Abstract
OBJECTIVES
Numerous challenges face clinically complex patients as they transition from hospital to home. The purpose of this project was to add pharmacy discharge services to an existing nurse-led discharge service (patient navigation program) to facilitate the transition of care process for clinically complex pediatric patients.
METHODS
For select patients referred to the service, a pharmacist resolved medication discrepancies, provided discharge counseling, and conducted follow-up telephone encounters on days 1, 7, and 14 post discharge. Patient demographics, admitting diagnosis, and number of discharge medications were recorded. The impact on patient outcomes was measured by the number and type of pharmacist interventions identified. Program utilization was measured by the number of referrals received, percentage of patients seen by a pharmacist, follow-up phone call completion rate, and pharmacist time required. Financial benefit gained from the program was estimated by translating each pharmaceutical intervention into potential cost savings.
RESULTS
There were 321 patient navigation referrals during the 5 months of pharmacist service. A pharmacist was able to provide discharge counseling for 56 discharges (17%). Patients who were provided pharmacy services had a median of 8 comorbidities, 10-day length of stay, and 4 discharge medications. Pharmacists identified 168 interventions, of which 93.5% were accepted or informational in nature. The most frequently identified interventions included clarification of drug order, assistance obtaining medication, and dose rounding. This program resulted in an estimated cost savings of $22,308 in the first 5 months.
CONCLUSIONS
A unique partnership between nurses and pharmacists facilitated the discharge process for clinically complex children.
Keywords: clinical pharmacy service, interprofessional health team, patient discharge, pediatrics, transitional care
Introduction
Patients and their families face many medication-related challenges during the discharge process, including medication errors and discrepancies, misunderstanding of discharge instructions, and difficulty obtaining new medications.1,2 Literature suggests that up to 60% of all medication errors occur during transitions of care,3,4 and nearly 1 in every 5 hospital discharges may result in readmission.5
Pediatric patients are at higher risk of medication errors resulting in harm or death owing to complex dosing regimens and limited evidence related to pediatric drug use and monitoring.6 In addition to prescribing errors, medication discrepancies (e.g., those that may appear in discharge paperwork) may pose a risk to pediatric patients. A prospective study to investigate medication discrepancies for the discharge of pediatric patients reported that 8% of medications contained discrepancies between documentation sources.7
To improve the discharge planning process, several hospitals have implemented programs in which patient navigators provide resources to guide patients through the discharge process. Studies have shown that the use of these navigators, who work to provide services such as increasing outpatient follow-up appointments and identifying medication discrepancies, can improve transitions of care.8–10 Several of these transition of care programs use pharmacists to optimize medication therapy and identify areas of potential medication safety concerns. Pharmacists working collaboratively with existing health care teams can help improve patient outcomes through medication reconciliation and medication counseling.3–5,11–13 Furthermore, initiatives to improve medication adherence may improve important clinical outcomes, such as readmission rates.14 However, there is limited published literature regarding pediatric transition of care programs. Therefore, this project aims to implement a transition of care program to improve the discharge process within a pediatric setting.
Background. This patient navigation program was created at a freestanding pediatric hospital licensed for 250 beds to address some of the barriers associated with providing successful discharge care. This program targeted clinically complex children, as defined by patients who 1) required 3 or more follow-up appointments after discharge, 2) were on complex medication regimens as determined by their provider, and/or 3) were clinically and/or psychosocially complex as determined by their provider. The inpatient medical or nursing team referred their patients who were eligible for the program. Nurse navigators then met caregivers at the bedside to help guide families through the discharge process, including arranging transportation, scheduling follow-up appointments, and connecting the families to social resources as needed. Through this program, the discharge process for these patients became more streamlined, which allowed patients to more successfully transition from inpatient to outpatient care.
However, despite evidence of the importance of pharmacists in identifying medication errors throughout the care continuum, pharmacist involvement in the patient navigation program was not standard of care. Providing focused medication-related education during the discharge process would require the addition of resources and expertise that was not currently available within the hospital's existing patient navigation team.
To address this gap, a partnership was established between the patient navigation program and the pharmacy department to add pharmacy services to the discharge program. As a result, this program had the goal of optimizing medication therapy to improve the clinical outcomes of clinically complex patients and improve the transition of care from the hospital to home.
Materials and Methods
The pilot program consisted of 2 months of developing the program structure (July through August 2016) and 5 months of active pharmacy discharge services (mid-September 2016 through early February 2017) (Figure 1). During the first 2 months, the collaboration between the patient navigation nurses and the pharmacy department was established and the workflow drafted. Under the collaboration, the nurse navigators continued to provide the traditionally offered services for patients consulted for patient navigation services, regardless of whether the patients were seen by pharmacists. In addition to the nursing services, the pharmacist provided medication reconciliation, provided bedside discharge counseling, and conducted follow-up telephone encounters on days 1, 7, and 14 post discharge (±1 day).
Figure 1.
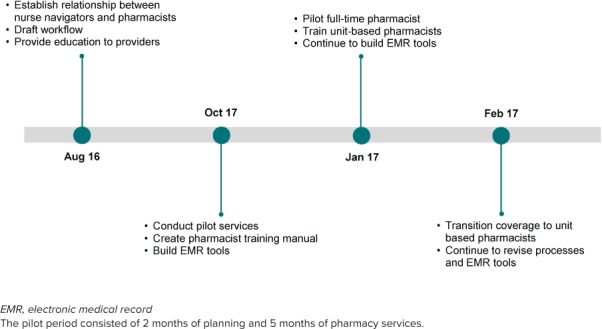
Timeline of the discharge program implementation process.
To prepare for the discharge counseling sessions, the discharge pharmacist would often communicate with the inpatient clinical pharmacist who was familiar with the patient in order to identify and resolve any medication issues as the patient transitioned from inpatient to outpatient care. During the bedside discharge counseling session, the pharmacist reviewed each medication in detail, including medication indication, dose, frequency, administration instructions, and potential side effects. To ensure consistency with discharge counseling, checklists were developed for each patient interaction. A customized, patient-friendly medication calendar was created by using the MedActionPlan program (MedActionPlan.com LLC, Peapack, NJ) and provided to each patient. Any medication-related problem identified by the pharmacist was resolved in a timely manner. Throughout the process, nurse navigators and pharmacists worked together to ensure a smooth discharge program for the patient. The nurse navigators helped pharmacists keep track of patients referred to the program. Following the pharmacy discharge counseling session, the pharmacists would send the patient's discharge medication list and pharmacist discharge summary to the nurse navigators. The nurse navigator would then compile these documents, along with the patient's follow-up schedule, to be sent to the identified primary care provider of the patient following discharge.
After establishing the workflow, pharmacist resources and technology tools were developed to facilitate the workflow processes. A pharmacist training manual was developed to serve as a reference guide for pharmacists involved in the initiative; the training manual included essential information ranging from detailed instructions for each step in the discharge process to sample speaking scripts that could be used during patient encounters. The training manual also included checklists to guide pharmacists through the preparation, execution, and follow-up process of each patient encounter (available from the corresponding author). The training manual also included information helpful for the nurse navigators, including a document that listed the workflow of the program and distinguished the responsibilities of nurse navigators from that of the pharmacists. An electronic tool was developed in the electronic medical record (EMR), EPIC (Epic Systems, Verona, WI), to facilitate the patient workup and post-patient encounter documentation. A patient list and transitions of care report were also developed within the EMR to capture all of the patients referred to the patient navigation service and to allow pharmacists to quickly view pertinent patient information, such as each patient's inpatient and outpatient medication lists, to facilitate prioritizing among patients.
From September through December 2017, the program was piloted with 3 pharmacists carrying out pharmacy discharge services. These pharmacists did not have dedicated time for the project, but rather carved out time from their existing daily responsibilities. When choosing among patients with whom to provide pharmacy services, the pharmacists prioritized patients who had a combination of the following: complex medication regimens, discharge medication regimens that were finalized by the medical team in a timely manner, and family who were available by the bedside during a time compatible with the pharmacists' schedules. During the fifth month of the pilot pharmacy services, there was a dedicated pharmacy resident to carry out the patient navigation discharge services on weekdays for at least 8 hours a day. During this month, the pharmacy resident attempted to provide pharmacy services to every patient who had a finalized discharge medication list and family who were available at the bedside during the dedicated pharmacy hours. If multiple patients were eligible for discharge counseling services at the same time, the pharmacy resident would prioritize the patients who had more complex medication regimens (as determined by the pharmacy resident and medical team).
During the month with dedicated pharmacy services, decentralized pharmacists were also trained on the process, so that coverage of these discharge services could eventually be transitioned to those pharmacists. An all-day training session was carried out by the pharmacists and nurses who developed the program. This session consisted of reviewing the training manual to teach the pharmacists a standardized approach to providing discharge counseling that included how to identify medication problems during transitions of care, how to explain the program to families, what information to provide to families, and where and how to document the provision of the education in the medical record. During this session, the pharmacists participated in computer tutorials of electronic tools used for the discharge program and conducted the discharge services under the supervision of the trainers. The training manual used to train the pharmacists was constantly updated as improvements were made to the program, and these pharmacists were consistently retrained on the updates.
Demographics of the patients referred to the patient navigation program, including sex, race, and age, were recorded. Patient characteristics, including number of documented comorbidities and hospital length of stay, were also recorded. Total discharge medications were also recorded for the patients who were provided pharmacy services through the discharge program. Chi-square and t tests were used to compare the demographics and characteristics of patient navigation patients who were assisted by pharmacists with patients who were not provided pharmacy services.
The primary outcome measure used to assess the success of the pilot program and identify areas for improvement was the quantity and type of documented pharmacist interventions identified during discharge counseling and telephone encounters. Resources required were measured by quantifying the time used by pharmacists to carry out the services offered by the discharge program. In addition, financial benefit gained from the program was estimated by translating each documented pharmacist intervention into potential cost savings. Potential cost savings, depending on the intervention category, were based on estimates established internally by the hospital using a standardized process. The amount of cost savings represented the savings from the perspective of the hospital and was informed by estimates published in the literature. Descriptive statistics were used to describe the outcome measures.
The institutional review board determined this to be a quality improvement project and therefore exempt from their review.
Results
During the 5 months of the pilot period, 311 unique patients received patient navigation referrals, totaling 321 total hospital encounters (Table 1). Discharge counseling and telephone encounter attempts were provided by a pharmacist for 55 unique patients, totaling 56 hospital encounters. The patients who received discharge counseling ranged from newborn to 17 years of age, and 50% of the patients were 1 year of age or younger. The patients who were provided discharge counseling had a median of 8 comorbidities, a median length of stay of 10 days, and were discharged on a median of 4 medications. Most of the patient demographics and characteristics between the patients who were assisted by pharmacists and patients who were not assisted by pharmacists were not significantly different between the 2 groups; however, the length of stay of patients who were seen by pharmacists at discharge was significantly greater (10 vs. 4 days, p = 0.02) (Table 1).
Table 1.
Demographics and Characteristics of Patient Navigation Program Patients
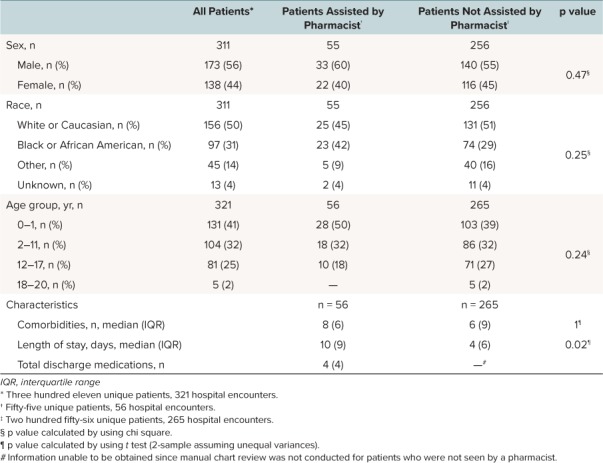
Pharmacists were able to provide discharge counseling services for 17% of the patient navigation consults. During the months without a dedicated pharmacist (September–December), a pharmacist was able to see 5% to 15% of the consults each month. During the period with a dedicated pharmacist (January through February 3), the percentage of patients who were seen by a pharmacist at discharge increased to 36% (Figure 2).
Figure 2.
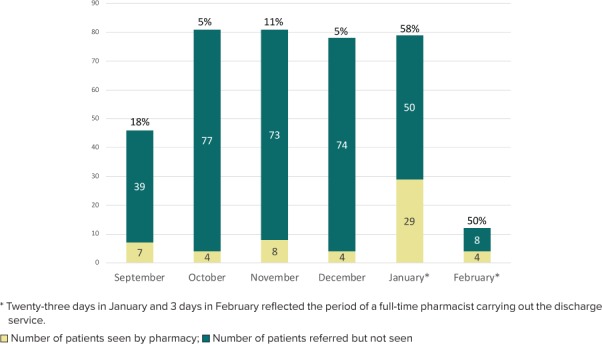
Percentage of referrals seen by a pharmacist at discharge.
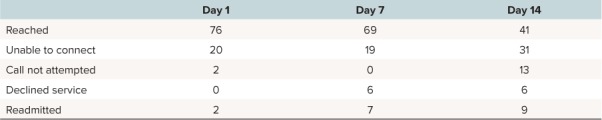
For telephone encounters, 76% of families were reached on day 1 post discharge, 69% on day 7 follow-up, and 41% on day 14 (Table 2). Inability to connect with patients and families via phone call was due to the pharmacist calling but unable to reach the family, the family declining follow-up phone call services, or the patient being readmitted before the scheduled date of the phone call. For day-14 phone calls, the pharmacist would often assess the utility of the phone call to decide whether to attempt the call or not. For example, some patients finished their new medications within 2 weeks following discharge, so no day-14 phone call attempt was made for those patients. These instances were categorized as “call not attempted,” along with cases in which a pharmacist was not available to call on the day (±1 day) of the scheduled phone call.
Table 2.
Percentage Reached for Telephone Encounters (n = 56)
A total of 168 pharmacist interventions were logged during the discharge counseling and telephone encounters (Table 3). The interventions were grouped into different categories and were further categorized as “accepted,” “informational” (interventions for which the pharmacist helped to optimize the medication regimen without resulting in a change in the prescription, such as clarifying confusing prescription information or identifying ways to optimize medication adherence), or “rejected.” The interventions were categorized by a member of the research team and independently checked by 2 other members of the team.
Table 3.
Pharmacy Interventions Identified During Discharge Counseling and Telephone Encounters
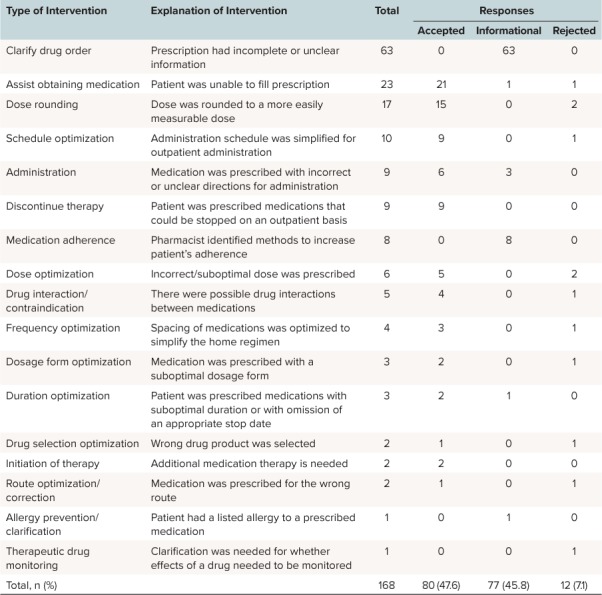
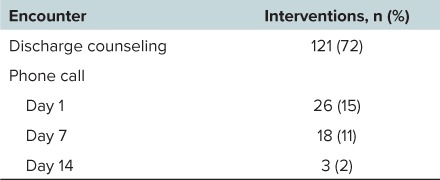
The most common interventions were “clarify drug order,” “assist obtaining medication,” “dose rounding,” and “schedule optimization.” The majority of the interventions were either accepted (47.6%) or informational in nature (45.8%). A small number of interventions (7.1%) were rejected. The rejected interventions were mostly minor in nature, with the intention of enhancing treatment efficacy rather than preventing medication error. When categorizing the number of interventions per patient encounter, most of the interventions (72%) were identified during the discharge counseling step of the patient navigation program (Table 4).
Table 4.
Pharmacist Interventions by Encounter (n = 168)
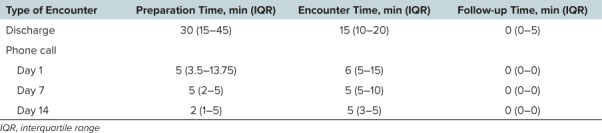
Estimated cost savings were assigned to each intervention category by using the hospital's internally validated system of assigning cost savings to pharmacist interventions (Table 5). The estimated cost savings of all accepted/informational interventions was $10,660. A general medication counseling cost savings ($208 of cost savings per discharge counseling session) resulted in an additional $11,648 of potential cost savings, for a total of $22,308 of potential cost savings over the 5-month pilot period. The pharmacists spent a median of 73 minutes per patient to prepare for and conduct each encounter and follow-up with any medication-related problems following the encounters (Table 6). The majority of time was spent on the discharge encounter, with a median of 30 minutes to prepare for the discharge counseling session and 15 minutes to conduct the discharge encounter.
Table 5.
Hospital's Internally Validated Estimated Cost Savings per Intervention Type
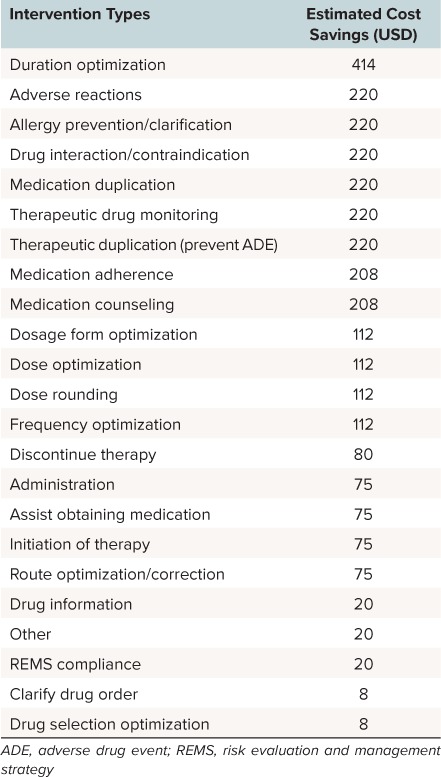
Table 6.
Time Spent by Pharmacists on Each Patient Encounter Type
Discussion
Medication-related problems were common throughout the pediatric discharge process, with a median of 3 interventions identified per consult. This finding is similar to other studies that report pharmacists identifying at least 1 medication discrepancy or error per patient.10,15–16 The most common interventions identified included “clarify drug order,” “assist obtaining medication,” “dose rounding,” and “schedule optimization.” Many of these interventions were not a result of prescribing error, but rather opportunities to simplify the home regimen as the patient transitioned to outpatient care. Most of the interventions were accepted or informational in nature.
The pharmacists spent a considerable amount of time on each patient, from the initial chart review to each of the patient encounters, throughout the discharge and postdischarge period. This is consistent with other studies that report the time-consuming process of quality transition of care.17
Most pharmacist interventions were identified while preparing and counseling the patient for discharge; fewer interventions were identified during the telephone encounters as more time passed since discharge. Overall, this pilot program not only resulted in benefits to the patients from receiving individualized pharmacy services in terms of changes to their prescriptions and clarification of their medications, but also resulted in significant cost savings.
Although the number of patients serviced by pharmacists through the patient navigation pilot program was an improvement from the minimal number of patients who received pharmacy discharge services before the implementation of the pilot program, there could be improvements in how many patients were seen by a pharmacist. One of the major challenges that limited the pharmacy department's ability to see more patients was the lack of dedicated pharmacist time for this project, as evident by the improvement in numbers of patients seen during the month with a dedicated pharmacist. The process, from preparing for the patient encounter to providing post-encounter documentation, was also extremely time intensive, which presented a barrier to providing multiple interventions in a short time. Discharges that occurred on a weekend or overnight were not eligible, as no pharmacists were available during these times to carry out discharge services. A possible time-saving measure is if the clinical pharmacist who was familiar with the patient during his or her inpatient stay was the same person providing counseling services at discharge. However, this model was not feasible with the current structure of the pharmacy department. Another contributing factor to the low number of patients seen was the small timeframe that the pharmacist had between the time that the discharge medications were finalized by the team and the time that the family was available to receive these discharge counseling services before discharge. In many instances, the medication list was finalized only minutes before the patient's discharge or the family was not available until directly before discharge. These challenges possibly skewed the patient population seen by the pharmacists, since the neonatal patients were more likely to have family members constantly available for discharge counseling as compared with some of the older patients. Furthermore, some patients were identified as eligible for patient navigation services owing to their need for multiple appointments following discharge, and not necessarily because they had complicated medication regimens. Some of these patients had no medications, which precluded them from requiring pharmacy services. This also contributed to the large number of neonatal patients who were referred to the program, as the majority of the patients discharged from the neonatal intensive care unit required multiple follow-up appointments following discharge. To help target more patients who are on complicated medication regimens in the future, the patient navigation referral form will be modified to allow providers to indicate the number of discharge medications for each patient referred for patient navigation services.
Another major challenge was resolving discrepancies between multiple forms of documentation (e.g., outpatient prescription, physician discharge summary, after visit summary) at a patient's discharge. Although many pharmacist recommendations were accepted verbally, at times there were difficulties in ensuring that prescriptions, discharge summaries, or after visit summaries were also updated correctly. Furthermore, it was often difficult for the pharmacist to identify where the responsibility of care of the patient lies after discharge (inpatient team vs. primary care provider), especially when a medication change was needed.
Many of the factors contributing to these challenges were unique to the discharge process of pediatric patients. As compared with the pharmacy discharge process of adult patients, the pediatric discharge process more frequently involves not only the patients, but also their parents or caregivers as well. This can make the process more time intensive, as the pharmacists and nurse navigators often spend a considerable amount of time to coordinate their bedside visits according to the availability of the parents or caregivers. For pediatric patients who were old enough to participate in managing their own medications, the pharmacists spent extra time to ensure that both the parents or caregivers and the pediatric patient achieved good understanding of the medication regimens. Furthermore, during the post-discharge telephone calls, the pharmacist often relied on the account of the parent or caregiver rather than speaking firsthand to the pediatric patient.
To address some of these challenges, the addition of more pharmacist time to carry out these discharge services is planned. Also, the EMR tool is constantly being updated to help make the patient workup and documentation process less time-consuming. Furthermore, to help the pharmacist communicate with the providers responsible for care of the patient following discharge, a process was put in place to allow pharmacists to include a note in the medical record following telephone encounters to be routed to the patient's primary care provider. Nurse navigators and pharmacists will continue to work together to efficiently schedule appointments with families before discharge. Challenges regarding discrepancies in documentation or identifying the provider who is responsible for the patient post discharge will continue to be addressed on a hospital-wide level. It is anticipated that these ongoing efforts will increase the number of patients seen by the program and continue to improve transitions of care for pediatric patients.
Following the pilot period, the unit-based pharmacists took the lead in providing discharge counseling to patients who were discharged from their respective units and were referred to the patient navigation program. To provide time for the unit-based pharmacists to prepare for and provide the discharge counseling, a second pharmacist covered the responsibilities of 1 or 2 unit-based pharmacists for a 2-hour block in the afternoon. Different unit-based pharmacists covered the discharge service on a rotating basis throughout the week. A tracking log was developed to allow monitoring of program success, and pharmacists were required to document daily how many patients were counseled and called. Also, a data dashboard was developed to track program data such as the number of interventions, associated cost savings, time needed for each encounter, and rate of acceptance of the service by families. From June 2017 to January 2018, the program provided discharge counseling for 37 complex patients with only 1 patient declining service. Patients were discharged on a total of 213 medications with pharmacists taking 2690 minutes to prepare and provide the discharge counseling. There were a total of 124 interventions on these patients for a total savings of $11,090.
In conclusion, implementation of the pilot patient navigation collaboration between nurse navigators and pharmacists resulted in improvements to the pediatric discharge process in terms of optimized medication therapy, improvements in patients' and caregivers' understanding of the medications, and potential cost savings. Coordinating the discharge of pediatric patients offers its own unique challenges, but this transition of care program has improved the process by intercepting and addressing potential, preventable adverse drug events. To ensure further success of the program during subsequent years, continued focus on process improvement is essential.
Acknowledgments
Presented at the Eastern States Residency Conference, Hershey, Pennsylvania, May 2017; Children's Hospital Association Quality and Safety Conference, Orlando, Florida, March 2017; and American Society of Health-System Pharmacists Midyear Clinical Meeting, Las Vegas, Nevada, December 2017.
ABBREVIATIONS
- ADE
adverse drug event
- EMR
electronic medical record
- REMS
risk evaluation and management strategy
Footnotes
Disclosures The authors received funding from the Cardinal Health E3 Grant Program. The authors declare no other conflicts or financial interest in any product or service mentioned in the manuscript, including equipment, medications, employment, gifts, and honoraria. The authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Copyright Published by the Pediatric Pharmacy Advocacy Group. All rights reserved. For permissions, email: matthew.helms@ppag.org
REFERENCES
- 1.Heath J., Dancel R., Stephens JR. Postdischarge phone calls after pediatric hospitalization: an observational study. Hosp Pediatr. 2015;5(5):241–248. doi: 10.1542/hpeds.2014-0069. [DOI] [PubMed] [Google Scholar]
- 2.Huynh C., Wong IC, Tomlin S. et al. Medication discrepancies at transitions in pediatrics: a review of literature. Paediatr Drugs. 2013;15(3):203–215. doi: 10.1007/s40272-013-0030-8. [DOI] [PubMed] [Google Scholar]
- 3.Balling L., Erstad BL, Weibel K. Impact of a transition-of-care pharmacist during hospital discharge. J Am Pharm Assoc. 2015;55(4):444–448. doi: 10.1331/JAPhA.2015.14087. [DOI] [PubMed] [Google Scholar]
- 4.Bishop MA, Cohen BA, Billings LK, Thomas EV. Reducing errors through discharge medication reconciliation by pharmacy services. Am J Health Syst Pharm. 2015;72(17 suppl 2):S120–S126. doi: 10.2146/sp150021. [DOI] [PubMed] [Google Scholar]
- 5.Anderegg SV, Wilkinson ST, Couldry RJ et al. Effects of a hospitalwide pharmacy practice model change on readmission and return to emergency department rates. Am J Health Syst Pharm. 2014;71(17):1469–1479. doi: 10.2146/ajhp130686. [DOI] [PubMed] [Google Scholar]
- 6.Caruso MC, Gittelman MA, Widecan ML, Luria JW. Pediatric emergency department discharge prescriptions requiring pharmacy clarification. Pediatr Emerg Care. 2015;31(6):403–408. doi: 10.1097/PEC.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 7.Gattari TB, Krieger LN, Hu HM, Mychaliska KP. Medication discrepancies at pediatric hospital discharge. Hosp Pediatr. 2015;5(8):439–445. doi: 10.1542/hpeds.2014-0085. [DOI] [PubMed] [Google Scholar]
- 8.Balaban RB, Galbraith AA, Burns ME et al. A patient navigator intervention to reduce hospital readmissions among high-risk safety-net patients: a randomized controlled trial. J Gen Intern Med. 2015;30(7):907–915. doi: 10.1007/s11606-015-3185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schell W. A review: discharge navigation and its effect on heart failure readmissions. Prof Case Manag. 2014;19(5):224–234. doi: 10.1097/NCM.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 10.Shiu JR, Fradette M., Padwal RS et al. Medication discrepancies associated with a medication reconciliation program and clinical outcomes after hospital discharge. Pharmacotherapy. 2016;36(4):415–421. doi: 10.1002/phar.1734. [DOI] [PubMed] [Google Scholar]
- 11.Bellone JM, Barner JC, Lopez DA. Postdischarge interventions by pharmacists and impact on hospital readmission rates. J Am Pharm Assoc. 2012;52(3):358–362. doi: 10.1331/JAPhA.2012.10172. [DOI] [PubMed] [Google Scholar]
- 12.Phatak A., Prusi R., Ward B. et al. Impact of pharmacist involvement in transitional care of high-risk patients through medication reconciliation, mediation education, and postdischarge call-backs (IPITCH Study) J Hosp Med. 2016;11(1):39–44. doi: 10.1002/jhm.2493. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez GM, Douglass MA, Mancuso MA. Revisiting Project Re-engineered Discharge (RED): the impact of a pharmacist telephone intervention on hospital readmission rates. Pharmacotherapy. 2015;35(9):805–812. doi: 10.1002/phar.1630. [DOI] [PubMed] [Google Scholar]
- 14.Ruppar TM, Cooper PS, Mehr DR et al. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. J Am Heart Assoc. 2016;5(6):e002606. doi: 10.1161/JAHA.115.002606. DOI: 10.1161/JAHA.115.002606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sebaaly J., Parsons LB, Pilch NA et al. Clinical and financial impact of pharmacist involvement in discharge medication reconciliation at an academic medical center: a prospective pilot study. Hosp Pharm. 2015;50(6):505–513. doi: 10.1310/hpj5006-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Surbhi S., Munshi KD, Bell PC, Bailey JE. Drug therapy problems and medication discrepancies during care transitions in super-utilizers. J Am Pharm Assoc. 2016;56(6):633–642. doi: 10.1016/j.japh.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 17.DaCosta AM, Sweet CB, Garavaglia LR et al. Pharmacist-led model to reduce hospital readmissions in medically complex children. J Pediatr Pharmacol Ther. 2016;21(4):346–352. doi: 10.5863/1551-6776-21.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]


