Abstract
Introduction
Retrospective evaluation of rotator cuff repair with arthroscopic or arthroscopic-assisted mini-open methods for a diagnosis of non-retracted rotator cuff tear.
Materials and methods
A total of 45 patients underwent rotator cuff repair; Group 1 (n = 24) with arthroscopic-assisted mini-open method and Group 2 (n = 21) with full arthroscopic method.
Results
Within both Group 1 and Group 2, a statistically significant results is p = 0.001. The patients of Group 2 were seen to return to daily life earlier than those of Group 1 (p = 0.001).
Conclusions
Patients where full arthroscopic repair was applied, there was evidence of an earlier return to daily life.
Level of evidence
IV, retrospective comparative study.
Keywords: Arthroscopic surgery, Rotator cuff tears, Shoulder joint
1. Introduction
Many studies have been made on the results of surgical treatment of rotator cuff tears using various treatment methods.1 Surgical techniques have progressed from traditional open repair to arthroscopic-assisted mini-open and as an increasingly less invasive method, towards full arthroscopic repair. With the use of a smaller incision in arthroscopic rotator cuff repair, despite the advantages such as preservation of the deltoid muscle, the possibility of diagnosis and treatment of concomitant intra-articular lesions, less soft tissue damage and less postoperative pain, which method is best for the repair of full thickness rotator cuff tears is still a matter of debate. The controversy continues because bone-tendon fixation is weaker with the full arthroscopic technique.2
In the full arthroscopic method, which is in widespread current use, the postoperative complication rate is lower than that of the open method.3 The arthroscopic-assisted mini-open repair method for rotator cuff was first described by Levy et al..4 In this study, a comparison was made of the clinical and functional results of the full arthroscopic and arthroscopic-assisted mini-open techniques used in the repair of rotator cuff tears.
2. Method
Between 2009 and 2012, a total of 55 patients with a diagnosis of non-retracted rotator cuff tear, 1–3 cm in size and who had not responded to conservative treatment underwent rotator cuff repair using the arthroscopy-assisted mini-open method (Group 1) or full arthroscopy (Group 2). The surgical technique was decided by the surgeon. This study comprised 45 patients who completed final follow-up examinations and gave informed consent to participate in the study. Follow-up time of 2 year (mean 26 months; range, 16–31 months) for the mini-open group and 2 year (mean 24 months; range, 15–28 months) for the arthroscopic group.
Physical examination, magnetic resonance imaging (MRI) and direct radiography were used in the diagnosis of the patients. Evaluation was made of pre-operative physical examination, direct radiographs, MRI and shoulder Constant Murley Scores and postoperative physical examination and shoulder Constant Murley Scores. The return to daily life of the whole patient group were determined. The patients were separated into groups of arthroscopy-assisted mini-open repair (Group 1) and full arthroscopy (Group 2).
The pre and postoperative physical examination focussed on range of movement and muscle strength. Active and passive range of movement was measured with a goniometer. Abduction, flexion, extension, internal and external rotation were examined.
The dimensions and features of the tear were evaluated intra-operatively. Patients with a non-retracted rotator cuff tear, 1–3 cm in size, were included in the study. The time to return to daily life was determined, with the key question being a record of improvement in night-time sleep. None of the patients participated in sports either at a professional or amateur level. The postoperative rehabilitation protocol was similar to that of previously reported studies and included a period of immobilization for 3–6 weeks postoperatively, followed by an active range-of-motion program at 3–6 weeks and strengthening at 6–12 weeks.3
Patients were excluded if there were signs of glenohumeral instability or restricted glenohumeral movement as a result of adhesive capsulitis, glenohumeral arthritis, or rheumatoid arthritis, any involvement of the subscapularis tendon, a SLAP lesion, any history of shoulder surgery, diabetes or where there was a high risk of non-compliance, such as patients without a permanent home or with ongoing substance abuse.
2.1. Surgical approach
The patients were operated on under general anaesthesia and in the beach-chair position. Arthroscopy portals were made as posterior, lateral and anterior portals. First, the acromion, clavicular distal tip, acromioclavicular joint, coracoid and portal locations were marked with a surgical pen. The posterior portal was opened approximately 2 cm medial and 2 cm inferior to the posterolateral corner of the acromion. The anterior portal was made approximately 2–3 cm anterior to the anterolateral corner of the acromion and the lateral portal approximately 2–4 cm lateral to the posterior of the acromioclavicular joint. The anterior portal was opened 1 cm lateral and 1 cm superior to the coracoid notch.
By first entering from the posterior portal, arthroscopic examination was made of the glenohumeral joint, then it was transferred to the subacromial space. In all patients, a clear angle and image was obtained with radiofrequence, then with the assistance of a shaver, the rotator cuff was cleaned and with full visualisation of the rotator cuff tear, the dimensions were recorded. In addition, acromioplasty was applied with a burr to create a wider space during the rotator cuff repair. Following arthroscopic debridement and arthroscopic acromioplasty in patients with the mini-open method, the deltoid muscle fibres were reached by widening the portal opened from the lateral towards the acromion anterolateral. By stripping the deltoid muscle fibres from the acromion attachment point with cautery, the rotator cuff was reached. Repair of the rotator cuff was made using knotted suture anchors in all the patients of Group 1 and Group 2. A shoulder-arm sling with abduction support was applied to all patients postoperatively.
2.2. Statistical analysis
Statistical analysis was performed using NCSS (Number Cruncher Statistical System) 2007&PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA). In the evaluation of the study data, descriptive statistical methods (mean, standard deviation, frequency, ratio, minimum, maximum) were used and in the comparison of quantitative data, Student's t-test was used in the comparison of parameters of 2 groups with normal distribution and the paired Samples t-test was used in the comparisons within the groups. Values of p < 0.01 and p < 0.05 were accepted as statistically significant.
3. Results
The study was completed with a total of 45 patients. The patients were 29 females and 16 males with a mean age of 48.78 ± 11.19 years (range, 32–69 years). The operated side was the right side in 25 (55.6%) cases and the left side in 20 (44.4%) cases. The operated side was the dominant side in 26 (57.8%) cases. The cases were evaluated in 2 groups as Group 1 (n = 24, 53.3%) where the arthroscopic-assisted mini-open technique was applied and Group 2 (n = 21, 46.7%) where a full arthroscopic operation was performed. The return to daily life of the whole patient group was determined as 10.91 ± 1.92 weeks (range, 8–15 weeks) (Table 1).
Table 1.
Distribution of descriptive characteristics of the patients.
| (n = 45) |
Min – Max |
Mean ± SD |
|
|---|---|---|---|
| Age (years) |
32–69 |
48.78 ± 11.19 |
|
| Return to Daily Life (weeks) |
8–15 |
10.91 ± 1.92 |
|
| n | % | ||
| Gender |
Female | 29 | 64.4 |
| Male |
16 |
33.6 |
|
| Side |
Right | 25 | 55.6 |
| Left |
20 |
44.4 |
|
| Dominant side |
Yes | 26 | 57.8 |
| No |
19 |
42.2 |
|
| Operation | Group 1 | 24 | 53.3 |
| Group 2 | 21 | 46.7 | |
In the examination of the pre-operative and postoperative physical examination findings, a statistically significant increase was determined in the Group 1 and Group 2 patients in the postoperative range of movement values compared to the pre-operative values (p = 0.001, p = 0.001). In the paired comparison between the Group 1 and Group 2 patients, no statistically significant difference was determined in any of the physiccal examination values (Table 2).
Table 2.
The pre and postoperative range of joint movement (External Rotation, Internal Rotation, Abduction and Flexion measurements).
| (n = 45) | (Group 1) Mean ± SD |
(Group 2) bp Mean ± SD |
|---|---|---|
| External Rotation preop postop | 40.12 ± 11.20 74.16 ± 12.80 |
41.09 ± 12.30 0.864 75.25 ± 13.79 0.723 |
| Internal Rotation preop postop | 44.11 ± 10.22 75.23 ± 12.97 |
45.29 ± 11.90 0.876 76.11 ± 10.90 0.853 |
| Abduction preop postop | 69.12 ± 11.27 140.72 ± 27.78 |
70.15 ± 12.30 0.972 138.72 ± 27.78 0.768 |
| Flexion preop postop | 75.22 ± 13.11 163.26 ± 23.50 |
73.80 ± 13.69 0.756 165.38 ± 24.80 0.790 |
*ap = 0.001 *ap = 0.001.
aStudent t-Test.
bPaired Samples Test.
*statistically highly significant for all increases between the pre-operative and postoperative range of joint movement measurements (external rotation, internal rotation, abduction, flexion).
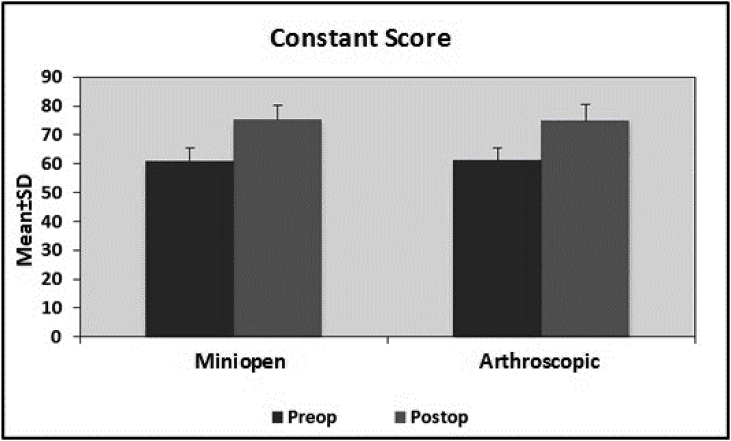
No statistically significant difference was determined in the comparison between the groups of the preoperative Constant scores (p = 0.869, p > 0.05). Similarly, no statistically significant difference was determined between the groups in the postoperative Constant scores (p = 0.874, p > 0.05). In the postoperative Constant scores a mean increase of 14.35 ± 5.68 was seen in Group 1 patients (p = 0.001) compared to the pre-operative values and in Group 2 this increase was 13.80 ± 5.94 (p = 0.001) and this was statistically highly significant (p < 0.01). No significant difference was determined between the two groups in respect of the increase in the postoperative Constant score (p = 0.790) (Table 3, Fig. 1).
Table 3.
Evaluation of the relationship between the Constant Score and the Operation Applied.
| Operation |
ap | |||
|---|---|---|---|---|
| Group 1 (n = 24) |
Group 2 (n = 21) |
|||
| Mean ± SD | Mean ± SD | |||
| Constant Score |
Preop | 60.94 ± 4.53 | 61.20 ± 4.23 | 0.869 |
| Postop |
75.29 ± 4.81 |
75.00 ± 5.61 |
0.874 |
|
|
bp |
0.001** |
0.001** |
||
| Preop – Postop change | 14.35 ± 5.68 | 13.80 ± 5.94 | 0.790 | |
**p < 0.01.
Student t-Test.
Paired Samples Test.
Fig. 1.
The change in Constant Scores from pre-operative to postoperative according to the treatment method applied.
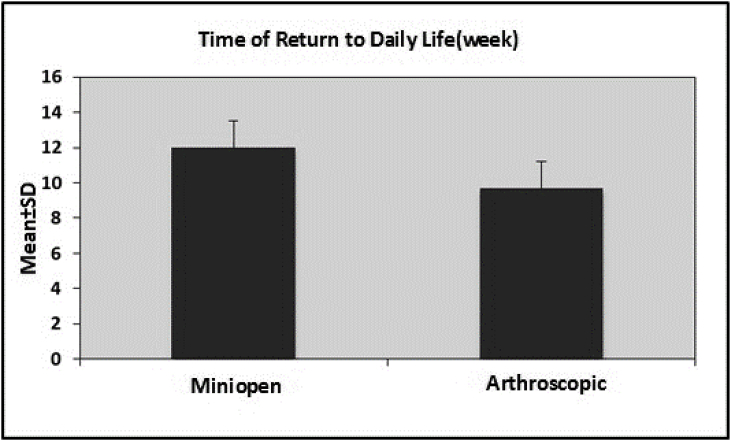
The time of return to daily life was 12.00 ± 1.54 weeks in Group 1 and 9.67 ± 1.54 weeks in Group 2. A statistically highly significant difference was determined between Groups 1 and 2 in respect of return to daily life (p = 0.001). The time of return to daily life of the Group 2 patients was seen to be shorter than that of Group 1 (Table 4, Fig. 2).
Table 4.
Time of return to daily life according to the operation applied.
| Operation |
ap | ||
|---|---|---|---|
| Group 1 (n = 24) |
Group 2 (n = 21) |
||
| Mean ± SD | Mean ± SD | ||
| Return to Daily Life (weeks) | 12.00 ± 1.54 | 9.67 ± 1.54 | 0.001** |
Student t-Test.
Fig. 2.
Time of return to daily life according to the treatment method applied.
4. Discussion
The results of this study showed a statistically significant improvement from pre-operative to postoperative in the Constant-Murley scores in all the patients (p < 0.005), but there was no significant difference between the patients who had undergone full arthroscopy and those who had undergone arthroscopy-assisted surgery. A statistically significant difference was determined between the two groups in respect of return to daily life. The time of return to daily life was shorter for the patients who had undergone fully arthroscopic surgery. There was no difference between the groups in respect of muscle strength, Constant-Murley score, wound healing or physical examination.
These findings demonstrate the reliability of both methods. For patients to be able to have a rapid return to daily life, a more experienced shoulder surgeon can select the full arthroscopic method. Rotator cuff tears are generally seen in the 40–70 years age group. Several factors are thought to be associated with the etiology of rotator cuff tears. Most attention has been focussed on two factors, which are the tensile strain of the tendon and the load borne by the rotator cuff5,6,.7
As a result of load-bearing on the shoulder, acute trauma will develop in nearly all patients over the age of 60 years. Although at a lower rate, repeated movements also cause rotator cuff tears. More extensive cuff tears are seen in elderly patients as the bone attachment points are weaker and this has been reported to increase with increasing age.
After the application of arthrosopic acromioplasty came into use, the repair of rotator cuff tears with a 3–4 cm incision between the deltoid fibres (mini-open technique) started to be used from the 1990s. As one of the first practitioners of this technique, Levy et al. reported 80% good and very good results from a 1-year follow-up of 25 patients. The necessity for acromioplasty during rotator cuff repair is controversial.8 In the current study, an antero-inferior acromioplasty procedure was applied to all the patients. Acromioplasty is recommended as it opens up space for the rotator cuff tendons, increases the quality of the tear repair by providing a better surgical view, provides protection of the tendons in the recovery period, prevents entrapment, accelerates rehabilitation and reduces postoperative pain. It is therefore applied routinely.
Although there was no statistically significant difference in the functional results between the patients to whom full arthroscopic surgery was applied and those to whom the arthroscopy-assisted mini-open method was applied, it was determined that in the full arthroscopy group the analgesia requirement of the patients was lower than that of the other group, the duration of hospitalisation was shorter, the return to preoperative activities was quicker and it was determined that the technique was helpful in the determination of glenohumeral intra-articular pathologies.9 However, in previous studies, no seriously significant difference has been determined in a comparison between the full arthroscopic method and the mini-open method10,11,12,13,.14
One of the most frequently seen complications following rotator cuff repair is the recurrence of the tear. Rates of recurrence after open surgery rotator cuff repair have been reported as varying between 13% and 68%.10 No recurrent tear was determined in the current study and no infection was seen in any patient.
Postoperatively, the affected extremities of the patients were immobilised during rehabilitation with a shoulder sling holding the shoulder joint in abduction. This method reduced postoperative pain and tension over the repaired tissue and prevented early active movements.
Full arthroscopic rotator cuff repair is technically difficult and needs experience. Early rehabilitation is an advantage in not creating damage over the deltoid muscle. However, a serious level of experience is required. The mini-open technique is less complex. When selecting the mini-open technique, the expectations of the patient must be considered together with the mechanical features of the torn cuff, the experience of the surgeon and the results obtained from various techniques.15 Although in previous studies there has been no long-term difference between the two methods, some advantages have been stated of the full arthroscopic method in the early weeks (6 weeks).16 In the current study, there was no difference between the functional scores in the long-term follow-up, but advantages of the full arthroscopic method were seen in daily activities in the early period.
5. Conclusions
The techniques of fully arthroscopic and arthroscopy-assisted mini-open surgical treatment and acromioplasty in rotator cuff repair both effectively increase the comfort of the patient and the strength and capability of active movement. While the long-term clinical and functional results of both methods were similar and successful, it was concluded that the return to dailys life was shorter in patients with full arthroscopic repair.
Ethical approval and consent to participate
Ethical approval was obtained by Fatih Sultan Mehmet Education and Research Hospital ethics committee/2014.
Consent to participate was obtained from the participants.
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Availability of supporting data
Not Applicable.
Competing interests
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Conflicts of interest
The authors declare that they have no conflict of interest.
Footnotes
No benefits in any form have been received or will be received from anybody or a commercial party related directly or indirectly to the subject of this article.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jor.2018.08.011.
Contributor Information
O. Karaman, Email: drozgurkaraman@hotmail.com.
O. Karakus, Email: ozgunkarakus@hotmail.com.
B. Saygi, Email: baranselsaygi@yahoo.com.
Abbreviations
- MRI
Magnetic Resonance İmaging
- NCSS
Number Cruncher Statistical System
- PASS
Power Analysis and Sample Size.
- SLAP
Superior Labrum Anterior Posterior
- Group 1
With arthroscopic-assisted mini-open method
- Group 2
With full arthroscopic method
Appendix ASupplementary data
The following is the supplementary data related to this article:
References
- 1.Romeo A.A., Hang D.W., Bach B.R.J.R., Shotts S. Repair of full thickness rotator cuff tears. Gender, age, and other factors affecting outcome. Clin Orthop. 1999 Oct;(367):243–255. [PubMed] [Google Scholar]
- 2.Yamaguchi K., Levine W.N., Marra G., Galatz L.M., Klepps S., Flatow E.L. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81–92. [PubMed] [Google Scholar]
- 3.Cofield R.H., Parvizi J., Hoffmeyer P.J., Lanzer W.L., IIstrup D.M., Rowland C.M. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg [Am] 2001 Jan;83-A(1):71–77. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Levy H.J., Uribe J.W., Delaney L.G. Arthroscopic assisted rotator cuff repair: preliminary results. Arthroscopy. 1990;6(1):55–60. doi: 10.1016/0749-8063(90)90099-y. [DOI] [PubMed] [Google Scholar]
- 5.McKee M.D., Yoo D.J. The effect of surgery for rotator cuff disease on general health status. Results of a prospective trial. J Bone Joint Surg [Am] 2000 Jul;82-A(7):970–979. doi: 10.2106/00004623-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Sonnabend D.H., Watson E.M. Structural factors affecting the outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002 May-Jun;11(3):212–218. doi: 10.1067/mse.2002.122272. [DOI] [PubMed] [Google Scholar]
- 7.Watson E.M., Sonnabend D.H. Outcome of rotator cuff repair. J Shoulder Elbow Surg. 2002 May-Jun;11(3):201–211. doi: 10.1067/mse.2002.122271. [DOI] [PubMed] [Google Scholar]
- 8.Hattrup S.J. Rotator cuff repair: relevance of patient age. J Shoulder Elbow Surg. 1995 Mar-Apr;4(2):95–100. doi: 10.1016/s1058-2746(05)80061-8. [DOI] [PubMed] [Google Scholar]
- 9.Demirhan M., Atalar A.C., Kocabey Y., Akalin Y. Arthroscopic-assisted mini-open rotator cuff repair. Acta Orthop Traumatol Turcica. 2002;36(1):1–6. [PubMed] [Google Scholar]
- 10.Demirhan M., Esenyel C.Z. All arthroscopic treatment ofrotator cuff tears. Acta Orthop Traumatol Turcica. 2003;37(Suppl 1):93–104. [PubMed] [Google Scholar]
- 11.Kang L., Henn R.F., Tashjian R.Z., Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007 Jun;23(6):573–582. doi: 10.1016/j.arthro.2007.01.011. e1-2. [DOI] [PubMed] [Google Scholar]
- 12.Sauerbrey A.M., Getz C.L., Piancastelli M., Lannotti J.P., Ramsey M.L., Wiliams G.R. Arthroscopic versus miniopen rotator cuff repair: a comparison of clinical outcome. Arthroscopy. 2005 Dec;21(12):1415–1420. doi: 10.1016/j.arthro.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Verma N.N., Dunn W., Adler R.S. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow up. Arthroscopy. 2006 Jun;22(6):587–594. doi: 10.1016/j.arthro.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Youm T., Murray D.H., Kubiak E.N., Rokito A.S., Zuckerman J.D. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg. 2005 Sep-Oct;14(5):455–459. doi: 10.1016/j.jse.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Harryman D.T., 2nd, Mack L.A., Wang K.Y., Jackins S.E., Richardson M.L., Matsen F.A. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg [Am] 1991 Aug;73(7):982–989. [PubMed] [Google Scholar]
- 16.Van Der Zwaal P., Thomassen B.J., Nieuwenhuijse M.J., Linderburg R., Swen J.W., Ankel E.R. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomized controlled trial in 100 patients with 1-year follow-up. Arthroscopy. 2013 Feb;29(2):266–273. doi: 10.1016/j.arthro.2012.08.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.