Abstract
Splenic artery aneurysms are common arterial lesions which might remain asymptomatic for a long period of time. In certain cases, these lesions might encounter a significant growth and might become symptomatic. Once diagnosed, a therapeutic strategy should be taken in consideration in order to avoid the apparition of life-threatening complications such as aneurysmal rupture. This is a case report of a 45-year-old patient diagnosed with a splenic artery aneurysm who was successfully submitted to an aneurysmal resection en bloc with distal spleno-pancreatectomy and parcelar gastrectomy.
Keywords: Splenic artery aneurysm, resection, distal splenopancreatectomy
Visceral arteries aneurysms represent uncommon but life-threatening situations, their global incidence being up to 10% in autopsy series; among these cases splenic artery aneurysms account for up to 60% of cases, being the third reported location of an aneurysmal dilatation after aortic and iliac lesions (1,2). Described for the first time by Beaussier in 1770, splenic artery aneurysms are defined by the presence of a splenic artery dilatation to more than 2 cm in diameter and are usually much more common in women compared to men (3,4). The most frequently incriminated risk factors include portal and arterial hypertension, atherosclerosis, traumas, arterial vascular lesions (such as fibrodysplasia) or after liver transplant (5,6). Among patients with splenic artery aneurysms only 20% are symptomatic while up to 3% of them will develop aneurysmal rupture; whenever this catastrophic scenario occurs, the mortality rate significantly increases, death being reported in up to 35% of cases (6). Due to these reasons, whenever a large splenic artery aneurysm is detected, therapeutic gestures should be taken in consideration in order to prevent the development of further complications.
Case Report
A 45-year-old patient with no significant medical history presented with severe upper abdominal pain and vomiting. The clinical examination did not reveal any pathological aspects while the biological tests were rather normal; however, the abdominal ultrasound revealed the presence of a large epigastric mass in close contact with the pancreatic body and tail, raising the suspicion of a splenic artery aneurysm. The patient was further submitted to a computed tomography angiogram which confirmed the presence of a partially clotted splenic artery aneurysm in close contact with the pancreas as well as with the posterior gastric wall measuring 7/5/5 cm (Figure 1 and Figure 2). The patient was submitted to surgery where the splenic artery aneurysm was resected en bloc with distal pancreatectomy, splenectomy and posterior parcelar gastrectomy (Figure 3 and Figure 4). The postoperative course was uneventful, and the patient was discharged in the fifth postoperative day. The histopathological studies revealed the presence of a 7.5/5.4/4.8 cm true aneurysm, all the three vascular layers being well represented; in the meantime, the pancreatic parenchyma was rather normal, no signs of acute or chronic pancreatitis being revealed. Therefore, these two aspects (the presence of the three layers of the vascular wall in association with a normal histology of the pancreatic parenchyma) enabled us to consider the lesion as a true one (and not a pseudoaneurysmal dilatation of the splenic artery).
Figure 1. Computed tomography (coronal view) revealing the presence of a splenic artery aneurysmal dilatation in close contact with the posterior gastric wall.

Figure 2. Computed tomography (axial view) revealing the presence of a splenic artery aneurysmal dilatation embedded by the pancreatic body and tai .
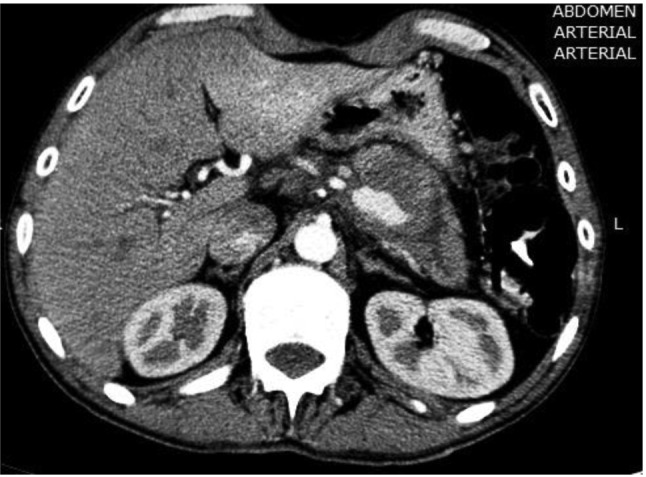
Figure 3. The final intraoperative aspect after removing the splenic artery aneurysm en bloc with distal pancreatectomy, splenectomy and parcelar gastrectomy. Forceps pointing the splenic artery stump.
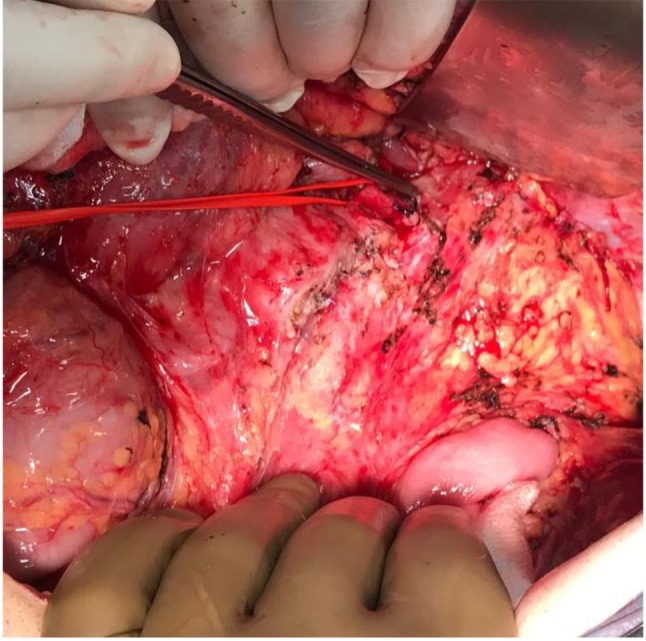
Figure 4. The specimen of splenic artery aneurysm en bloc with distal pancreatectomy, splenectomy and parcelar gastrectomy. On section the presence of intra-aneurysmal blood cloths can be observed.

Discussion
Splenic artery aneurysms usually develop at the level of the main splenic artery trunk, before its bifurcation; in up to 75% of cases they are located in the distal third of the arterial trunk followed by the middle third of the artery (in up to 20% of cases) (7,8). These vascular malformations rarely exceed 3 cm in diameter and are associated with other visceral aneurysms in up to 14% of cases (9). Depending on their structure, splenic artery aneurysms might be true lesions (if all the three layers of the arterial wall are affected) or pseudoaneurysms (if one or more vessel’s layer lack) (10). Regarding the etiology, the most commonly incriminated causes for the development of a true splenic artery aneurysm include arterial or portal hypertension, cirrhosis, liver transplantation or pregnancy (9,11). In the meantime, in cases developing pseudoaneurysmal dilatation of the splenic artery the most commonly incriminated pathogenic factor is represented by chronic pancreatitis; in such cases it is believed that the pancreatic enzymes released at the moment of each episode of pancreatitis will induce the fragmentation of the elastic layer of the vessel inducing in this way a pseudoaneurysmal dilatation (12).
Although the majority of patients with this pathology remain asymptomatic for a long period of time, the aneurysm being incidentally discovered during routine abdominal imaging, epigastric pain, anorexia or vomiting might be reported (10). A dramatic scenario in such cases is represented by the aneurysmal rupture, where at that moment the patient presents sharp abdominal pain and hemodynamic shock (13,14). In such situations mortality rate reaches 25% of cases; therefore, it is strongly recommended that a therapeutic gesture is performed whenever a large splenic artery aneurysm is detected. Trastek et al. recommend that all aneurysms larger than 2 cm as well as those in which an increase during a follow-up period is reported to be treated; moreover, pregnant women or those who plan to become pregnant and who are diagnosed with an asymptomatic splenic artery aneurysm should be also submitted to a therapeutic maneuver regarding this vascular malformation (15).
Therapeutic options in such cases include a large variety of strategies including standard surgery (consisting of resection) or endovascular surgical procedures (such as percutaneous stent placement or percutaneous aneurysmal embolization). Although percutaneous maneuvers intend to be less invasive and assure a good preservation of the spleen, a significant rate of splenic infarcts or impaired splenic function has been reported (16). Percutaneous embolization of the splenic artery aneurysms was initially described by Probst et al. in 1978 and has been widely performed in asymptomatic patients presenting splenic artery aneurysms (excluding those in which the lesion is located in the splenic hylum) (17). However, this therapeutic strategy remains the option of choice in patients presenting high risk for a classic surgical approach, an important number of cases developing complications (such as coil migration, infarction, splenic abscess, aneurysmal recanalization or even aneurysmal rupture) (18); moreover, embolization might fail in cases presenting tortuous splenic arteries (10). Endovascular stent placement might be also tempted; however, the method has the same limitations as the embolization, size, localization and tortuosity of the splenic artery being sometimes responsible for the failure of this method (10). However, this method has a lower risk of splenic infarction (10).
In cases in which percutaneous endovascular techniques fail or cannot be applied, classic surgery remains the option of choice. The strong development of the vascular surgery techniques in patients presenting splanchnic arteries’ malformations played a central role as part of the management of patients presenting visceral aneurysms (19-21). Moreover, surgical intervention is considered as the conventional treatment in most centers especially in patients presenting large symptomatic lesions (22). This is the explanation why surgery was proposed as the first intention treatment in our case (large aneurysm in a symptomatic patient).
In a large study conducted by the surgeons from Ohio regarding the therapeutic strategies in patients diagnosed with splenic artery aneurysms, 128 such cases were introduced (23). Among these cases open surgery was needed in 13 cases and consisted of aneurysmal resection or resection en bloc with splenectomy (in seven cases), aneurysmal ligation (in four cases) and arterial reconstruction (in two cases). Moreover, seven of the 13 cases were submitted to surgery for ruptured aneurysms, two of them dying due to the hemorrhagic shock. Other reported complications among surgically treated patients included postoperative bleeding requiring reoperation (in two cases), wound infection (in one case) and a pancreatic fistula (in one case). However, the postoperative length of hospital-stay was significantly longer among patients treated surgically when compared to those treated by an endovascular technique. This fact can be explained by the larger complexity of the cases treated by open surgery (23).
A similar case to the one presented in the current article was the one reported by Yadav and co. in the International Journal of Surgery Case Reports in 2012 (24). The authors reported the case of a 58-year-old female who presented for the apparition of a pulsatile mass in the left upper abdomen which proved to be a 10.6/10.38 cm splenic artery aneurysm arising from the distal segment, while the pancreas presented no pathological aspect. The patient was submitted to open surgery, the aneurysm being removed en bloc with distal pancreatectomy and splenectomy. The macroscopic analysis of the specimen revealed the presence of a 12.7/11.8 cm aneurysm with clotted blood inside, while the histopathological studies confirmed that it was a true arterial aneurysm, all the three layers being revealed (24).
When it comes to the necessity of associating a pancreatic resection, it seems that this gesture is almost always imposed when the aneurysmal dilatation is embedded within the pancreatic parenchyma (25), as in our case. Once the decision of performing a concomitant pancreatic resection is made, the surgeon should be aware of the significantly increased risk of developing acute postoperative complications such as pancreatic fistulas or long-term complications such as diabetes mellitus (26). However, due to improvements in the surgical technique and postoperative management of cases necessitating pancreatic resections, the perioperative morbidity rate significantly decreased in the last decades conducting to the safe association of pancreatic resections for various pathological processes involving these viscera (26,27,28).
Conclusion
Splenic artery aneurysms remain asymptomatic for a long period of time, being usually incidentally diagnosed while performing imagistic studies for other pathologies. However, once diagnosed these vascular malformations should be treated especially in patients presenting large lesions as well as in symptomatic patients, the most dangerous associated risk, if not treated, consisting of spontaneous rupture and life-threatening hemorrhage. In the current case, decision to submit the patient to surgery was imposed by the large dimension of the lesion, as well as by the important associated risk of spontaneous rupture.
References
- 1.Bedford PD, Lodge B. Aneurysm of the splenic artery. Gut. 1960;1:312–320. doi: 10.1136/gut.1.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dave SP, Reis ED, Hossain A, Taub PJ, Kerstein MD, Hollier LH. Splenic artery aneurysm in the 1990s. Ann Vasc Surg. 2000;14:223–229. doi: 10.1007/s100169910039. [DOI] [PubMed] [Google Scholar]
- 3.Beaussier M. Sur un aneurisimie de l’artere splenique dont les parois se sont ossifies. J Med Clin Pharm (Paris) 1770;32:157. [Google Scholar]
- 4.Arca MJ, Gagner M, Heniford BT, Sullivan TM, Beven EG. Splenic artery aneurysms: methods of laparoscopic repair. J Vasc Surg. 1999;30:184–188. doi: 10.1016/s0741-5214(99)70190-4. [DOI] [PubMed] [Google Scholar]
- 5.Mandal S, Das PM, Mandal AK. Caroli's syndrome leading to splenic artery aneurysm: a rare presentation. Int J Surg Pathol. 2009;17:78–80. doi: 10.1177/1066896908315805. [DOI] [PubMed] [Google Scholar]
- 6.Annicchiarico BE, Avolio AW, Caracciolo G, Barbaro B, Di Stasi C, Agnes S, Siciliano M. Late development of splenic artery aneurysm after orthotopic liver transplantation: a case report. Transplant Proc. 2009;41:1383–1385. doi: 10.1016/j.transproceed.2009.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Mattar SG, Lumsden AB. The management of splenic artery aneurysms: experience with 23 cases. Am J Surg. 1995;169:580–584. doi: 10.1016/s0002-9610(99)80225-6. [DOI] [PubMed] [Google Scholar]
- 8.Karaman K, Onat L, Sirvanci M, Olga R. Endovascular stent graft treatment in a patient with splenic artery aneurysm. Diagn Interv Radiol. 2005;11:119–121. [PubMed] [Google Scholar]
- 9.Abbas MA, Stone WM, Fowl RJ, Gloviczki P, Oldenburg WA, Pairolero PC, Hallett JW, Bower TC, Panneton JM, Cherry KJ. Splenic artery aneurysms: two decades experience at Mayo clinic. Ann Vasc Surg. 2002;16:442–449. doi: 10.1007/s10016-001-0207-4. [DOI] [PubMed] [Google Scholar]
- 10.Al Habbal Y, Christophi C, Muralidharan V. Aneurysms of the splenic artery – a review. Surgeon. 2010;8:223–231. doi: 10.1016/j.surge.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 11.Lee PC, Rhee RY, Gordon RY, Fung JJ, Webster MW. Management of splenic artery aneurysms: the significance of portal and essential hypertension. J Am Coll Surg. 1999;189:483–490. doi: 10.1016/s1072-7515(99)00168-4. [DOI] [PubMed] [Google Scholar]
- 12.Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC, Gloviczki P. Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Surg. 2003;38:969–974. doi: 10.1016/s0741-5214(03)00710-9. [DOI] [PubMed] [Google Scholar]
- 13.Sadat U, Dar O, Walsh S, Varty K. Splenic artery aneurysms in pregnancy – a systematic review. Int J Surg. 2008;6:261–265. doi: 10.1016/j.ijsu.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Khan HR, Low S, Selinger M, Nelson N. Splenic artery aneurysm rupture in pregnancy. J Coll Physicians Surg Pak. 2004;14:298–299. [PubMed] [Google Scholar]
- 15.Trastek VF, Pairolero PC, Joyce JW, Hollier LH, Bernatz PE. Splenic artery aneurysms. Surgery. 1982;91:694–699. [PubMed] [Google Scholar]
- 16.Nincheri KM, Pantalone D, Borri A, Paolucci R, Pernice LM, Taruffi F, Andreoli F. Management of true splenic artery aneurysms. Two case reports and review of the literature. Minerva Chir. 2003;58:247–256. [PubMed] [Google Scholar]
- 17.Probst P, Castaneda-Zuniga WR, Gomes AS, Yonehiro EG, Delaney JP, Amplatz K. Nonsurgical treatment of splenic-artery aneurysms. Radiology. 1978;128:619–623. doi: 10.1148/128.3.619. [DOI] [PubMed] [Google Scholar]
- 18.Reidy JF, Rowe PH, Ellis FG. Splenic artery aneurysm embolisation – the preferred technique to surgery. Clin Radiol. 1990;41:281–282. doi: 10.1016/s0009-9260(05)81667-8. [DOI] [PubMed] [Google Scholar]
- 19.Bacalbasa N, Brezean I, Anghel C, Barbu I, Pautov M, Balescu I, Brasoveanu V. successful resection and vascular ligation of a large hepatic artery aneurysm – A case report and literature review. In Vivo. 2017;31:979–982. doi: 10.21873/invivo.11157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bacalbasa N, Brezean I, Anghel C, Barbu I, Pautov M, Balescu I, Brasoveanu V. Management of a fulminant upper gastrointestinal bleeding exteriorized through hemobilia due to arteriobiliary fistula between the common bile duct and a right hepatic artery aneurysm – A case report. In Vivo. 2017;31:983–989. doi: 10.21873/invivo.11158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brasoveanu V, Anghel C, Barbu I, Pautov M, Ionescu MI, Motthor M, Balescu I, Dima S, Bacalbasa N. Pancreatoduodenectomy en bloc with portal and superior mesenteric artery resection – a case report and literature review. Anticancer Res. 2015;35:1613–1618. [PubMed] [Google Scholar]
- 22.Abdulrahman A, Shabkah A, Hassanain M, Aljiffry M. Ruptured spontaneous splenic artery aneurysm: A case report and review of the literature. Int J Surg Case Rep. 2014;5:754–757. doi: 10.1016/j.ijscr.2014.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lakin RO, Bena JF, Sarac TP, Shah S, Krajewski LP, Srivastava SD, Clair DG, Kashyap VS. The contemporary management of splenic artery aneurysms. J Vasc Surg. 2011;53:958–964. doi: 10.1016/j.jvs.2010.10.055. [DOI] [PubMed] [Google Scholar]
- 24.Yadav S, Sharma P, Singh PK, Punia S, Desai P, Anjan AK, Jain S. Giant splenic artery aneurysm: A rare but potentially catastrophic surgical challenge. Int J Surg Case Rep. 2012;3:533–536. doi: 10.1016/j.ijscr.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Messina LM, Shanley CJ. Visceral artery aneurysms. Surg Clin North Am. 1997;77:425–442. doi: 10.1016/s0039-6109(05)70559-4. [DOI] [PubMed] [Google Scholar]
- 26.Kitamura H, Nakayama K, Kitano T, Ozaki N, Nagaoka S. Removal of a splenic artery with a large aneurysm adhered to the pancreas without pancreatectomy: report of a case. Surg Today. 2002;32:747–749. doi: 10.1007/s005950200141. [DOI] [PubMed] [Google Scholar]
- 27.Bacalbasa N, Balescu I, Dima S, Brasoveanu V, Popescu I. Pancreatic resection as part of cytoreductive surgery in advanced-stage and recurrent epithelial ovarian cancer – A single-center experience. Anticancer Res. 2015;35:4125–4129. [PubMed] [Google Scholar]
- 28.Pantea S, Jiga L, Ionac M, Lazar F. Arterio-venous fistula using nonpenetrating titanium clips (VCS) Chirurgia (Bucur) 2013;108:563–567. [PubMed] [Google Scholar]


