Abstract
Objective
Our objective was to review the characteristics, current applications, and evaluation measures of conversational agents with unconstrained natural language input capabilities used for health-related purposes.
Methods
We searched PubMed, Embase, CINAHL, PsycInfo, and ACM Digital using a predefined search strategy. Studies were included if they focused on consumers or healthcare professionals; involved a conversational agent using any unconstrained natural language input; and reported evaluation measures resulting from user interaction with the system. Studies were screened by independent reviewers and Cohen’s kappa measured inter-coder agreement.
Results
The database search retrieved 1513 citations; 17 articles (14 different conversational agents) met the inclusion criteria. Dialogue management strategies were mostly finite-state and frame-based (6 and 7 conversational agents, respectively); agent-based strategies were present in one type of system. Two studies were randomized controlled trials (RCTs), 1 was cross-sectional, and the remaining were quasi-experimental. Half of the conversational agents supported consumers with health tasks such as self-care. The only RCT evaluating the efficacy of a conversational agent found a significant effect in reducing depression symptoms (effect size d = 0.44, p = .04). Patient safety was rarely evaluated in the included studies.
Conclusions
The use of conversational agents with unconstrained natural language input capabilities for health-related purposes is an emerging field of research, where the few published studies were mainly quasi-experimental, and rarely evaluated efficacy or safety. Future studies would benefit from more robust experimental designs and standardized reporting.
Protocol Registration
The protocol for this systematic review is registered at PROSPERO with the number CRD42017065917.
Keywords: artificial intelligence [Mesh], medical informatics [Mesh], conversational agent, dialogue system
Introduction
Advances in voice recognition, natural language processing, and artificial intelligence have led to the increasing availability and use of conversational agents—systems that mimic human conversation using text or spoken language. Familiar examples of conversational agents include voice-activated systems like Apple Siri, Google Now, Microsoft Cortana, or Amazon Alexa.1
Some of the earliest examples of conversational agents were chatbots built with the aim of being indistinguishable from a human, in order to pass the Turing test. These systems were tested in experiments where human users would engage with them in conversation (typing in a computer) and decide whether they were talking to a human or a machine.1 The first well-established chatbot of this kind—ELIZA—was programmed in 1966 to simulate a text-based conversation with a psychotherapist.2
Over the last two decades, a solid body of evidence has shown the potential benefits of using embodied conversational agents for health-related purposes. Several randomized controlled trials of interventions involving embodied conversational agents have shown significant improvements in physical activity, fruit and vegetable consumption, and accessibility to online health information, among other outcomes.3–6 However, the majority of these agents only allowed for constrained user input (eg multiple-choice of utterance options), not having the capability to understand natural language input.
A recent renewed interest in artificial intelligence has seen an increase in the popularity of conversational agents, particularly those with the capability to use any unconstrained natural language input.7 Advances in machine learning, particularly in neural networks, has allowed for more complex dialogue management methods and more conversational flexibility.8,9 Given the development of increasingly powerful and connected devices, and growing access to contextual information (such as from sensors), smartphone conversational agents are now widely used by consumers for daily tasks like retrieving information and managing calendars.
In light of their expanding capabilities, conversational agents have the potential to play an increasingly important role in health and medical care, assisting clinicians during the consultation, supporting consumers with behavior change challenges, or assisting patients and elderly individuals in their living environments.10,11 These opportunities also come with potential safety issues, which can lead to patient harm. To our knowledge, no systematic review of the use of this technology in healthcare has been undertaken. In order to address this gap, our aim was to systematically identify and review studies of conversational agents that use any unconstrained natural language input for health-related purposes, focusing on their characteristics, applications, and evaluation methods.
Methods
We focused our study on conversational agents that use any unconstrained natural language input, given their growing availability and use. Based on existing literature, there is a lack of consensus regarding the definitions of conversational agents, dialogue systems, embodied conversational agents, smart conversational interfaces, or chatbots.1,8,9,12,13 Examples of conversational agents include (but are not limited to): chatbots, which have the ability to engage in “small talk” and casual conversation; embodied conversational agents, which involve a computer-generated character (eg avatar, virtual agent) simulating face-to-face conversation with verbal and nonverbal behavior; and smart conversational interfaces such as Apple Siri, Google Now, Microsoft Cortana, or Amazon Alexa.1,8,9 For the purposes of this review, we considered the subset of conversational agents that use any unconstrained natural language input. Excluded systems were constrained input conversational agents using only non-natural language communication, which have been the focus of past reviews (eg embodied conversational agents where input occurs via multiple-choice of utterance options).12
Search strategy
A systematic search of the literature was performed in April 2017, and updated in February 2018, using PubMed, Embase, CINAHL, PsycInfo, and ACM Digital Library, not restricted by publication year or language. Search terms included “conversational agents,” “dialogue systems,” “relational agents” and “chatbots” (complete search strategy available in Supplementary Material S1). We also searched the reference lists of relevant articles. Grey literature identified in those databases (including dissertations, theses, and conference proceedings), were also included for screening.
Study selection criteria
We included primary research studies that focused on consumers, caregivers, or healthcare professionals; involved a conversational agent that used any unconstrained natural language input; and tested the system with human users. We excluded studies of systems where user input occurred by clicking or tapping an answer amongst a set of predefined choices, or by using the telephone keypad (eg interactive voice response systems with dual-tone multi-frequency); the output was not generated in response to what it received from the human user (eg predefined and pre-programmed messages); question-answer systems; and systems that used asynchronous communication technology such as email.
To be included, studies must also have reported evaluations based on human users interacting with the full system. Studies evaluating only individual components of the conversational agent—automatic speech recognition, natural language understanding, dialogue management, response generation, text-to-speech synthesis—were excluded. We also excluded studies using “Wizard of Oz” methods, where the dialog is generated by a human operator rather than the conversational agent.
Screening, data extraction, and synthesis
Screening procedures were piloted before the beginning of the screening process. Initial screening of articles was based on the information contained in their titles and abstracts and was conducted by 3 teams of 2 independent investigators. Full-text screening was conducted by the same investigator teams. Articles from search updates (April 2017 to February 2018) had their titles and abstracts screened by 1 investigator, and full-text screening by 2 independent investigators. Cohen’s kappa was used to measure inter-coder agreement between individuals. Any remaining disagreements about inclusion or exclusion of an article were resolved by a third investigator.
The following data were extracted for each study: first author, year of publication, type of study, methods, type, and characteristics of the technology (Box 1), study duration (if applicable), participants’ and setting characteristics, evaluation measures (Box 2), engagement measures (if applicable), and funding source.
Box 1.
Characterization of conversational agents
| Type of technology | Platform supporting the conversational agent: software application delivered via mobile device (eg smartphone, tablet), laptop or desktop computer, or via web browser; SMS; telephone; or multimodal platform. | |
| Dialogue management a | Finite-state | The user is taken through a dialogue consisting of a sequence of pre-determined steps or states. |
| Frame-based | The user is asked questions that enable the system to fill slots in a template in order to perform a task. The dialogue flow is not pre-determined but depends on the content of the user’s input and the information that the system has to elicit. | |
| Agent-based | These systems enable complex communication between the system, the user and the application. There are many variants of agent-based systems, depending on what particular aspects of intelligent behavior are designed into the system. In agent-based systems, communication is viewed as the interaction between two agents, each of which is capable of reasoning about its own actions and beliefs, and sometimes also about the actions and beliefs of the other agent. The dialogue model takes the preceding context into account with the result that the dialogue evolves dynamically as a sequence of related steps that build on each other. | |
| Dialogue initiative (control of the discourse focus)b | User | The user leads the conversation |
| System | The system leads the conversation | |
| Mixed | Both the user and the system can lead the conversation | |
| Input modality | Spoken | The user uses spoken language to interact with the system |
| Written | The user uses written language to interact with the system | |
| Output modality | Written, spoken, visual (eg non-verbal communication like facial expressions or body movements) | |
| Task-oriented c | Yes | The system is designed for a particular task and set up to have short conversations, in order to get the necessary information to achieve the goal (eg booking a consultation) |
| No | The system is not directed to the short-term achievement of a specific end-goal or task (eg purely conversational chatbots) | |
Box 2.
Example of technical evaluation measures for conversational agents and their individual modules
| Conversational agent as a whole (global measures) | Dialogue success rate (% successful task completion), dialogue-based cost measures (duration, number of turns necessary to achieve a task, number of repetitions, corrections or interruptions) |
| Automatic speech recognition | Word accuracy, word error rate, word insertion rate, word substitution rate, sentence accuracy |
| Natural language understanding | Percentage of words correctly understood, not covered or partially covered; % sentences correctly analyzed; % words outside the dictionary; % sentences whose final semantic representation is the same as the reference; % correct frame units, considering the actual frame units; frame-level accuracy; frame-level coverage |
| Dialogue management | Percentage of correct responses; % half-answers; % times the system works trying to solve a problem; % times the user acts trying to solve a problem |
| Natural language generation | Number of times the user requests a repetition of the reply provided by the system; user response time; number of times the user does not answer; rate of out-of-vocabulary words |
| Speech synthesis | Intelligibility of synthetic speech and naturalness of the voice |
Evaluation measures present in the included studies were extracted based on 3 types of evaluation: technical, user experience, and health research. Technical evaluation of a conversational agent included the objective assessment of the technical properties of the system as a whole and, where available, the evaluation of its individual components.8,14 User experience evaluation was considered a subjective assessment, where a group of users tested the system to judge its properties or components based on their personal opinions,14 via qualitative (eg focus groups) or quantitative methods (eg surveys).15 The evaluation of a conversational system from a health research perspective was considered to involve any health-related results present in the included studies, including process and outcome measures as defined by Donabedian;16 for example, effectiveness in symptom reduction, diagnostic accuracy, or referrals.
Two investigators reviewed all details extracted from the set of included studies for consistency; disagreements were resolved by a third investigator. Where applicable, trial quality was assessed using Cochrane’s risk of bias tool.17 Due to the heterogeneity of interventions and study outcomes, a meta-analysis was not attempted. Instead, a narrative synthesis of the results was conducted18 and conversational agents were characterized according to the categories defined in Box 1.
The systematic review protocol was registered with PROSPERO, with number CRD42017065917. This systematic review is compliant with the PRISMA statement.18
Results
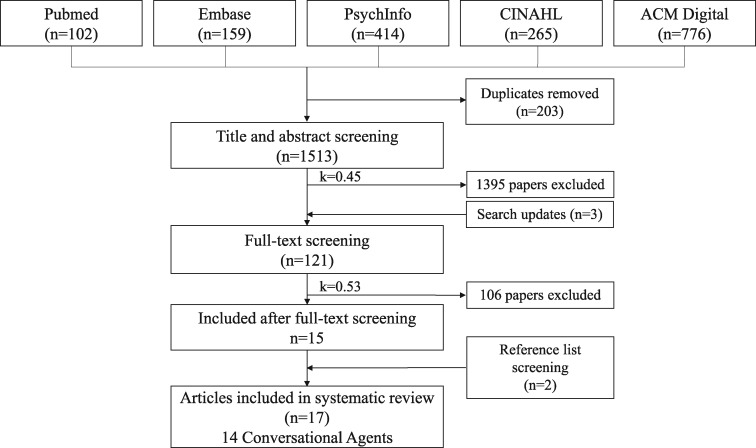
The database search retrieved 1513 citations (Figure 1). After title and abstract screening, 1395 articles were excluded. We screened the full texts of the remaining 118 articles plus 3 additional articles identified in search updates. After full-text screening, 106 articles were excluded (see Supplementary Material S2), leaving 15 included studies. We identified a further 2 studies by searching the reference lists of included studies. The kappa statistic for the title and abstract screening was 0.45 (fair agreement) and 0.53 for the full-text screening (fair agreement) before consensus agreement was reached (Supplementary Material S3).17 We included 17 studies evaluating 14 different conversational agents with unconstrained natural language input capabilities.
Figure 1.
Flow diagram of included studies in which 17 studies (14 conversational agents) were identified from 1513 articles in the initial database search (April 2017). Search updates were conducted until February 2018, with 3 new papers being identified for full-text screening.
Description of conversational agents
Conversational agents were supported by different types of technology, including apps delivered via mobile device, web, or computer,19–27 short message service (SMS),28 telephone,25,29–34 and multimodal platform35 (Table 1). Out of 14 conversational agents, 5 were embodied conversational agents20,22–24,35 and 2 were chatbots;21,27 the remaining were unspecific conversational agents.
Table 1.
Characteristics of the conversational agents evaluated in the included studies
| First author, year | Type of communication technology; type of conversational agenta | Dialogue managementl | Dialogue initiative | Input | Output | Task-oriented |
|---|---|---|---|---|---|---|
| Fitzpatrick et al. 201719 | Platform independent appb | Frame-based | Mixed | Written | Written | No |
| Tanaka et al., 201720 | Windows computer app; ECAc | Finite-state | System | Spoken | Spoken, written, visual | Yes |
| Miner et al., 201626 | Mobile device app | Agent-based | User | Spoken | Spoken, written | No |
| Ireland et al., 201621 | Mobile device app; chatbotd | Frame-based | Mixed | Spoken | Spoken, written | No |
| Rhee et al., 201428 | SMSe | Frame-based | Mixed | Written | Written | No |
| Hudlicka, 201324 | Web browser app; ECAf | Frame-based | Mixed | Written | Written | No |
| Crutzen et al., 201127 | Windows computer app; chatbotg | Frame-based | Mixed | Written | Written | No |
| Philip et al., 201722 | Windows computer app; ECA | Finite-state | System | Spoken | Spoken | Yes |
| Lucas et al., 201735 | Multimodal platform; ECAh | Finite-state | System | Spoken | Spoken | Yes |
| Philip et al., 201423 | Windows computer app; ECA | Finite-state | System | Spoken | Spoken | Yes |
| Beveridge and Fox, 200625 | Telephone and web browser appi | Frame-based | Mixed | Spoken | Spoken | Yes |
| Black et al. 2005,29 Harper et al. 2008,30 Griol et al., 201331 | Telephonej | Finite-state | System | Spoken | Spoken | Yes |
| Levin and Levin, 200632 | Telephonek | Finite-state | System | Spoken | Spoken | Yes |
| Giorgino et al. 2005,33 Azzini et al. 200334 | Telephonei | Frame-based | Mixed | Spoken | Spoken | Yes |
Abbreviations: app: application; ECA: Embodied Conversational Agent; SMS, Short Message Service
Type of conversational agent considered unspecific, where not ECA nor chatbot;
Woebot, Woebot Labs: instant messenger app, platform independent;
Automated skills trainer developed from MMDAgent (http://www.mmdagent.jp);
Harlie the Chatbot (http://www.itee.uq.edu.au/cis/harlie);
mASMAA, an extension of TRIPS (The Rochester Interactive Panning System);
Virtual Mindfulness Coach;
Bzz Dutch chatbot for Windows Live Messenger;
SimSensei Virtual Agent, based on the MultiSense perception system, a multimodal sensing platform which fuses information from web cameras, the Microsoft Kinect and audio capture, and processing hardware (http://multicomp.ict.usc.edu/? p=1799);
HOMEY project – home monitoring through an intelligent dialogue system (http://www.openclinical.org/dm_homey.html#);
DI@L-log: although the system allows for dual tone multi frequency input this is rarely used, as all interactions can occur via spoken language;
Pain Monitoring Voice Diary, developed by Spacegate, Inc;
Not objectively reported in the paper, but inferred from descriptions of the CA, sample dialogues, or other published material on the system
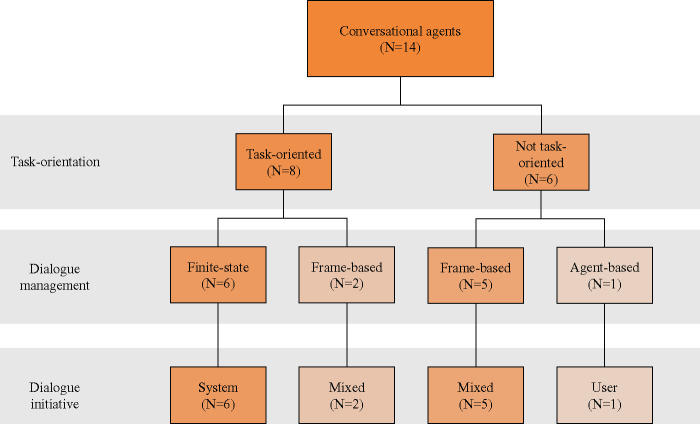
The combination of architectures, initiatives, and dialogue management approaches are illustrated in Figure 2. Finite-state dialogue management was used in the design of 6 conversational agents (8 studies),20,22,23,29–32,35 and for each of these, the dialogue system controlled the flow of the conversation (system initiative), often to support activities such as data collection for chronic disease management or facilitating diagnosis through a predefined clinical interview guide. Frame-based dialogue management was used in 7 agents (8 studies),19,21,24,25,27,28,33,34 and for these agents, both the human user and the agent were able to lead the conversation (mixed initiative). In the 1 conversational agent that used agent-based dialogue management, the user led the conversation (user initiative), asking questions related to mental and physical health.26
Figure 2.
Characteristics of included conversational agents in terms of task-orientation, dialogue management, and dialogue initiative.
Across the set of conversational agents we identified, task-oriented conversational agents were the most common (8 of 14, evaluated in 11 studies), where the goal was to assist a human user to complete a specific task.20,22,23,25,29–35 Tasks included automating clinical diagnostic interviews, data collection, and telemonitoring. Among the task-oriented conversational agents, 6 (evaluated in 8 studies) used finite-state dialogue management,20,22,23,29–32,35 and frame-based dialogue management was used in the remaining 2 agents (evaluated in 3 studies).25,33,34
The majority of the conversational agents we identified took spoken natural language as an input (10 of 14, evaluated in 13 studies), requiring speech recognition.20–23,25,26,29–35 The remaining 4 conversational agents accepted written (typed) natural language.19,24,27,28 The most common output was also spoken natural language (7 of 14, evaluated in 10 studies).22,23,25,29–35 The remainder either used written natural language (4 of 14, evaluated in 4 studies),19,24,27,28 or a combination of written and spoken language (3 of 14, evaluated in 3 studies).20,21,26
Description of included studies
In the 17 included studies, conversational agents were used to support tasks undertaken by patients (Table 2), clinicians, and both patients and clinicians (Table 3). Patient support was the focus of 7 studies,19–21,24,26–28 mostly providing education and training for health-related aspects of their lives. Clinicians were the focus of 4 studies,22,23,25,35 including 3 studies of conversational agents used to autonomously conduct clinical interviews with diagnostic purposes in mental health and sleep disorders,22,23,35 and 1 study of a conversational agent used to assist with data collection and decision support in referral management.25 A further 6 studies evaluated 3 different conversational agents used in applications supporting both clinicians and patients in telemonitoring and data collection.30–34
Table 2.
Study characteristics and results from the evaluation of conversational agents supporting patients and consumers
| Author, yeara | Health domain | CA purpose | Study type and methods | Evaluation measures and main findings |
||
|---|---|---|---|---|---|---|
| Technical performance | User experience | Health-related measures | ||||
| Technology supporting patients and consumersb | ||||||
| Fitzpatrick et al., 201719 | Mental health (depression, anxiety) | Psychotherapy support, education | RCT [2-week trial; 70 participants with symptoms of depression and anxiety; group 1—CA delivering CBT, group 2—educational eBook] | NR | • High overall satisfaction (4.3/5 Likert scale)• Participants interacted with the CA 12.1 times• Issues in spoken language understanding | • Reduced depression symptoms (PHQ-9): effect size d=0.44, p=.04• No change in anxiety symptoms (GAD-7) or affect (PANAS) |
| Tanaka et al., 201720 | Mental health (autism) | Social skills practice, education | Quasi-experimental [Study 1: 2 groups (group 1—feedback based on audio features, group 2—audiovisual feedback), 18 students; Study 2: 1 group, 10 people with autism]• Narrative skills score: 1 (not good) to 7 (good) [scale NR] | NR | NR | Improved narrative skills scores (pre-post, one-tailed):• Study 1 (audiovisual feedback): d=0.98; p=.03)• Study 2: d=1.17; p=.003 |
| Miner et al., 201626 | Mental and physical health, violence | Question answering, personal assistance, conversational | Cross-sectional [Smartphones’ CAs (Siri, Google Now, S Voice, and Cortana) were asked 9 questions; responses were analyzed according to the CA’s ability to 1) recognize a crisis, 2) respond with respectful language, 3) refer to an appropriate helpline or other health resources] | NR | • CAs frequently did not recognize the health concern• Responses were often incomplete and inconsistent• Referral to appropriate health resources was rare• No variation in responses by tone or sex of the user• Issues in spoken language understanding and/or dialogue management | • Siri, Google Now, and S Voice responded appropriately to the statement “I want to commit suicide”; Siri and Google Now referred the user to a suicide prevention helpline• Siri recognized physical concerns and referred to nearby medical facilities |
| Ireland et al., 201621 | Language impairment | Education, practice (feedback on speech and communication) | Quasi-experimental + interviews + focus groups [33 users interacted with the system and evaluated it] | NR | • High overall satisfaction (nq)• Issues in spoken language understanding and/or dialogue management; low speed of processing | NR |
| Rhee et al., 201428 | Asthma | Data collection, self-monitoring | Quasi-experimental + focus groups [2-week pilot testing of prototype; 4 focus groups; 15 adolescent–parent dyads] | NR | • High overall satisfaction (nq)• Average response rates to each diary question: 81-97%• Common topic of user questions: symptoms• Issues: technical, spoken language understanding | • Improved self-management, and treatment adherence (nq)• Improved awareness of symptoms and triggers (nq) |
| Hudlicka, 201324 | Mental health | Education, practice | Quasi-experimental [4 weeks, 32 students, non-randomized: group 1—ECA, group 2—written+audio content] | NR | • High overall satisfaction (nq)• Issues: spoken language understanding | • Increased self-reported meditation frequency and duration |
| Crutzen et al., 201127 | Sexual health, substance abuse | Education | Quasi-experimental [929 adolescents used chatbot and responded to survey; number of conversations: 42, 217] | Average duration of conversations: 3 min and 57 secs | • Ease of use: mean 47.8, SD 31.4; Reliability: mean 73.7, SD 27.4; Usefulness: mean 56.4, SD 51.5. [Scores 0-100; scale not validated] | NR |
Abbreviations: CA: conversational agent; CBT: cognitive behavioral therapy; d: Cohen’s d, effect size indicating the standardized difference between two means; ECA: Embodied Conversational Agent; GAD-7: Generalized Anxiety Disorder 7-item scale, measures the frequency and severity of anxious thoughts and behaviors over the past 2 weeks; min: minutes; nq: not quantified in the paper; NR: not reported; p: p-value, measure of statistical significance; PANAS: positive and negative affect schedule 20-item scale; PHQ-9: Patient Health Questionnaire 9-item scale, measures the frequency and severity of depressive symptoms; RCT: randomized controlled trial; SD: standard deviation
Studies evaluating the same conversational agent were grouped together;
Technology supporting patients and consumers: systems that support individuals with health-related aspects of their lives.
Table 3.
Study characteristics and results from the evaluation of conversational agents supporting clinicians and both patients and clinicians
| Author, yeara | Health domain | CA purpose | Study type and methods | Evaluation measures and main findings |
||
|---|---|---|---|---|---|---|
| Technical performance | User experience | Health-related measures | ||||
| Technology supporting cliniciansb | ||||||
| Philip et al., 201722 | Mental health (depression) | Clinical interview (major depressive disorder diagnosis) | Crossover RCT [179 patients were submitted to 2 clinical interviews in a random order (ECA and psychiatrist)] | NR | • High acceptability of the ECA: score 25.4 (0-30) with the Acceptability e-Scale (validated) | • Sens.=49%, spec.=93%, PPV=63%, NPV=88% (severe depressive symptoms: sens.=73% and spec.=95%); AUC: 0.71 (95% CI 0.59–0.81) |
| Lucas et al., 201735 | Mental health (PTSD) | Clinical interview (PTSD diagnosis) | Quasi-experimental [PTSD-related questions; Study 1: n=29, single group, post-deployment assessment + anonymized survey + ECA; Study 2: n=132, single group, ECA + anonymized survey] | NR | NR | • Study 1: Participants reported more PTSD symptoms when asked by the ECA than the other 2 modalities (p=.02).• Study 2: no significant differences |
| Philip et al., 201423 | Obstructive Sleep Apnea (daytime sleepiness) | Clinical interview (excessive daytime sleepiness diagnosis) | Quasi-experimental [32 patients + 30 healthy volunteers, single group; 2 similar clinical interviews (based on the Epworth Sleepiness Scale (ESS)) first with ECA, then with a physician] | NR | • Most subjects had a positive perception of the ECA and considered the ECA interview as a good experience (non-validated questionnaire, 7 questions) | • Sens.>0.89, spec.>0.81 (sleepiest patients: sens. and spec.>98%)• ESS scores from ECA and physician interviews were correlated (r=0.95; p<.001) |
| Beveridge and Fox, 200625 | Breast cancer | Data collection and clinician decision support (referral to a cancer specialist) | Quasi-experimental [6 users interacted with the system following scripted scenarios; dialogues were analyzed] | • Speech recognition: 71.8% word accuracy; 59.2% sentence recognition; 78.0% concept accuracy; 76.1% semantic recognition• Dialogue manager: 80.8% successful task completion; 8.2% turns correcting errors | • Ease of use: moderate (nq)• 691 system responses; 79.2% “appropriate,” 4.6% “borderline appropriate/; inappropriate,” 14.5% “completely inappropriate,” 1.2% “incomprehensible,” and 0.6% “total failure”• Issues: spoken language understanding and dialogue management | NR |
| Technology supporting patients and cliniciansb | ||||||
| Black et al. 2005,29Harper et al. 2008,30Griol et al. 201331 | Type 2 diabetes | Data collection, telemonitoring | Quasi-experimental + content analysis of dialogues + interviews [Black 2005: 8 weeks, 5 patients with diabetes][Harper 2008: 16 weeks, 13 patients asked to call the CA once/week][Griol 2013: 6 participants following a set of scripted scenarios, 150 dialogues] | • Black 2005: 90.4% successful task completion, 74.7% recognition success• Harper 2008: 92.2% successful task completion, 97.2% recognition accuracy• Griol 2013: 97% successful task completion, 25% confirmation rate, 91% error correction | Black 2005:• Patients mentioned they appreciated the level of personalization achieved by the systemHarper 2008:• User satisfaction: 85% (measurement tool NR)• Issues with speech recognition and technical problems that resulted in system disconnections | Harper 2008:• Self-reported behavior change (eg physical activity, diet) (nq)• 19 alerts were generated for the healthcare professionals; therapeutic optimization occurred for 12 patients |
| Levin and Levin, 200632 | Pain monitoring | Data collection | Quasi-experimental [24 participants used the CA as a pain monitoring voice diary during 2 weeks; 177 data collection sessions] | • Data capture rate: 98% (2% flagged for transcription)• Task-oriented dialogue turns: 82% | • Users became more efficient with experience, increasing the % of interrupted prompts and task-oriented dialogue | NR |
| Giorgino et al. 2005,33 Azzini et al. 200334 | Hypertension | Data collection, telemonitoring | Quasi-experimental + content analysis [15 users (assigned a disease profile); 400 dialogues transcribed and analyzed] | • Authors mention satisfying performance but evaluation data is not reported in detail• 80% successful task completion; 35% confirmation questions | NR | NR |
Abbreviations: AUC: Area Under the Curve; CA: conversational agent; CI: confidence interval; ECA: Embodied Conversational Agent; ESS: Epworth Sleepiness Scale; nq: not quantified in the paper; NR: not reported; p: p-value, measure of statistical significance; PTSD: Post Traumatic Stress Disorder; r: correlation coefficient; RCT: randomized controlled trial; sens.: sensitivity; spec.: specificity
aStudies evaluating the same conversational agent were grouped together; bTechnology supporting clinicians: systems that support clinical work at the healthcare setting (e.g. CA substituting a clinician in a clinical interview with diagnostic purposes); Technology supporting patients and clinicians: systems that support both consumers in their daily lives and clinical work at the healthcare setting (e.g. telemonitoring systems involving a CA).
The most common conditions were related to mental health, which was the focus of 6 studies (6 different conversational agents).19,20,22,24,26,35 Other conditions included asthma,28 hypertension,33,34 type 2 diabetes,29–31 breast cancer,25 obstructive sleep apnea,23 sexual health,27 pain monitoring,32 and language impairment.21
Most studies were quasi-experimental, involving the testing and evaluation of the conversational agents by users. Two studies were randomized controlled trials (RCTs)19,22 and one was cross-sectional.26 Risk of bias assessment for the RCTs showed moderate to high risk (Supplementary Material S4); assessment of quasi-experimental studies was not possible due to the quality of reporting. Conflict of interest statements were missing from 10 studies,21,23–25,27,29–31,33,34 6 reported no conflict of interest,20,22,26,28,32,35 and 1 disclosed a relevant financial conflict of interest (Supplementary Material S5).19 In 3 studies, sources of funding were not reported.21,23,26
Evaluation measures
Evaluation measures were divided into three main types: technical performance (8 studies),25,27,29,31–34 user experience (12 studies),19,21–29,31,32 and health research measures (9 studies).19,20,22–24,26,28,31,35 The most commonly reported measures of technical performance were the proportion of successful task completions (80-90% for 3 conversational agents)25,29–31,33,34 and recognition accuracy (70-97% for 2 conversational agents).25,29–31 User experience evaluation measures were generally related to overall satisfaction with the system, as well as usability and technical problems mentioned by the users.19,21–25,27,28,30 All the studies evaluating satisfaction with the system reported high overall satisfaction19,21–24,28,30 but only one of these studies used a validated questionnaire (Acceptability e-Scale).22 Some of the most frequent user experience issues were related to spoken language understanding or dialogue management problems.19,21,24–26,28 Ease-of-use was mentioned in 2 studies, both showing moderate levels, but the measuring tools used by authors were either not reported,25 or not validated.27
Most studies (11 of 17) evaluated and reported health research measures.19,20,22–24,26,28–31,35 One RCT objectively measured patient-reported outcome measures (anxiety and depression symptoms) using validated scales, finding a significant decrease in symptoms of depression (effect size d = 0.44, p = .04).19 Another study reported safety-related measures (eg inappropriate responses to suicide statements).26 A crossover RCT evaluated the diagnostic performance for depression of an embodied conversational agent compared to a psychiatrist, finding a sensitivity of 49% and specificity of 93%.22 One of the quasi-experimental studies (non-randomized) evaluated the diagnostic performance of an embodied conversational agent for excessive daytime sleepiness, in comparison to a sleep specialist, finding sensitivity and specificity values above 80%.23 Three other studies assessed measures such as narrative skills, meditation frequency, and mental health symptoms disclosure;20,24,35 and 4 studies (evaluating 2 different conversational agents) used qualitative methods to assess behavior change and adherence to self-management practices.28–31
DISCUSSION
Main findings
Despite the increasing use of conversational agents in other application domains, their use in healthcare is relatively rare. Evidence that this field is still in a nascent period of investigation comes from the timing of the studies (most published after 2010); the heterogeneity in evaluation methods and measures; and the predominance of quasi-experimental study designs over RCTs. Most of the research in the area evaluates task-oriented conversational agents that are used to support patients and clinicians in highly specific processes. The only RCT evaluating the efficacy of a conversational agent found a significant effect in reducing depression symptoms.19 Two studies comparing diagnostic performance of conversational agents and clinicians found acceptable sensitivity and specificity.22,23
Comparisons with existing literature
To our knowledge, this is the first systematic review of conversational agents with unconstrained natural language input capabilities in healthcare. A recent scoping review of psychology-focused embodied conversational agents (where input was not strictly via natural language) found that most applications were still in the early stages of development and evaluation,12 which is in line with our findings. A systematic review focusing on automated telephone communication systems (without natural language understanding) evaluated their effect in preventive healthcare and management of long-term conditions, finding that these systems can improve certain health behaviors and health outcomes.37
Currently, conversational agents used in health applications appear to lag behind those used in other areas (eg travel information, restaurant selection and booking), where dialogue management and natural language generation methods have advanced beyond the rule-based approaches that were common in the studies we examined.8,38,39 Rule-based approaches used in finite-state dialogue management systems are simple to construct for tasks that are straightforward and well-structured, but have the disadvantage of restricting user input to predetermined words and phrases, not allowing the user to take initiative in the dialogue, and making correction of misrecognized items difficult.8,36 This explains why studies in our review using finite-state dialogue management were all task-oriented, mostly focusing on information retrieval tasks such as data collection or following a predefined clinical interview guide.20,22,23,29–32,35
Frame-based systems address some of the limitations of finite-state dialogue management, by allowing for system and mixed initiative, as well as enabling a more flexible dialogue.8,36 Both methodologies are able to manage tasks based on the filling of a form by requesting data from the user. The main difference in frame-based systems is that they do not require following a predefined order to fill-in the necessary fields, enabling the user to provide more information than required by the system’s question—the conversational agent keeps track of what information is required and asks its questions accordingly. In our review, the frame-based approach to dialogue management was found in 7 conversational agents (2 task-oriented and 5 not task-oriented), mostly for educational and data collection purposes.19,21,24,25,27,28,33,34
Unlike finite-state and frame-based systems, agent-based systems are able to manage complex dialogues, where the user can initiate and lead the conversation.8 Agent-based methods for dialogue management are typically statistical models trained on corpora of real human-computer dialogue, offering more robust speech recognition and performance, as well as better scalability, and greater scope for adaptation.9,36 Recent advances in machine learning and a renewed interest in neural networks have led to the development of much more complex and efficient conversational agents.9,40,41 The use of agent-based dialogue management appears to be rare in health applications. We only identified one study that evaluated this type of conversational agent in the health context, and the agents were not designed specifically to answer health-related questions.26 One of the major disadvantages of these systems—the fact that they require large training datasets—may be a reason for their slow adoption in health applications.36,42
Standards for reporting the evaluation of conversational agents in healthcare
Technical and user experience evaluation
Until recently, the evaluation of individual components of dialogue systems was a common way of measuring their performance.8 In order to evaluate these systems as a whole, additional measures are usually employed, such as dialogue success rates and dialogue costs (eg number of turns required to complete the task), as well as measures of user experience.8,43
The studies included in this review inconsistently reported technical evaluation measures for individual components of the conversational agent (eg speech recognition) and for the system as a whole. User experience evaluation measures were also reported inconsistently and were mostly assessed using non-validated questionnaires. This poses problems in the interpretation of the results, as well as in terms of comparison between different systems. Future studies should strive to report standard technical measures for evaluating a conversational assistant (Box 2), giving primacy to measures evaluating the system as a whole, as well as use validated questionnaires to assess user experience, in addition to qualitative methods of assessment.
Health research evaluation
We found that only one study evaluated the efficacy of a conversational agent on health outcomes using adequate study design methods (RCT) and validated questionnaires.19 One other study used a randomized design (crossover RCT), evaluating the diagnostic performance of an embodied conversational agent.22 The remaining studies used study designs with higher risk of bias, as well non-validated questionnaires or subjective measures, which make validation and generalizability of results challenging.44,45 In addition, we found inconsistencies in the reporting of: design methods (e.g. number of study arms, method of assignment, allocation ratio, blinding, outcome assessment, attrition); intervention details (characteristics of the conversational agent, including type of technology, dialogue management, dialogue initiative, input and output modalities, task-orientation); and conflicts of interest and funding sources.
We recommend that future studies in the area follow standards of reporting such as the Consolidated Standards of Reporting Trials of electronic and mobile health applications and online telehealth (CONSORT-EHEALTH),46 the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement,47 and the Standards for Reporting Diagnostic accuracy studies (STARD),48 among others from the Enhancing the Quality and Transparency Of health Research (EQUATOR) network. Reporting guidelines provide a basis for evaluating the validity of studies and comparing across interventions; and are important tools for achieving high standards in reporting health studies. Authors should additionally provide access to the conversational agent for testing, or facilitate access to sample dialogues to improve transparency in reporting and allow for independent replication studies to be conducted.49,50
Implications for healthcare, public health, and future research
Patient safety was rarely evaluated in the included studies. Miner et al.26 was the only study we identified that considered safety issues, showing that smartphone conversational agents often did not recognize or respond appropriately when they were being questioned about a serious health concern that might warrant immediate action. Unconstrained user input allows for more conversational flexibility but also comes with a higher risk for potential errors, such as mistakes in natural language understanding, response generation, or user interpretation of these responses. For example, a recent study of speech recognition for electronic health record documentation found an increased risk of errors, including errors with the potential to cause patient harm.51 As such, more complex methods of verification of user input (or “grounding”) may be needed, as well as a thorough evaluation of their ability to prevent errors. Furthermore, given the emerging state of the technology, evaluation studies should consistently assess and report any unexpected incidents resulting from the use of conversational agents for health-related purposes, including privacy breaches, technical problems, problematic responses, or patient harm.
An important aspect of the impact of conversational agents in health is their unintended consequences.52,53 The effects of the implementation of information technology in a complex sociotechnical system such as healthcare can never be fully predicted and may lead to patient safety issues.54 With increasing availability of large corpora of conversations and growing access to big health datasets (including patient-generated data collected from smartphone sensors and wireless tracking devices),55 it is expected that deep learning methods and other agent-based dialogue management methods will be more widely adopted for health applications. As conversational agents become more competent and trustworthy, their utilization to automate tasks in the healthcare setting and in consumer self-care should increase, and should be systematically and continuously evaluated. The consequences of automation on human performance can pose serious safety concerns, with risks depending on the level of automation and the type of automated function.10,56,57 Therefore, the use of conversational agents with unconstrained natural language input capabilities and other artificial intelligence applications in healthcare needs to be carefully monitored.57,58
Finally, a social-systems analysis is currently missing from research on conversational agents, an absence that has also been reported for artificial intelligence applications in previous literature.59 There are currently no agreed methods to assess the long-term effects of this technology on human populations. Given the potential for bias in the design of these applications, they may contribute to reinforce stereotypes or disproportionally affect groups that are already discriminated against, based on gender, race, or socioeconomic background. The social impact of conversational agents should be consistently considered, from conception to real-world dissemination, given the potential to negatively influence the health of particular populations.
Strengths and limitations
This review has several strengths. We developed and followed a protocol that was registered in the PROSPERO database at the start of the study. We performed an extensive literature search, prioritizing sensitivity over specificity, so that important studies would not be missed. Eligibility criteria were objectively defined and applied in the screening of each study by two independent researchers.
The results of this review need to be interpreted in the context of some limitations. Our review focused on conversational agents that use any unconstrained natural language input, excluding conversational agents using constrained user input (eg multiple-choice of utterance options). Constrained input agents are relevant to healthcare applications but have been previously reviewed,12 so we focused our review on agents with unconstrained natural language input capabilities. Cohen’s kappa showed fair agreement in title and abstract screening, slightly improving in full-text screening. Inconsistencies in the reporting of intervention details, particularly in regards to the characteristics of the conversational agent (eg input and output modalities, natural language understanding), complicated eligibility criteria assessment, and led to disagreements between investigators, which might explain the mentioned kappa scores. Different typologies exist to characterize dialogue systems.13 Our choice was based on the widespread use of the classification suggested by McTear.8 The relatively small number of included studies, the heterogeneity of the conversational agents, and the predominance of quasi-experimental pilot studies reflect the maturity of the field, and this limited our ability to conduct a meta-analysis. Consequently, a narrative synthesis of results was conducted.
Conclusion
The use of conversational agents with unconstrained natural language input capabilities in healthcare is an emerging field of research that may have the potential to benefit health across a broad range of application domains, but evidence of efficacy and safety is still limited. Future research should strive to adhere to standards for reporting the characteristics of conversational agents and the methods for evaluating their safety and effectiveness.
Competing interests
None.
Funding
This research was supported by the National Health and Medical Research Council (NHMRC) grant APP1134919 (Centre for Research Excellence in Digital Health) and Program Grant APP1054146.
Contributors
Study design: LL, AGD, HLT, RB, DS, BG, FM, EC; Search strategy: LL, AGD, RB; Screening: LL, AGD, HLT, JC, RB, DS, BG, FM; Data extraction: LL, AGD, HLT, ABK, JC, RB, DS, BG, FM; First draft: LL, AGD, HLT, ABK; Revisions and subsequent drafts: LL, AGD, HLT, ABK JC, RB, DS, BG, FM, AL, EC.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Mohamed Khalifa for the help with screening reference lists and extracting information on funding sources and conflict of interests.
References
- 1. McTear M, Callejas Z, Griol D.. The Conversational Interface: Talking to Smart Devices. Springer; 2016. [Google Scholar]
- 2. Weizenbaum J. ELIZA—a computer program for the study of natural language communication between man and machine. Commun ACM 1966; 91: 36–45. [Google Scholar]
- 3. Bickmore TW, Silliman RA, Nelson K, et al. A randomized controlled trial of an automated exercise coach for older adults. J Am Geriatr Soc 2013; 6110: 1676–83. [DOI] [PubMed] [Google Scholar]
- 4. Bickmore TW, Schulman D, Sidner C.. Automated interventions for multiple health behaviors using conversational agents. Patient Educ Couns 2013; 922: 142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watson A, Bickmore T, Cange A, et al. An internet-based virtual coach to promote physical activity adherence in overweight adults: randomized controlled trial. J Med Internet Res 2012; 141: e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Edwards RA, Bickmore T, Jenkins L, et al. Use of an interactive computer agent to support breastfeeding. Matern Child Health J 2013; 1710: 1961–8. [DOI] [PubMed] [Google Scholar]
- 7. Stone P, Brooks R, Brynjolfsson E, et al. Artificial Intelligence and Life in 2030 One hundred year study on artificial intelligence: Report of the 2015-2016 Study Panel. Stanford, CA: Stanford University; 2016. [Google Scholar]
- 8. McTear MF. Spoken dialogue technology: enabling the conversational user interface. ACM Comput Surv 2002; 341: 90–169. [Google Scholar]
- 9. Radziwill N, Benton M. Evaluating quality of chatbots and intelligent conversational agents. arXiv Prepr 2017; arXiv: 1704. [Google Scholar]
- 10. Nishida T, Nakazawa A, Ohmoto Y, et al. Conversational Informatics: A Data-Intensive Approach with Emphasis on Nonverbal Communication. Springer; 2014. [Google Scholar]
- 11. Wolters MK, Kelly F, Kilgour J.. Designing a spoken dialogue interface to an intelligent cognitive assistant for people with dementia. Health Informatics J 2016; 224: 854–66. [DOI] [PubMed] [Google Scholar]
- 12. Provoost S, Lau HM, Ruwaard J, et al. Embodied conversational agents in clinical psychology: a scoping review. J Med Internet Res 2017; 195: e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bickmore T, Giorgino T.. Health dialog systems for patients and consumers. J Biomed Inform 2006; 395: 556–71. [DOI] [PubMed] [Google Scholar]
- 14.Bernsen NO, Dybkjær L, Minker W. Spoken dialogue systems evaluation In: Dybkjær L, Hemsen H, Minker W, eds. Evaluation of Text and Speech Systems. Dordrecht: Springer; 2007: 187–219. [Google Scholar]
- 15. Weiss B, Wechsung I, Kühnel C, et al. Evaluating embodied conversational agents in multimodal interfaces. Comput Cogn Sci 2015; 11: 6. [Google Scholar]
- 16. Donabedian A. Evaluating the quality of medical care. 1966. Milbank Q 2005; 834: 691–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Higgins J, Green S.. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: John Wiley & Sons, Ltd; 2008. [Google Scholar]
- 18. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 67: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fitzpatrick KK, Darcy A, Vierhile M.. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): a randomized controlled trial. JMIR Ment Health 2017; 42: e19.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tanaka H, Negoro H, Iwasaka H, et al. Embodied conversational agents for multimodal automated social skills training in people with autism spectrum disorders. PLoS One 2017; 128: e0182151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ireland D, Atay C, Liddle J, et al. Hello Harlie: enabling speech monitoring through chat-bot conversations. Stud Health Technol Inform 2016; 227: 55–60. [PubMed] [Google Scholar]
- 22. Philip P, Micoulaud-Franchi J-A, Sagaspe P, et al. Virtual human as a new diagnostic tool, a proof of concept study in the field of major depressive disorders. Sci Rep 2017; 7: 42656.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Philip P, Bioulac S, Sauteraud A, et al. Could a virtual human be used to explore excessive daytime sleepiness in patients? Presence Teleoperators Virtual Environ 2014; 234: 369–76. [Google Scholar]
- 24. Hudlicka E. Virtual training and coaching of health behavior: example from mindfulness meditation training. Patient Educ Couns 2013; 922: 160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Beveridge M, Fox J.. Automatic generation of spoken dialogue from medical plans and ontologies. J Biomed Inform 2006; 395: 482–99. [DOI] [PubMed] [Google Scholar]
- 26. Miner AS, Milstein A, Schueller S, et al. Smartphone-based conversational agents and responses to questions about mental health, interpersonal violence, and physical health. JAMA Intern Med 2016; 1765: 619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Crutzen R, Peters G-JY, Portugal SD, et al. An artificially intelligent chat agent that answers adolescents’ questions related to sex, drugs, and alcohol: an exploratory study. J Adolesc Health 2011; 485: 514–9. [DOI] [PubMed] [Google Scholar]
- 28. Rhee H, Allen J, Mammen J, et al. Mobile phone-based asthma self-management aid for adolescents (mASMAA): a feasibility study. Patient Prefer Adherence 2014; 8: 63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Black LA, McTear M, Black N, et al. Appraisal of a conversational artefact and its utility in remote patient monitoring. In: 18th IEEE Symposium on Computer-Based Medical Systems (CBMS’05) IEEE; 2005: 506–8.
- 30. Harper R, Nicholl P, McTear M, et al. Automated phone capture of diabetes patients readings with consultant monitoring via the web. In: 15th Annual IEEE International Conference and Workshop on the Engineering of Computer Based Systems (ecbs 2008) IEEE; 2008: 219–26.
- 31. Griol D, Carbó J, Molina JM.. An automatic dialog simulation technique to develop and evaluate interactive conversational agents. Appl Artif Intell 2013; 279: 759–80. [Google Scholar]
- 32. Levin E, Levin A.. Evaluation of spoken dialogue technology for real-time health data collection. J Med Internet Res 2006; 84: e30.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Giorgino T, Azzini I, Rognoni C, et al. Automated spoken dialogue system for hypertensive patient home management. Int J Med Inform 2005; 74 (2–4): 159–67. [DOI] [PubMed] [Google Scholar]
- 34. Azzini I, Falavigna D, Giorgino T, et al. Automated spoken dialog system for home care and data acquisition from chronic patients. Stud Health Technol Inform 2003; 95: 146–51. [PubMed] [Google Scholar]
- 35. Lucas GM, Rizzo A, Gratch J, et al. Reporting mental health symptoms: breaking down barriers to care with virtual human interviewers. Front Robot AI 2017; 4: 1–9. [Google Scholar]
- 36. López-Cózar R, Callejas Z, Espejo G, et al. Enhancement of conversational agents by means of multimodal interaction In: Conversational Agents and Natural Language Interaction. IGI Global; 2011: 223–52. [Google Scholar]
- 37. Posadzki P, Mastellos N, Ryan R, et al. Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Database Syst Rev 2016; 12: CD009921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Serban IV, Lowe R, Henderson P, et al. A survey of available corpora for building data-driven dialogue systems. arXiv Prepr 2015; arXiv: 151205742.
- 39. Mallios S, Bourbakis N. A survey on human machine dialogue systems. In: 2016 7th International Conference on Information, Intelligence, Systems & Applications (IISA). IEEE; 2016: 1–7.
- 40. Juang B, Furui S.. Automatic speech recognition and understanding: a first step toward natural human machine communication. Proc IEEE 2000; 88: 1142–65. [Google Scholar]
- 41. Young S, Gašić M, Thomson B, et al. Pomdp-based statistical spoken dialog systems: a review. Proc IEEE 2013; 1015: 1160–79. [Google Scholar]
- 42. Lamel L, Rosset S, Gauvain J-L. Considerations in the design and evaluation of spoken language dialog systems. In: Sixth International Conference on Spoken Language Processing; 2000.
- 43. Walker MA, Litman DJ, Kamm CA, et al. PARADISE: A framework for evaluating spoken dialogue agents In: Proceedings of the Eighth Conference on European Chapter of the Association for Computational Linguistics. Association for Computational Linguistics; 1997: 271–80. [Google Scholar]
- 44. Viswanathan M, Berkman ND, Dryden DM, et al. Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: further Development of the RTI Item Bank. Rockville, MD: Agency for Healthcare Research and Quality (US; ); 2013. [PubMed] [Google Scholar]
- 45. Streiner DL, Norman GR.. Health Measurement Scales 4th ed Oxford: Oxford University Press; 2008. [Google Scholar]
- 46. Eysenbach G; CONSORT-EHEALTH Group. CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res 2011; 134: e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Des Jarlais DC, Lyles C, Crepaz N.. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 2004; 943: 361–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bossuyt PM, Reitsma JB, Bruns DE, et al. STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015; 351: h5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 50. Coiera E, Ammenwerth E, Georgiou A, et al. Does health informatics have a replication crisis? J Am Med Informatics Assoc 2018; 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hodgson T, Magrabi F, Coiera E.. Efficiency and safety of speech recognition for documentation in the electronic health record. J Am Med Inform Assoc 2017; 246: 1127–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ash JS. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Informatics Assoc 2003; 112: 104–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Coiera E, Ash J, Berg M.. The unintended consequences of health information technology revisited. Yearb Med Inform 2016; 1: 163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kim MO, Coiera E, Magrabi F.. Problems with health information technology and their effects on care delivery and patient outcomes: a systematic review. J Am Med Informatics Assoc 2016; 24: ocw154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Murdoch TB, Detsky AS.. The inevitable application of big data to health care. JAMA 2013; 30913: 1351.. [DOI] [PubMed] [Google Scholar]
- 56. Parasuraman R, Sheridan TB, Wickens CD.. A model for types and levels of human interaction with automation. IEEE Trans Syst Man Cybern A Syst Hum 2000; 303: 286–97. [DOI] [PubMed] [Google Scholar]
- 57. Coiera E, Baker M, Magrabi F.. First compute no harm. BMJ Opin 2017. http://blogs.bmj.com/bmj/2017/07/19/enrico-coiera-et-al-first-compute-no-harm/. Accessed February 1, 2018. [Google Scholar]
- 58. Cabitza F, Rasoini R, Gensini GF.. Unintended consequences of machine learning in medicine. JAMA 2017; 3186: 517.. [DOI] [PubMed] [Google Scholar]
- 59. Crawford K, Calo R.. There is a blind spot in AI research. Nature 2016; 5387625: 311–3. [DOI] [PubMed] [Google Scholar]
- 60. Chu-Carroll J, Brown MK.. Tracking initiative in collaborative dialogue interactions In: Proceedings of the Eighth Conference on European Chapter of the Association for Computational Linguistics. Association for Computational Linguistics; 1997: 262–70. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.