Abstract
Rationale: The “gut–lung axis” is commonly invoked to explain the microbiome’s influence on lung inflammation. Yet the lungs harbor their own microbiome, which is altered in respiratory disease. The relative influence of gut and lung bacteria on lung inflammation is unknown.
Objectives: To determine whether baseline lung immune tone reflects local (lung–lung) or remote (gut–lung) microbe–host interactions.
Methods: We compared lung, tongue, and cecal bacteria in 40 healthy, genetically identical, 10-week-old mice, using 16S ribosomal RNA gene quantification and sequencing. We measured inflammatory cytokines, using a multiplex assay of homogenized lung tissue. We compared lung bacteria in healthy mice treated with varied durations of systemic antibiotics.
Measurements and Main Results: Lung bacterial communities are highly variable among mice, cluster strongly by cage, shipment, and vendor, and are altered by antibiotics in a microbiologically predictable manner. Baseline lung concentrations of two key inflammatory cytokines (IL-1α and IL-4) are correlated with the diversity and community composition of lung bacterial communities. Lung concentrations of these inflammatory cytokines correlate more strongly with variation in lung bacterial communities than with that of the gut or mouth.
Conclusions: In the lungs of healthy mice, baseline innate immune tone more strongly reflects local (lung–lung) microbe–host interactions than remote (gut–lung) microbe–host interactions. Our results independently confirm the existence and immunologic significance of the murine lung microbiome, even in health. Variation in lung microbiota is likely an important, underappreciated source of experimental and clinical variability. The lung microbiome is an unexplored therapeutic target for the prevention and treatment of inflammatory lung disease.
Keywords: lung microbiome, 16S, innate immunity, host–microbiome interactions
At a Glance Commentary
Scientific Knowledge on the Subject
In both animal models and clinical studies, disruption of the microbiome influences lung immunity. This is generally ascribed to a purported “gut–lung axis.” Yet the lungs harbor their own microbiome, and the relative influence of lung and gut microbiota on lung immunity is unknown.
What This Study Adds to the Field
We here show that in the lungs of healthy mice, variation in baseline innate immune tone more strongly reflects variation in lung microbiota than that of gut bacteria. Lung bacterial communities in experimental mice have high animal-to-animal variation, cluster strongly by cage, shipment, and vendor, and are altered by antibiotics in a microbiologically predictable manner. Baseline lung concentrations of two key inflammatory cytokines (IL-1α and IL-4) are correlated with the diversity and community composition of lung bacterial communities. Our results independently confirm the existence and immunologic significance of the murine lung microbiome, even in health. Variation in lung microbiota is likely an important, underappreciated source of experimental and clinical variability.
A provocative connection has been uncovered between the microbiome and lung immunity. This relationship has proven robust across species, disease states, and techniques of study. For example, early childhood microbial exposure confers decreased asthma susceptibility (1), whereas early antibiotic exposure confers increased risk of developing asthma (2). Clinical trials of probiotics have suggested benefit in the prevention of cystic fibrosis exacerbations (3, 4) and ventilator-associated pneumonia (5). In animal models, the severity of allergic airway disease is influenced by antibiotic exposure (6, 7) and dietary manipulation (8), and microbiome suppression (via antibiotics or use of germ-free mice) influences susceptibility to models of influenza (9), bacterial pneumonia (10), acute lung injury (11), and chronic obstructive pulmonary disease (12). In most discussions and reviews, these findings are explained via the invocation of a “gut–lung axis,” that is, indirect effects of intestinal microbiota on systemic and alveolar immunity (10, 13, 14).
Yet the lungs, previously considered sterile in health, have been shown to harbor diverse and dynamic communities of bacteria (15, 16): the lung microbiome. In various disease states, variation in lung microbiota has been correlated with physiologic severity of disease (17, 18), intensity of alveolar inflammation (19, 20), rate of disease progression (21, 22) and exacerbation frequency (23), response to therapy (24, 25), and mortality (21). Even in healthy volunteers, baseline variation in lung microbiota is significantly correlated with the character and intensity of alveolar immunity (26). Thus both in health and disease, lung immunity reflects lung microbiota.
Thus a fundamental question is unanswered: does the baseline immune state of the lungs in health reflect remote (gut–lung) or local (lung–lung) host–microbe interactions (27)? To date, this question has been unanswerable in human studies, due both to the lack of paired gut and lung specimens from the same subjects as well as the confounding influences of host genetics and uncontrolled exposures. For this reason, we designed an experiment using inbred mice, identical in their genetics, sex, age, and exposure history. With these variables controlled, we could directly compare the microbiota of the gut and lung in their correlations with key features of lung immunity.
We here demonstrate that laboratory mice vary dramatically in their lung microbiota, which cluster by cage, shipment, and vendor. Lung microbiota exhibit more interanimal variability than do upper or lower gastrointestinal microbiota. We show that baseline differences in lung concentrations of key inflammatory cytokines correlate more strongly with lung bacteria than with gut bacteria. Our results provide independent confirmation of the reality and immunologic significance of the lung microbiome in health, and have important implications regarding interpretation of microbiome studies and the reproducibility of experimental models of inflammatory lung disease.
Methods
Ethics Statement
The animal studies described in this manuscript were approved by the Institutional Animal Care and Use Committee at the University of Michigan. Laboratory animal care policies at the University of Michigan follow the Public Health Service Policy on Humane Care and Use of Laboratory Animals.
Mice
Eight-week-old female C57BL/6 mice were purchased from Jackson Laboratories and Charles River Laboratories and housed under specific pathogen–free conditions. Mice were studied in sequential weeks over a 4-week period. Mice were housed in five-animal cages, and allowed to acclimate for 2 weeks before harvest at 10 weeks of age. Details regarding experimental exposures, tissue collection, and processing are reported in the online supplement.
16S Ribosomal RNA Gene Sequencing
DNA was extracted, amplified, and sequenced according to previously published protocols (28–30). Sequencing was performed with the MiSeq platform (Illumina). Details are provided in the online supplement.
Bacterial DNA Quantification
Bacterial DNA was quantified with a QX200 droplet digital PCR (ddPCR) system (Bio-Rad). Details are provided in the online supplement.
Cytokine Measurement
Cytokine concentrations were measured in homogenized lung tissue according to manufacturer instructions, using a Cytokine 20-Plex mouse panel (Thermo Fisher) on the LX-200 platform (Luminex).
Statistical Analysis
Sequence data were processed and analyzed with mothur version 1.35.1 software (31, 32) and the vegan package 2.2-1 and mvabund in R (33–35). Details regarding statistical and ecologic analysis are reported in the online supplement.
Results
To answer our research question, we studied 40 healthy, genetically identical mice obtained in four shipments from two vendors (Charles River Laboratories and Jackson Laboratory). We characterized the bacterial communities in the cecum, oropharynx, and lungs, and compared variation in microbiota with variation in lung concentration of key inflammatory cytokines. We quantified bacterial DNA burden by ddPCR of the 16S ribosomal RNA (rRNA) gene, and characterized microbiota by 16S rRNA gene sequencing. We obtained 3,573,615 total reads (18,612 ± 18,428 [mean ± SD] reads per specimen; range, 3,854–96,081). No operational taxonomic units (OTUs) were removed, and all specimens were included in the analysis.
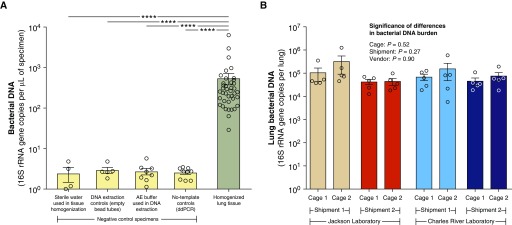
Bacterial DNA Is Detectable in the Lungs of Healthy Adult Mice
To measure the absolute abundance of bacterial DNA in murine lungs, we used ddPCR to quantify the 16S rRNA gene in homogenized lung tissue. ddPCR is an ultrasensitive PCR platform that performs absolute quantification with superior resolution at low biomass concentrations (e.g., lung specimens) compared with conventional quantitative PCR (36). We compared the bacterial DNA composition of homogenized lung tissue with negative control specimens representing potential sources of DNA contamination: sterile water used in lung homogenization, DNA extraction controls (empty bead tubes processed in parallel with tissue specimens), AE buffer used in DNA extraction, and no-template controls for the ddPCR. We detected significantly more bacterial DNA in homogenized mouse lung tissue than in all negative control specimens (Figure 1A) (P = 9.2 × 10−12, collectively; P ≤ 0.0001 for all specific control types). The smallest amount of bacterial DNA detected in lung homogenate was greater than the greatest amount detected among negative control specimens. Per unit of volume, homogenized lung tissue contained, on average, more than 200 times the bacterial DNA content of negative control specimens. On average, mouse lungs contained 1.1 × 105 ± 2.1 × 105 copies of the bacterial 16S rRNA gene per lung (Figure 1B). Although we found considerable variation across mice (95% confidence interval, 4.0 × 104–1.7 × 105 copies/lung), we found no significant difference in lung bacterial DNA burden across vendors, shipments, or cages (P > 0.05 for all). We thus concluded that bacterial DNA is detectable in the lungs of healthy adult mice and does not systematically vary by vendor, shipment, or cage.
Figure 1.
Bacterial DNA is detectable in the lungs of healthy mice. Bacterial DNA was quantified by droplet digital PCR of the 16S ribosomal RNA gene. (A) Homogenized lung tissue contained more bacterial DNA than did all negative control specimens (****P < 0.0001 for all comparisons). The lowest-abundance lung specimen had more bacterial DNA than the highest-abundance negative control specimen. (B) We found a 200-fold variation in lung bacterial DNA burden across individual mice, but no difference across vendors, shipments, or cages (P > 0.05 for all). Significance was determined by (A and B) Mann-Whitney test and by (B) Kruskal-Wallis test. Data presented are means and SEMs. ddPCR = droplet digital PCR; rRNA = ribosomal RNA.
Lung Microbiota Show Minimal Evidence of Procedural and Sequencing Contamination
In low-biomass microbiome studies, it is essential to determine the influence of contamination on sequencing results, as reagents used in DNA isolation and library preparation contain bacterial DNA that can contaminate sequencing-based studies of microbial communities (37). To identify potential sources of contamination in sequencing, we collected multiple (25) procedural control specimens, including sterile water used in tissue collection (exposed to instruments used in harvesting and tissue homogenization), DNA extraction controls (empty bead tubes processed in parallel with tissue specimens), AE buffer used in DNA extraction, and blank wells in the MiSeq sequencing run. As shown in Figure E1 in the online supplement, we found minimal evidence of procedural and sequencing contamination influencing the taxa detected in lung, tongue, and cecum specimens. Bacterial taxa detected in lung, tongue, and cecum specimens were all collectively distinct from those detected in procedural and sequencing control specimens (P ≤ 0.0001 for all comparisons; permutational multivariate ANOVA [PERMANOVA]). The five most abundant OTUs detected in lung specimens, comprising 29.8% of all sequences detected in lung specimens, comprised only 0.3% of all sequences detected in procedural and sequencing control specimens (Figure E1A). The most abundant OTU detected in procedural and sequencing control specimens (OTU00001; Bacillus) comprised only 2.9% of all sequences detected in lung specimens (Figure E1B). By contrast, we found a significant influence of procedural and sequencing contamination on nasal rinse specimens, which we excluded from further analysis. Lung communities were distinct from those detected in oral specimens (P = 0.0006; PERMANOVA) and cecal specimens (P < 0.0001; PERMANOVA). We concluded that the detection of bacteria in lung, tongue, and cecum specimens was not significantly influenced by procedural and sequencing contamination.
Lung Bacterial Communities Are Highly Variable among Experimental Mice
As it has previously been demonstrated that gut microbiota are highly variable among experimental mice (38, 39), we sought to determine the variability in lung microbiota between experimental mice. As shown in Figure 2, we found marked variation in the bacterial taxa detected in the lungs of mice. There was no “core microbiome,” common to the lungs of all mice. No single OTU was detected in the majority of all mice. In many instances, the lung communities of two experimental mice contained zero common OTUs.
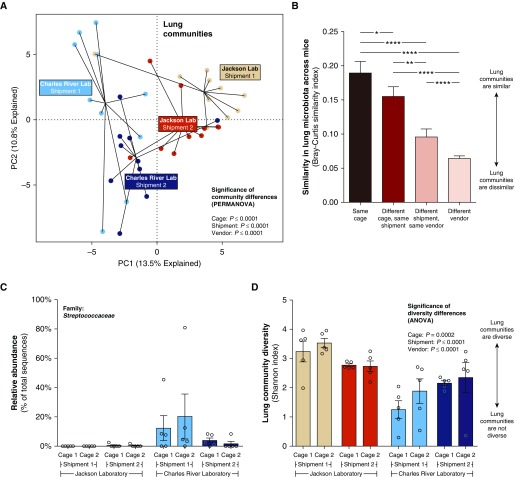
Figure 2.
Murine lung bacteria are highly variable and cluster by cage, shipment, and vendor. (A) Bacterial communities detected in the lungs of healthy, genetically identical mice cluster by cage, shipment, and vendor. (B) Lung bacteria communities were most similar among cohoused mice, and most dissimilar when mice from different vendors were compared. (C) As an example, members of the Streptococcaceae family were almost absent from Jackson Laboratory mice (2 of 20 mice, 0.2% of all sequences) but were common and abundant in mice from Charles River Laboratories (12 of 20 mice, 9.5% of all sequences). (D) Lung community diversity differed by cage, shipment, and vendor. Significance was determined by (A) permutational multivariate ANOVA and by (B and D) ANOVA with Holm-Sidak multiple comparisons test. *P ≤ 0.05; **P ≤ 0.01; ****P < 0.0001. Data presented in B–D are means and SEMs. PC1 and PC2 = principal components 1 and 2; PERMANOVA = permutational multivariate ANOVA.
Lung Bacterial Communities Cluster by Cage, Shipment, and Vendor
We then sought to determine whether this variation in lung microbiota reflected each mouse’s environment. As shown in Figure 2A, lung communities clustered significantly by cage, shipment, and vendor (P ≤ 0.0001 for all comparisons; PERMANOVA). The similarity of lung microbiota across mice (as measured by the Bray-Curtis similarity index) was greatest when comparing mice sharing a single cage, and was increasingly distinct when compared across cages (P ≤ 0.05), shipments (P ≤ 0.0001), and vendors (P ≤ 0.0001) (Figure 2B). To provide a clinically and immunologically relevant example, we show in Figure 2C differences in relative abundance of the Streptococcaceae family in lung specimens across cages, shipments, and vendors. Members of the Streptococcaceae family were barely detected in the lungs of mice obtained from Jackson Laboratory (2 of 20 mice, 0.2% of all sequences) but were common and abundant in the lungs of mice from Charles River Laboratories (12 of 20 mice, 9.5% of all sequences). The diversity of lung bacterial communities, as measured by the Shannon diversity index, was also highly variable across cages (P = 0.0002), shipments (P ≤ 0.0001), and vendors (P ≤ 0.0001) (Figure 2D). Lung bacterial diversity (Shannon diversity index) was not correlated with lung bacterial burden (16S rRNA gene copies) (P = 0.63; R2 = 0.006), indicating that variation in lung diversity was not an artifact of differences in bacterial burden. Figure E2 shows that clustering of mice from the same vendor was found for oral and cecal bacterial communities, with less intercage variation among mice from the same shipment than was observed for lung microbiota (P > 0.05). Of note, for gut and oral bacterial communities, intragroup similarities for mice from the same vendor and shipment were higher than were seen for lung bacterial communities.
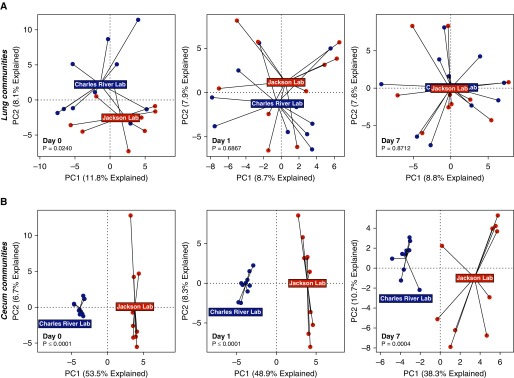
Lung Microbial Communities of Healthy Mice Converge with Increased Duration of Cohousing
Having determined that the lung communities of healthy mice cluster by their environment, we then asked how rapidly lung communities change after changes in environment. To determine the temporal dynamics of lung microbiota, we performed an experiment testing various durations of cohousing. We obtained healthy, genetically identical mice from two different vendors and placed them in shared cages. We characterized the bacterial communities of the lungs, tongue, and cecum at various durations of cohousing (Day 0, Day 1, and Day 7).
As shown in Figure 3, the lung communities of cohoused mice rapidly converge. The lung communities of mice acquired from different vendors, although distinct on Day 0, converged by Day 1 and were indistinguishable by Day 7 (Figure 3A). In dramatic contrast, the cecal communities of cohoused mice remained significantly distinct by vendor even after 7 days (Figure 3B). Oral communities, like lung communities, were distinct on Day 0 (P = 0.0002) but converged by Day 1 (P = 0.7271). We thus concluded that lung microbiota, like oral bacteria, are more dynamic and rapidly susceptible to environmental influence than are lower gastrointestinal bacteria.
Figure 3.
Murine lung bacteria converge with increased duration of cohousing. Genetically identical mice from two vendors were housed together and harvested at various durations of cohousing. (A) Lung communities converged within 1 day of cohousing and were indistinguishable after 1 week. (B) By contrast, cecal communities remained distinct by vendor even after 1 week of cohousing. Significance was determined by permutational multivariate ANOVA. PC1 and PC2 = principal components 1 and 2.
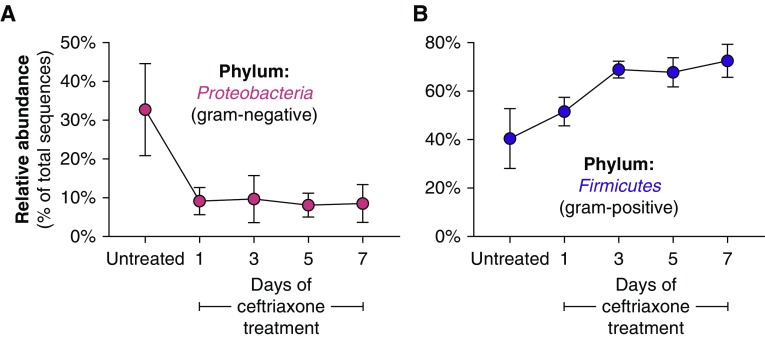
Lung Microbiota of Healthy Mice Are Altered by Antibiotics in a Microbiologically Predictable Manner
Having demonstrated that murine lung bacteria are variable and cluster by environment, and given the well-demonstrated observation that antibiotic exposure influences susceptibility to inflammatory lung disease (2, 6, 7, 9–12), we then asked whether lung microbiota are altered by antibiotic exposure. We treated healthy adult mice with systemic ceftriaxone, a third-generation cephalosporin antibiotic selected because of its common clinical use, its favorable lung penetration, and its well-defined antimicrobial spectrum of coverage (selective activity against gram-negative bacteria). We exposed healthy, cohoused, adult C57BL/6 mice to various durations of systemic (intraperitoneal) ceftriaxone (50 mg/kg/d) and assessed taxonomic changes in lung bacterial communities. We focused on the relative abundance of Proteobacteria and Firmicutes, respectively, the most abundant phyla of gram-negative and gram-positive bacteria commonly detected in lung communities. As predicted, the lung communities of ceftriaxone-treated mice had lower relative abundance of the Proteobacteria (gram-negative) phylum (P = 0.002) (Figure 4A). In contrast, ceftriaxone-treated mice had higher relative abundance of the Firmicutes (gram-positive) phylum (P = 0.009) (Figure 4B). We thus concluded that even in health, the lung microbiome can be altered by antibiotics in a microbiologically predictable manner.
Figure 4.
The lung microbiome of healthy mice is altered by systemic antibiotics in a microbiologically predictable manner. Healthy, cohoused, 10-week-old mice were administered various durations of systemic (intraperitoneal) ceftriaxone, a third-generation cephalosporin with antimicrobial activity against gram-negative bacteria. After treatment, (A) the relative abundance of Proteobacteria (the most abundant phylum of gram-negative lung bacteria) was rapidly and persistently suppressed; (B) in contrast, the relative abundance of Firmicutes (the most abundant phylum of gram-positive lung bacteria) was increased. Data presented are means and SEMs.
Lungs of Healthy Mice Vary in Concentrations of Key Cytokines Involved in the Innate and Adaptive Immune Response
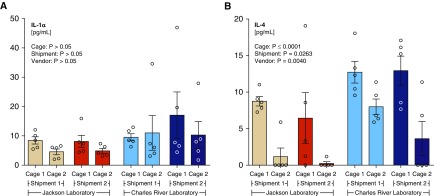
We then asked whether the baseline immune tone of lungs is also variable across healthy mice. To broadly characterize lung immune status, we used a multiplex cytokine assay with the Luminex LX-200 platform. Concentrations of lung cytokines are shown in Table E1. As expected in uninjured, uninfected mice, concentrations of many acute inflammatory cytokines (e.g., TNF (tumor necrosis factor)-α, IFN-γ, and IL-10) were largely below the limit of detection of the assay. However, two cytokines (IL-1α and IL-4) were notable in their mouse-to-mouse variability and their broad detectability. We chose to focus our analysis on these two key cytokines that serve as important indices of the innate (IL-1α) and adaptive (IL-4) immune response of the lungs (40–43).
As shown in Figure 5, we observed wide variability in basal concentrations of both cytokines in the lungs of healthy mice. Although we found a greater than 20-fold difference in lung concentrations of IL-1α among individual mice, we detected no significant correlation between environment and IL-1α concentrations, as analyzed by cage, shipment, or vendor (P > 0.05 for all comparisons) (Figure 5A). By contrast, we found a significant relationship between lung IL-4 concentrations and cage (P ≤ 0.0001), shipment (P = 0.0263), and vendor (P = 0.0040) (Figure 5B). As a specific example, two cages of mice obtained from Jackson Laboratory had undetectable IL-4 concentrations in the lungs of four of five mice, whereas two cages obtained from Charles River Laboratories had IL-4 detected in all mice with mean concentrations greater than 10 pg/ml.
Figure 5.
Variation in inflammatory cytokines in the lungs of healthy mice. Concentrations of inflammatory cytokines were measured in homogenized lung tissue collected from genetically identical 10-week-old mice. Twenty-fold differences in both cytokines were detected between mice. (A) Lung concentrations of IL-1α did not significantly differ by cage, shipment, or vendor, whereas (B) lung concentrations of IL-4 differed by cage, shipment, and vendor. Significance was determined by ANOVA with the Holm-Sidak multiple comparisons test (shipment and cage) and Student’s t test (vendor). Concentrations of IL-1α were log-normalized before comparison. Data presented are means and SEMs.
Lung Concentrations of Inflammatory Cytokines Correlate with Differences in Lung Microbiota
We then asked whether this variation in lung immunity reflects variation in lung, gut, and oral microbiota. We compared the burden, diversity, and community composition of bacterial communities with lung concentrations of IL-1α and IL-4.
We first compared the burden of lung communities with indices of lung immunity. We found no relationship between lung bacterial burden (16S rRNA gene copies) and lung concentrations of IL-1α (P = 0.832; R2 = 0.001) and IL-4 (P = 0.717; R2 = 0.004). This indicates that variation in these key inflammatory cytokines is not attributable to differences in total lung bacterial burden.
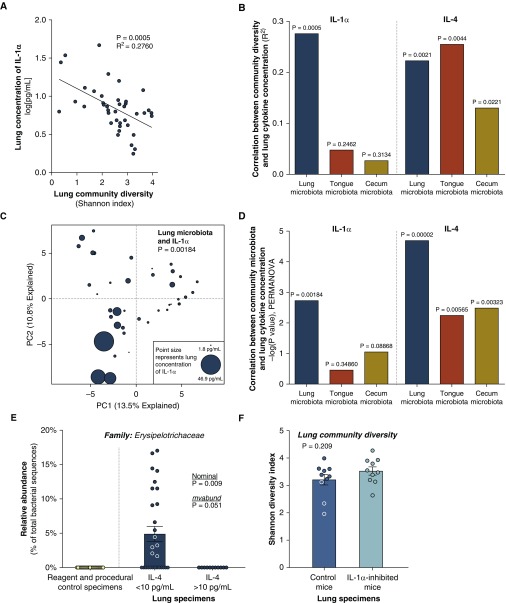
We then compared diversity of lung, oral, and gut communities with indices of lung immunity. As shown in Figure 6A, we observed a significant negative correlation between lung community diversity (as measured by the Shannon diversity index) and lung concentrations of IL-1α (P = 0.0005; R2 = 0.2760). Diversity of lung bacteria was significantly and negatively correlated with lung concentrations of IL-4 (P = 0.0021; R2 = 0.2228). Lung concentrations of IL-4 were also significantly correlated with diversity of oral (P = 0.0044) and cecal (P = 0.0221) bacterial communities (Figure 6B). Yet notably, we found no correlation between the diversity of oral and cecal microbiota and lung concentrations of IL-1α (P > 0.05 for both) (Figure 6B). Thus baseline lung concentrations of IL-1α are exclusively correlated with the diversity of lung microbiota, and are unrelated to the diversity of gut and oral bacteria.
Figure 6.
Lung microbial communities are correlated with lung immunity in healthy mice. Lung bacterial communities and concentrations of inflammatory cytokines were compared in genetically identical 10-week-old mice. (A) Lung concentrations of IL-1α were significantly and negatively associated with the community diversity of lung bacteria. Of the variation in lung IL-1α concentrations, 27.6% was explained by lung bacterial diversity. (B) Lung concentrations of IL-1α were not correlated with the diversity of tongue or cecal microbiota. Lung concentrations of IL-4 were significantly and negatively correlated with community diversity of lung, tongue, and cecal bacteria. (C) The community composition of lung microbiota was significantly associated with lung concentrations of IL-1α: specimens with similar microbiota had similar concentrations of IL-1α. (D) Although lung IL-1α concentrations were significantly correlated with lung microbiota, they had no detectable relationship with tongue or cecal microbiota. Lung IL-4 concentrations were most strongly correlated with lung communities. (E) The anaerobic Erysipelotrichaceae family was not detected in negative control specimens and was enriched in the lungs of mice with low concentrations of IL-4. (F) Inhibition of IL-1α via systemic antibodies to the IL-1 receptor had no effect on lung community diversity or community composition. Significance was determined by (A and B) linear regression, (C and D) permutational multivariate ANOVA, (E and F) t test, and (E) mvabund. Data presented in E and F are means and SEMs. PC1 and PC2 = principal components 1 and 2; PERMANOVA = permutational multivariate ANOVA.
We then compared community composition of lung, oral, and gut communities with indices of lung immunity. As shown in Figure 6C, we found a significant relationship between lung community composition and lung concentrations of IL-1α (P = 0.00184; PERMANOVA). No relationship was found between the community composition of oral and gut bacteria and lung concentrations of IL-1α (Figure 6D). By contrast, lung concentrations of IL-4 were significantly correlated with the community composition of bacteria in the lungs (P = 0.00002), tongue (P = 0.00565), and cecum (P = 0.00323) (Figure 6D).
To determine whether specific community members were associated with lung concentrations of either cytokine, we used the mvabund function in R, which performs analysis of multivariate abundance data against measured gradients (such as cytokine concentrations) and conservatively controls for multiple comparisons. As shown in Table E2, no specific taxa were individually responsible for the correlation between community composition and elevated concentrations of IL-1α. Among candidate taxa, the Erysipelotrichaceae family was most closely associated with lung IL-4 concentrations. This family of anaerobic and microaerophilic bacteria was the third most abundant family in lung specimens, detected in 16 of 40 mice, comprising 8.9% of all lung bacterial sequences when present (Figure 6E). By linear regression, variation in relative abundance of Erysipelotrichaceae explained more than one-quarter of the variation in lung IL-4 concentrations (nominal P = 0.0004; R2 = 0.288). Concentrations of IL-4 in the lung were less strongly associated with relative abundance of Erysipelotrichaceae in oral communities (nominal P = 0.0294; R2 = 0.119) and were unrelated to relative abundance of Erysipelotrichaceae in cecal communities (nominal P = 0.69; R2 = 0.004). The Erysipelotrichaceae family was comparably abundant in tongue communities (detected in 17 of 40 mice, comprising 8.7% of bacterial sequences when present) and uncommon in cecal communities (detected in 11 of 40 mice, comprising 1.7% of bacterial sequences when present).
We thus concluded that our key index of the lung’s innate immune response, IL-1α, reflects the diversity and community composition of lung bacteria, not oral bacteria or cecal bacteria. Another key cytokine involved in the lung’s adaptive immune response, IL-4, reflects the diversity and community composition of bacterial communities throughout the aerodigestive tract (lung, mouth, and cecum). Additional comparisons of detectable lung cytokines (IL-2, VEGF [vascular endothelial cell growth factor], and MIG [monokine induced by IFN-γ]) and features of lung, oral, and cecal communities are reported in Table E3.
Lung Microbiota of Healthy Mice Are Not Influenced by Inhibition of IL-1α Activity
The strong correlations identified between lung microbiota and lung concentrations of IL-1α could reflect multiple causal relationships: IL-1α could influence lung microbiota; lung microbiota could influence IL-1α concentrations; or both could be effects of a third, unmeasured cause. To determine whether IL-1α influences lung microbiota, we asked whether inhibition of IL-1α activity influences lung microbiota. We did this by administering a neutralizing antibody against the IL-1 receptor, which nonspecifically blocks the activity of both IL-1α and IL-1β. We compared the lungs of IL-1–inhibited mice with those of genetically identical, cohoused mice administered IgG isotype control.
The lung communities of healthy mice were not detectably altered by 1 week of IL-1 inhibition. IL-1 inhibition did not significantly change the diversity of lung bacteria, measured either via the Shannon diversity index (Figure 6F; P = 0.209) or by community richness (unique OTUs per 10,000 sequences; P = 0.1027). The community composition of lung bacteria was not distinct among IL-1–inhibited mice (P = 0.2757; PERMANOVA). IL-1 inhibition did have a significant effect on oral communities (P = 0.017; PERMANOVA) but not on cecal communities (P = 0.7282; PERMANOVA). The diversity of oral and cecal communities, measured both by Shannon diversity index and unique OTUs per 10,000 sequences, was unchanged by IL-1 inhibition.
We thus concluded that the strong correlation between IL-1α and lung microbiota is not explained by the effect of IL-1α on lung bacteria. This suggests that the identified correlation between lung microbiota and lung IL-1α may be attributable to the local effects of lung microbiota on host immunity rather than the inverse (the effects of lung immunity on lung microbiota).
Discussion
The core finding of our study is that the lung microbiota of healthy mice are highly variable, cluster strongly by environment, are altered by antibiotics, and correlate with concentrations of key inflammatory cytokines in the lung. Concentrations of the inflammatory cytokines IL-1α and IL-4 in the lung more strongly reflect local (lung–lung) interactions than they do remote (gut–lung) interactions. The correlation between the lung microbiome and host response is incompletely explained by the host’s influence on lung microbiota. Our results underscore the reality and immunologic significance of the lung microbiome in health, and have important implications both for the interpretation of human studies and for the experimental study of inflammatory lung diseases.
The “gut–lung axis” is commonly invoked (10, 13, 14) to explain the well-demonstrated association between perturbation of the microbiome and alterations in lung immunity and susceptibility to inflammatory lung disease (1–6, 8–12). Yet before the current study, no direct comparison has been made between gut and lung microbiota regarding their relative influence on baseline lung innate immunity. In our controlled study, we found that key indices of baseline lung immunity more closely reflect lung microbiota than they do lower gut microbiota, demonstrating that local (lung–lung) interactions between the host and microbiome are as important as remote (gut–lung) interactions in health. This observation has implications for the interpretation of human microbiome studies, which commonly sample only stool (and not lung specimens), presumably due to the relative convenience of specimen collection. As microbiome interventions (such as systemic antibiotics) impact both gut and lung microbiota (44–46), it will be crucial for subsequent studies of the role of the microbiome in respiratory disease to consider both gut and lung microbiota (27).
Our findings have important experimental implications beyond the field of lung microbiome studies, and may identify a partial explanation behind the so-called “reproducibility crisis” (38, 39, 47). Inbred mice are widely used for experimental research because they permit the controlling of confounding variables: genetics, sex, age, exposure history, and so on. Yet it has been thoroughly established that between-mouse differences in gut microbiota convey profound differences in host immunity (e.g., the presence of segmented filamentous bacterium inducing the development of IL-17–producing CD4+ T helper cells [48]). Our findings extend this observation to lung microbiota, and indicate that the lung microbiome may represent an important unmeasured confounder in experimental models of lung immunity. Although this source of experimental variation may be controlled via use of germ-free and gnotobiotic mice, this solution is expensive and impractical for routine use. Rather, we recommend that key findings in experimental models be validated using mice acquired from various environmental sources (vendors, shipments, and breeding facilities) to ensure their robustness across a variety of microbial contexts. By interrogating the relationship between lung microbiota and lung immunity in health and disease models, we hope the field will identify novel targets for biologic and therapeutic study at the host–microbe interface.
Given the ubiquitous use of mice in the study of inflammatory lung disease, it is crucial to determine the immunologic and biologic significance of variation in murine lung bacteria. One research group reported their difficulty in detecting lung bacteria in one-third of the healthy adult mice studied (49). Despite technical limitations to their approach (e.g., omitting quantification of total bacterial DNA burden, studying a single shipment of mice, using small sections of excised lung tissue rather than whole lungs, not using the touchdown PCR protocol preferred for low-biomass amplification [50]), the authors interpreted this lack of signal as evidence of lung sterility. Our results demonstrate the danger of such premature generalization. We show here that lung bacteria, when studied optimally, are indeed detectable in healthy mice, are altered by housing conditions and antibiotics, and are correlated with key features of lung immunity. In fact, multiple research groups have detected lung bacteria in mice, and the murine lung microbiome has been correlated with age (51), sex (52), environment (51), inflammation (12, 52), and lung injury (53). Taken together with the existing literature, our results underscore the reality and immunologic significance of a distinct lung microbiome, even in healthy mice.
We identified a strong association between concentrations of a key index of innate immunity, IL-1α, and baseline difference in lung bacteria. IL-1α is constitutively expressed by lung epithelial cells as well as alveolar macrophages, and is considered a “frontline” cytokine in the lungs’ defense against bacterial pathogens (40, 43). Its production is stimulated by microbial exposure (40) and mediates neutrophil recruitment and activation of the innate immune response (43). IL-1α is released into the extracellular space by stressed and necrotic cells, and is immediately biologically active without need for subsequent cleavage (42). It thus functions as a damage-associated molecular pattern, provoking a local cascade of inflammatory mediators (54). It is thus immunologically plausible that variation in IL-1α would reflect differences in local microbial exposure, as demonstrated by our culture-independent approach. Our results demonstrate that the lungs’ innate immune apparatus is not only relevant in the context of acute infection, but rather is continuously calibrated to the identity and diversity of lung microbiota. IL-4 is a critical cytokine in the adaptive immune response. In contrast to IL-1α, variation in lung concentrations of IL-4 was correlated not merely with lung communities but also with microbiota of the tongue and cecum. Further study will be needed to elucidate the relative contribution of gut and lung bacteria to the lungs’ adaptive immune response.
The ecologic and microbiologic features of the lung microbiome that are most strongly correlated with baseline concentrations of inflammatory cytokines merit further consideration and study. Baseline lung IL-1α concentrations were strongly correlated with the diversity of lung bacteria, with the latter explaining 28% of variation in the former. We have previously demonstrated that in the human lung microbiome, low community diversity is associated with clinical, immunologic, and ecologic features of pneumonia: positive culture growth, high alveolar neutrophilia and catecholamine concentration, high relative abundance of a dominant taxonomic group, and high bacterial DNA burden (55, 56). Yet the mice in the current study were nonmorbid and exhibited no clinical evidence of pneumonia. Our findings demonstrate that the relationship between lung microbiome diversity and lung inflammation exists even in health, and is not reserved for conditions of acute infection. In fact, we found no correlation between total bacterial DNA burden (measured by the highly sensitive ddPCR platform) and indices of lung immunity, suggesting that in the lungs of healthy mice, relative abundance (who is present) matters more than absolute abundance (how much is present). Given our current understanding of the ecology of the respiratory tract, we suspect that interactions at the host–microbiome interface are dynamic, bidirectional, and continuous (15, 16). We also found a dramatic relationship between baseline lung concentrations of IL-4 and the relative abundance of the Erysipelotrichaceae family: these bacteria comprised 5% of lung bacteria in mice with low lung concentrations of IL-4, but were undetected in mice with elevated lung IL-4. This bacterial family, composed of anaerobic and microaerophilic organisms, would not be detected by conventional aerobic culture techniques. Provocatively, the Erysipelotrichaceae family has been shown to be markedly enriched in the fecal microbiome of mice treated with a low-fiber diet, which is associated with increased severity of allergic airway disease (8). Within the gut microbiome, the presence of specific bacteria has been shown to stimulate host immune maturation, for example, induction of T-helper cell type 17 cells by segmented filamentous bacteria (48). Our findings provide direction for further interrogation of the host–microbiome interface: does the presence of Erysipelotrichaceae mute IL-4 production, or are conditions of elevated IL-4 inhospitable to the growth of Erysipelotrichaceae? The lack of a detectable effect of IL-1 inhibition on lung bacterial communities suggests that the causal relationship behind these host–microbiome correlations is at least in part driven by the effect of the microbiome on the host. Considerable cell-to-cell and organism-to-organism variability exists even among genetically identical organisms; beyond microbial variation, some of this variation is likely attributable to nonmicrobial factors such as epigenetics, nongenetic inheritance, and subtle microenvironmental differences in cell stimuli (57).
Our findings revealed fundamental differences in the ecology of the lungs and gastrointestinal tract. Although lung communities clustered significantly by environment, within-cage and within-shipment similarity of lung microbiota across mice was modest compared with the tight clustering observed in oral and cecal communities. This relative difference in β diversity (high in lung communities, moderate in tongue communities, and low in cecal communities) reflects fundamental differences in the ecology of these anatomic sites. The lungs are topographically outside of the body, and are continuously exposed to potential sources of microbial immigration (inhalation, aspiration, and mucosal dispersion [15]). In human studies, lung microbiota exhibit minimal evidence of site-specific selective pressure (58), indicating that the lung microbiome is instead determined by the dynamic balance of microbial immigration and elimination (the “adapted island model of lung biogeography” [15, 59, 60]). By contrast, the cecum is an ecologically “protected” site with numerous barriers to microbial immigration: in order for bacteria to invade and occupy an animal’s cecum, they must survive both the low pH of the stomach and the high pH of the duodenum before outcompeting the high-biomass communities of the lower gastrointestinal tract. This ecologic interpretation is supported by the differences in stability of lung and cecal communities over time when animals are cohoused (Figure 3): lung communities are dynamic and rapidly converge in cohoused mice, whereas cecal communities remain distinct and resistant to change even after 1 week of cohousing. Our findings, taken together with parallel observations in a human study by Segal and colleagues (26), confirm that although transient and dynamic, lung microbiota are not invisible to the host, and are reflected in variation in baseline host immune tone.
In summary, these data demonstrate that the lung microbiota of healthy mice are highly variable, cluster strongly by environment, and correlate with concentrations of key inflammatory cytokines in the lung. In healthy mice, the immune tone of the lungs reflects local (lung–lung) microbe–host interactions more strongly than it does remote (gut–lung) microbe–host interactions. Our findings suggest that variation in lung microbiota is an important, underappreciated source of experimental and clinical variability in health and inflammatory lung disease.
Acknowledgments
Acknowledgment
The authors thank the University of Michigan Multidisciplinary Intensive Care Research Workgroup for helpful discussions, Peter Sun for bioinformatic assistance, and our anonymous reviewers for constructive critiques and suggestions.
Footnotes
Supported by the NIH (UL1TR000433 [R.P.D.], K23HL130641 [R.P.D.], and R01HL121774 [G.B.H.]). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Also supported by the Michigan Institute for Clinical and Health Research (R.P.D.), the Host Microbiome Initiative of the University of Michigan (R.P.D.), and the University of Michigan Center for Integrative Research in Critical Care (R.P.D.).
Availability of sequencing data: Sequences are available via the National Center for Biotechnology Information Sequence Read Archive (accession number PRJNA388464). Operational taxonomic unit, taxonomy, and metadata tables are available for download at https://github.com/dicksonlunglab/mouse_lung_microbiome_variability.
Author Contributions: Conception and design: R.P.D. and N.R.F. Acquisition of data: R.P.D., N.R.F., and E.M.H. Analysis and interpretation of data: R.P.D., J.R.E.-D., S.L.A., and G.B.H. Drafting or revising of manuscript: R.P.D., J.R.E.-D., N.R.F., E.M.H., S.L.A., and G.B.H. Final approval of manuscript: R.P.D., J.R.E.-D., N.R.F., E.M.H., S.L.A., and G.B.H.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.201711-2180OC on March 13, 2018
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Ege MJ, Mayer M, Normand AC, Genuneit J, Cookson WO, Braun-Fahrländer C, et al. GABRIELA Transregio 22 Study Group. Exposure to environmental microorganisms and childhood asthma. N Engl J Med. 2011;364:701–709. doi: 10.1056/NEJMoa1007302. [DOI] [PubMed] [Google Scholar]
- 2.Hoskin-Parr L, Teyhan A, Blocker A, Henderson AJ. Antibiotic exposure in the first two years of life and development of asthma and other allergic diseases by 7.5 yr: a dose-dependent relationship. Pediatr Allergy Immunol. 2013;24:762–771. doi: 10.1111/pai.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss B, Bujanover Y, Yahav Y, Vilozni D, Fireman E, Efrati O. Probiotic supplementation affects pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Pediatr Pulmonol. 2010;45:536–540. doi: 10.1002/ppul.21138. [DOI] [PubMed] [Google Scholar]
- 4.Bruzzese E, Raia V, Spagnuolo MI, Volpicelli M, De Marco G, Maiuri L, et al. Effect of Lactobacillus GG supplementation on pulmonary exacerbations in patients with cystic fibrosis: a pilot study. Clin Nutr. 2007;26:322–328. doi: 10.1016/j.clnu.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Morrow LE, Kollef MH, Casale TB. Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial. Am J Respir Crit Care Med. 2010;182:1058–1064. doi: 10.1164/rccm.200912-1853OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noverr MC, Falkowski NR, McDonald RA, McKenzie AN, Huffnagle GB. Development of allergic airway disease in mice following antibiotic therapy and fungal microbiota increase: role of host genetics, antigen, and interleukin-13. Infect Immun. 2005;73:30–38. doi: 10.1128/IAI.73.1.30-38.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Noverr MC, Noggle RM, Toews GB, Huffnagle GB. Role of antibiotics and fungal microbiota in driving pulmonary allergic responses. Infect Immun. 2004;72:4996–5003. doi: 10.1128/IAI.72.9.4996-5003.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trompette A, Gollwitzer ES, Yadava K, Sichelstiel AK, Sprenger N, Ngom-Bru C, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med. 2014;20:159–166. doi: 10.1038/nm.3444. [DOI] [PubMed] [Google Scholar]
- 9.Ichinohe T, Pang IK, Kumamoto Y, Peaper DR, Ho JH, Murray TS, et al. Microbiota regulates immune defense against respiratory tract influenza A virus infection. Proc Natl Acad Sci USA. 2011;108:5354–5359. doi: 10.1073/pnas.1019378108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schuijt TJ, Lankelma JM, Scicluna BP, de Sousa e Melo F, Roelofs JJ, de Boer JD, et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut. 2016;65:575–583. doi: 10.1136/gutjnl-2015-309728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Souza DG, Vieira AT, Soares AC, Pinho V, Nicoli JR, Vieira LQ, et al. The essential role of the intestinal microbiota in facilitating acute inflammatory responses. J Immunol. 2004;173:4137–4146. doi: 10.4049/jimmunol.173.6.4137. [DOI] [PubMed] [Google Scholar]
- 12.Yadava K, Pattaroni C, Sichelstiel AK, Trompette A, Gollwitzer ES, Salami O, et al. Microbiota promotes chronic pulmonary inflammation by enhancing IL-17A and autoantibodies. Am J Respir Crit Care Med. 2016;193:975–987. doi: 10.1164/rccm.201504-0779OC. [DOI] [PubMed] [Google Scholar]
- 13.Budden KF, Gellatly SL, Wood DL, Cooper MA, Morrison M, Hugenholtz P, et al. Emerging pathogenic links between microbiota and the gut–lung axis. Nat Rev Microbiol. 2017;15:55–63. doi: 10.1038/nrmicro.2016.142. [DOI] [PubMed] [Google Scholar]
- 14.Marsland BJ, Trompette A, Gollwitzer ES. The gut–lung axis in respiratory disease. Ann Am Thorac Soc. 2015;12:S150–S156. doi: 10.1513/AnnalsATS.201503-133AW. [DOI] [PubMed] [Google Scholar]
- 15.Dickson RP, Erb-Downward JR, Freeman CM, McCloskey L, Falkowski NR, Huffnagle GB, et al. Bacterial topography of the healthy human lower respiratory tract. MBio. 2017;8:e02287-16. doi: 10.1128/mBio.02287-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dickson RP, Erb-Downward JR, Martinez FJ, Huffnagle GB. The microbiome and the respiratory tract. Annu Rev Physiol. 2016;78:481–504. doi: 10.1146/annurev-physiol-021115-105238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia-Nuñez M, Millares L, Pomares X, Ferrari R, Pérez-Brocal V, Gallego M, et al. Severity-related changes of bronchial microbiome in chronic obstructive pulmonary disease. J Clin Microbiol. 2014;52:4217–4223. doi: 10.1128/JCM.01967-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cox MJ, Allgaier M, Taylor B, Baek MS, Huang YJ, Daly RA, et al. Airway microbiota and pathogen abundance in age-stratified cystic fibrosis patients. PLoS One. 2010;5:e11044. doi: 10.1371/journal.pone.0011044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dickson RP, Singer BH, Newstead MW, Falkowski NR, Erb-Downward JR, Standiford TJ, et al. Enrichment of the lung microbiome with gut bacteria in sepsis and the acute respiratory distress syndrome. Nat Microbiol. 2016;1:16113. doi: 10.1038/nmicrobiol.2016.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iwai S, Huang D, Fong S, Jarlsberg LG, Worodria W, Yoo S, et al. The lung microbiome of Ugandan HIV-infected pneumonia patients is compositionally and functionally distinct from that of San Franciscan patients. PLoS One. 2014;9:e95726. doi: 10.1371/journal.pone.0095726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molyneaux PL, Cox MJ, Willis-Owen SA, Mallia P, Russell KE, Russell AM, et al. The role of bacteria in the pathogenesis and progression of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2014;190:906–913. doi: 10.1164/rccm.201403-0541OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han MK, Zhou Y, Murray S, Tayob N, Noth I, Lama VN, et al. COMET Investigators. Lung microbiome and disease progression in idiopathic pulmonary fibrosis: an analysis of the COMET study. Lancet Respir Med. 2014;2:548–556. doi: 10.1016/S2213-2600(14)70069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rogers GB, Zain NM, Bruce KD, Burr LD, Chen AC, Rivett DW, et al. A novel microbiota stratification system predicts future exacerbations in bronchiectasis. Ann Am Thorac Soc. 2014;11:496–503. doi: 10.1513/AnnalsATS.201310-335OC. [DOI] [PubMed] [Google Scholar]
- 24.Huang YJ, Nelson CE, Brodie EL, Desantis TZ, Baek MS, Liu J, et al. National Heart, Lung, and Blood Institute’s Asthma Clinical Research Network. Airway microbiota and bronchial hyperresponsiveness in patients with suboptimally controlled asthma. J Allergy Clin Immunol. 2011;127:372–381.e1–3. doi: 10.1016/j.jaci.2010.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goleva E, Jackson LP, Harris JK, Robertson CE, Sutherland ER, Hall CF, et al. The effects of airway microbiome on corticosteroid responsiveness in asthma. Am J Respir Crit Care Med. 2013;188:1193–1201. doi: 10.1164/rccm.201304-0775OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Segal LN, Clemente JC, Tsay JC, Koralov SB, Keller BC, Wu BG, et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat Microbiol. 2016;1:16031. doi: 10.1038/nmicrobiol.2016.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dickson RP, Cox MJ. Gut microbiota and protection from pneumococcal pneumonia. Gut. 2017;66:384. doi: 10.1136/gutjnl-2016-311823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mason KL, Erb Downward JR, Mason KD, Falkowski NR, Eaton KA, Kao JY, et al. Candida albicans and bacterial microbiota interactions in the cecum during recolonization following broad-spectrum antibiotic therapy. Infect Immun. 2012;80:3371–3380. doi: 10.1128/IAI.00449-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caporaso JG, Lauber CL, Walters WA, Berg-Lyons D, Lozupone CA, Turnbaugh PJ, et al. Global patterns of 16S rRNA diversity at a depth of millions of sequences per sample. Proc Natl Acad Sci USA. 2011;108:4516–4522. doi: 10.1073/pnas.1000080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kozich JJ, Westcott SL, Baxter NT, Highlander SK, Schloss PD. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl Environ Microbiol. 2013;79:5112–5120. doi: 10.1128/AEM.01043-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schloss PD.MiSeq SOP: mothur 2015. [accessed 2017 Mar 1]. Available from: http://www.mothur.org/wiki/MiSeq_SOP
- 32.Schloss PD, Westcott SL, Ryabin T, Hall JR, Hartmann M, Hollister EB, et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol. 2009;75:7537–7541. doi: 10.1128/AEM.01541-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oksanen JF, Blanchet G, Kindt R, Legendre P, Minchin PR, O’Hara RB, et al. Vegan: community ecology package. R package version 2.0-4. 2012.
- 34.R Core Team. Vienna, Austria: R Foundation for Statistical Computing; 2013. R: a language and environment for statistical computing. [Google Scholar]
- 35.Wang Y, Naumann U, Wright ST, Warton DI. mvabund: an R package for model-based analysis of multivariate abundance data. Methods Ecol Evol. 2012;3:471–474. [Google Scholar]
- 36.Sze MA, Abbasi M, Hogg JC, Sin DD. A comparison between Droplet Digital and quantitative PCR in the analysis of bacterial 16S load in lung tissue samples from control and COPD GOLD 2. PLoS One. 2014;9:e110351. doi: 10.1371/journal.pone.0110351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Salter SJ, Cox MJ, Turek EM, Calus ST, Cookson WO, Moffatt MF, et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 2014;12:87. doi: 10.1186/s12915-014-0087-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Servick K. Mouse microbes may make scientific studies harder to replicate. Science. 2016;353:741–743. doi: 10.1126/science.353.6301.741. [DOI] [PubMed] [Google Scholar]
- 39.Reardon S. A mouse’s house may ruin studies: environmental factors lie behind many irreproducible rodent experiments. Nature. 2016;530:264. doi: 10.1038/nature.2016.19335. [DOI] [PubMed] [Google Scholar]
- 40.Arbour NC, Lorenz E, Schutte BC, Zabner J, Kline JN, Jones M, et al. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat Genet. 2000;25:187–191. doi: 10.1038/76048. [DOI] [PubMed] [Google Scholar]
- 41.Kopf M, Le Gros G, Bachmann M, Lamers MC, Bluethmann H, Köhler G. Disruption of the murine IL-4 gene blocks Th2 cytokine responses. Nature. 1993;362:245–248. doi: 10.1038/362245a0. [DOI] [PubMed] [Google Scholar]
- 42.Borthwick LA. The IL-1 cytokine family and its role in inflammation and fibrosis in the lung. Semin Immunopathol. 2016;38:517–534. doi: 10.1007/s00281-016-0559-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barry KC, Fontana MF, Portman JL, Dugan AS, Vance RE. IL-1α signaling initiates the inflammatory response to virulent Legionella pneumophila in vivo. J Immunol. 2013;190:6329–6339. doi: 10.4049/jimmunol.1300100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rogers GB, Bruce KD, Martin ML, Burr LD, Serisier DJ. The effect of long-term macrolide treatment on respiratory microbiota composition in non–cystic fibrosis bronchiectasis: an analysis from the randomised, double-blind, placebo-controlled BLESS trial. Lancet Respir Med. 2014;2:988–996. doi: 10.1016/S2213-2600(14)70213-9. [DOI] [PubMed] [Google Scholar]
- 45.Slater M, Rivett DW, Williams L, Martin M, Harrison T, Sayers I, et al. The impact of azithromycin therapy on the airway microbiota in asthma. Thorax. 2014;69:673–674. doi: 10.1136/thoraxjnl-2013-204517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Segal LN, Clemente JC, Wu BG, Wikoff WR, Gao Z, Li Y, et al. Randomised, double-blind, placebo-controlled trial with azithromycin selects for anti-inflammatory microbial metabolites in the emphysematous lung. Thorax. 2017;72:13–22. doi: 10.1136/thoraxjnl-2016-208599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Laman JD, Kooistra SM, Clausen BE. Reproducibility issues: avoiding pitfalls in animal inflammation models. Methods Mol Biol. 2017;1559:1–17. doi: 10.1007/978-1-4939-6786-5_1. [DOI] [PubMed] [Google Scholar]
- 48.Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–498. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Scheiermann J, Klinman DM. Three distinct pneumotypes characterize the microbiome of the lung in BALB/cJ mice. PLoS One. 2017;12:e0180561. doi: 10.1371/journal.pone.0180561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Korbie DJ, Mattick JS. Touchdown PCR for increased specificity and sensitivity in PCR amplification. Nat Protoc. 2008;3:1452–1456. doi: 10.1038/nprot.2008.133. [DOI] [PubMed] [Google Scholar]
- 51.Kostric M, Milger K, Krauss-Etschmann S, Engel M, Vestergaard G, Schloter M, et al. Development of a stable lung microbiome in healthy neonatal mice. Microb Ecol. 2018;75:529–542. doi: 10.1007/s00248-017-1068-x. [DOI] [PubMed] [Google Scholar]
- 52.Barfod KK, Vrankx K, Mirsepasi-Lauridsen HC, Hansen JS, Hougaard KS, Larsen ST, et al. The murine lung microbiome changes during lung inflammation and intranasal vancomycin treatment. Open Microbiol J. 2015;9:167–179. doi: 10.2174/1874285801509010167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Poroyko V, Meng F, Meliton A, Afonyushkin T, Ulanov A, Semenyuk E, et al. Alterations of lung microbiota in a mouse model of LPS-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2015;309:L76–L83. doi: 10.1152/ajplung.00061.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen CJ, Kono H, Golenbock D, Reed G, Akira S, Rock KL. Identification of a key pathway required for the sterile inflammatory response triggered by dying cells. Nat Med. 2007;13:851–856. doi: 10.1038/nm1603. [DOI] [PubMed] [Google Scholar]
- 55.Dickson RP, Erb-Downward JR, Prescott HC, Martinez FJ, Curtis JL, Lama VN, et al. Analysis of culture-dependent versus culture-independent techniques for identification of bacteria in clinically obtained bronchoalveolar lavage fluid. J Clin Microbiol. 2014;52:3605–3613. doi: 10.1128/JCM.01028-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dickson RP, Erb-Downward JR, Prescott HC, Martinez FJ, Curtis JL, Lama VN, et al. Intraalveolar catecholamines and the human lung microbiome. Am J Respir Crit Care Med. 2015;192:257–259. doi: 10.1164/rccm.201502-0326LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Snijder B, Pelkmans L. Origins of regulated cell-to-cell variability. Nat Rev Mol Cell Biol. 2011;12:119–125. doi: 10.1038/nrm3044. [DOI] [PubMed] [Google Scholar]
- 58.Venkataraman A, Bassis CM, Beck JM, Young VB, Curtis JL, Huffnagle GB, et al. Application of a neutral community model to assess structuring of the human lung microbiome. MBio. 2015;6:e02284-14. doi: 10.1128/mBio.02284-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dickson RP, Erb-Downward JR, Huffnagle GB. Towards an ecology of the lung: new conceptual models of pulmonary microbiology and pneumonia pathogenesis. Lancet Respir Med. 2014;2:238–246. doi: 10.1016/S2213-2600(14)70028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dickson RP, Erb-Downward JR, Freeman CM, McCloskey L, Beck JM, Huffnagle GB, et al. Spatial variation in the healthy human lung microbiome and the adapted island model of lung biogeography. Ann Am Thorac Soc. 2015;12:821–830. doi: 10.1513/AnnalsATS.201501-029OC. [DOI] [PMC free article] [PubMed] [Google Scholar]