD | 63.50 ± 11.14 | 77.22 ± 9.65 | 66.07 ± 7.42 | 56.04 ± 6.71 | 44.84 ± 5.52 | 15227.926 | <0.001 | 68.80 ± 10.60 | 57.83 ± 8.63 | 111.768 | <0.001 |
| BMI(kg/m2), mean ± SD | 24.83 ± 3.57 | 30.30 ± 2.16 | 25.85 ± 1.12 | 21.87 ± 1.45 | 17.53 ± 1.00 | 62611.671 | <0.001 | 27.12 ± 2.93 | 22.39 ± 2.37 | 174.127 | <0.001 |
| WC (cm), mean ± SD | 84.08 ± 10.40 | 97.10 ± 7.52 | 87.07 ± 6.13 | 76.52 ± 6.58 | 65.47 ± 5.33 | 19677.480 | <0.001 | 91.27 ± 7.56 | 76.40 ± 6.96 | 201.722 | <0.001 |
BMI, body mass index; WC, waist circumference.
Among the 39034 participants, 20167 were diagnosed with abdominal obesity. The mean WC were 91.27 cm for participants with abdominal obesity and 76.40 cm for participants without abdominal obesity (P < 0.001). Compared with the subjects without abdominal obesity, the subjects with abdominal obesity had the following characteristics: older age, being women, higher percentage of lower education level, higher per capita monthly income, never cigarette smoking, never alcohol drinking, inadequate vegetable and fruit intake, high fat diet, physical inactivity, lower level of height, higher level of weight and BMI (P < 0.05 for each).
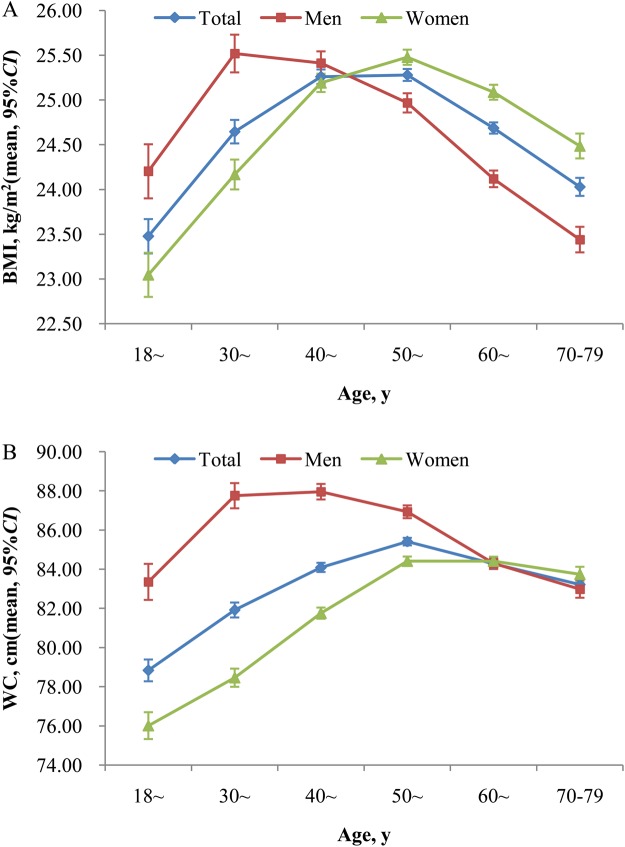
The sex-specific distributions of BMI and WC according to age
Figure 1 displays the sex-specific distributions of BMI and WC according to age. The age- and sex-adjusted mean levels (95% confidence intervals, CI) of BMI and WC were 24.79 (24.75–24.82) kg/m2 and 84.34 (84.23–84.44) cm, respectively. The age-adjusted mean levels (95%CI) of BMI and WC were 24.56 (24.51–24.62) kg/m2 vs. 25.01 (24.97–25.06) kg/m2 and 85.55 (85.39–85.71) cm vs. 83.12 (82.99–83.25) cm for men and women (P < 0.001), respectively. There were statistically significant U-shaped associations between the mean levels of BMI, WC and age groups (All P < 0.05), with the highest mean values among study participants with age of 30 to 39 in men and 50 to 59 in women. In general, women had higher sex specific mean levels of BMI and WC than men at age above 50 years and 60 years, respectively.
Figure 1.
Mean (95%CI) of BMI and WC according to age in both sexes. Error bars indicate 95% confidence intervals. The mean was adjusted for age and sex in total population. All P values for U-shaped (quadratic term) association with age for BMI and WC in both sexes from the Curve Estimation <0.05. CI, confidence intervals; BMI, body mass index; WC, waist circumference.
Prevalence of overweight and obesity
Table 2 describes the prevalence of overweight and obesity among various characteristics. The prevalence of overweight, general obesity, and abdominal obesity were 39.57%, 17.76%, and 51.67%, and the corresponding age-standardized rates were 34.97%, 16.82%, and 43.71%, respectively. Subgroups study showed that the prevalence of overweight, general obesity, and abdominal obesity were higher in those who were older, being female, married/cohabiting, with higher per capita monthly income, never cigarette smoking, current alcohol drinking, inadequate vegetable and fruit intake, high fat diet, and lack of physical activity, and were universally high in all subgroups (>26.00%, 13.00%, and 30.00%).
Table 2.
Prevalence of overweight and obesity among various characteristics (N = 39034).
| Variable | BMI (N = 39034) | WC (N = 39034) | |||||
|---|---|---|---|---|---|---|---|
| General obesity (n = 6932) | Overweight (n = 15446) | χ 2 | P | Abdominal obesity (n = 20167) | χ 2 | P | |
| Age, n (%) | 903.493 | <0.001 | 557.220 | <0.001 | |||
| 18~ | 182 (14.03) | 340 (26.21) | 400 (30.84) | ||||
| 30~ | 500 (18.08) | 956 (34.56) | 1157 (41.83) | ||||
| 40~ | 1448 (19.89) | 3098 (42.55) | 3797 (52.16) | ||||
| 50~ | 2154 (20.05) | 4649 (43.28) | 6247 (58.15) | ||||
| 60~ | 2024 (16.56) | 4780 (39.11) | 6348 (51.94) | ||||
| 70~79 | 624 (13.20) | 1623 (34.33) | 2218 (46.92) | ||||
| Sex, n (%) | 117.717 | <0.001 | 2796.344 | <0.001 | |||
| Women, n (%) | 4477 (18.96) | 9541 (40.40) | 14753 (62.47) | ||||
| Men, n(%) | 2455 (15.92) | 5905 (38.30) | 5414 (35.11) | ||||
| Marital status, n (%) | 60.609 | <0.001 | 0.302 | 0.583 | |||
| Married/cohabiting | 6355 (18.13) | 14074 (40.16) | 18311 (52.25) | ||||
| Widowed/single/divorced/separation | 490 (15.42) | 1170 (36.82) | 1676 (52.75) | ||||
| Education, n (%) | 20.361 | <0.001 | 144.241 | <0.001 | |||
| ≤Primary school | 3184 (18.23) | 6784 (38.83) | 9615 (55.04) | ||||
| ≥Junior school | 3748 (17.38) | 8662 (40.17) | 10552 (48.93) | ||||
| Per capita monthly income, n (%) | 86.542 | <0.001 | 29.107 | <0.001 | |||
| ≤500 RMB | 2281 (16.39) | 5322 (38.23) | 6949 (49.92) | ||||
| 500 RMB ~ | 2384 (18.57) | 5229 (40.73) | 6822 (53.14) | ||||
| ≥1000 RMB | 2267 (18.47) | 4895 (39.87) | 6396 (52.10) | ||||
| Smoking, n (%) | 216.362 | <0.001 | 1647.513 | <0.001 | |||
| Never | 5315 (18.71) | 11479 (40.42) | 16435 (57.87) | ||||
| Ever | 567 (17.86) | 1283 (40.41) | 1266 (39.87) | ||||
| Current | 1050 (14.08) | 2684 (35.99) | 2466 (33.07) | ||||
| Drinking, n (%) | 58.449 | <0.001 | 546.729 | <0.001 | |||
| Never | 5334 (17.69) | 11869 (39.35) | 16521 (54.78) | ||||
| Ever | 259 (14.23) | 702 (38.57) | 641 (35.22) | ||||
| Current | 1339 (18.98) | 2875 (40.75) | 3005 (42.59) | ||||
| Adequate vegetable and fruit intake, n (%) | 2710 (16.62) | 6444 (39.52) | 33.630 | <0.001 | 8081 (49.56) | 49.929 | <0.001 |
| High fat diet, n (%) | 1384 (18.58) | 3009 (40.39) | 25.852 | <0.001 | 3786 (50.83) | 2.599 | 0.107 |
| Physical activity, n (%) | 84.917 | <0.001 | 159.083 | <0.001 | |||
| Low | 2504 (19.90) | 4928 (39.16) | 6825 (54.24) | ||||
| Moderate | 2519 (17.09) | 5870 (39.82) | 7860 (53.31) | ||||
| High | 1909 (16.31) | 4648 (39.70) | 5482 (46.83) | ||||
Changes of overweight and obesity in different subgroups
Figure 2 presents that the age-standardized prevalence of overweight and obesity displayed U-shaped association with aging in both sexes (All P < 0.05). The age-standardized prevalence of overweight, general obesity, and abdominal obesity in men and women were 36.04% vs. 34.55%, 18.98% vs. 15.42%, and 35.36% vs. 49.12%, respectively. The prevalence of overweight, general obesity, and abdominal obesity increased with age until 40 years in men and 60 years in women and then decreased. Women had a higher prevalence of overweight than men at age above 40 years, but lower prevalence when they were in midlife and youth (Fig. 2A). Figure 2B implies that men had more probability of having general obesity than women except the highest two age groups. As to abdominal obesity, women had higher prevalence than men in the entire age ranges except the age group of 30 to 39 (Fig. 2C).
Figure 2.
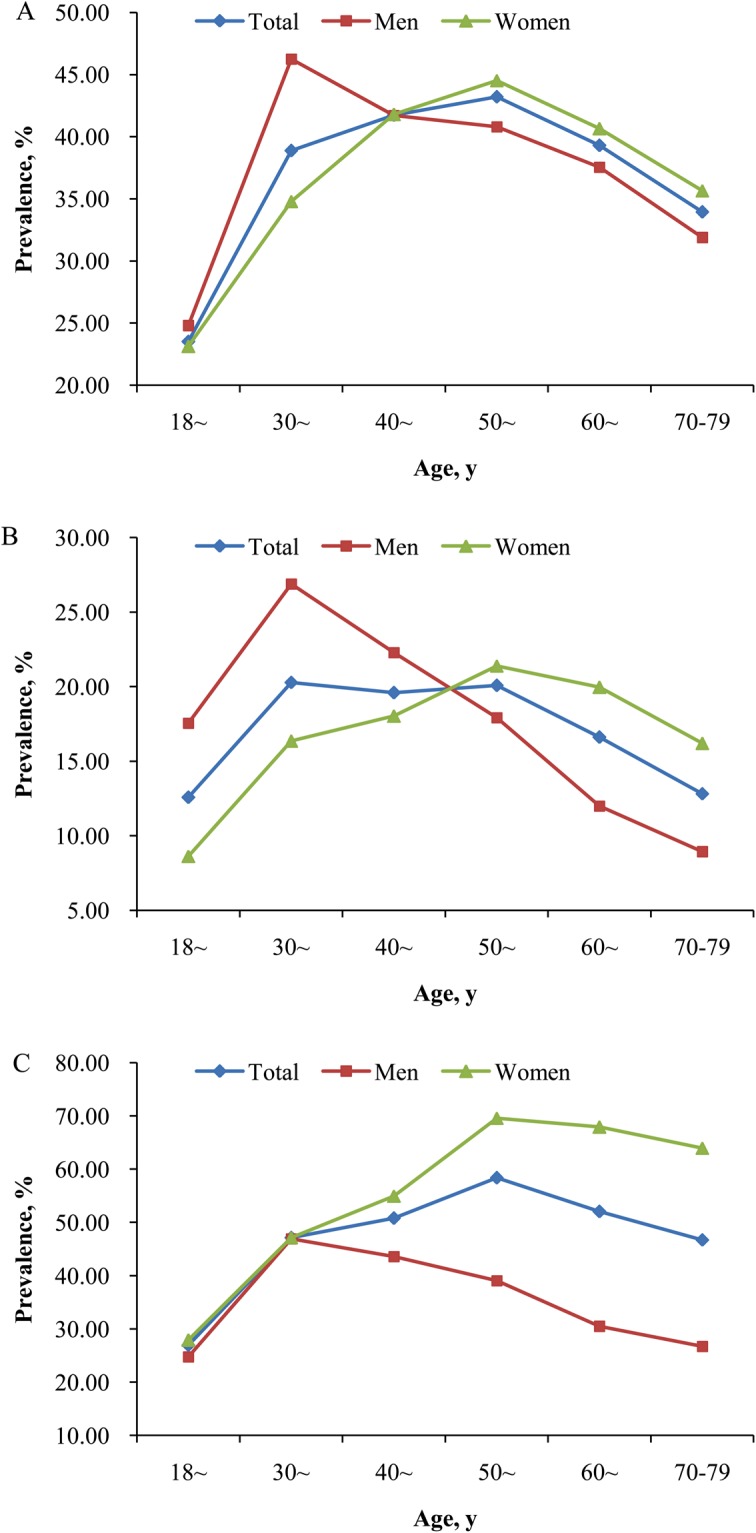
Changes in the age-standardized prevalence of overweight and obesity with aging in different sexes. (A) is for overweight, (B) is for general obesity, (C) is for abdominal obesity. All P values for U-shaped (quadratic term) association with age for overweight and obesity in both sexes from the Curve Estimation <0.05.
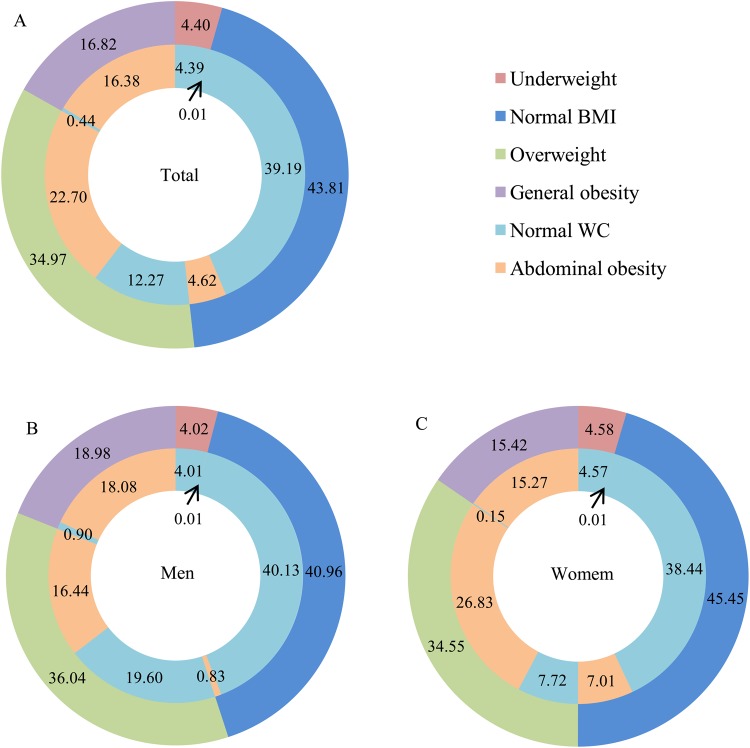
The percentage according to the cut-off points of BMI and WC in different sexes
Figure 3 shows the age-standardized percentage according to the cut-off points of BMI and WC in different sexes. A total of 24902 subjects (8567 men and 16335 women) had excess BMI or WC, and the corresponding age-standardized prevalence was 56.41% (55.85% in men and 56.98% in women). In detail, 4619, 123, 2524, 10827, and 6809 were diagnosed with single overweight, single general obesity, single abdominal obesity, abdominal obesity &overweight, and abdominal obesity & general obesity, and the corresponding age-standardized prevalence were 12.27%, 0.44%, 4.62%, 22.70%, and 16.38%, respectively. The age-standardized prevalence of participants with both excess BMI and abdominal obesity was 39.08% (34.52% for men and 42.10% for women). The prevalence of general obesity and abdominal obesity differed depending on the cut-offs of BMI or WC in both sexes. Among the participants with a normal BMI, 10.55% (2.02% for men and 15.42% for women) still had abdominal obesity. Likewise, among participants with general obesity, 2.62% (4.74% for men and 0.97% for women) had a normal WC.
Figure 3.
The age-standardized percentage according to the cut-off points of BMI and WC in different sexes. BMI, body mass index; WC, waist circumference.
Analysis of influencing factors
Table 3 describes the odds ratios (ORs) of potential influencing factors associated with overweight, general obesity and abdominal obesity. Old age, married/cohabiting, higher per capita monthly income, never cigarette smoking, current alcohol drinking, inadequate vegetable and fruit intake, high fat diet, and lack of physical activity were significantly positively associated with the prevalence of overweight, general obesity and abdominal obesity. Men were negatively associated with the prevalence of general obesity and abdominal obesity. Higher education level was only related to general obesity.
Table 3.
Associations of potential risk factors for overweight and obesity.
| Variable | Overweight | General obesity | Abdominal obesity |
|---|---|---|---|
| OR(95%CI) | OR(95%CI) | OR(95%CI) | |
| Age | |||
| 18~ | 1.00 | 1.00 | 1.00 |
| 30~ | 1.39 (1.17–1.65) | 1.45 (1.17–1.79) | 1.52 (1.30–1.77) |
| 40~ | 2.13 (1.82–2.49) | 1.93 (1.58–2.35) | 2.42 (2.09–2.80) |
| 50~ | 2.29 (1.97–2.67) | 2.09 (1.72–2.54) | 3.27 (2.83–3.77) |
| 60~ | 1.79 (1.53–2.10) | 1.41 (1.15–1.72) | 2.73 (2.36–3.15) |
| 70~79 | 1.40 (1.18–1.65) | 0.96 (0.78–1.19) | 2.26 (1.94–2.64) |
| P trend | 0.748 | <0.001 | <0.001 |
| Gender | |||
| Women | 1.00 | 1.00 | 1.00 |
| Men | 0.94 (0.87–1.02) | 0.87 (0.79–0.96) | 0.30 (0.28–0.32) |
| Marital status | |||
| Married/cohabiting | 1.00 | 1.00 | 1.00 |
| Widowed/single/divorced/separation | 0.89 (0.82–0.97) | 0.86 (0.77–0.96) | 0.90 (0.83–0.97) |
| Education | |||
| ≤Primary school | 1.00 | 1.00 | 1.00 |
| ≥Junior school | 0.98 (0.93–1.03) | 0.82 (0.77–0.88) | 0.96 (0.91–1.01) |
| Per capita monthly income | |||
| ≤500 RMB | 1.00 | 1.00 | 1.00 |
| 500 RMB~ | 1.13 (1.07–1.19) | 1.17 (1.09–1.25) | 1.12 (1.07–1.18) |
| ≥1000 RMB | 1.08 (1.02–1.14) | 1.14 (1.05–1.22) | 1.13 (1.07–1.19) |
| P trend | 0.008 | 0.001 | <0.001 |
| Smoking | |||
| Never | 1.00 | 1.00 | 1.00 |
| Ever | 0.94 (0.84–1.04) | 0.95 (0.83–1.09) | 1.03 (0.94–1.14) |
| Current | 0.67 (0.61–0.72) | 0.56 (0.50–0.63) | 0.77 (0.71–0.84) |
| Drinking | |||
| Never | 1.00 | 1.00 | 1.00 |
| Ever | 1.09 (0.97–1.23) | 1.03 (0.87–1.21) | 1.08 (0.96–1.21) |
| Current | 1.33 (1.24–1.43) | 1.56 (1.42–1.72) | 1.53 (1.43–1.64) |
| Adequate vegetable and fruit intake | 0.93 (0.88–0.97) | 0.84 (0.79–0.89) | 0.87 (0.84–0.91) |
| High fat diet | 1.06 (1.00–1.13) | 1.12 (1.04–1.20) | 1.19 (1.13–1.26) |
| Physical activity | |||
| low | 1.00 | 1.00 | 1.00 |
| Moderate | 0.89 (0.84–0.94) | 0.73 (0.68–0.78) | 0.79 (0.75–0.83) |
| High | 0.86 (0.81–0.91) | 0.68 (0.64–0.74) | 0.71 (0.67–0.75) |
| P trend | <0.001 | <0.001 | <0.001 |
OR: odds ratios, CI: confidence intervals.
Discussion
The present large survey specialized in Chinese rural population provided important new evidence on the current burden of overweight and obesity in China. Overall, the mean levels of BMI, WC, and prevalence of overweight, general obesity, and abdominal obesity were much higher in Chinese rural adults than the previous national studies in China6–8. Men had more likely to be placed in the categories of general obesity, while women were more probability of being abdominal obesity. There were statistically significant U-shaped associations between the mean levels of BMI and WC and age groups, with the highest mean values among study participants with age of 30 to 39 in men and 50 to 59 in women. Similar significant trends were observed in the prevalence of overweight, general obesity, and abdominal obesity in both men and women. Subgroup analysis found that the proportions of overweight, general obesity, and abdominal obesity varied significantly across subpopulations, and were universally high in all subgroups (>26.00%, 13.00%, and 30.00%). Further study indicated that approximately forty percent of the rural adults in China had both excess BMI and WC. The multiple logistic regression analysis showed that old age, married/cohabiting, higher per capita monthly income, never cigarette smoking, current alcohol drinking, inadequate vegetable and fruit intake, high fat diet, and lack of physical activity were associated influencing factors for overweight, general obesity and abdominal obesity.
Evidences from previous epidemiological studies showed that BMI and WC levels had increased dramatically in Chinese populations6,7,13,15. Similar results were found in our study. The mean levels (95%CI) of BMI and WC were 24.79 (24.75–24.82) kg/m2 and 84.34 (84.23–84.44) cm, respectively. Despite of adjusting for sex and age, the mean levels of BMI and WC documented a 7.32% (or 1.69 kg/m2) and 5.95% (or 4.74 cm) increase compared with the national data in the study of Reynolds et al.6 conducted in 2000–2001, respectively. Due to changes in BMI and WC levels, the prevalence of overweight, general obesity, and abdominal obesity have been increasing in the past decades, and overweight and obesity have become the most important public health problems due to their common associations with many chronic diseases in China2,4,5,8,15. Although China brought obesity and overweight into the non-communicable disease (NCD) targets, the rates of overweight, general obesity, and abdominal obesity still increased rapidly in the Chinese population, especially in rural population7,8,15. The overall age-standardized prevalence of overweight and general obesity in current study were obviously higher than those in rural areas of the China in 2010 although there was no difference in prevalence of abdominal obesity between the current study and the CHNS in 20119,10. However, the subgroup analysis showed that the rates of overweight, general obesity, and abdominal obesity were universally high in all subgroups. Thus, effective measures should be taken to improve the status of the prevention and control of obesity and overweight, especially in rural areas with limited health care resources.
Data from Working Group on Obesity in China (WGOC) shows that the subjects with excess BMI or WC, especially with the aggregation of excess BMI and WC, were more susceptible to diabetes, hypertension, dyslipidemia, and the accumulation of risk factors compared to people with normal BMI and WC11. In the current study, exceeded fifty five percentages of the rural adults had excess BMI or WC in China, and the prevalence of participants with both abnormal BMI and WC were even approximately forty percent. Therefore, effective preventive measures are needed to maintain both BMI and WC levels close to normal and decrease the incidence of overweight and obesity as well as related complications. In addition, the prevalence of excess BMI and abdominal obesity differed depending on the cut-off points of BMI or WC in both sexes. There was a considerable number of participants with a normal BMI had abdominal obesity. Likewise, among participants with overweight and general obesity, there was still a considerable number who had normal WC. Therefore, it seems that it’s unreasonable to use only one indicator as the cardiovascular risk factor. The combination use of BMI and WC might be the best marker for indirectly reflecting cardiometabolic risk11,12.
Previous studies have declared that the prevalence of overweight and general obesity were higher in men than women while abdominal obesity was more prevalent in women than men8,15. Similar results were found in our study. The age-standardized prevalence of overweight, general obesity, and abdominal obesity in men and women were 36.04% vs. 34.55%, 18.98% vs. 15.42%, and 35.36% vs. 49.12%, respectively. Further study showed that there were different change trends in the prevalence of overweight, general obesity, and abdominal obesity in men and women. Women had obviously higher prevalence of overweight and general obesity than men at age above 50 years, but lower prevalence when they were in midlife and young. As to abdominal obesity, women had higher prevalence than men in the entire age ranges except the age group of 30 to 39. The phenomenon might attribute to the different cut-off values of WC in men and women. But the prevalence of overweight, general obesity, and abdominal obesity were obviously higher in women than men above 50 years of age. Age and the rapid hormone changes during the menopausal transition might explain for the BMI and WC distribution changes in women6,13,16. Moreover, Men aged 30 to 39 years had the highest prevalence, whereas women aged 50 to 69 years had the highest prevalence. These data all implied that the overweight and obesity management guidelines in our country should post middle-aged men and postmenopausal women as the priority management groups. Previous epidemiological studies have found that unhealthy lifestyle, such as alcohol drinking, inadequate vegetable and fruit intake, high fat diet, and lack of physical activity, was associated with the prevalence of overweight and obesity3,11. Our results were in accordance with the findings. With rapid economic growth, Chinese food consumption patterns have changed from predominantly rice, wheat and related products to high animal food consumption, frequency of alcohol consumption increased, and physical activities were reduced due to advances in technology and transportation3,8,11,17,18. Those dietary pattern and lifestyle changes might account for the major proportion of the increase in overweight, general obesity and abdominal obesity among Chinese adults3,8,11,18. Therefore, we should use mass media and government programs to encourage retention of its high-dietary fiber, low-fat, low-energy density traditional cuisine, moderate alcohol drinking, and sufficient physical activity life3,11. Furthermore, the emphasis of healthy education should be different for different high-risk populations. For men, a good lifestyle (e.g. no cigarette smoking or alcohol drinking), healthy diet (e.g. adequate vegetable and fruit intake and low fat diet), as well as exercise are also crucial in controlling obesity. For pregnant and breastfeeding women, promotion of breast feeding and healthy complementary feeding according to WHO recommendations is the most importance. For perimenopausal women, the key points of primary health care should be put on diet diversity and physical activity, such as increase consumption of fruit and vegetables, as well as legumes, whole grains and nuts; engage in regular physical activity; and keep good mood. As for wealthier populations, low-energy diets are effective in the short term, but reducing inactivity, increasing walking, and developing an activity programme might increase the effectiveness of obesity therapy. As for people with unhealthy lifestyle, lifestyle changes were effective in controlling body weight and WC3,11. The relationship between smoking status and body shape remains controversial. The current finding that the current cigarette smokers were generally leaner than never smokers was in agreement with most previous studies19. In contrast, there was no or positive association between smoking and body weight in some studies20,21. The reasons for the inconsistent association between smoking and higher BMI remained unclear. Unhealthy lifestyle (such as increased frequency of alcohol consumption, physical inactivity, and so on) or the different social classes might be partially responsible for the inconsistency16.
The current study synthesized the epidemiologic characteristics and influencing factors of overweight and obesity based on a relatively large sample size of rural population in China. The standardized survey tools, training and field implementation, and adjusting for a wide range of potential confounders guarantee the reliability of the analysis. However, several limitations should also be addressed. Firstly, these findings were derived from a cross-sectional study not a prospective cohort design, no causal relationships could be precisely delineated. Secondly, some residents such as college students and migrant workers were not included in the current study for studying or working outside. These groups were more likely to be young and healthy, with lower prevalence of overweight and obesity, which might lead to the overestimation of overweight and obesity in the rural population. Finally, the results were based on one geographical region in the middle area of China, which might not be a representative sample of the Chinese rural population. However, the rural population of Henan province accounts for 9% of rural Chinese population. Therefore, the results from the relatively large rural epidemiological study, to some extent, could reflect the prevalence of overweight and obesity in Chinese rural areas.
In conclusion, overweight and obesity have become one of the severe public problem in rural China. Therefore, closely monitoring high risk factors and promoting healthy lifestyle are essential to curb the obesity epidemic in the population including older, middle-aged men, postmenopausal women, people with unhealthy lifestyle in Chinese rural areas.
Methods
Study subjects
The Henan Rural Cohort Study was conducted in Yuzhou county, Suiping county, Xinxiang county, Kaifeng county, and Yima county of Henan province in China from July 2015 to September 2017, which has been registered in Chinese Clinical Trial Register (Registration number: ChiCTR-OOC-15006699) before the onset of patient enrollment22. The target population was permanent residents aged 18–79 years who lived in the five rural areas. A multistage, stratified cluster sampling method was used to select the sample. In the first stage, 5 counties were selected from different geographical regions (central, south, north, east, and west) in Henan Province in consideration of the adherence of the masses and local medical conditions. In the second stage, 1~3 typical rural communities (referred to as a “township”) in each county were selected by the local Centre for Disease Control and Prevention. In the final stage, all permanent residents who satisfied the inclusion criteria and signed informed consent in each sampled rural district were selected as the study sample. Overall, a total of 39259 participants aged 18–79 years old in rural areas completed the survey, with a response rate of 93.7%. To estimate the prevalence of overweight, general obesity, and abdominal obesity overall and by age, sex, and other demographic characteristics, and to explore potential influencing factors in rural areas, 144 who lacked weight, height, and WC data, 30 who were on a diet or took diet teas or diet pills, and 51 who were pregnant were excluded. Finally, 39034 subjects were included for the present study. Written informed consent was obtained from each participant before data collection. The Henan Rural Cohort Study was approved by the Zhengzhou University Life Science Ethics Committee (Code: [2015] MEC (S128)), and was conducted according to the 1975 Declaration of Helsinki.
Assessment of covariates
The detailed information on demographic characteristics, smoking, alcohol drinking, dietary habits, physical activities, personal history of disease, and family history were collected through face-to-face interview by the trained research staff using a standardized questionnaire. Education level was classified into two categories: participants attained up to primary school level were considered as ‘≤Primary school’, while those attained junior school or higher levels of education were defined as ‘ ≥Junior school’. Smoking status was classified into current smoker (a person who smoked more than one cigarette per day in the past 6 months), ever smoker (a person who ever smoked) and never smoker. Alcohol drinking status was categorized into current drinking (a person who consumed twelve or more alcoholic drinks in the past one year, whether spirits, beer, wine or other forms of alcohol beverage), ever drinking (a person who ever drank), and never drinking. According to Chinese dietary guidelines15, adequate vegetable and fruit intake was considered as a person who consumed an average of more than 500 g vegetable and fruit per day. High fat diet was defined as a person who took an average of more than 75 g meat of livestock and poultry per day in accordance with the dietary guidelines for Chinese residents23. According to the international physical activity questionnaire (IPAQ 2001), physical activity was categorized into low, moderate, and high24.
Assessment of outcomes
Body weight with light clothing was measured to the nearest 0.1 kg using a weight measurement device (V. BODY HBF-371, OMRON, Japan). Height was measured to the nearest 0.1 cm without shoes using a standard right-angle device and a fixed measurement tape. WC was measured at a point midway between the lowest rib and the iliac crest in a horizontal plane to the nearest 0.1 cm using non-elastic tape. All measurements were conducted twice by trained research staff according to a standard protocol from WGOC11, and the mean values were used for the statistical analysis. BMI was estimated as body weight (kg) divided by height square (m2). According to the criteria recommended by WGOC, underweight was defined as BMI < 18.5 kg/m2, normal weight was defined as 18.5 ≤ BMI < 24 kg/m2, overweight was defined as 24.0 kg/m2 ≤ BMI < 28.0 kg/m2, and general obesity was defined as BMI ≥ 28.0 kg/m211. Abdominal obesity was defined according to guidelines of the International Diabetes Federation for Chinese populations as a WC ≥ 90 cm for men and ≥80 cm for women. Normal WC was defined as a WC <90 cm for men and <80 cm for women25.
Statistical analysis
Continuous variables presented as mean ± SD were compared using the t-test or analysis of variance, while categorical variables presented as numbers and proportions were compared using chi-square test. The age- or sex-adjusted means (95%CI) of BMI and WC overall and in different sexes were estimated and compared by multiple linear regression. The stratified subgroup analyses for prevalence of overweight, general obesity, and abdominal obesity were performed according to the demographic characteristics. The presence of a U-shaped association between age group and overweight and obesity was tested using quadratic term of age group as a continuous variable in the curve estimation. The prevalence of overweight, general obesity, and abdominal obesity were standardized using the direct method according to the Chinese Population Census 201026. The multivariable logistic regression models were used to calculate OR and 95%CI between the potential influencing factors and the prevalence of overweight, general obesity, and abdominal obesity. All selected characteristics were included in multivariable logistic regression models. Besides, to explore whether there had a linear trend of ORs between age groups, per capita monthly income, physical activity and obesity, the three indices were taken as continuous variables. All tests were two-tailed and a P value < 0.05 was the threshold for statistical significance. All statistical analyses were performed using SAS9.1 software package (SAS Institute, USA).
What is already known on this subject?
Previous studies have concentrated on prevalence of obesity in China, but the studies focusing on epidemiology and risk factors in areas with limited resources are still limited. More importantly, little is known about the recent epidemiology in overweight, general obesity, and abdominal obesity in rural areas of China.
What does this study add?
Prevalence and risk factors associated obesity assessed by two metrics were explored in the current study. The mean levels of body mass index (BMI) and waist circumference (WC) were high, and the prevalence of overweight, general obesity, and abdominal obesity were severe overall and in various subgroups in Chinese rural adults. Further, the study found that there were statistically significant U-shaped associations between the prevalence of overweight, general obesity, and abdominal obesity and age groups (All P < 0.05), with the highest prevalence among study participants with age of 30 to 39 in men and 50 to 59 in women, respectively. In addition, the prevalence of participants with both abnormal BMI and WC were approximately forty percent. Aging, married/cohabiting, higher per capita monthly income, and unhealthy lifestyles were independent influencing factors of overweight, general obesity and abdominal obesity. In conclusion, overweight and obesity were severe in rural China. Closely monitoring high risk factors and promoting healthy lifestyle are essential to curb the obesity epidemic among rural population.
The current study provides a contextual epidemiological analysis of overweight, general obesity, and abdominal obesity prevalence information for rural China, with a multiple regression analysis, to determine the strength of associations between obesity, overweight, and demographic and risk factors for the rural adults.
Acknowledgements
This research was supported by the National Key Research and Development Program Precision Medicine Initiative of China (Grant NO: 2016YFC0900803), National Natural Science Foundation of China (Grant NO: 81573243, 81602925), Henan Natural Science Foundation of China (Grant NO: 182300410293), Science and Technology Foundation for Innovation Talent of Henan Province (Grant NO: 164100510021), Science and Technology Innovation Talents Support Plan of Henan Province Colleges and Universities (Grant NO: 14HASTIT035), High-level Personnel Special Support Project of Zhengzhou University (Grant NO: ZDGD13001). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank the participants, the coordinators, and administrators for their supports during the study. To Dr. Fang Wang, the authors would like to express her gratitude for her critical reading of the manuscript.
Author Contributions
C.J.W. conceived and designed the experiments. X.T.L., W.D.W., Z.X.M., W.Q.H., R.Q.T., X.L.Q., X.Z., Z.Y.T., H.Q.Z., J.J.J., and Y.Q.L. performed and conducted the experiments. X.T.L., R.Q.T., X.L.Q., X.Z., Z.Y.T., H.Q.Z., J.J.J., and Y.Q.L. analyzed the data and take responsibility for the integrity and accuracy of the information. X.T.L., W.D.W., Z.X.M., and W.Q.H. contributed to the reagents/materials/analysis tools. X.T.L. drafted and revised the manuscript. All authors have approved the final manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet, 387, 1377–1396 (2016). [DOI] [PMC free article] [PubMed]
- 2.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Available at: http://www.who.int/mediacentre/factsheets/fs311/en/. (Accessed January 8, 2018)
- 4.Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects). Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 383, 970-983 (2014). [DOI] [PMC free article] [PubMed]
- 5.Sun J, Zhou W, Gu T, Zhu D, Bi Y. A retrospective study on association between obesity and cardiovascular risk diseases with aging in Chinese adults. Sci Rep. 2018;8:5806. doi: 10.1038/s41598-018-24161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds K, et al. Prevalence and risk factors of overweight and obesity in China. Obesity (Silver Spring). 2007;15:10–18. doi: 10.1038/oby.2007.527. [DOI] [PubMed] [Google Scholar]
- 7.Chen WW, et al. The report of cardiovascular diseases in China–2016 profiles. Chinese Circulation Journal. 2017;32:521–530. [Google Scholar]
- 8.Xi B, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes Rev. 2012;13:287–296. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li XY, et al. Prevalence and characteristic of overweight and obesity among adults in China, 2010. Chin J Prev Med. 2012;46:683–686. [PubMed] [Google Scholar]
- 10.Du P, et al. Prevalence of abdominal obesity among Chinese adults in 2011. J Epidemiol. 2017;27:282–286. doi: 10.1016/j.je.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Working Group on Obesity in China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Acta nutrimenta sinica. 26, 1–4 (2004). [PubMed]
- 12.Wildman RP, et al. Are waist circumference and body mass index independently associated with cardiovascular disease risk in Chinese adults? Am J Clin Nutr. 2005;82:1195–1202. doi: 10.1093/ajcn/82.6.1195. [DOI] [PubMed] [Google Scholar]
- 13.Jin MJ, et al. Prevalence of overweight and obesity and their associations with socioeconomic status in a rural Han Chinese adult population. PLoS One. 2013;8:e79946. doi: 10.1371/journal.pone.0079946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu L, et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS One. 2017;12:e0183934. doi: 10.1371/journal.pone.0183934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mi YJ, et al. Prevalence and Secular Trends in Obesity Among Chinese Adults, 1991–2011. Am J Prev Med. 2015;49:661–669. doi: 10.1016/j.amepre.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sternfeld B, et al. Menopause, physical activity, and body composition/fat distribution in midlife women. Med Sci Sports Exerc. 2005;37:1195–1202. doi: 10.1249/01.mss.0000170083.41186.b1. [DOI] [PubMed] [Google Scholar]
- 17.Zhai F, et al. Prospective study on nutrition transition in China. Nutr Rev. 2009;67(Suppl 1):S56–61. doi: 10.1111/j.1753-4887.2009.00160.x. [DOI] [PubMed] [Google Scholar]
- 18.Du SF, Wang HJ, Zhang B, Zhai FY, Popkin BM. China in the period of transition from scarcity and extensive undernutrition to emerging nutrition-related non-communicable diseases, 1949–1992. Obes Rev. 2014;15(Suppl 1):8–15. doi: 10.1111/obr.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Akbartabartoori M, Lean ME, Hankey CR. Relationships between cigarette smoking, body size and body shape. Int J Obes (Lond). 2005;29:236–243. doi: 10.1038/sj.ijo.0802827. [DOI] [PubMed] [Google Scholar]
- 20.Caks T, Kos M. Body shape, body size and cigarette smoking relationships. Int J Public Health. 2009;54:35–39. doi: 10.1007/s00038-008-7061-x. [DOI] [PubMed] [Google Scholar]
- 21.Clair C, et al. Dose-dependent positive association between cigarette smoking, abdominal obesity and body fat: cross-sectional data from a population-based survey. BMC Public Health. 2011;11:23. doi: 10.1186/1471-2458-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu X, et al. Dyslipidemia prevalence, awareness, treatment, control, and risk factors in Chinese rural population: the Henan rural cohort study. Lipids Health Dis. 2018;17:119. doi: 10.1186/s12944-018-0768-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chinese Nutrition Society. The dietary guidelines for Chinese residents. The Tibet people’s Publishing House: Lhasa, 2011, pp 97, 197, 198.
- 24.International Physical Activity Questionnaire: Short Last 7 Days Self-Administered Format 2005. Available at: http://www.ipaq.ki.se/downloads.htm. (Accessed 26 October 2015)
- 25.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. Available at: https://www.idf.org/our-activities/advocacy-awareness/resources-and-tools/60:idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html. (Accessed December 1, 2017)
- 26.National Bureau of Statistics of the People’s Republic of China. China statistical yearbook, 2010. Beijing, China: China statistic press; 2010.