Abstract
Mesenteric fibromatosis (MF) is a locally aggressive proliferative spindle cell lesion of the mesentery. A 34-year-old male presented with increasing abdominal pain and constipation. On workup, patient was found to have a large pelvic mass on CT A/P concerning for cancer. The patient underwent surgical excision of >15 cm intra-abdominal tumor along with adherent small bowel section. Histology of the tumor showed a spindle cell lesion consistent with MF. Previous reports have shown association of MF with Gardner syndrome and familial adenomatous polyposis. We present the first reported case of MF in a patient with previous neuroblastoma.
INTRODUCTION
Mesenteric fibromatosis (MF) is a rare intra-abdominal desmoid tumor of the mesentery with an incidence of 0.73% among all abdominal tumors [1]. It was first described by John Macfarlane more than 150 years ago [2]. It results from an aggressive proliferation of dermal and subcutaneous connective tissue and the development of soft tissue tumors referred to as fibromas [3]. Most fibromatosis’s are benign and lack metastatic potential, however, local recurrence following resection of MF is common [1].
The pathogenesis of MF has been described as ‘incomprehensible’ [4] as the nature of the tumor’s development has remained obscure for many years [5]. Some reports have shown association of the tumor with previous abdominal trauma, including previous surgery, hormonal estrogenic disorders and hyperestrogenic states, and genetic disorders such as familial adenomatous polyposis (FAP) and Gardner syndrome [5]. Sporadic cases of MF are extremely rare and are usually associated with genetic mutations in the APC sequence on chromosome 5 or with neurofibromatosis [6].
The clinical presentation and disease progression of MF are unpredictable. There have been reports of stable tumors with no growth for an extended period of time, there have also been cases of spontaneous tumor regression [7]. Yet aggressively proliferating and invading tumor can result in a diffuse infiltration of the mesentery and bowel leading to intestinal ischemia or to obstruction [7]. In these cases, presenting symptoms can include acute abdominal pain, constipation, ureteral obstruction and pyrexia of unknown origin often with a raised C-reactive protein [8].
We report a case of a 34-year-old male with a previous history of neuroblastoma who presented with abdominal pain and was diagnosed with MF following pathologic evaluation of the resected mass. The report will review literature on this topic and discuss possible links between MF and neuroblastoma.
CASE REPORT
A 34-year-old Caucasian male with a history of neuroblastoma presented to his primary care physician with abdominal pain and constipation. Physical exam revealed a large, firm and easily palpable mobile mass on the lower abdomen. CT revealed a heterogeneously enhancing lower abdominal neoplasm from the small bowel and sigmoid mesentery. Patient denied any other presenting symptoms. His past medical history was significant only for neuroblastoma, which was surgically resected at an outside hospital when patient was <1 year old, followed by 18 months of adjuvant chemotherapy. His family history was significant for a paternal grandfather with pancreatic cancer and squamous cell carcinoma of the forehead in the mother.
The patient was clinically stable throughout presentation. He underwent an elective exploratory laparotomy which immediately revealed a large solid mass in the pelvis arising from the small bowel mesentery of the mid-ileum and sigmoid colon wall. The mass (Fig. 1) was circumscribed until the segment of small bowel attached to the mass was reached. The attached small bowel measuring 22 cm × 2.8 cm was transected and the specimen was sent to pathology for review.
Figure1:

Gross image of mesenteric fibromatosis measuring >15 cm.
The intra-mesenteric mass was encapsulated, tan-gray colored and had a smooth and shiny external surface. The margins were free of the lesion. Histology showed a spindle cell lesion with immunohistochemical stains positive for beta-catenin consistent with MF (Fig. 2). The patient recovered well and was discharged on post-op Day 2. Patient reported to his 3 weeks follow up with no further problems.
Figure 2:
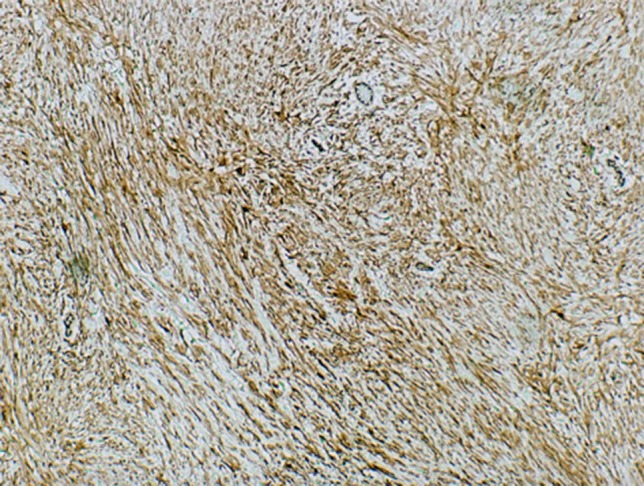
Microscopic images of beta catenin positive mesenteric fibromatosis tumor cells.
DISCUSSION
MF is a rare disease comprising only 0.73% of all abdominal tumors [1]. Of the desmoid fibromatosis, the mesenteric type is the most biologically aggressive, able to invade into both pelvic and abdominal organs [1]. The most common differential diagnosis is a Gastro Intestinal Stromal Tumor (GIST) which also presents as a spindle cell lesion [6]. Both types of tumors tend to be large, but can be differentiated based on morphology as well as histochemical stains of the tumors. While GISTs are soft and lobulated often presenting with hemorrhage and necrosis [9], MFs are usually firm, lobulated and well-circumscribed, and stain positive for CD34 and beta catenin on histochemical assays. Differentiating between the two types of tumors is important because while MF tumors are usually benign, GISTS have malignant potential [9].
Interestingly, while much of the focus has been placed on differentiating the two tumors, there have also been a number of reports of patients diagnosed with both types of tumors. Following the assessment of 28 patients with both types of tumors, Dumont et al. [10] indicated a non-random association of MF-like desmoid tumors with GISTs after a standardized incidence ratio statistical analysis showed evidence for ‘concomitant development of GIST and DT’. Their findings suggested a potential link between the two tumors and the possibility of a cancer predisposition syndrome [10]. Their report further highlights the need for more reports elucidating MF’s disease patterns and associated features.
We present a novel case of MF in a patient with a previous history of neuroblastoma. Neuroblastoma is a malignancy of the developing sympathetic nervous system that often presents in early childhood with widespread metastatic disease [11]. It accounts for 12% of childhood cancer-related deaths. Mutations in ALK and PHOX2B genes have been shown to increase the risk of developing disease [12].
Desmoid tumors, including MF, have been associated with mutations in the CTNNB1 and APC genes, with 85% of sporadic tumors presenting with CTNNB1 mutations [13]. APC gene mutations are often seen with MF associated with FAP [14]. Both CTNNB1 and APC contribute to the cell signaling pathways that control the proliferation and differentiation of cells [13]. Due to the low frequency of disease, it is likely that there are other genes involved in the development of MF.
Since this is the first case report on a patient with these two neoplasms, it’s hard to denote what type of association this presentation may indicate. It may be a coincidental association; it may also be a non-random association that is yet to be revealed statistically. Additionally, the presentation may be unrelated to the neuroblastoma itself but associated with the patient’s previous abdominal surgery performed to remove the neuroblastoma presenting as abdominal trauma—a causal entity indicated in the development of MF [5]. Nevertheless, because knowledge of MF disease pattern is scarce, this report will contribute to and guide further investigation on the pathogenesis, pathophysiology and associative features of MF in order to better detect and treat disease.
Supplementary Material
CONFLICT OF INTEREST STATEMENT
There are no financial disclosures and no conflict of interest.
FUNDING
No funding was received for this work.
REFERENCES
- 1. Li Destri G, Ferraro MJ, Calabrini M, Pennisi M, Magro G. Desmoid-type fibromatosis of the mesentery: report of a sporadic case with emphasis on differential diagnostic problems. Case Rep Med 2014;2014:850180. 10.1155/2014/850180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Macfarlane J. Clinical Reports on the Surgical Practice of the Glasgow Royal Infirmary. Glasgow: D. Robertson, 1832;63–6. [Google Scholar]
- 3. Nicolas G, Kfoury T, Shimlati R, Tohme M, Wakim R. Incidental finding and management of mesenteric fibromatosis. Am J Case Rep 2016;17:389–94. doi:10.12659/AJCR.898122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stout AP. Juvenile fibromatoses. Cancer 1954;7:953–78. [DOI] [PubMed] [Google Scholar]
- 5. Magro G, Piana M, Venti C, Lacagnina A, Ruggieri M. Solitary neurofibroma of the mesentery: report of a case and review of the literature. Pathol Res Pract 2000;196:713–8. 10.1016/s0344-0338(00)80123-5. [DOI] [PubMed] [Google Scholar]
- 6. Bethune R, Amin A. Mesenteric fibromatosis: a rare cause of acute abdominal pain. Ann R Coll Surg Engl 2006;88:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wronski M, Ziarkiewicz-Wroblewska B, Slodkowski M, Cebulski W, Gornicka B, Krasnodebski IW. Mesenteric fibromatosis with intestinal involvement mimicking a gastrointestinal stromal tumour. Radiol Oncol 2011;45:59–63. 10.2478/v10019-010-0051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang Z, Li P, Qin S, Li J. The diagnosis of mesenteric fibromatosis: a 90-month five patients case report. J Cancer Res Ther 2016;12:1318. 10.4103/09731482.199539. [DOI] [PubMed] [Google Scholar]
- 9. Yantiss R, Spiro I, Compton C, Rosenberg A. Gastrointestinal stromal tumor versus intra-abdominal fibromatosis of the bowel wall. Am J Surg Pathol 2000;24:947–57. 10.1097/00000478-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 10. Dumont AG, Rink L, Godwin AK, et al. A nonrandom association of gastrointestinal stromal tumor (GIST) and desmoid tumor (deep fibromatosis): case series of 28 patients. Ann Oncol 2012;23:1335–40. 10.1093/annonc/mdr442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pugh TJ, Morozova O, Attiyeh EF, et al. The genetic landscape of high-risk neuroblastoma. Nat Genet 2013;45:279–84. 10.1038/ng.2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Neuroblastoma Genetics Home Reference 2018. https://ghr.nlm.nih.gov/condition/neuroblastoma#genes. (10 June 10 2018, date last accessed).
- 13. Desmoid tumor Genetics Home Reference 2018. https://ghr.nlm.nih.gov/condition/desmoid-tumor#statistics. (11 June 2018, date last accessed).
- 14. Patel H. A patient with Gardner’s syndrome and familial adenomatous polyposis presenting with extra-abdominal desmoid tumors and diffuse intestinal polyposis. ACG Case Rep J 2015;2:133–4. doi:10.14309/crj.2015.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


