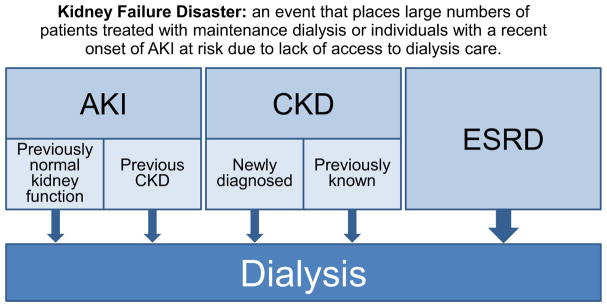
A kidney failure disaster can be defined as an event that places large numbers of patients treated with maintenance dialysis or individuals with a recent onset of acute kidney injury (AKI) at risk due to lack of access to dialysis care (Fig 1).
Figure 1.
Kidney failure in disasters. Individuals who require dialysis after a disaster may have acute kidney injury or chronic kidney disease. The majority is likely composed of individuals with end-stage renal disease already enrolled in maintenance dialysis programs.
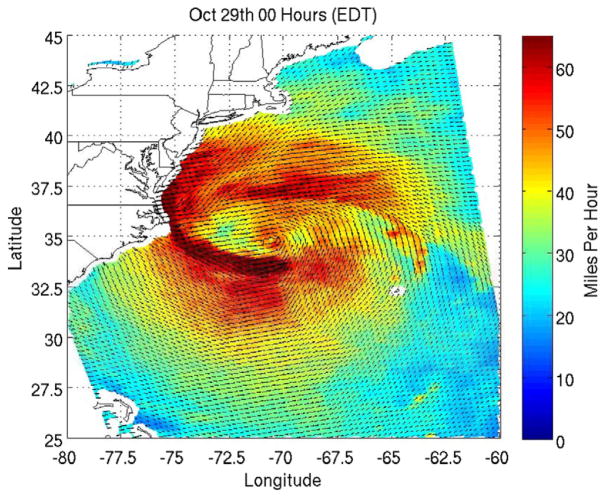
Recent reports have addressed aspects of kidney failure disasters, including Hurricane Katrina in 2005,1–4 Hurricanes Gustav and Ike in 2008,5 the L’Aquila earthquake in Italy in 2009,1,4 the Haiti earthquake in 2010,6,7 the Queensland (Australia) floods and cyclone of 2011,8 and the Fukushima earthquake and Daichii power plant accident of 2011 in Japan.9 The 2012 Atlantic hurricane season was unusually active, producing 19 named storms between June 1 and November 30. Hurricane Sandy was the largest Atlantic hurricane ever recorded and the second costliest after Hurricane Katrina. Katrina was a typical tropical cyclone with winds that circulated in a counterclockwise direction around a low-pressure center. By contrast, Sandy was a late-season extratropical cyclone that developed when both warm and cool air masses were present and was dispersed rather than compact10 (Fig 2). Although such storms typically lose force as they expand, some, like Sandy, retain hurricane force winds (≥74 mph). Sandy became a category 1 hurricane on October 24, 2012 while it was still over the Caribbean and then turned north, traveling along the Eastern United States seaboard. As it approached the coast, an unusual event occurred: Sandy interacted with a winter storm to the north, producing a “super storm.” Hurricane force winds extended 175 miles, and tropical force winds (≥39 mph) extended 485 miles. Worse, a full moon increased tides.
Figure 2.
Hurricane Sandy at the time of landfall in the United States. The image depicts the surface winds along the northeast coast of the United States at midnight October 29, 2012. Data were acquired with a radar scatterometer on board the Indian Space Research Organization’s OceanSat-2 satellite. Colors indicate wind speed and arrows indicate wind direction. Figure reproduced from the NASA Jet Propulsion Laboratory.
Sandy made landfall near Atlantic City, NJ, at 8:00 PM on Monday, October 29, 2012, with winds of 80 mph (129 km/h). The hurricane affected 24 US states, primarily along the eastern seaboard, with the most severe damage occurring in New York and New Jersey. On October 30, during the peak of service disruption, 8.5 million customers lost electrical power. Widespread evacuations were necessary. The death toll included 131 people in the United States and 122 in the Caribbean.11 US economic losses have been estimated at $83 billion. The Secretary of the US Department of Health and Human Services determined that public health emergencies existed in New York and New Jersey.
Hurricane Sandy was a kidney failure disaster as well. Dialysis care was disrupted as facilities closed either in anticipation of storm landfall or as a result of the storm, generally due to structural damage, flooding, and/or loss of electrical power. The Kidney Community Emergency Response (KCER) Coalition is a partnership that includes representatives from kidney organizations, dialysis providers, and governments.12 Technical assistance is provided to facilitate effective response to disasters that affect kidney patients. KCER held daily teleconferences as a result of Hurricane Sandy. Preliminary records of dialysis facility closures in the regions affected by the storm, particularly New York and New Jersey, for the 3 largest dialysis providers (DaVita, Fresenius Medical Care, and Dialysis Clinics Inc) are as follows: 306 facilities were closed on Tuesday, October 30 (most closures were planned in advance to minimize travel for patients and staff during the peak of the storm), 19 were closed on October 31, 12 on November 1, 4 on November 2, and 2 on November 3. By Wednesday, October 31, most facilities had reopened, one facility with severe damage had relocated, and some with severe damage remained closed. KCER data may underestimate the renal impact of the storm because information from smaller independent dialysis providers was incomplete.
The process of evaluating the impact of Sandy on the health care system in general13,14 and on the kidney care community in particular is just beginning. At the time of writing, analytic reports containing lessons learned and recommendations have been issued by KCER15 and are expected from the Centers for Medicare & Medicaid Services (CMS). Preliminary evidence suggests that the dialysis community responded well, and much credit is due to dialysis providers that had planned extensively for such events and executed their plans successfully. Fortunately, hurricane predictions usually are accurate and well publicized, allowing for sufficient warning to permit evacuation and preparation. In anticipation of the storm, many dialysis facilities dialyzed Monday patients on Sunday and Tuesday patients on Monday immediately before the storm arrived. Some treatments were reduced to 3 hours to ensure that all patients were dialyzed before the storm’s arrival Monday evening. In the face of power outages, generators were available at many dialysis facilities, but some generators failed and access to diesel fuel and gasoline was limited.16
Major infrastructure, including transportation facilities, generally was preserved, although flooding in some areas was severe, notably forcing New York University-Langone Medical Center and Bellevue Hospital in Manhattan to close.14,17 Nearby hospitals, including Beth Israel, efficiently absorbed the evacuated patients and documented a surge in maintenance dialysis patients presenting to their emergency department in need of dialysis, often with hyperkalemia. Despite the kidney community’s impressive response, some patients faced increased health risks, and some may have experienced significant health consequences due to missed dialysis sessions. For maintenance dialysis patients, the state of uncertainty may have resulted in both acute and long-term mental health consequences.18
The impact of a major disaster is particularly severe on minority communities, the elderly, the poor, and the chronically ill, a demographic pattern that mirrors the end-stage renal disease population. These are the individuals who most often are left behind without food, water, housing, or health care. The poor are more vulnerable to disasters because not only do they have fewer financial resources, but they also may reside in areas that are more vulnerable to natural disasters. The economically disadvantaged might not receive warning of impending disasters or could lack the means of evacuation, and they may have less developed social networks outside the disaster impact area for support when they leave their homes.
Food, water, shelter, safety, and acute health care needs are the first priority for responders and only later will attention be directed to caring for those with chronic disease. There are other chronic diseases that are more prevalent than kidney failure. With a disaster,19 patients may need to cope with chronic disease exacerbation, as well as the psychological impact of what they had experienced.
A recent editorial, coauthored by the Assistant Secretary for Preparedness and Response of the US Department of Health and Human Services, argues for greater community resilience in responding to people with functional needs to enable our health care system to better cope with disasters,19 and no group merits this approach more than maintenance dialysis patients. Hemodialysis care requires specialized equipment, electrical power, and high-quality water, all of which may be compromised by a disaster. Patients may present to hospital emergency departments for dialysis if their regular dialysis facility is nonoperational, but local hospitals are ill equipped to accommodate a large influx of maintenance dialysis patients. In the aftermath of a disaster, normal hospital function may be compromised. Maintenance dialysis patients need to be informed through predetermined communication systems where they will receive dialysis care. Redundant communication techniques and transportation plans are essential. Hospital emergency departments should be able to focus on people who are acutely ill while other individuals have their health care needs addressed elsewhere.
During a kidney failure disaster, particularly an unpredicted one of large scale such as a major earthquake, many dialysis units may be closed or damaged. A large-scale disaster that closes many dialysis units likely would require moving large numbers of patients. The absence of dialysis staff due to evacuation, transportation difficulties, or emergent family needs can result in the closure of dialysis units. No plans currently exist for the deployment of emergency dialysis teams in the United States. Larger dialysis providers, which have abundant resources, are the most likely to have the ability to deploy personnel and equipment to an affected region. However, the interstate movement of dialysis personnel to assist in a disaster may be difficult due to licensure restrictions. In kidney failure disasters, dialysis equipment and the personnel to operate the equipment, specifically nurses and technicians, are the most critical renal resources because a single nephrologist can supervise the care of many patients.
Other individuals who require dialysis after a disaster may include those who experience AKI, such as a crush injury with rhabdomyolyis after an earthquake, as well as those with preexisting chronic kidney disease who were not receiving dialysis care previously. Maintenance dialysis patients, including peritoneal dialysis patients, are likely to be in the largest group to require dialysis after a disaster, especially in the developed world (Fig 1). Individuals who were not receiving dialysis on a regular basis previously are not likely to have vascular access, and the resources to provide acute dialysis access will be necessary.
What are the cardinal features of kidney failure disaster preparedness? Areas that are earthquake or hurricane prone have a particular need to plan for such disasters.20
Health care officials in earthquake-prone areas need to consider the influx of large numbers of individuals with AKI as a result of crush injuries and have a plan for sufficient resources to care for patients with AKI. Isolated communities cannot depend on the arrival of additional resources within any affected disaster area for a period of days or longer
The means to assess the need for urgent dialysis must be available, including laboratory equipment for rapid measurement of serum potassium, bicarbonate, and creatinine
Means to transport patients who require dialysis outside the disaster impact area are needed because local dialysis resources are likely to be compromised. Accordingly, knowledge of nearby dialysis reserve capacity is necessary
Delays in evacuation of patients who require dialysis can be anticipated, and there may be a need for additional dialysis resources, including portable dialysis systems that can be deployed in an emergency
Essential dialysis-related medications will be needed, especially sodium polystyrene sulfonate resin to control hyperkalemia
A local kidney care/dialysis coordinator who understands community resources and is located within the local emergency operations center is highly recommended
Patients also have responsibilities. Maintenance dialysis patients must identify themselves quickly and vigorously when interacting with disaster responders because responders may not understand the consequences of missing dialysis treatments and other priorities may absorb responders’ attention. If possible, patients with chronic disease should maintain contact with their dialysis units and listen for public service announcements.
The frequency of natural disasters due to severe weather is increasing in parallel with increasing global temperatures.21 A hurricane of Sandy’s magnitude was anticipated.22 Community resilience, especially with regard to caring for those with functional needs such as dialysis dependency can be improved. Dialysis centers can improve their ability to withstand power outages by having access to emergency generators and fuel. Many dialysis centers in New York and New Jersey were able to reopen after Sandy’s landfall using generator power, although in some emergencies, plans for alternate water sources, such as water tankers, may be needed. The kidney care community has an obligation to advocate for patients and to participate in disaster-related kidney care and planning. Nephrologists should educate first responders in their local communities with respect to the needs of kidney patients so that their patients receive timely dialysis. With each kidney failure disaster, preparedness and response should improve.
Acknowledgments
The authors gratefully acknowledge receiving data on dialysis closures from the KCER and critical manuscript review by CMS staff and CDR Michelle Braun, US Public Health Service (National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK]).
Support: This work was supported in part the Intramural Research Program of the NIDDK, National Institutes of Health.
Financial Disclosure: The authors declare that they have no relevant financial interest.
Contributor Information
Kenneth D. Lempert, Nephrology Consultants of Northwest Ohio, Toledo, Ohio.
Jeffrey B. Kopp, National Institutes of Health, Bethesda, Maryland.
References
- 1.Bonomini M, Stuard S, Dal Canton A. Dialysis practice and patient outcome in the aftermath of the earthquake at L’Aquila, Italy, April 2009. Nephrol Dial Transplant. 2011;26:2595–2603. doi: 10.1093/ndt/gfq783. [DOI] [PubMed] [Google Scholar]
- 2.Kopp JB, Ball LK, Cohen A, et al. Kidney patient care in disasters: emergency planning for patients and dialysis facilities. Clin J Am Soc Nephrol. 2007;2:825–838. doi: 10.2215/CJN.01220307. [DOI] [PubMed] [Google Scholar]
- 3.Kopp JB, Ball LK, Cohen A, et al. Kidney patient care in disasters: lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol. 2007;2:814–824. doi: 10.2215/CJN.03481006. [DOI] [PubMed] [Google Scholar]
- 4.Vanholder R, Stuard S, Bonomini M, Sever MS. Renal disaster relief in Europe: the experience at L’Aquila, Italy, in April 2009. Nephrol Dial Transplant. 2009;24:3251–3255. doi: 10.1093/ndt/gfp335. [DOI] [PubMed] [Google Scholar]
- 5.Kleinpeter MA. Disaster preparedness of dialysis patients for Hurricanes Gustav and Ike 2008. Adv Perit Dial. 2009;25:62–67. [PubMed] [Google Scholar]
- 6.Portilla D, Shaffer RN, Okusa MD, et al. Lessons from Haiti on disaster relief. Clin J Am Soc Nephrol. 2010;5:2122–2129. doi: 10.2215/CJN.03960510. [DOI] [PubMed] [Google Scholar]
- 7.Vanholder R, Borniche D, Claus S, et al. When the earth trembles in the Americas: the experience of Haiti and Chile 2010. Nephron Clin Pract. 2011;117:c184–c197. doi: 10.1159/000320200. [DOI] [PubMed] [Google Scholar]
- 8.Johnson DW, Hayes B, Gray NA, Hawley C, Hole J, Mantha M. Renal services disaster planning: lessons learnt from the 2011 Queensland floods and North Queensland cyclone experiences. Nephrology (Carlton) 2013;18:41–46. doi: 10.1111/nep.12008. [DOI] [PubMed] [Google Scholar]
- 9.Kamei D, Kuno T, Sato S, Nitta K, Akiba T. Impact of the Fukushima Daiichi nuclear power plant accident on hemodialysis facilities: an evaluation of radioactive contaminants in water used for hemodialysis. Ther Apher Dial. 2012;16:87–90. doi: 10.1111/j.1744-9987.2011.01029.x. [DOI] [PubMed] [Google Scholar]
- 10.Sever MS, Erek E, Vanholder R, et al. Features of chronic hemodialysis practice after the Marmara earthquake. J Am Soc Nephrol. 2004;15:1071–1076. doi: 10.1097/01.asn.0000119145.40232.67. [DOI] [PubMed] [Google Scholar]
- 11.Wikipedia. [Accessed December 31, 2012];Hurricane Sandy. http://enwikipediaorg/wiki/Hurricane_Sandy.
- 12.Hanthorn M, Gore S, Holloway S. KCER serves as community source for disaster preparedness and response. Nephrol News Issues. 2011;25:25–27. [PubMed] [Google Scholar]
- 13.Abramson DM, Redlener I. Hurricane Sandy: lessons learned, again. Disaster Med Public Health Prep. 2012;6:328–329. doi: 10.1001/dmp.2012.76. [DOI] [PubMed] [Google Scholar]
- 14.Redlener I, Reilly MJ. Lessons from Sandy—preparing health systems for future disasters. N Engl J Med. 2012;367:2269–2271. doi: 10.1056/NEJMp1213486. [DOI] [PubMed] [Google Scholar]
- 15.Kidney Community Emergency Response Coalition (KCER) [Accessed February 17, 2013];Hurricane Sandy after action report. 2012 Dec; http://www.kcercoalition.com/
- 16.Lindsey H. Hurricane Sandy. Dialysis community manages damage, outages, displacement. Nephrol Times. 2012;5:8–11. [Google Scholar]
- 17.Ofri D. The storm and the aftermath. N Engl J Med. 2012;367:2265–2267. doi: 10.1056/NEJMp1213843. [DOI] [PubMed] [Google Scholar]
- 18.Neria Y, Shultz JM. Mental health effects of Hurricane Sandy: characteristics, potential aftermath, and response. JAMA. 2012;308:2571–2572. doi: 10.1001/jama.2012.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jan S, Lurie N. Disaster resilience and people with functional needs. N Engl J Med. 2012;367:2272–2273. doi: 10.1056/NEJMp1213492. [DOI] [PubMed] [Google Scholar]
- 20.Fukagawa M. Nephrology in earthquakes: sharing experiences and information. Clin J Am Soc Nephrol. 2007;2:803–808. doi: 10.2215/CJN.00530107. [DOI] [PubMed] [Google Scholar]
- 21.Grinsted A, Moore JC, Jevrejeva S. Homogeneous record of Atlantic hurricane surge threat since 1923. Proc Natl Acad Sci U S A. 2012;109:19601–19605. doi: 10.1073/pnas.1209542109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rozenzweig C, Soelcki WD, Blake R, et al. Developing coastal adapatation to climate change in the New York City infrastructure-shed: process, approach, tools, and strategies. Climate Change. 2011;106:93–127. [Google Scholar]