Abstract
Recreational drug use is a significant societal issue and remains a clinical challenge in emergency and critical care departments. We report on a 19-year-old woman admitted to hospital semiconscious and with severe hyponatraemia. Urinalysis was positive for methamphetamine and supported a diagnosis of hyponatraemia related to ecstasy use together with a syndrome of inappropriate antidiuretic hormone secretion (SIADH). The woman was transferred to an intensive care unit, where a hypertonic saline infusion was started. Three hours postadmission she developed polyuria. Follow-up urinalysis at this point was consistent with water intoxication. This case is a reminder that hyponatraemia is a potentially fatal complication after the ingestion of 3,4-methylenedioxymethamphetamine, illustrates the sequential nature of an SIADH and water intoxication and highlights the importance of considering the sequence of onset of hyponatraemia, as the patient may be admitted at any stage.
Keywords: toxicology, unwanted effects/adverse reactions, fluid electrolyte and acid–base disturbances
Background
3,4-Methylenedioxymethamphetamine (MDMA), commonly known as ecstasy, has been a popular synthetic recreational drug on the nightclub and dance scene since 1980.1 2 It is a psychostimulant drug which increases emotional sensitivity and empathy, provides a feeling of pleasure and euphoria and reduces anxiety and defensiveness.2 3 However, common negative symptoms related to MDMA use are tachycardia, hypertension, nausea, vomiting, sweating, blurred vision and muscle cramps.1 4 The central nervous system’s reaction is complex. Ecstasy has major effects on serotonin, norepinephrine and dopamine.2 3 After oral use, the onset of action is about 30–60 min and its effects last for 3–6 hours.1 3
Fortunately, in Switzerland, despite being widely used, severe intoxication remains rare.3 Medical statistics from Swiss hospitals report 0.1–0.5 acute and chronic hospitalisations per 100 000 inhabitants aged 15 years or more. The Swiss Federal Statistical Office has recorded no deaths related to any psychostimulant drugs other than cocaine since 2001. In Switzerland, as in the rest of Europe, after a decline in MDMA use at the beginning of the millennium, its popularity has been increasing again since 2010. Analysis of the Swiss market has shown that pills sold now have higher concentrations of MDMA and more added substances—such as ketamine and atropine—than in past years. Severe intoxication may be under-reported. According to the European Monitoring Centre for Drugs and Drug Addiction and to different national health institutes, however, deaths related to ecstasy seem to be increasing in the UK and the Netherlands. Hyperthermia is the most dangerous manifestation of intoxication and has been related to several deaths.2 Hyponatraemia is another complication about which the literature raises concerns. Severe or fatal hyponatraemia has been reported in association with MDMA ingestion.5–11 Despite complications such as seizures, cerebral oedema and coma, most patients recovered fully. In this context, hyponatraemia seems to have numerous causes12 due to the syndrome of inappropriate antidiuretic hormone secretion (SIADH) associated with high water intake and dancing and sweating in a hot environment. Even in the late 1990s, by which time all the different complications linked to MDMA intoxication had been very well described, there were few reports of hyponatraemia linked to water intoxication or to the combination of an SIADH and water intoxication. This report is a reminder that hyponatraemia is a potentially fatal complication after the ingestion of MDMA, and it is also proof that an SIADH and water intoxication can occur concurrently.
Case presentation
We report on a 19-year-old woman, admitted to an emergency room at 03:30 am for trouble with consciousness. Airways and breathing were normal (Respiration rate 12/min, saturation 94%). She had tachycardia of 96/min, good peripheral perfusion and blood pressure of 130/76 mm Hg. Neurologically, she only reacted to pain and had bilateral reactive mydriasis. Temperature was 38°C, and the rest of examination was unremarkable. The patient was transferred to an intensive care unit for close monitoring of her neurological state and natraemia. A central line was placed and hypertonic saline infusion started.
According to her friends, they were at a party where the patient drank a glass of vodka at 10:00 pm and complained about feeling unwell at around midnight. She vomited, then rapidly lost consciousness. An ambulance was called at 02:30 am. The patient was taking no regular medication and had no known allergies.
Investigations
Blood sugar level was 7.4 mmol/L, and ECG was unremarkable. On admission, her blood chemistry sodium level was 122 mmol/L and osmolality was 253 mOsm/kg. In urine, her sodium level was 134 mmol/L and osmolality 404 mOsm/kg. Toxicological screening of blood returned negative for ethanol, at <2.2 mmol/L or <0.10 g/L, and urinalysis was positive for methamphetamine. A brain CT scan with contrast showed no abnormality.
Three hours after admission, at the onset of polyuria, urine osmolality dropped to 55 mOsm/kg, and urine sodium was measured at <20 mmol/L.
Differential diagnosis
Neurological presentation was suggestive of marked acute hyponatraemia. In hypotonic hyponatraemia, classification according to the patient’s volume status, combined with plasma and urine chemistry, are guides to possible aetiologies and their treatment. In euvolemic hyponatraemia, urine osmolality will distinguish between an SIADH and water intoxication. In our patient, examination and plasma and urine chemistry initially pointed towards an SIADH related to the consumption of ecstasy. The second analysis, performed 3 hours later, showed a low urine osmolality suggestive—at that moment—of a water intoxication resulting from high water intake during the episode of SIADH and a drop in the level of plasmatic antidiuretic hormone (ADH) in order of autocorrection of hyponatraemia. A urinary index may be difficult to analyse since in an MDMA intoxication, hyponatraemia may be due to the combination of an SIADH and water intoxication.
Treatment
Initial hyponatraemia of 122 mmol/L was partially corrected using hypertonic 3% saline. Then the patient developed polyuria. Urine osmolality was 55 mOsm/kg, and urine sodium was below 20 mmol/L, consistent with one component of water intoxication. The hypertonic saline perfusion was replaced with a normal saline solution and natraemia rose to 133 mmol/L in 2.5 hours and then returned to a normal 140 mmol/L 27 hours after admission. Retrospectively, natraemia correction seemed fast, even if hypertonic saline had been stopped as soon as polyuria had set in. Desmopressin could have been given to avoid overcorrection of natraemia.13
Outcome and follow-up
Clinically, the patient remained semiconscious for 4 hours after admission and then became arousable before getting agitated and needing sedation. On the following day, she was calm. Before being discharged, the patient insisted that she had not knowingly taken any drugs at all. However, she did remember being very thirsty and drinking lots of water.
Fortunately, our patient suffered no complications from the rapid correction of natraemia, such as osmotic demyelination syndrome (ODS). Patients with self-induced water intoxication tend to autocorrect hyponatraemia via the physiological suppression of ADH, which leads to an acute excretion of large volumes of urine, thus the risk of ODS in these situations seems to be low.13
Discussion
Hyponatraemia induced by an SIADH and water intoxication have been well described in association with MDMA use. Our case illustrates the sequential appearance of an SIADH and water toxicity in the same patient, as documented by blood and urinalyses. Direct and indirect mechanisms have been suggested to induce an SIADH in such a context, but neither have been well characterised. Pharmacodynamics explain increased levels of serotonin by enhancing extracellular concentration and presynaptic depletion.3 14 15 Precisely how high serotonin levels influence the secretion of vasopressin remains unclear, but it is regulated by the serotoninergic pathway.14 Even a small dose of MDMA can be related to an increase in vasopressin.16 There is evidence of higher vasopressin levels after MDMA ingestion.17–19
Women seem to be more at risk of developing hyponatraemia18 and to be more symptomatic after MDMA ingestion. Most case reports, especially the fatal ones, concern women. van Dijken et al measured serum sodium concentrations in 63 ecstasy users and 44 controls at a rave party.20 Results confirmed the difference between men and women. In the small study by Simmler et al,21 the significantly elevated copeptin plasma concentrations measured in women after MDMA ingestion, but not in the men tested, added further proof of this sex difference. Furthermore, they demonstrated that duloxetine blocks the AVP (Arginine vasopressin response to MDMA in women by preventing the transporter-mediated release of serotonin and norepinephrine. Women are also more at risk of developing symptomatic hyponatraemia in other situations, such as during medical treatments, sports or postoperatively. Oestrogens seem to influence brain cell volume regulation and stimulate vasopressin secretion.22 Furthermore, according to Juul et al, women may have greater numbers of vasopressin receptors and so respond more significantly to desmopressin, resulting in a larger antidiuretic response and more hyponatraemia.23
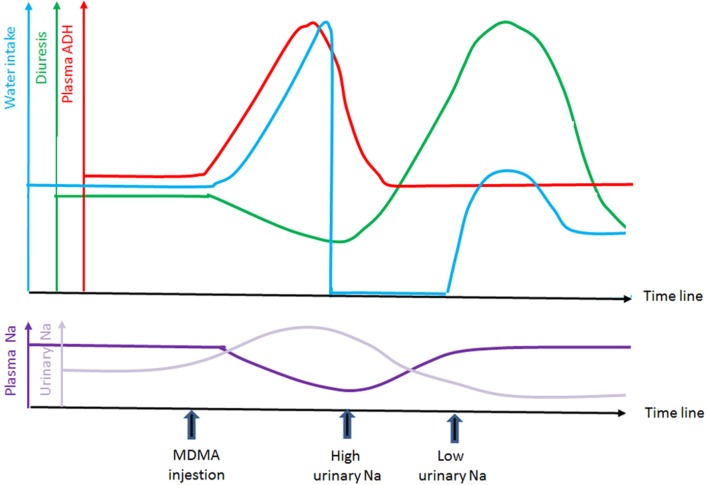
However, our patient’s first urine values were suggestive of an SIADH. The sudden change to polyuria, with low natriuresis and diluted urines, suggested the onset of water intoxication. As mentioned in the Introduction, ingesting MDMA and dancing in a hot environment both stimulate thirst and lead to the ingestion of large amounts of water. This happens in parallel with inappropriate vasopressin secretion, which also generates thirst. Awareness of the consumption of ecstasy and its side effects in nightclubbers led to prevention efforts, especially for hyperthermia, being based on encouraging ravers to drink lots of water.11 However, this worsens the risk of hyponatraemia by dilution.24 Even though today’s prevention efforts have changed and clubbers are encouraged to drink less water and visit chill-out rooms, our patient was not aware that she had ingested MDMA and so could not knowingly act against side effects. As she stated at discharge, she only remembered being very thirsty and drinking lots of water before losing consciousness. Both vasopressin secretion and water intoxication contribute to rapid and massive dilution of the blood by water. The case reported by Brvar et al,25 of an 18-year-old woman who took 300 mg of ecstasy in a suicide attempt, illustrated an SIADH followed by uncontrolled potomania worsening symptoms 3 hours after ingestion. Simple water restriction enabled resolution of the symptoms. It is thus important to understand that a patient admitted with hyponatraemia after ingesting MDMA may either be in an initial phase corresponding to an SIADH or in a secondary phase corresponding to water intoxication. Figure 1 outlines the possible timings and changes of these different elements. When correcting severe symptomatic hyponatraemia in this context, first-line doctors must be aware of this evolution and the sudden drop in ADH. We recommend closely monitoring measurements of urine, plasma sodium and osmolality to adapt treatment. Often, as in the present case, the exact time of ingestion and the different components of the pill are unknown, especially if consumption is accidental.
Figure 1.
Possible timing and changes of these different elements. ADH, antidiuretic hormone; MDMA, 3,4-methylenedioxymethamphetamine; Na, sodium.
Hyponatraemia induced by MDMA is a complex process involving pharmacokinetics, sex and the patient’s circumstances and behaviour. It has previously been suggested that water dilution and an SIADH both contribute to severe hyponatraemia in cases of MDMA ingestion but, to the best of our knowledge, this is the first case report to document both patterns in the same patient.
Learning points.
Both syndrome of inappropriate antidiuretic hormone secretion and water intoxication can contribute to hyponatraemia, but spot urine samples may be difficult to analyse.
After 3,4-methylenedioxymethamphetamine ingestion, the chronology of the onset of hyponatraemia is essential to deciding on the correct treatment.
An overcorrection of natraemia following self-induced water intoxication is difficult to avoid since these patients tend to autocorrect hyponatraemia via rapid excretion of large amounts of urine.
Severe hyponatraemia may be fatal, but the majority of cases do recover.
Women are at a higher risk of hyponatraemia with regards to the frequency and gravity of symptoms.
Footnotes
Contributors: CS: substantial contributions towards acquisition, analysis or interpretation of data. Revising the work critically for important intellectual content. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. A-LB: substantial contributions towards acquisition, analysis or interpretation of data. Revising the work critically for important intellectual content. DT: revising the work critically for important intellectual content. Final approval of the version published. Design of the figure.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Abuse NIoD. Drug Facts: MDMA (Ecstasy/Molly). 2016. https://www.drugabuse.gov/publications/drugfacts/mdma-ecstasymolly2016
- 2.Morton J. Ecstasy: pharmacology and neurotoxicity. Curr Opin Pharmacol 2005;5:79–86. 10.1016/j.coph.2004.08.007 [DOI] [PubMed] [Google Scholar]
- 3.Bodmer M, Nemec M, Scholer A, et al. Les intoxications aux amphétamines: importance pour la médecine durgences. Forum Médical Suisse ‒ Swiss Medical Forum 2008;8:534–8. [Google Scholar]
- 4.Traub SJ, Hoffman RS, Nelson LS. The “ecstasy” hangover: hyponatremia due to 3,4-methylenedioxymethamphetamine. J Urban Health 2002;79:549–55. 10.1093/jurban/79.4.549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Connor A, Cluroe A, Couch R, et al. Death from hyponatraemia-induced cerebral oedema associated with MDMA (“Ecstasy”) use. N Z Med J 1999;112:255–6. [PubMed] [Google Scholar]
- 6.Bråbäck L, Humble M. [Young woman dies of water intoxication after taking one tablet of ecstasy. Today’s drug panorama calls for increased vigilance in health care]. Lakartidningen 2001;98:817–9. [PubMed] [Google Scholar]
- 7.Hoorn EJ. A fatal case of Ecstasy poisoning. Paediatr Child Health 2001;6:491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parr MJ, Low HM, Botterill P. Hyponatraemia and death after “ecstasy” ingestion. Med J Aust 1997;166:136–7. [DOI] [PubMed] [Google Scholar]
- 9.Hartung TK, Schofield E, Short AI, et al. Hyponatraemic states following 3,4-methylenedioxymethamphetamine (MDMA, ’ecstasy') ingestion. QJM 2002;95:431–7. 10.1093/qjmed/95.7.431 [DOI] [PubMed] [Google Scholar]
- 10.Kupferschmidt H, Retnsch K, Schneemann M. Tödliches hirnàodern nach einnahme von ecstasy und benzylpiperazin. Dtsch Med Wschr 2001;126:809–11. [DOI] [PubMed] [Google Scholar]
- 11.Matthai SM, Davidson DC, Sills JA, et al. Cerebral oedema after ingestion of MDMA (“ecstasy”) and unrestricted intake of water. BMJ 1996;312:1359 10.1136/bmj.312.7042.1359b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Campbell GA RM. The agony of ecstasy: MDMA and the kidney. Clin J Am Soc Nephro 2008;3:1852–60. [DOI] [PubMed] [Google Scholar]
- 13.Uptodate. Overview of the treatment of hyponatremia in adults [database on the internet]. 2018. https://www.uptodate.com/contents/overview-of-the-treatment-of-hyponatremia-in-adults
- 14.Henry JA, Fallon JK, Kicman AT, et al. Low-dose MDMA (“ecstasy”) induces vasopressin secretion. Lancet 1998;351:1784 10.1016/S0140-6736(05)78744-4 [DOI] [PubMed] [Google Scholar]
- 15.Gowing LR, Henry-Edwards SM, Irvine RJ, et al. The health effects of ecstasy: a literature review. Drug Alcohol Rev 2002;21:53–63. 10.1080/09595230220119363 [DOI] [PubMed] [Google Scholar]
- 16.Tisdale JE, Miller DA. Drug-induced diseases: American Society of Health-System P, 2010. [Google Scholar]
- 17.Fallon JK, Shah D, Kicman AT, et al. Action of MDMA (ecstasy) and its metabolites on arginine vasopressin release. Ann N Y Acad Sci 2002;965:399–409. 10.1111/j.1749-6632.2002.tb04181.x [DOI] [PubMed] [Google Scholar]
- 18.Moritz ML, Kalantar-Zadeh K, Ayus JC. Ecstacy-associated hyponatremia: why are women at risk? Nephrol Dial Transplant 2013;28:2206–9. 10.1093/ndt/gft192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wolff K, Tsapakis EM, Winstock AR, et al. Vasopressin and oxytocin secretion in response to the consumption of ecstasy in a clubbing population. J Psychopharmacol 2006;20:400–10. 10.1177/0269881106061514 [DOI] [PubMed] [Google Scholar]
- 20.van Dijken GD, Blom RE, Hené RJ, et al. High incidence of mild hyponatraemia in females using ecstasy at a rave party. Nephrol Dial Transplant 2013;28:2277–83. 10.1093/ndt/gft023 [DOI] [PubMed] [Google Scholar]
- 21.Simmler LD, Hysek CM, Liechti ME. Sex differences in the effects of MDMA (ecstasy) on plasma copeptin in healthy subjects. J Clin Endocrinol Metab 2011;96:2844–50. 10.1210/jc.2011-1143 [DOI] [PubMed] [Google Scholar]
- 22.Ayus JC, Achinger SG, Arieff A. Brain cell volume regulation in hyponatremia: role of sex, age, vasopressin, and hypoxia. Am J Physiol Renal Physiol 2008;295:F619–24. 10.1152/ajprenal.00502.2007 [DOI] [PubMed] [Google Scholar]
- 23.Juul KV, Klein BM, Sandström R, et al. Gender difference in antidiuretic response to desmopressin. Am J Physiol Renal Physiol 2011;300:F1116–22. 10.1152/ajprenal.00741.2010 [DOI] [PubMed] [Google Scholar]
- 24.Cook TM. Cerebral oedema after MDMA (“ecstasy”) and unrestricted water intake. BMJ 1996;313:689 10.1136/bmj.313.7058.689a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brvar M, Kozelj G, Osredkar J, et al. Polydipsia as another mechanism of hyponatremia after ‘ecstasy’ (3,4 methyldioxymethamphetamine) ingestion. Eur J Emerg Med 2004;11:302–4. [DOI] [PubMed] [Google Scholar]