Abstract
Allogeneic natural killer (NK) cell therapy is a potential therapeutic approach for a variety of solid tumors. We established an expansion method for large-scale production of highly purified and functionally active NK cells, as well as a freezing medium for the expanded NK cells. In the present study, we assessed the effect of cryopreservation on the expanded NK cells in regards to viability, phenotype, and anti-tumor activity. NK cells were enormously expanded (about 15,000-fold expansion) with high viability and purity by stimulating CD3+ T cell-depleted peripheral blood mononuclear cells (PBMCs) with irradiated autologous PBMCs in the presence of IL-2 and OKT3 for 3 weeks. Cell viability was slightly reduced after freezing and thawing, but cytotoxicity and cytokine secretion were not significantly different. In a xenograft mouse model of hepatocellular carcinoma cells, cryopreserved NK cells had slightly lower anti-tumor efficacy than freshly expanded NK cells, but this was overcome by a 2-fold increased dose of cryopreserved NK cells. In vivo antibody-dependent cell cytotoxicity (ADCC) activity of cryopreserved NK cells was also demonstrated in a SCID mouse model injected with Raji cells with rituximab co-administration. Therefore, we demonstrated that expanded/frozen NK cells maintain viability, phenotype, and anti-tumor activity immediately after thawing, indicating that expanded/frozen NK cells can provide ‘ready-to-use’ cell therapy for cancer patients.
Keywords: Natural killer cells, NK cell expansion, Allogeneic NK therapy, Cryopreservation, Cancer
INTRODUCTION
Natural killer (NK) cells play a role in the defense against viral infections and cancer without antigen-specific receptors (1). These cells do not express the T cell marker CD3, but express CD56 and CD16, which is involved in antibody-dependent cell cytotoxicity (ADCC) (2,3). NK cells exert effector functions by killing target cells in a perforin- and granzyme-dependent manner and by producing cytokines, such as interferon (IFN)-γ and tumor necrosis factor (TNF)-α (4,5).
An anti-leukemic effect of NK cells has been demonstrated in the setting of allogeneic hematopoietic stem cell transplantation in patients with hematological malignancies (6). In addition, adoptive transfer of ex vivo-expanded haploidentical NK cells after lymphodepleting chemotherapy has been shown to result in NK cell expansion in vivo without inducing graft-versus-host disease (GVHD) (7). Furthermore, NK cell-based immunotherapies have been attempted for the treatment of solid tumors. Clinical trials using ex vivo-expanded allogeneic NK cells have been performed in patients with advanced non-small cell lung cancer (phase I) and recurrent ovarian or breast cancers (phase II) (8,9,10). Our group has also performed a phase I clinical trial with ex vivo-expanded allogeneic NK cells derived from random donors in patients with malignant lymphoma or advanced sold tumors (11). These studies have demonstrated the safety of allogeneic NK cell therapy.
For clinical use of NK cells, large-scale production of highly purified NK cells is critical. Most NK cell expansion strategies achieve this goal by using feeder cells, such as irradiated peripheral blood mononuclear cells (PBMCs), Epstein-Barr virus-transformed lymphoblastoid cell lines, or gene-modified, irradiated K562 cells (12,13,14,15). After large-scale production of NK cells, cryopreservation of expanded NK cells until use is a practical option because the expanded NK cells have a short expiry period. However, there are concerns regarding the activity of cryopreserved NK cells.
Cryopreservation of expanded NK cells has been shown to reduce the expression of NKG2D and TRAIL and cytotoxicity, which could be reversed by IL-2 (16). In addition, expanded and frozen NK cells have been shown to be functional, even after 12 months of cryopreservation, but immediately after thawing NK cells fail to lyse K562 cells unless allowed to rest overnight (15). More recently, GMP-compliant expanded NK cells were shown to be fully functional with or without cryopreservation (17). In vivo administration of expanded/cryopreserved NK cells into NOD/IL-2Rgc/Rag (NSG) mice has been shown to result in the survival of fewer NK cells than when using non-cryopreserved NK cells (18). When expanded NK cells were infused into relapsed multiple myeloma patients, peripheral blood NK cell counts remained lower in the patients who received cryopreserved NK cells than in the patients who received freshly expanded NK cells (19). Taken together, previous reports suggest that cryopreservation of ex vivo-expanded NK cells reduces survival and anti-tumor activity, although exposure to cytokines could restore them.
Establishing an optimal cryopreservation method for large-scale expanded NK cells will improve the efficiency of allogeneic NK cell immunotherapy in terms of the cost and convenience for patients. In the present study, we assessed the effect of cryopreservation on large-scale expanded NK cells and compared the characteristics and anti-tumor activity of NK cells with or without cryopreservation. In particular, we evaluated anti-tumor activity immediately after thawing without additional cytokine stimulation.
MATERIALS AND METHODS
Ethics statement
Healthy donors were enrolled in the study after providing written informed consent in accordance with the Declaration of Helsinki. This research protocol was reviewed and approved by the Institutional Review Board of Seoul National University Hospital (permit number: H-1004-027-315).
NK cell enrichment, expansion, and cryopreservation
PBMCs were collected from healthy donors via leukapheresis. CD3+ T cells were removed by VarioMACS (Miltenyi Biotec, Bergisch Gladbach, Germany). Ten million CD3-depleted cells were seeded in 30 ml of CellGro SCGM medium (CellGenix, Freiburg, Germany) with 1% autologous plasma, irradiated (2,000 rad) autologous PBMCs (5×107 cells), 500 IU/ml IL-2 (Proleukin; Novartis, Basel, Switzerland), and 10 ng/ml anti-CD3 monoclonal antibody OKT3 (eBioscience, Thermo Fisher Scientific, Waltham, MA, USA) in an A-350N culture bag (NIPRO, Osaka, Japan). Cultured NK cells were restimulated on day 7 of the culture by adding 5×107 feeder cells per 1×107 NK cells in 60 ml of CellGro SCGM containing 1% plasma, and then transferred into an A-1000NL culture bag (NIPRO). The A-1000NL culture bag enables co-culture of 4–8×107 cultured NK cells and 2–4×108 feeder cells. OKT (10 ng/ml) and IL-2 (500 IU/ml) were added. Fresh medium with IL-2 (500 IU/ml) was added to the NK cell culture every 2 days to maintain a concentration of 0.5–2×106 cells/ml for 21 days. Harvested cells were suspended in freezing media (RPMI1640 [50%; Gibco®, Thermo Fisher Scientific, Waltham, MA, USA]) containing albumin (20%; GC pharma, Yongin, Korea), dextran (40-Dex) (25%; DAI HAN PHARM, Seoul, Korea), and DMSO (5%; Mylan Teoranta Limited, Galway, IL, USA) to make 1×108 cells/mL for cell cryopreservation. Frozen NK cells were preserved for 3–6 months in liquid nitrogen. Cells were thawed in 37°C water bath and slowly diluted with RPMI1640 containing 10% fetal bovine serum (FBS). NK cell count and viability were assessed by propidium iodide staining using an automatic fluorescence cell counter (AlphaMetrix Biotech, Rodermark, Germany).
Human cell lines
K562, Huh7, Hep3B, HepG2, and Raji cells were purchased from American Type Culture Collection (ATCC; Manassas, VA, USA). SNU354 cells was purchased from the Korean Cell Line Bank (KCLB; Seoul, Korea). Cell lines were cultured in RPMI1640 medium or DMEM medium supplemented with 10% FBS and 2 mM L-glutamine (All from Gibco®, Thermo Fisher Scientific).
Immunostaining and flow cytometric analysis
The following monoclonal antibodies were used to stain NK cells: anti-NKRP-1-PE (HP-3G10), anti-CCR5-PE (NP-6G4), ant-CXCR4-PE (12G5) (eBioscience, Thermo Fisher Scientific), anti-CD3-FITC (UCHT1), anti-CD16-PE (3G8), anti-DNAM-1-PE (DX11), anti-CD56-PE-Cy5 (B159), anti-CXCR3-PE (1C6/CXCR3), anti-NKp30-PE (P30-15), anti-NKp44-PE (P44-8.1), anti-NKp46-PE (9E2/NKp46), anti-CD158b-FITC (CH-L) (BD Biosciences, Franklin Lakes, NJ, USA), anti-NKG2A-PE (131411), anti-NKG2C-PE (134591), anti-NKG2D-PE (149810) (R&D systems, Minneapolis, MN, USA), anti-CD158a-APC (EB6B), and anti-CD158e-PE (Z27.3.7) (Beckman Coulter, Brea, CA, USA). Stained NK cells were acquired on an LSR Fortessa (BD Biosciences) and data analysis performed using FlowJo software (FLOWJO, LLC, Ashland, OR, USA).
Fluorometric cytotoxicity assay
The cytotoxicity of NK cells against target cells was assessed by a fluorometric cytotoxicity assay (20). Target cells are stained with 30 mM calcein-AM (Molecular Probes, Thermo Fisher Scientific) for 1 h at 37°C. NK cells and labeled target cells were co-cultured in U-bottom 96-well plates (Nunc cell culture, Thermo Fisher Scientific) in triplicate at effector:target (E:T) ratios of 0.1:1 to 30:1 per 1×104 target cells at 37°C and 5% CO2 for 4 h. To assess the ADCC of NK cells, 0.5 ng/mL of rituximab (Roche, Basel, Switzerland) was added. RPMI1640 medium containing 10% FBS or 0.1% triton-X100 (Sigma-Aldrich, St. Louis, MO, USA) was added to the target cells as spontaneous and maximum release controls, respectively. Measurements were made at an excitation wavelength of 485 nm and emission wavelength of 535 nm using a fluorometer (VICTOR 3; PerkinElmer, Waltham, MA, USA). The percentage of specific calcein-AM release was calculated as follows:
| % specific release = [(mean experimental release−mean spontaneous release)/(mean maximal release−mean spontaneous release)]×100 |
Intracellular cytokine and CD107a staining
NK cells were co-cultured with tumor cells at a 1:1 ratio for 4 h in the presence of anti-CD107a-APC (H4A3; BD Biosciences), BD GolgiStop™ (BD Biosciences), and BD GolgiPlug™ (BD Biosciences). After 4 h, the cells were washed with FACS buffer and stained with anti-CD3-FITC, anti-CD56-APC-eFluor®780 (CMSSB; Thermo Fisher Scientific, eBioscience), and 7-AAD (Beckman Coulter). The cells were then permeabilized by BD CytoFix/CytoPerm™ (BD Biosciences) and stained with anti-IFN-γ-PE (B27; BD Biosciences) and anti-TNF-α-PE-Cy7 (Mab11; Thermo Fisher Scientific, eBioscience). Stained cells were acquired on an LSR Fortessa and the data analyzed using FlowJo software.
In vivo animal model of hepatocellular carcinoma
In order to assess the anti-tumor effects of expanded NK cells, human hepatocellular carcinoma SNU354 cells were transplanted to Balb/c nu/nu nude mice (Nara Biotech Co. Seoul, Korea) via subcutaneous injection (6×106 cells/mouse). The 2 h later, expanded NK cells (1 or 2×107 cells/mouse) with or without cryopreservation were administered into the tail vein. Thereafter, NK cells were administered at 1-wk intervals a total of 4 times. As vehicle controls, human serum albumin-Hartman solution (5%; JW Pharmaceutical, Seoul, Korea) or freezing medium was administered intravenously on the same schedule. Doxorubicin (2 mg/kg; Sigma-Aldrich) was intraperitoneally administered 13 times at 2-day intervals as a positive control. Mice were monitored for weight changes and clinical signs, and the anti-tumor efficacy of infused NK cells was evaluated by measuring the tumor size from day 9 to day 28 and tumor weight on the final day. All experiments were performed in accordance with the national guidelines governing animal care in Korea.
In vivo animal model of lymphoma
To evaluate the in vivo ADCC activity of expanded NK cells, Raji cells (1×105 cells/mouse) were intravenously injected into the tail vein of CB-17-Prkdcscid mice (Charles River Laboratories, Yokohama, Japan), and expanded NK cells (2×107 cells/mouse) with or without cryopreservation were administered 5 times, every 2 or 3 days from day 1 to day 10. As a vehicle control, freezing medium was administered intravenously on the same schedule. Rituximab was administered subcutaneously, alone or with expanded NK cells, at a dose of 0.01 µg/mouse on day 1. Mice were monitored daily for tumor-associated morbidity, mortality, and paraplegia of the hind limbs. All experiments were performed in accordance with the national guidelines governing animal care in Korea.
Statistical analysis
Statistical analyses were performed using the Student's t-test. A p-value <0.05 was considered significant for all tests. Body weight and tumor size were analyzed by 2-way ANOVA and Bonferroni's multiple comparison test. Tumor weight was analyzed by 1-way ANOVA and Dunnett's multiple comparison test. Statistical analyses were performed using GraphPad Prism software (GraphPad Software Inc., La Jolla, CA, USA).
RESULTS
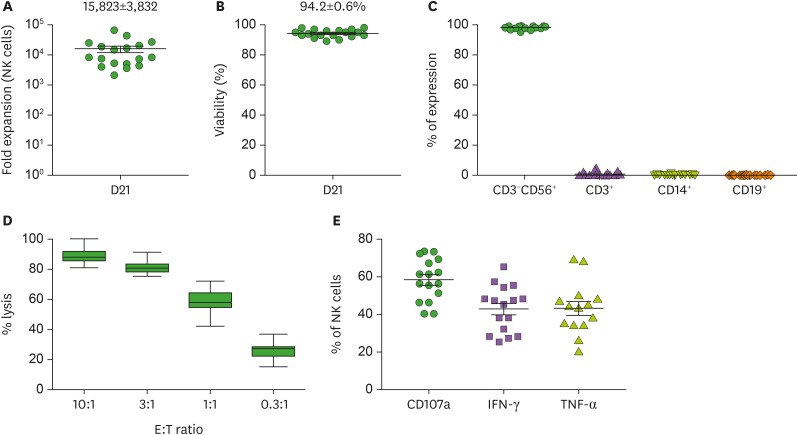
Characteristics of large-scale expanded NK cells
We previously established a method for large-scale expansion of NK cells for 2 wk (12). However, we needed to improve the method to obtain larger numbers of NK cells in the product and expanded NK cells for 3 weeks in a modified method. CD3+ T cell-depleted PBMCs were stimulated with irradiated autologous PBMCs in the presence of IL-2 and OKT3 on days 0 and 7 to increase the number of NK cells. During 21 days of culture, the number of NK cells increased up to 15,000-fold on average (Fig. 1A). The expansion kinetics of NK cells from 16 donors is presented (Supplementary Fig. 1). On day 21, the viability of the expanded cells was 94.2%±0.6% (Fig. 1B) and the percentage of CD3−CD56+ NK cells was 98.2%±0.3%, whereas the percentages of CD3+ T cells, CD14+ monocytes, and CD19+ B cells were 0.9%±0.3%, 0.2%±0.1%, and 0.11%±0.1%, respectively (Fig. 1C; Supplementary Fig. 2). The expanded cells were assessed for direct killing activity and cytokine secretion in response to K562 cells. The expanded cells exhibited robust cytolytic activity against K562 cells, particularly at high E:T ratios (Fig. 1D). In addition, they demonstrated vigorous degranulation activity as measured by CD107a expression and strong activity for IFN-γ and TNF-α secretion (Fig. 1E).
Figure 1. Characterization of NK cells expanded for 21 days in large-scale. CD3-depleted cells were expanded by stimulating irradiated PBMCs in the presence of IL-2 and OKT3 on 0 days and 7 days. (A) The fold expansion of NK cells was assessed after 21 days of culture (n=18). (B) The viability of expanded cells was measured by an automatic cell counter using propidium iodide (n=18). (C) The percentages of NK cells, T cells, monocytes, and B cells were analyzed by CD3−CD56+, CD3+, CD14+ and CD19+ phenotype, respectively (n=18). (D) Direct cytotoxicity was assessed by Calcein-AM release assay. Expanded NK cells were co-cultured with K562 cells for 4 h at E:T) ratios of 10:1 to 0.3:1 (n=18). (E) Intracellular cytokines (IFN-γ and TNF-α) and CD107a expression were assessed by flow cytometry. Expanded cells were co-cultured with K562 cells for 4 h at the E:T ratio of 1:1 (n=16). Mean and standard error are presented.
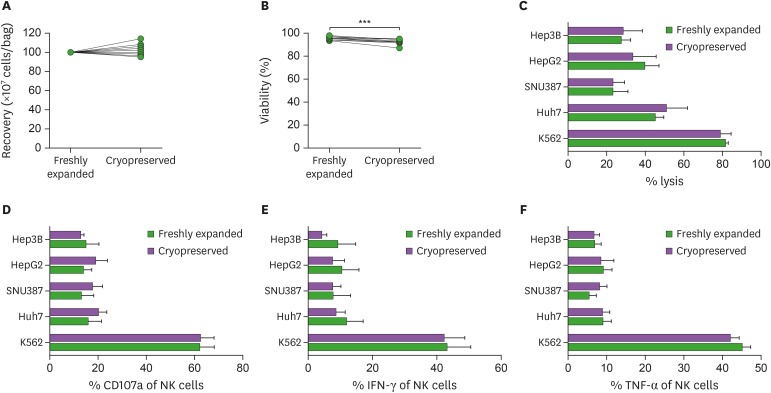
Functional activities of ex vivo-expanded NK cells with or without cryopreservation
We established an optimal freezing medium for expanded NK cells by testing various freezing media that can be applied to clinical trials. We evaluated changes in the characteristics of expanded NK cells after cryopreservation. Cryopreserved NK cells were analyzed immediately after thawing without further culture or cytokine stimulation. When expanded NK cells were frozen and thawed, we found no significant difference in cell recovery compared to freshly expanded NK cells (Fig. 2A), but the cell viability was reduced from 95.9%±0.5% to 92.2%±0.8% after cryopreservation (p=0.0003; Fig. 2B). However, direct cytotoxicity against K562 cells and various hepatocellular carcinoma cells was not significantly different with or without cryopreservation (Fig. 2C). In addition, the degranulation activity measured by CD107a expression and the secretion of IFN-γ and TNF-α was not significantly different with or without cryopreservation when NK cells were co-cultured with K562 cells and various hepatocellular carcinoma cells (Fig. 2D). We also analyzed cryopreserved NK cells not only immediately after thawing but also after incubation for 24 or 48 h with or without IL-2 (500 IU/ml) following thawing. As results, the cell number, viability, and cytotoxic activity of thawed NK cells were not significantly influenced by the incubation time and the presence of IL-2 (Supplementary Fig. 3). Therefore, the cryopreservation of expanded NK cells did not impair the cytotoxic activity and cytokine-secreting activity, though it slightly reduced the cell viability.
Figure 2. Comparison of freshly expanded and cryopreserved NK cells. (A) The cell recovery was expressed as the number of total nucleated cells per bag before and after cryopreservation (n=9). (B) The viability was measured by an automatic cell counter using propidium iodide before and after cryopreservation (n=9). (C) Killing activity of NK cells was assessed by co-culture with various tumor cells for 4 h at the E:T ratio of 10:1. (D) Intracellular cytokines and CD107a expression of NK cells were assessed by co-culture with various tumors for 4 h at the E:T ratio of 1:1. Cryopreserved NK cells were analyzed immediately after thawing without further culture or cytokine stimulation. Mean and standard error are presented (n=6).
***p<0.001.
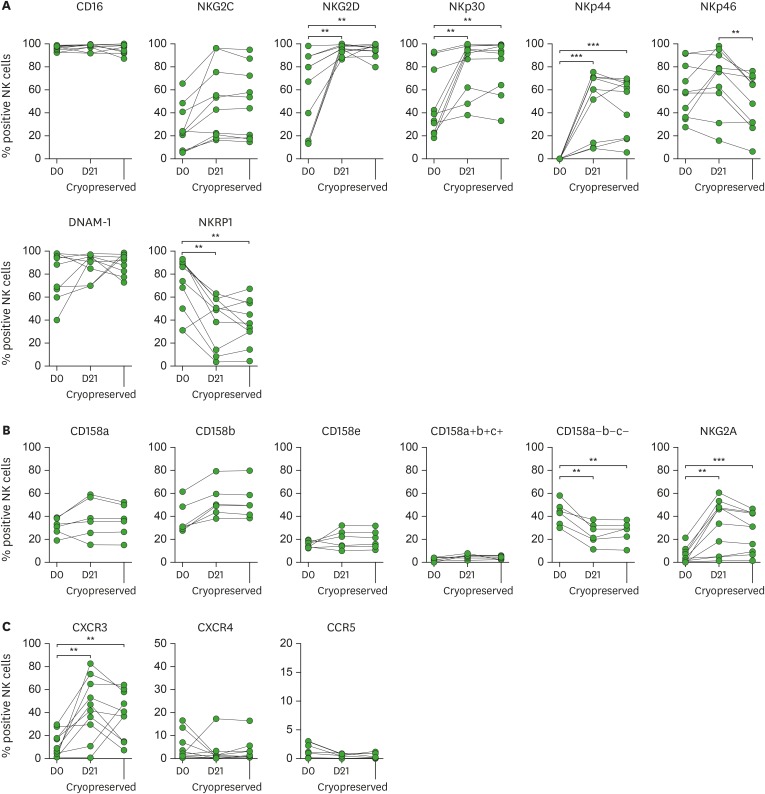
Phenotypes of ex vivo-expanded NK cells with or without cryopreservation
Next, we analyzed the expression of diverse receptors on NK cells before ex vivo expansion (day 0), after 21 days of expansion (day 21), and after freezing and thawing (cryopreservation). The 21-day expansion significantly increased the percentage of NK cells expressing activating receptors, such as NKG2D, NKp30, and NKp44, though the percentages of NK cells expressing CD16, NKG2C, NKp46, and DNAM-1 were not increased (Fig. 3A). The percentage of NKRP-1+ NK cells was significantly decreased by the 21-day expansion. Importantly, the percentages of NK cells expressing activating receptors were not further changed by freezing and thawing, with the exception of NKp46 (Fig. 3A); the percentage of NKp46+ NK cells was significantly decreased by cryopreservation (Fig. 3A). We also examined the expression of inhibitory receptors. The percentage of NK cells expressing CD158 killer inhibitory receptors (KIRs) was not changed by the 21-day expansion (Fig. 3B). However, the percentage of CD158 KIR− NK cells was significantly reduced and the percentage of NKG2A+ NK cells significantly increased by the 21-day expansion. The percentages of NK cells expressing inhibitory receptors were not further changed by freezing and thawing (Fig. 3B). Among chemokine receptors, the percentage of CXCR3+ NK cells was significantly increased by the 21-day expansion, whereas the percentages of CXCR4+ or CCR5+ NK cells were not changed (Fig. 3C). There were no further changes in the expression of chemokine receptors by freezing and thawing NK cells.
Figure 3. Phenotypic analysis of NK cells before expansion (D0), after expansion (D21), and after cryopreservation. Expression of activating receptors (A), inhibitory receptors (B), and chemokine receptors (C) of NK cells was analyzed by flow cytometry. Cryopreserved NK cells were analyzed immediately after thawing without further culture or cytokine stimulation.
**p<0.01; ***p<0.001.
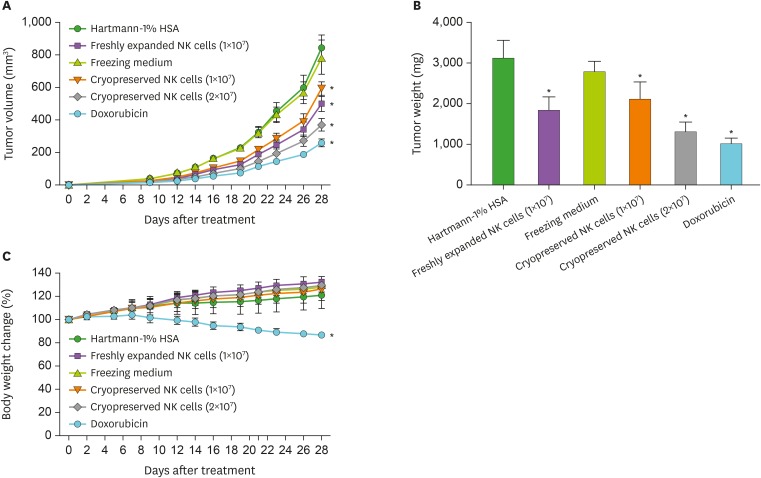
In vivo anti-tumor activity of expanded NK cells with or without cryopreservation
We assessed the in vivo anti-tumor activity of expanded NK cells using a SNU354 xenograft mouse model. When the same dose (1×107 cells/mouse) of expanded NK cells was administered, cryopreserved NK cells had lower tumor inhibition than freshly expanded NK cells, though the difference was slight (Fig. 4A). This reduced efficacy was overcome by the administration of a 2-fold dose (2×107 cells/mouse) of cryopreserved NK cells. In addition, the administration of a 2-fold dose (2×107 cells/mouse) of cryopreserved NK cells resulted in significantly higher anti-tumor efficacy than the regular dose (1×107 cells/mouse) of freshly expanded NK cells (Fig. 4A). These results were confirmed by evaluating tumor weight when the mice were sacrificed (Fig. 4B). However, no special signs and safety issues were observed in expanded NK cell-administered mice, regardless of cryopreservation. Animals exhibited normal weight increases except the doxorubicin-treated group (Fig. 4C). Our data indicate that cryopreservation slightly decreases the anti-tumor activity of expanded NK cells, but it can be overcome by dosage control.
Figure 4. Anti-tumor activity of freshly expanded and cryopreserved NK cells in SNU354 xenograft model. SNU354 cells were subcutaneously transplanted into nude mice. NK cells were administered into a caudal vein of nude mice 2 h after transplantation of SNU354 cells, and NK cells were administered once a week (total 4 times). Cryopreserved NK cells were used immediately after thawing without further culture or cytokine stimulation. Doxorubicin (positive control) was administered total 13 times at 2-day intervals. (A) Tumor size was measured 9 times from day 9. (B) Tumors were isolated and weighed at the final day. (C) Body weight changes of mice compared to the body weight at day 0 (100%) were assessed. Mean and standard deviation are presented (n=10).
*p<0.01.
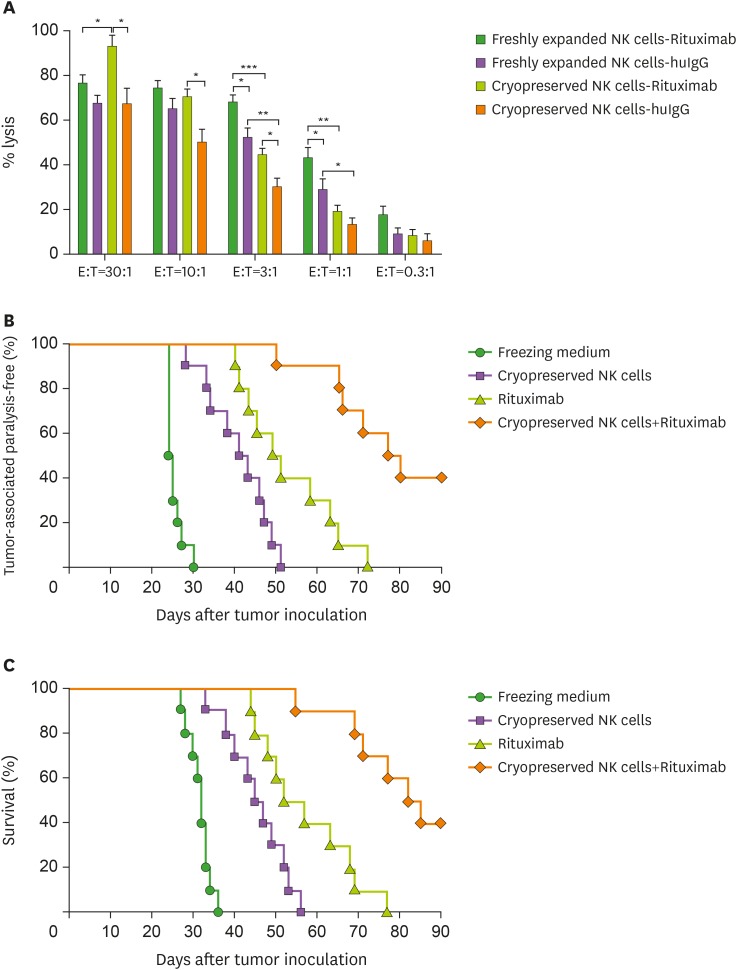
ADCC activity of expanded and cryopreserved NK cells
We also evaluated whether ex vivo-expanded and cryopreserved NK cells exert ADCC activity against Raji lymphoma cells in the presence of rituximab, an anti-CD20 monoclonal antibody. In in vitro ADCC assays, addition of rituximab increased the cytotoxic activity of both freshly expanded NK cells and cryopreserved NK cells after expansion (Fig. 5A). However, cryopreservation reduced the ADCC activity against Raji cells when the E:T ratio was 3:1 or less, but there was no difference in the ADCC activity when the E:T ratio was 10:1 or more (Fig. 5A). To investigate the in vivo anti-tumor ADCC activity, we administered ex vivo-expanded and cryopreserved NK cells with low-dose rituximab to SCID mice injected intravenously with Raji cells, assessing hind-leg paralysis and mortality for 90 days. Hind-leg paralysis developed from day 24 in the vehicle control (freezing medium) group (Fig. 5B), but was delayed by the administration of either cryopreserved NK cells or rituximab, and further delayed by co-administration of cryopreserved NK cells and rituximab (Fig. 5B). The median survival was 32 days for the vehicle control (freezing medium) group, and it was prolonged by the administration of either cryopreserved NK cells (46 days) or rituximab (54.5 days) (Fig. 5C). The median survival was further prolonged by co-administration of cryopreserved NK cells and rituximab up to 83.5 days (Fig. 5C). These results indicate that co-administration of rituximab and expanded/cryopreserved NK cells leads to a desirable therapeutic effect.
Figure 5. The ADCC activity of cryopreserved NK cells in combination with rituximab in Raji lymphoma model. (A) In vitro ADCC activity of expanded NK cells with or without cryopreservation was assessed against Raji cells. Cryopreserved NK cells were used immediately after thawing without further culture or cytokine stimulation. Calcein-AM labeled Raji cells were co-cultured with NK cells for 4 h at E:T ratios of 30:1 to 0.3:1 in the presence of rituximab or huIgG. The percentage of specific lysis of Raji cells is expressed as the mean±standard error (n=6). (B, C) To determine in vivo ADCC activity of cryopreserved NK cells, Raji cells were intravenously transplanted into SCID mice and cryopreserved NK cells were administered 5 times at 2 to 3-day intervals. Cryopreserved NK cells were used immediately after thawing without further culture or cytokine stimulation. Rituximab was administered with NK cells together on day 1. Paralysis (%) (B) and survival rate (%) (C) were assessed.
huIgG, human IgG.
*p<0.05; **p<0.01; ***p<0.001.
DISCUSSION
Allogeneic NK cell therapy has been developed for the treatment of cancer patients because NK cells with KIR-major histocompatibility incompatibility could induce a graft-versus-tumor response without causing GVHD (21). In our previous study, we established an efficient method for large-scale expansion of NK cells from healthy donors under GMP conditions for 2 weeks (12). We also completed a phase I clinical trial for solid tumor patients, administering NK cells produced from the 2 week-manufacturing process (11). However, the expansion of NK cells by the 2 wk-manufacturing process was limited in terms of the number of NK cells in the final products. Moreover, we could not cryopreserve the expanded NK cells because the effect of freezing and thawing on the expanded NK cells was not established. Therefore, we produced NK cell products several times for high-dose administration, which was inconvenient due to the labor-intensive manufacturing process, high-cost quality control, and short shelf-life.
In the present study, we expanded NK cells for 3 wk for larger-scale expansion. The difference in fold expansion of NK cells between 2-wk (691±170) and 3-wk cultures (15,823±3,832) was 23 times on average. Despite the robust proliferation of 3-wk cultured NK cells, they exhibited strong cytotoxic activity and cytokine production. The highly efficient expansion of functionally active NK cells urged us to establish a method to cryopreserve them without impairing their survival and functional activity.
Previous studies reported that cryopreservation of NK cells reduces their cytotoxicity against tumor cells immediately after thawing (16,22). The cytotoxic activity of frozen and thawed NK cells was recovered by culturing them with IL-2, but most of the cells died during this process (16). Therefore, cryopreserved NK cells were difficult to apply in clinical practice (23). However, a recent report demonstrated that expanded/frozen NK cells maintain their phenotype, cytotoxicity, and cytokine production after thawing (17). We established a freezing medium applicable to clinical practice to develop an effective freezing method for expanded NK cells (PCT/KR2017/000859). In the present study, we observed that expanded/frozen NK cells in this freezing medium maintained their viability, phenotype, cytotoxicity, and cytokine production immediately after thawing. Although the cell viability was decreased after freezing and thawing, the difference was less than 4%. Therefore, we successfully established a large-scale NK cell culture system and optimal freezing condition that maintains viability and function without damaging the expanded NK cells.
We also examined whether cryopreservation affects the in vivo anti-tumor activity of ex vivo-expanded NK cells using a SNU354 xenograft mouse model. No study has compared the in vivo anti-tumor efficacy of expanded NK cells with or without cryopreservation until now. We found that the 2-fold dose of expanded/frozen NK cells resulted in significantly higher anti-tumor efficacy than freshly expanded NK cells, though expanded/frozen NK cells had slightly lower anti-tumor efficacy at the same dose. Therefore, we conclude that cryopreservation slightly decreases the anti-tumor activity of expanded NK cells, but it can be overcome with increased dosage.
NK cells exert ADCC activity because they express CD16 Fc receptor (FcγRIII). The percentage of CD16+ NK cells was not changed by cryopreservation. Recently, the combination of NK cells with therapeutic antibodies was shown to suppress tumors more effectively (24,25). Rituximab is the first monoclonal antibody successfully used for the treatment of patients with CD20+ lymphoma or leukemia (26,27). In the present study, we used rituximab to assess the in vitro ADCC activity of expanded/frozen NK cells. As a result, cryopreservation reduced ADCC activity against Raji cells when the E:T ratio was 3:1 or less. However, there was no difference in the ADCC activity with or without cryopreservation when the E:T ratio was 10:1 or more (Fig. 5A). These data suggest that cryopreservation slightly decreases the ADCC activity of expanded NK cells, but it may be overcome by increasing the dose of NK cells. We also evaluated in vivo ADCC activity using SCID mice injected intravenously with Raji cells. The survival and paralysis of the mice were significantly improved by administering rituximab and cryopreserved NK cells immediately after thawing.
In conclusion, we established a method for optimal cryopreservation of ex vivo-expanded NK cells for adoptive immunotherapy. This freezing formulation of expanded allogeneic NK cells is currently being applied in a phase II clinical trial of patients with hepatocellular carcinoma after transcatheter arterial chemoembolization (ClinicalTrials.gov, NCT02854839) in Korea, which will demonstrate the safety and efficacy. In the present study, we demonstrated that expanded/frozen NK cells maintain their viability, phenotype, and functional activity in vitro and anti-tumor efficacy in vivo immediately after thawing without further culture with IL-2. These results indicate that expanded/frozen NK cells can complete all quality control tests before the scheduled administration, provide ‘ready-to-use’ cell therapy for patients, and be supplied worldwide regardless of distance.
Abbreviations
- ADCC
antibody-dependent cell cytotoxicity
- E:T
effector:target
- FBS
fetal bovine serum
- GVHD
graft-versus-host disease
- IFN
interferon
- KIR
killer inhibitory receptor
- NK
natural killer
- PBMC
peripheral blood mononuclear cell
- TNF
tumor necrosis factor
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
Author Contributions: Conceptualization: Min B, Choi H, Hwang YK, Shin EC; Formal analysis: Min B, Choi H, Her JH, Jung MY; Investigation: Min B, Choi H, Her JH, Jung MY, Kim HJ, Jung MY, Lee EK; Methodology: Min B, Choi H, Her JH; Supervision: Cho SY, Hwang YK, Shin EC; Writing - original draft: Min B, Hwang YK, Shin EC; Writing - review & editing: Min B, Cho SY, Hwang YK, Shin EC.
SUPPLEMENTARY MATERIALS
Growth kinetics of NK cells expanded for 21 days in a large-scale. For NK cell expansion, CD3-depleted cells were expanded by stimulating with γ-irradiated autologous PBMCs in the presence of IL-2 and OKT3 on days 0 and 7. Mean and standard deviation of total cell numbers are presented (n=16).
Gating strategy for identification of various immune cells. Figures present gating strategy to define CD3−CD56+ NK cells, CD3+ T cells, CD14+ monocytes and CD19+ B cells in flow cytometry analysis.
Characteristics of cryopreserved NK cells with or without incubation and/or IL-2 stimulation after thawing. The cell number (A), viability (B), and cytotoxic activity (C) of cryopreserved NK cells were examined with or without incubation (24 or 48 h) and/or IL-2 (500 IU/ml) stimulation after thawing. The cytotoxic activity was assessed by co-culture with K562 cells for 4 h at the E:T ratio of 10:1. Mean and standard error are presented (n=3).
References
- 1.Lanier LL, Phillips JH, Hackett J, Jr, Tutt M, Kumar V. Natural killer cells: definition of a cell type rather than a function. J Immunol. 1986;137:2735–2739. [PubMed] [Google Scholar]
- 2.Robertson MJ, Ritz J. Biology and clinical relevance of human natural killer cells. Blood. 1990;76:2421–2438. [PubMed] [Google Scholar]
- 3.Beano A, Signorino E, Evangelista A, Brusa D, Mistrangelo M, Polimeni MA, Spadi R, Donadio M, Ciuffreda L, Matera L. Correlation between NK function and response to trastuzumab in metastatic breast cancer patients. J Transl Med. 2008;6:25. doi: 10.1186/1479-5876-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trapani JA, Smyth MJ. Functional significance of the perforin/granzyme cell death pathway. Nat Rev Immunol. 2002;2:735–747. doi: 10.1038/nri911. [DOI] [PubMed] [Google Scholar]
- 5.Deauvieau F, Ollion V, Doffin AC, Achard C, Fonteneau JF, Verronese E, Durand I, Ghittoni R, Marvel J, Dezutter-Dambuyant C, et al. Human natural killer cells promote cross-presentation of tumor cell-derived antigens by dendritic cells. Int J Cancer. 2015;136:1085–1094. doi: 10.1002/ijc.29087. [DOI] [PubMed] [Google Scholar]
- 6.Lim O, Jung MY, Hwang YK, Shin EC. Present and future of allogeneic natural killer cell therapy. Front Immunol. 2015;6:286. doi: 10.3389/fimmu.2015.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK, McKenna D, Le C, Defor TE, Burns LJ, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood. 2005;105:3051–3057. doi: 10.1182/blood-2004-07-2974. [DOI] [PubMed] [Google Scholar]
- 8.Iliopoulou EG, Kountourakis P, Karamouzis MV, Doufexis D, Ardavanis A, Baxevanis CN, Rigatos G, Papamichail M, Perez SA. A phase I trial of adoptive transfer of allogeneic natural killer cells in patients with advanced non-small cell lung cancer. Cancer Immunol Immunother. 2010;59:1781–1789. doi: 10.1007/s00262-010-0904-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krause SW, Gastpar R, Andreesen R, Gross C, Ullrich H, Thonigs G, Pfister K, Multhoff G. Treatment of colon and lung cancer patients with ex vivo heat shock protein 70-peptide-activated, autologous natural killer cells: a clinical phase i trial. Clin Cancer Res. 2004;10:3699–3707. doi: 10.1158/1078-0432.CCR-03-0683. [DOI] [PubMed] [Google Scholar]
- 10.Geller MA, Cooley S, Judson PL, Ghebre R, Carson LF, Argenta PA, Jonson AL, Panoskaltsis-Mortari A, Curtsinger J, McKenna D, et al. A phase II study of allogeneic natural killer cell therapy to treat patients with recurrent ovarian and breast cancer. Cytotherapy. 2011;13:98–107. doi: 10.3109/14653249.2010.515582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Y, Lim O, Kim TM, Ahn YO, Choi H, Chung H, Min B, Her JH, Cho SY, Keam B, et al. Phase I study of random healthy donor–derived allogeneic natural killer cell therapy in patients with malignant lymphoma or advanced solid tumors. Cancer Immunol Res. 2016;4:215–224. doi: 10.1158/2326-6066.CIR-15-0118. [DOI] [PubMed] [Google Scholar]
- 12.Lim O, Lee Y, Chung H, Her JH, Kang SM, Jung MY, Min B, Shin H, Kim TM, Heo DS, et al. GMP-compliant, large-scale expanded allogeneic natural killer cells have potent cytolytic activity against cancer cells in vitro and in vivo . PLoS One. 2013;8:e53611. doi: 10.1371/journal.pone.0053611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lundqvist A, Berg M, Smith A, Childs RW. Bortezomib treatment to potentiate the anti-tumor immunity of ex-vivo expanded adoptively infused autologous natural killer cells. J Cancer. 2011;2:383–385. doi: 10.7150/jca.2.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Denman CJ, Senyukov VV, Somanchi SS, Phatarpekar PV, Kopp LM, Johnson JL, Singh H, Hurton L, Maiti SN, Huls MH, et al. Membrane-bound IL-21 promotes sustained ex vivo proliferation of human natural killer cells. PLoS One. 2012;7:e30264. doi: 10.1371/journal.pone.0030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lapteva N, Durett AG, Sun J, Rollins LA, Huye LL, Fang J, Dandekar V, Mei Z, Jackson K, Vera J, et al. Large-scale ex vivo expansion and characterization of natural killer cells for clinical applications. Cytotherapy. 2012;14:1131–1143. doi: 10.3109/14653249.2012.700767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berg M, Lundqvist A, McCoy P, Jr, Samsel L, Fan Y, Tawab A, Childs R. Clinical-grade ex vivo-expanded human natural killer cells up-regulate activating receptors and death receptor ligands and have enhanced cytolytic activity against tumor cells. Cytotherapy. 2009;11:341–355. doi: 10.1080/14653240902807034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torelli GF, Rozera C, Santodonato L, Peragine N, D'agostino G, Montefiore E, Napolitano MR, Monque DM, Carlei D, Mariglia P, et al. A good manufacturing practice method to ex vivo expand natural killer cells for clinical use. Blood Transfus. 2015;13:464–471. doi: 10.2450/2015.0231-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller JS, Rooney CM, Curtsinger J, McElmurry R, McCullar V, Verneris MR, Lapteva N, McKenna D, Wagner JE, Blazar BR, et al. Expansion and homing of adoptively transferred human natural killer cells in immunodeficient mice varies with product preparation and in vivo cytokine administration: implications for clinical therapy. Biol Blood Marrow Transplant. 2014;20:1252–1257. doi: 10.1016/j.bbmt.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Szmania S, Lapteva N, Garg T, Greenway A, Lingo J, Nair B, Stone K, Woods E, Khan J, Stivers J, et al. Ex vivo-expanded natural killer cells demonstrate robust proliferation in vivo in high-risk relapsed multiple myeloma patients. J Immunother. 2015;38:24–36. doi: 10.1097/CJI.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neri S, Mariani E, Meneghetti A, Cattini L, Facchini A. Calcein-acetyoxymethyl cytotoxicity assay: standardization of a method allowing additional analyses on recovered effector cells and supernatants. Clin Diagn Lab Immunol. 2001;8:1131–1135. doi: 10.1128/CDLI.8.6.1131-1135.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A, Posati S, Rogaia D, Frassoni F, Aversa F, et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science. 2002;295:2097–2100. doi: 10.1126/science.1068440. [DOI] [PubMed] [Google Scholar]
- 22.Holubova M, Miklikova M, Leba M, Georgiev D, Jindra P, Caprnda M, Ciccocioppo R, Kruzliak P, Lysak D. Cryopreserved NK cells in the treatment of haematological malignancies: preclinical study. J Cancer Res Clin Oncol. 2016;142:2561–2567. doi: 10.1007/s00432-016-2247-8. [DOI] [PubMed] [Google Scholar]
- 23.Klingemann H. Challenges of cancer therapy with natural killer cells. Cytotherapy. 2015;17:245–249. doi: 10.1016/j.jcyt.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 24.Mentlik James A, Cohen AD, Campbell KS. Combination immune therapies to enhance anti-tumor responses by NK cells. Front Immunol. 2013;4:481. doi: 10.3389/fimmu.2013.00481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Battella S, Cox MC, Santoni A, Palmieri G. Natural killer (NK) cells and anti-tumor therapeutic mAb: unexplored interactions. J Leukoc Biol. 2016;99:87–96. doi: 10.1189/jlb.5VMR0415-141R. [DOI] [PubMed] [Google Scholar]
- 26.Weiner GJ. Rituximab: mechanism of action. Semin Hematol. 2010;47:115–123. doi: 10.1053/j.seminhematol.2010.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hallek M, Fischer K, Fingerle-Rowson G, Fink AM, Busch R, Mayer J, Hensel M, Hopfinger G, Hess G, von Grünhagen U, et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet. 2010;376:1164–1174. doi: 10.1016/S0140-6736(10)61381-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Growth kinetics of NK cells expanded for 21 days in a large-scale. For NK cell expansion, CD3-depleted cells were expanded by stimulating with γ-irradiated autologous PBMCs in the presence of IL-2 and OKT3 on days 0 and 7. Mean and standard deviation of total cell numbers are presented (n=16).
Gating strategy for identification of various immune cells. Figures present gating strategy to define CD3−CD56+ NK cells, CD3+ T cells, CD14+ monocytes and CD19+ B cells in flow cytometry analysis.
Characteristics of cryopreserved NK cells with or without incubation and/or IL-2 stimulation after thawing. The cell number (A), viability (B), and cytotoxic activity (C) of cryopreserved NK cells were examined with or without incubation (24 or 48 h) and/or IL-2 (500 IU/ml) stimulation after thawing. The cytotoxic activity was assessed by co-culture with K562 cells for 4 h at the E:T ratio of 10:1. Mean and standard error are presented (n=3).