Abstract
Objective:
Radiation-protective aprons are commonly used by interventionists to protect against the harmful effects of ionizing radiation. Choice of appropriate aprons with respect to lead equivalence and weight is necessary for effective protection and reduced physical strain. This study evaluates the knowledge and practice of using radiation-protective aprons by interventionists.
Materials and Methods:
Ninety-one interventional radiologists who attended an annual interventional conference were provided with a questionnaire which included age, years of experience, area of expertise, type and weight of apron used, and physical strain caused due to the use of apron.
Results:
About 14.3% of the interventionists practiced in an angiographic suite for less than an hour a day, 45% for 2–4 h, 21% for 4–6 h, 10% for 6–10 h, and the rest above 10 h/day. About 68% of the interventionists wore 0.5 mm lead-equivalent (Pbeq) aprons; 15.4% with 0.25 mm Pbeq; about 5.5% with 0.35 mm Pbeq aprons, and the remaining were not aware of the lead equivalence. About 47% reported that they had body aches due to wearing single-sided aprons. Interventionists working more than 10 h/day wearing single-sided lead apron predominantly complained of shoulder pain and back pain.
Conclusion:
A large fraction of interventionists reported that they had physical strain. It is suggestive for interventionists to wear correct fit and light-weight aprons with appropriate lead equivalence.
KEYWORDS: Lead apron, lead equivalence, physical strain, radiation safety

INTRODUCTION
Protective lead aprons play an important role in radiation protection of personnel working in fluoroscopy and angiographic suites. The basic necessity of the lead-equivalent (Pbeq) apron is to provide shielding from secondary radiation. These aprons are designed to shield approximately 75% of radiosensitive organs[1] in our body. The protective Pbeq apparels should have protective equivalent of not <0.25 mm Pbeq for X-rays up to 100 kV and not <0.35 mm lead for X-rays over 100 kV.[2] A minimum Pbeq of 0.5 mm is recommended for radiation personnel; for women interventionists, customized aprons that reach below mid-thigh level and wrap completely around the pelvis are beneficial in order to eliminate accidental exposure to conceptus.[3,4]
Conventionally, lead aprons consist of lead-impregnated rubber or vinyl material with maximum Pbeq of 1 mm which were heavy and uncomfortable for the wearer, particularly when worn for long periods. However, recent developments in manufacturing protective aprons emphasize more on the material used in order to reduce physical stress on the wearer. It has been reported that the use of lead apron is linked to the development of back pain.[5] This has led to the introduction of lead-free aprons consisting of materials of lower atomic weight such as antimony, tin, and barium. This study evaluates the knowledge and practice of using lead aprons by interventional radiologists (IRs) through a simple survey.
MATERIALS AND METHODS
Ninety one IRs who were registered in the 19th Annual Conference of the Indian Society for Vascular and Interventional Radiology (ISVIR) were provided with a simple questionnaire to evaluate the use of lead aprons in the catheterization lab. Table 1 shows the questionnaire used in the study which was framed by a team of interventionists and medical physicists. Figure 1 illustrates the different models of aprons available commercially.
Table 1.
Questionnaire for evaluating use of radiation-protective aprons by interventional radiologists
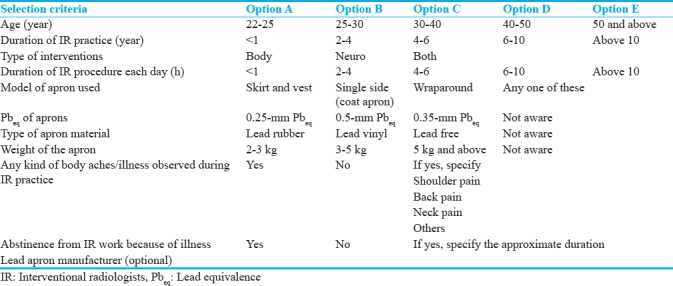
Figure 1.
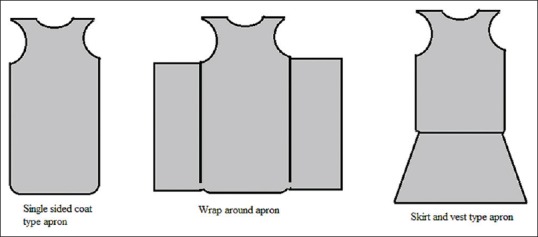
Different models of radiation protective aprons available commercially.
RESULTS
Out of the 91 IRs involved in interventional radiological procedures, 44% were between the age group of 30 and 40 years and 29% were between 40 and 50 years. Nearly 31% of the interventionists had a work experience of 2–4 years and 24% between 6 and 10 years. Almost 52% of IRs involved both body and neuro-interventions, 43% in body interventions, and the remaining were involved only in neuro-interventions. In the context of duration of IR practice, about 14% practiced for less than an hour per day, 43% for 2–4 h, 20% for 4–6 h, 10% for 6–10 h, and 8% above 10 h per day as illustrated in Figure 2. Regarding the type of aprons used, about 29% used skirt and vest, 31% wore single-sided apron, 23% wrap around, and the remaining wore any of the available aprons in the interventional suite. Most of the interventionists wore aprons with lead equivalence of 0.5 mm (68%); about 15.4% wore aprons with Pbeq of 0.25 mm; about 5.5% wore aprons with Pbeq of 0.35 mm, and the remaining were not aware of the lead equivalence. About 50% responded that they did not know the manufacturer of the apron.
Figure 2.
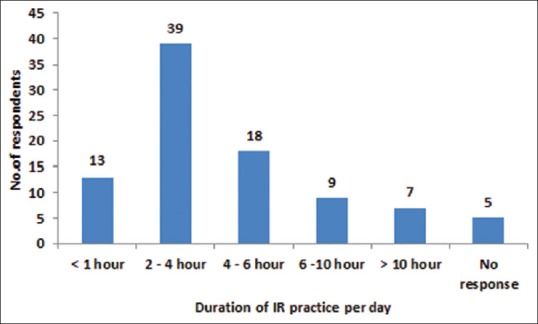
Illustration of the duration of interventional radiology practice by interventionists.
In order to reduce the physical stress caused by wearing lead aprons, different types of apron materials are available. About 29% responded that they were not aware of the type of apron they were wearing, 25% responded that they were using lead rubber aprons, 25% were using lead vinyl, and the remaining were using lead-free aprons. Apart from the type of aprons, the knowledge on the weight of the aprons was also assessed. About 48% responded that they were wearing aprons weighing 3–5 kg; about 22% wore aprons weighing about 2–3 kg, 11% above 5 kg, and the remaining were not aware of the weight of the aprons. About 47% reported that they had some kind of body aches due to wearing single-sided aprons, while the rest did not report any body pain. Most of the interventionists who wore lead-free aprons did not complain of any physical strain.
DISCUSSION
Radiation safety has been of grave importance currently as the number of minimally invasive procedures performed in catheterization labs have been increasing. Occupational workers performing lengthy interventions have been reported with cataract as well as loss of hair in the legs.[6,7] The United Nations Scientific Committee on the Effects of Atomic Radiation reports that interventional procedures are the main source of causing radiation burden among the occupational workers.[8] The major contributor to radiation dose to patients is from primary beam, while the major source for occupational workers is from the scatter radiation. Concerning IR, contribution of scatter radiation to the operator from body interventions is higher than the neuro-interventions as it involves a larger field of view and high exposure factors. Among the basic elements of radiation safety – time, distance, and shielding – the two major elements to be practiced by operators are minimize time and maximize shielding, while distance may not be applicable in this context as the interventionists have to perform procedures close to the patient and near the X-ray source. In the context of time duration, 8% of the interventionists practiced for over 10 h/day. These operators were in the age group of 30–40 years with <5 years of interventional experience. They predominantly complained of shoulder pain and back pain wearing the lead aprons (single-sided coat type) for longer duration of time. Out of the 91 interventionists who responded to the questionnaire, only 3 abstained from work due to illness.
When a procedure involves increased time duration, use of appropriate shielding accessories is important. Several models of lead aprons are available which help in even distribution of weight on the wearer, for example, physical strain is reduced with the help of wraparound apron though the weight of this apron is heavier than single-sided apron as the weight is evenly distributed on the body. About 17% of the interventionists wore either skirt and vest or single-sided or wraparound apron and about 11% did not know the Pbeq of the apron being used. Apart from this, 29% responded that they were not aware of whether they were using lead or lead-free aprons. In this context, knowledge about the intrinsic details and structural integrity of aprons worn by operators is essential. The integrity of the apron based on lead equivalence and weight and percentage attenuation can be assessed using simple step wedge for lead and lead-free aprons from different manufacturers.[9] Use of aprons with 0.5 mm Pbeq is suggestive for the interventionist staying close to the X-ray tube as the tube potentials would reach above 100 kVp during imaging a thick part of the body, especially during thorax and abdominal interventions.[10]
In order to reduce the physical burden on the body, it is also important to reduce the weight of the aprons. Studies have shown that in a survey conducted, nearly half of the 424 respondents reported of spine problems of which more than one-third missed work.[11] In our study, 11% responded that they wore aprons heavier than 5 kg and 22% responded that the aprons were between 2 and 3 kg. In recent years, lead-free aprons with antimony, bismuth, and barium sulfate are available commercially. The weight of these aprons generally ranges between 2 and 4.5 kg depending on their length and width. Some lead-free apron manufactures incorporate a bi-layer combination based on k-edges of low- and high atomic weight-material which could provide protection of 20% more effective than lead.[12] In order to reduce the physical burden, it is suggestive to wear 0.25mm Pbeq wraparound aprons which would provide 0.5 mm Pbeq in the front when wrapped around. In our study, only one interventionist recommended the use of skirt and vest. Nearly 49% (45 interventionists) responded that they did not have any body aches or illness, while the remaining 43 interventionists responded that they had body pain, with a majority involving back pain followed by shoulder pain and neck-and-leg pain. These could be attributed to the time duration, years of experience, and age of the interventionist.
Protective lead-equivalent apron with thyroid collar is a standard for radiation protection in cath labs. In addition to protective lead apparels, safety accessories such as lead goggles, ceiling mounted movable lead barriers, lead drapes mounted on patient table, and lead cap are used by interventionists to minimize radiation dose accumulated over a time period. The summation of scatter and leakage radiation from X-ray tube can greatly influence operators' exposure and result in deterministic effects. Use of protective lead drapes has found to significantly reduce the radiation dose to the lower extremities of interventionists. The average radiation dose from both lower extremities demonstrated a 64% decrease in radiation dose, with left extremity receiving higher radiation dose compared to right extremity.[13] However, while adopting extremely steeper tube angulations, such protective drapes may cause hindrance during the work.[14] Ceiling mounted lead glass shields are extremely found vital in minimizing the scatter radiation exposure to eye, face, and hands of the interventionists. In the absence of lead goggles worn by interventionists, lead glass shields can effectively minimize scatter reaching the eye of the interventionists. Operators receive high exposure on the left side of their head and have the possibility of increasing their risk when unprotected. Lead caps of 0.5-mm Pb were effective in lowering the radiation dose levels to 1.8 nSv/Gycm2 and in combination with lead glass shields resulted in an attenuation of 0.5 nSv/Gycm2.[15]
CONCLUSION
The study assessed the knowledge and practice of interventionists using radiation-protective lead aprons in IR with the help of a simple questionnaire. Majority of the IR responded that they had more physical strain due to the use of single-sided lead rubber aprons. Use of aprons with bi-layer combination of low- and high atomic weight-material is considered to provide effective protection and reduce physical strain.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/34/239707
REFERENCES
- 1.Hubbert TE, Vucich JJ, Armstrong MR. Lightweight aprons for protection against scattered radiation during fluoroscopy. AJR Am J Roentgenol. 1993;161:1079–81. doi: 10.2214/ajr.161.5.8273614. [DOI] [PubMed] [Google Scholar]
- 2.York: IPEM; 2002. Institute of Physics and Engineering in Medicine. Medical and Dental Guidance Notes: A Good Practice Guide on all Aspects of Ionising Radiation Protection in the Clinical Environment; pp. 60–1. [Google Scholar]
- 3.Wagner LK, Hayman LA. Pregnancy and women radiologists. Radiology. 1982;145:559–62. doi: 10.1148/radiology.145.2.7134471. [DOI] [PubMed] [Google Scholar]
- 4.Shymko MJ. Minimizing occupational exposure. Radiol Technol. 1998;70:89–90. [PubMed] [Google Scholar]
- 5.Moore JD, Shim D, Sweet J, Arheart KL, Beekman RH., 3rd Radiation exposure to children during coil occlusion of the patent ductus arteriosus. Catheter Cardiovasc Interv. 1999;47:449–54. doi: 10.1002/(SICI)1522-726X(199908)47:4<449::AID-CCD13>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 6.Wiper A, Katira R, Roberts DH. Images in cardiology. Interventional cardiology: It's a hairy business. Heart. 2005;91:1432. doi: 10.1136/hrt.2005.064899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vano E, Kleiman NJ, Duran A, Romano-Miller M, Rehani MM. Radiation-associated lens opacities in catheterization personnel: Results of a survey and direct assessments. J Vasc Interv Radiol. 2013;24:197–204. doi: 10.1016/j.jvir.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 8.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) Report to the General Assembly (II) 2000:2–17. [Google Scholar]
- 9.Livingstone RS, Varghese A. Simple quality control tool for assessing integrity of lead equivalent aprons. Indian J Radiol Imaging. 2018;28:258–62. doi: 10.4103/ijri.IJRI_374_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christodoulou EG, Goodsitt MM, Larson SC, Darner KL, Satti J, Chan HP. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med Phys. 2003;30:1033–8. doi: 10.1118/1.1573207. [DOI] [PubMed] [Google Scholar]
- 11.Goldstein JA, Balter S, Cowley M, Hodgson J, Klein LW Interventional Committee of the Society of Cardiovascular Interventions. Occupational hazards of interventional cardiologists: Prevalence of orthopedic health problems in contemporary practice. Catheter Cardiovasc Interv. 2004;63:407–11. doi: 10.1002/ccd.20201. [DOI] [PubMed] [Google Scholar]
- 12.Kiarmor Bi-layer Protection Against Scatter Radiation. [Last accessed on 2018 Jan 19]. https://www.infabcorp.com/wp-content/uploads/2012/02/kiarmor-brochure-130731.pdf .
- 13.Shortt CP, Al-Hashimi H, Malone L, Lee MJ. Staff radiation doses to the lower extremities in interventional radiology. Cardiovasc Intervent Radiol. 2007;30:1206–9. doi: 10.1007/s00270-007-9071-0. [DOI] [PubMed] [Google Scholar]
- 14.Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R, et al. Occupational radiation protection in interventional radiology: A joint guideline of the cardiovascular and interventional radiology society of Europe and the society of interventional radiology. Cardiovasc Intervent Radiol. 2010;33:230–9. doi: 10.1007/s00270-009-9756-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuon E, Birkel J, Schmitt M, Dahm JB. Radiation exposure benefit of a lead cap in invasive cardiology. Heart. 2003;89:1205–10. doi: 10.1136/heart.89.10.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]


