Abstract
Background
Concussions are responsible for numerous emergency department visits and hospitalizations among children annually. However, there remains a great deal of confusion about how to prevent and manage concussions in youth. To teach children aged 6 to 8 years about concussion safety, the Centers for Disease Control and Prevention (CDC) created a mobile gaming application called HEADS UP Rocket Blades. This report introduces the game and presents findings on its evaluation.
Methods
The aim of the game is to teach children what a concussion is, its commons signs and symptoms, how to prevent one, and what to do if one occurs. An early version of the game went through two rounds of usability testing with children and parents to obtain initial impressions and make improvements.
Results
The first round of usability testing focused on the mechanics of the game. Based on feedback from this session, CDC and the developers simplified the messaging and adjusted the game’s level of difficulty. The second round focused on the gaming experience. The children indicated that they enjoyed playing, and nearly all were able to relay at least one learning objective.
Conclusions
Parents and children rated Rocket Blades as a good learning tool and indicated that they would download it for personal use.
Keywords: concussion, mobile gaming, health communication
INTRODUCTION
In 2013, traumatic brain injuries (TBIs) were responsible for 640,000 emergency department (ED) visits, 18,000 hospitalizations, and 1,500 deaths among children 14 years of age and younger (C. A. Taylor, Bell, Breiding, & Xu, 2017). A concussion is a type of TBI that is caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement may cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and potentially damaging brain cells (Centers for Disease Control and Prevention [CDC], 2017). Within the pediatric population, a substantial percentage of concussions occur during sports- or recreation-related activities (Coronado et al., 2015; Stewart, Gilliland, & Fraser, 2014). Despite increased attention to concussions, research has demonstrated that there is still confusion among children and parents about how to both prevent concussions and handle them after an injury has occurred (Lin et al., 2015; Mannings, Kalynych, Joseph, Smotherman, & Kraemer, 2014; McKinlay, Bishop, & McLellan, 2011; University of Pittsburgh Medical Center, 2016). Making sure that parents of youth athletes know what to do if a concussion is sustained is critical for reducing the health burden of this injury.
Over the past decade, the CDC’s HEADS UP campaign has designed and disseminated concussion awareness materials for coaches, parents, and school and health care professionals. The HEADS UP campaign includes a website (www.cdc.gov/headsup) that houses information and tools for youth athletes, parents, coaches, and others interested in concussion prevention in youth and online trainings for youth sports coaches, clinicians, and youth sports officials. While such materials play an important role in concussion education, there are limits to the potential impact of didactic delivery modalities in terms of learner engagement and content retention (e.g., Höffler & Leutner, 2007). Experiential learning, and online gaming in particular, is a potentially promising avenue for education about concussion. Previous research has shown that mobile phone–based gaming applications can be valuable sources for increasing knowledge and changing behavior for a variety of health issues. For example, results from a 34-site study of young cancer patients found that the game Re-Mission was highly effective. Players showed a 70% faster acquisition of cancer-related knowledge, a threefold increase in cancer-specific efficacy, and greater adherence to medication regimens (Kato, Cole, Bradlyn, & Pollock, 2008; Tate, Haritatos, & Cole, 2009). Specific to the topic of head injuries, these applications have also been shown to increase awareness of the dangers of concussion and improve decision making with regard to removal from and returning to play (Curaudeau, Sharma, & Rovin, 2011). With this evidence and the fact that mobile applications are playing an increasingly prominent role in children’s education and entertainment (Ching, Lowenstein, Rejeski, & Thai, 2009; Kabali et al., 2015; The NPD Group, 2013), in 2015 the CDC developed an application called “HEADS UP Rocket Blades” to teach basic concussion safety to youth ages 6 to 8 years old. The application is available to download free of charge to the general public. This article is a description of the application development process, formative evaluation, and dissemination plans concerning HEADS UP Rocket Blades.
BACKGROUND
Program Overview and Theoretical Foundations
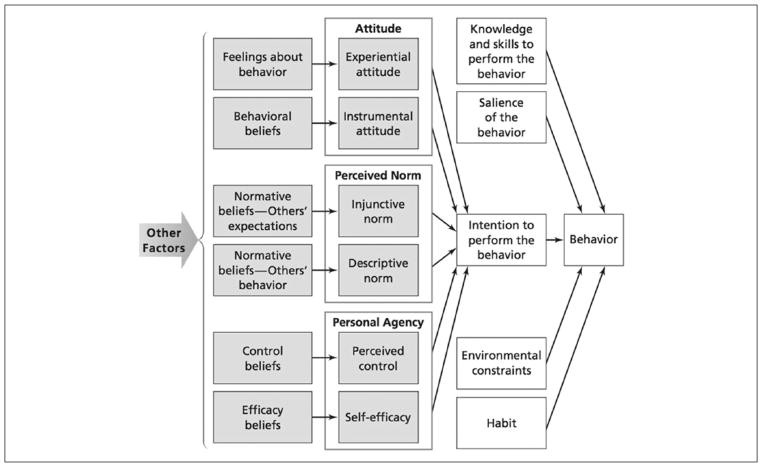
Using the backdrop of a futuristic world of racing adventures, the game aims to help children learn the benefits of engaging in recreational activities in a safe and smart manner. Using Sawyer and Smith’s (2008) taxonomy, Rocket Blades can be characterized as a preventive and educational public health–focused game. The application seeks to address two key behaviors: reporting a possible concussion to an adult and resting after sustaining a concussion. The integrated behavioral model (IBM; Montano & Kasprzyk, 2015) informed game conceptualization, targeting cognitions such as knowledge and skills necessary to report and rest after a concussion. Consistent with IBM, the constructs of habit and self-efficacy, or confidence in one’s ability to perform these behaviors, were also targeted. Habit was an integral component of the game, as game mechanics encourages players to engage in the same concussion prevention behaviors with each new level they entered. The construct of self-efficacy was applied during the game through repeated opportunities for experiential learning, verbal reinforcement, and progressive goal setting (winning the next game level). The IBM (Montano & Kasprzyk, 2015) served as a conceptual guide to situate and understand the pathways through which Rocket Blades could influence behavior. Experiential and instrumental attitudes are described as contributing factors that lead to intention or decision to perform a behavior (Montano & Kasprzyk, 2015). Attitudes in this context would refer to a player’s overall perception of favorableness or unfavorableness toward concussion prevention activities (e.g., reporting a possible concussion to an adult and resting after sustaining a concussion). Experiential attitudes would refer to the player’s emotional response to the idea of performing the concussion prevention activities. Instrumental attitudes would be determined by the player’s beliefs about outcomes of concussion prevention activities (Figure 1).
FIGURE 1.
Integrated Behavioral Model
Rocket Blades takes advantage of the fact that at the ages of 6 to 8, children are in a critical stage of developing learned attitudes toward injury. Data suggest that a majority of older adolescent and young adult athletes will continue to play a sport even after experiencing symptoms of a concussion (Llewellyn, Burdette, Joyner, & Buckley, 2014; Meehan, Mannix, O’Brien, & Collins, 2013). This behavior may result from learned attitudes regarding “toughness” that are reinforced during sport participation. Early intervention to shape safety-supportive attitudes has the potential to establish healthy behavioral patterns and reshape what is considered normative behavior (Kroshus, Gillard, Haarbauer-Krupa, Goldman, & Bickham, 2016; Morrongiello et al., 2008). Consequently, it was critical to ensure that the content of the game was developmentally appropriate. Children aged 6 to 8 benefit from learning that is based on logic and generally would be able to understand that injuries come with easily recognized symptoms that can resolve with rest (Kroshus et al., 2016; Piaget, 2003). The more “invisible” concussion symptoms, such as “feeling foggy” or “trouble remembering,” may be more difficult for children of this age to understand (Andrews, 2011). Rocket Blades illustrates some of these less-somatic symptoms with concrete graphics and cartoons.
METHOD
Development of the Game
A five-phase digital game–based learning-instructional design (DGBL-ID) model (Zin, Jaafar, & Yue, 2009) was used to develop the mobile gaming application. The DGBL-ID development process was applied to influence both experiential and instrumental attitudes, which are elements to one of the four main constructs represented in the IBM discussed above. The five phases of DGBL-ID are as follows:
Analysis: Developed a creative brief based on background research to document the characteristics of the target audience, learning objectives, and creative considerations
Design: Created a storyboard design reflecting the game’s proposed settings, characters, and interactions
Development: Created static images of the game and programmed core game mechanics
Quality assurance: Tested a prototype to ensure quality functionality
Implementation and evaluation: Conducted two rounds of usability testing to assess learning outcomes
Findings from the formative evaluations informed critical updates to key messages and design. CDC successfully implemented the DGBL-ID model to create the Rocket Blades application.
Description of the Game
Rocket Blades employs an “endless runner” design in which a player dodges obstacles while trying to complete a racecourse. The game has six levels, and the racecourse becomes progressively more difficult with each subsequent level. A user cannot “beat” the game; instead, a user earns a high score and then aims to top his or her high score in future games. From a user’s perspective, the goal of the game is for a team of three healthy players to successfully complete each game level and collect as many power gems—that is, prizes that contribute to a player’s score—as possible. The intention is to teach children about concussion while at the same time providing an enjoyable gaming experience.
Before children begin playing, however, they are required to watch a short video. The video explains the game and introduces information about concussion safety. Specifically, the video introduces the futuristic world of Rocket Blades, defines “concussion,” emphasizes the importance of safety gear (helmets), states the importance of avoiding head injury, and informs children that resting and taking a break from play after experiencing a head injury is essential for recovery.
After the intro video, the game begins in a “tutorial mode” to allow the children an opportunity to learn the mechanics of gameplay. The tutorial level also reinforces educational messages while orienting children to gameplay. The game is centered on a futuristic race where “rocket blades” are similar to rollerblades. The three skaters (players in the game) on the team wear helmets during the race, and children are told that the color of each of their players’ helmets indicates brain health (Figure 2). If a player has a green helmet, he or she has not injured his or her brain. If the player hits an obstacle or falls, the helmet will turn yellow and she or he will start to experience concussion symptoms. The child will notice that the player does not move or react as quickly and has blurry vision (Figure 3). When one of their players gets a concussion (yellow helmet), children receive a message that the player is hurt, they should tell a grown-up, and they should swap their injured player for a healthy teammate on the bench.
FIGURE 2.

Rocket Blades Screenshot Describing the Meaning of the Skaters’ Different Helmet Colors.
FIGURE 3.
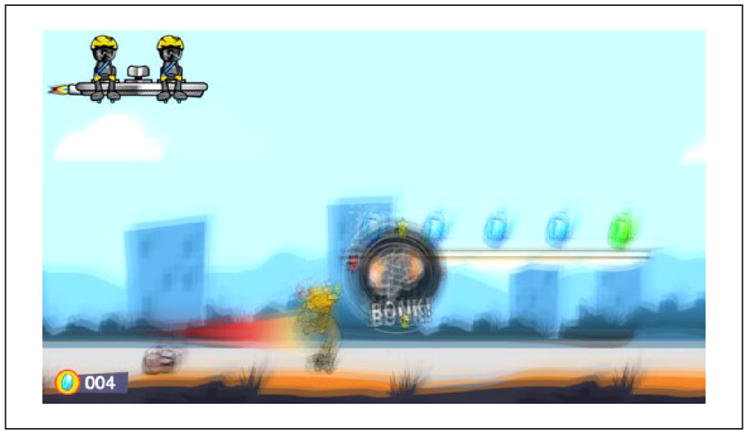
Rocket Blades Screenshot Illustrating What It lLooks Like for a Skater to Experience Concussion Symptoms.
If a child chooses not to swap out an injured player for a healthy teammate and his or her player hits another obstacle, the concussion symptoms get worse and the player’s helmet turns red. When this happens, children receive a message indicating that “[you have] hit your head while your brain was already hurt. This puts your brain in danger. You’ll need to rest and recover before playing again” (Figure 4). If all three players get concussions, then the whole team must rest and the level ends.
FIGURE 4.
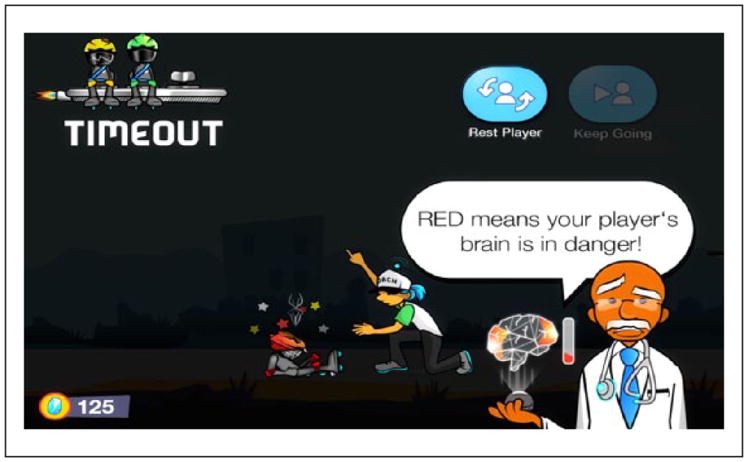
Rocket Blades Screenshot Illustrating the Warning Message Children Will Receive if One of Their Players Gets Injured After an Initial Concussion.
Children playing the game aim to safely lead their players through the course and successfully avoid obstacles to prevent a crash and subsequent concussion. As the children keep their players safe, they have the opportunity to collect “power gems.” Power gems are worth points, which accumulate to “power up” their spaceship. Injured players are not able to collect power gems. If a team fails to complete a level, the doctor and coach provide a summary about the negative effects of concussions and the importance of resting after a head injury. After completing all six levels of gameplay, players will reach “Galactic City” and are rewarded by having their photo taken for the Galactic News using the phone’s built-in camera.1 After winning, children are able to see themselves take off in their spaceship to the All-Star Party in Galactic City (Figure 5).
FIGURE 5.

Rocket Blades Screenshot Showing the All-Star Party in Galactic City That the Children Reach After Successful Completion of the Game.
Usability Testing
CDC conducted two rounds of usability testing with children and parents in January 2015 and May/June 2016 to determine the following:
If the gaming application successfully delivered intended concussion messages
If children enjoyed playing the game
If children understood the mechanics and objectives of the gaming application
Whether or not parents felt that Rocket Blades is a learning tool they would download for their children
The first round of testing focused on the application’s functionality. A pool of 12 eligible participant pairs (one child and one parent) were recruited from a market research and product-testing panel. Response saturation was met after nine pairs were interviewed, and thus interviewing was halted at that time. All participating children were between the ages of 6 and 8, were involved in team sports or other athletic activities, and played games on mobile devices regularly. The sample was divided between boys and girls. Interview guides and child-friendly feedback forms were used to solicit feedback from children and their parents during testing.
Each testing session for the first round had three distinct parts. The first part was a short introductory conversation with the child and the parent that focused on the child’s current gameplay behaviors. Next, the parent was escorted to a separate viewing room where they watched the child play Rocket Blades on a large monitor. The interviewer asked the child questions that focused on the child’s own assessment of his or her gameplay behaviors. The second part of the session focused on the task of playing the game. The child was given his or her first opportunity to play the game without any guidance from the interviewer. After several minutes of gameplay, the interviewer asked the child to pause and answer a series of questions about the child’s reactions to the game and to rate the playability and various design features of the game. The child was then given a second opportunity to play the game. The interviewer again paused the gameplay and asked the child a series of questions that focused on the child’s cognitive processing of the information he or she received while playing. The third part of the usability testing session began when the interviewer invited the parent back into the room. This final conversation with the parent and the child was structured around the parent’s assessment of the game, their recommendations for improvement, and whether they would be interested in letting their child play.
Numerous changes to the game were made after the first round of testing, including simplifying the messaging and expanding the instructions, and thus it was determined that a second round was needed. The second round of testing focused on a different set of children’s (n = 13) and parents’ (n = 12) perceptions and impressions of the game and the content. Sessions were conducted with one child–parent pair at a time. Each testing session had three distinct parts: (a) an introductory conversation with the child and the parent, (b) the child playing the game without guidance, and (c) final conversations with the child and the parent. Each session lasted between 35 and 60 minutes. Interviewers used standardized interview guides for usability testing.
At the beginning of each testing session, each child–parent pair were interviewed together regarding the child’s experience with and knowledge of concussion, the child’s exposure to video and mobile games, and how the pair identify games for the child to play. Following this initial interview, the child was taken to a separate room from the parent where he or she was asked to play Rocket Blades three times and answer questions about the game after each time. The parent was led into a room where he or she could observe the child playing the game and was subsequently asked follow-up questions regarding whether he or she thought that Rocket Blades was a good learning tool and whether this was the type of game the parent would download for his or her child. Parents were also asked general questions about concussion awareness.
Analysis
During development, CDC determined that the game would be considered successful in achieving its purpose if all of the children understood at least one of the following three learning objectives after playing the game. These learning objectives for Rocket Blades were formulated based on (a) research on concussions in youth and (b) research on how youths of this age can absorb health-related information (Coronado et al., 2015; Höffler & Leutner, 2007; Kroshus et al., 2016; Piaget, 2003; Stewart et al., 2014; C. A. Taylor et al., 2017).
Hitting your head can cause brain injury (concussion): This is important for children to learn because experiencing a concussion in childhood can interrupt the normal course of neurological development (Graham, Rivara, Ford, & Spicer, 2014; Prins & Giza, 2012) and cause long-term changes in behavior (Anderson, Godfrey, Rosenfeld, & Catroppa, 2012; Keightley et al., 2014; Li & Liu, 2013; Liu & Li, 2013; H. G. Taylor et al., 2015). In Rocket Blades, concussion is simulated by implementing strategic changes to gameplay after a character in the game hits his or her head on an object. After a skater hits an object, the screen blurs (representing blurry vision), the skater’s speed and reaction time slow, and the skater is unable to collect gems for the rest of the round (representing decreased skill postinjury).
You should tell your coach, parent, or another adult if you hit your head: This learning objective speaks to the idea that to recover properly from a concussion, a child must first let an adult know that the child hit his or her head. This concept is conveyed throughout the game through strategic messaging delivered by characters depicting a coach and a doctor.
You should rest before returning to play and see a doctor after a concussion: The final learning objective is based on the fact that once a person sustains one concussion, he or she is more likely to sustain another (CDC, 2016; Guskiewicz, McCrea, Marshall, & et al., 2003). Individuals who sustain multiple concussions tend to have longer lasting symptoms (Chrisman, Rivara, Schiff, Zhou, & Comstock, 2013; Corwin et al., 2014) and are more likely to suffer from serious neurological consequences later on (Iverson, Echemendia, LaMarre, Brooks, & Gaetz, 2012). Therefore, it is critical that if a child is suspected of having a concussion, he or she should cease activity, see a health care provider, and get cleared for activity before returning to play. In the game, the coach and doctor characters encourage children to rest an injured player and let a noninjured teammate finish the race. If the children decide to continue playing their injured player, their performance will diminish.
To determine if these learning objectives were met, after playing the game in the second round of usability testing, a trained interviewer asked each child a series of questions:
What did you think of that game?
Did you see/read the messages on the screen? Do you remember what any of them said?
What role does the coach/doctor play?
Why are they wearing helmets?
What happens when they fall? What do you think you should do when they get hurt?
What would you do if this was real life and you fell like that?
How can a person get an injury to his or her brain?
If you thought that you had an injury to your brain, would you tell someone?
Answers to the questions were recorded and analyzed for overall themes.
RESULTS
Usability Testing
The first round of usability testing focused on the mechanics of the game. Based on first-round feedback, CDC and the application developers simplified the messaging, introduced the idea of a “player swap” (the ability of the user to switch out an injured player—with a yellow or red helmet—for one who is on the bench), and added the introductory video to help explain the purpose of the game, better define concussion, and discuss basic rules of the game.
An updated version of the game was tested with children and parents during the second round of testing. During this second round of testing, all of the children seemed to enjoy playing Rocket Blades and found it generally fun and educational. Almost all of the testers could point to the purpose of the game (to avoid concussion), understood that they needed to switch out injured players to allow them to rest, and clarified their definition of “concussion” after playing the game. All of the children understood at least one of the learning objectives outlined above, and most were able to report on all three. After getting feedback during this round of testing about the messages in the application disappearing too quickly for the children to fully comprehend, messages were retained longer on the screen and certain messages were further simplified in the final version of the game. Additionally, the tutorial level was enhanced because testers stated that they would like more instructions up front about how the game works. Most testers indicated that they would recommend Rocket Blades to their friends as a fun game to play.
The parents who participated in the second round of testing similarly had positive impressions of the game after observing their children play during the testing sessions. All of the parents agreed that Rocket Blades was a good learning tool for their children, and most said that they were likely to download Rocket Blades for their children to play at home. Parents liked Rocket Blades because it clearly captures children’s attention, the information presented is easy for the children to understand, it teaches children about an important health and safety topic, it is age-appropriate, and it will be free for download.
DISCUSSION
The purpose of this article was to describe the HEADS UP Rocket Blades gaming application, which was developed using a systematic approach based on best practices for developing health communication programming for children. Findings from the usability testing were critical to achieving CDC’s aim of developing an entertaining concussion education tool for young children based on the latest science. Ultimately, both children and parents rated it as a good learning tool that was able to convey its primary learning objectives. Digital games have long been viewed as a means of child’s play and fantasy, but they are also well-suited teaching tools (Murphy et al., 2002). Similar to previous games (e.g., Kato et al., 2008; Tate et al., 2009), this evaluation of Rocket Blades has demonstrated that it has the ability to increase knowledge and change attitudes. A full evaluation of Rocket Blades will be conducted after the application has been launched to the public in order to allow CDC to collect data on how often the application is downloaded and how children use the application.
Consistent with dissemination strategies used for other CDC HEADS UP products, CDC aims to use an innovative and cost-effective approach for dissemination of Rocket Blades. The game will primarily be disseminated through partnerships with youth and sports organizations. These organizations offer existing and extensive dissemination mechanisms like email lists, newsletters, and social media platforms. Furthermore, they offer credibility among the target audience. In addition, these organizations are key influencers for concussion in sports education efforts and have contact with millions of children and parents that CDC would not otherwise be able to reach. Digital or online promotion, such as through social media platforms, will also be used. Both of these strategies have been successful in the past in disseminating HEADS UP and similar materials (Damschroder et al., 2009; Sarmiento, Hoffman, Dmitrovsky, & Lee, 2014).
To help support dissemination, CDC also developed supporting informational materials for parent and coaches, including a short video about Rocket Blades, infographics, PowerPoint slides, a handout that provides an overview of the game, and a tip sheet for parents that includes strategies for talking to their children about concussion safety. All of these materials are available for view or download on the CDC HEADS UP website (https://www.cdc.gov/headsup).
There are a few limitations to this study. First, the sample used to conduct the two sessions of usability testing was small and not randomly selected. It is also possible that the parents volunteered because they were already aware and concerned about concussions and therefore might have already taught their children about concussions and how to avoid them. The usability testing was also done in a lab setting and not in the field, which may have caused the children place more importance on their answers and to respond differently than they would if they were playing the game in a more relaxed setting. Because of these reasons, the results that we found cannot necessarily be generalizable to the entire population of children age 6 to 8. Finally, it is not clear if there are specific aspects of the Rocket Blades game that may be more or less effective, and future research would be helpful to examine how particular components of Rocket Blades influence behavior. Despite these limitations, findings from the formative evaluation have important implications for efforts designed to prevent TBIs among children. CDC’s efforts to increase concussion knowledge, embedded in an entertaining but informative context, may more likely influence the behavior of children than content distributed in a more didactic manner.
CONCLUSION
Further research is needed to understand how families are using Rocket Blades and whether there are any barriers to its use that can be addressed through an augmented dissemination and implementation strategy. CDC plans to collect data from the application after it is released to track and analyze the acquisition, engagement, and behavior of users.
Footnotes
A privacy policy in the game’s tutorial explicitly states that CDC does not save or send the photo. The decision to take a photo within the application is optional.
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. 10Years outcome from childhood traumatic brain injury. International Journal of Developmental Neuroscience. 2012;30:217–224. doi: 10.1016/j.ijdevneu.2011.09.008. [DOI] [PubMed] [Google Scholar]
- Andrews R. Concussions: Invisible injuries. International Journal of Sports & Ethics. 2011;1:31–33. [Google Scholar]
- Centers for Disease Control and Prevention. Facts about concussion and brain injury. 2016 Retrieved from https://www.cdc.gov/traumaticbraininjury/pdf/fact_sheet_concusstbi-a.pdf.
- Centers for Disease Control and Prevention. What is a concussion? 2017 Retrieved from https://www.cdc.gov/headsup/basics/concussion_whatis.html.
- Ching D, Lowenstein D, Rejeski D, Thai AM. Game changer: Investing in digital play to advance children’s learning and health. New York, NY: Joan Ganz Cooney Center; 2009. [Google Scholar]
- Chrisman SP, Rivara FP, Schiff MA, Zhou C, Comstock RD. Risk factors for concussive symptoms 1 week or longer in high school athletes. Brain Injury. 2013;27:1–9. doi: 10.3109/02699052.2012.722251. [DOI] [PubMed] [Google Scholar]
- Coronado VG, Haileyesus T, Cheng TA, Bell JM, Haarbauer-Krupa J, Lionbarger MR, … Gilchrist J. Trends in sports- and recreation-related traumatic brain injuries treated in US emergency departments: The National Electronic Injury Surveillance System—All Injury Program (NEISS-AIP) 2001–2012. Journal of Head Trauma Rehabilitation. 2015;30:185–197. doi: 10.1097/HTR.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin DJ, Zonfrillo MR, Master CL, Arbogast KB, Grady MF, Robinson RL, … Wiebe DJ. Characteristics of prolonged concussion recovery in a pediatric subspecialty referral population. Journal of Pediatrics. 2014;165:1207–1215. doi: 10.1016/j.jpeds.2014.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curaudeau GA, Sharma N, Rovin RA. Development of an iPhone application for sideline concussion testing. Neurosurgical Focus. 2011;31(5):E4. doi: 10.3171/2011.8.FOCUS11186. [DOI] [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham R, Rivara FP, Ford MA, Spicer CM. Sports-related concussions in youth: Improving the science, changing the culture. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- Guskiewicz KM, McCrea M, Marshall SW, Cantu RC, Randolph C, Barr W, … Kelly JP. Cumulative effects associated with recurrent concussion in collegiate football players: The NCAA concussion study. Journal of the American Medical Association. 2003;290:2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- Höffler TN, Leutner D. Instructional animation versus static pictures: A meta-analysis. Learning and Instruction. 2007;17:722–738. [Google Scholar]
- Iverson GL, Echemendia RJ, LaMarre AK, Brooks BL, Gaetz MB. Possible lingering effects of multiple past concussions. Rehabilitation Research and Practice. 2012 doi: 10.1155/2012/316575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabali HK, Irigoyen MM, Nunez-Davis R, Budacki JG, Mohanty SH, Leister KP, Bonner RL. Exposure and use of mobile media devices by young children. Pediatrics. 2015;136:1044–1050. doi: 10.1542/peds.2015-2151. [DOI] [PubMed] [Google Scholar]
- Kato PM, Cole SW, Bradlyn AS, Pollock BH. A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics. 2008;122:e305–e317. doi: 10.1542/peds.2007-3134. [DOI] [PubMed] [Google Scholar]
- Keightley ML, Côté P, Rumney P, Hung R, Carroll LJ, Cancelliere C, Cassidy JD. Psychosocial consequences of mild traumatic brain injury in children: Results of a systematic review by the International Collaboration on Mild Traumatic Brain Injury Prognosis. Archives of Physical Medicine and Rehabilitation. 2014;95:S192–S200. doi: 10.1016/j.apmr.2013.12.018. [DOI] [PubMed] [Google Scholar]
- Kroshus E, Gillard D, Haarbauer-Krupa J, Goldman R, Bickham D. Talking with young children about concussions: An exploratory study. Child: Care, Health and Development. 2016;43:758–767. doi: 10.1111/cch.12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L, Liu J. The effect of pediatric traumatic brain injury on behavioral outcomes: A systematic review. Developmental Medicine & Child Neurology. 2013;55:37–45. doi: 10.1111/j.1469-8749.2012.04414.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin AC, Salzman GA, Bachman SL, Burke RV, Zaslow T, Piasek CZ, … Upperman JS. Assessment of parental knowledge and attitudes toward pediatric sports-related concussions. Sports Health. 2015;7:124–129. doi: 10.1177/1941738115571570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Li L. Parent-reported mild head injury history and behavioural performance in children at 6 years. Brain Injury. 2013;27:1263–1270. doi: 10.3109/02699052.2013.804205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llewellyn T, Burdette GT, Joyner AB, Buckley TA. Concussion reporting rates at the conclusion of an intercollegiate athletic career. Clinical Journal of Sport Medicine. 2014;24:76–79. doi: 10.1097/01.jsm.0000432853.77520.3d. [DOI] [PubMed] [Google Scholar]
- Mannings C, Kalynych C, Joseph MM, Smotherman C, Kraemer DF. Knowledge assessment of sports-related concussion among parents of children aged 5 years to 15 years enrolled in recreational tackle football. Journal of Trauma and Acute Care Surgery. 2014;77(3 Suppl 1):S18–S22. doi: 10.1097/TA.0000000000000371. [DOI] [PubMed] [Google Scholar]
- McKinlay A, Bishop A, McLellan T. Public knowledge of “concussion” and the different terminology used to communicate about mild traumatic brain injury (MTBI) Brain Injury. 2011;25:761–766. doi: 10.3109/02699052.2011.579935. [DOI] [PubMed] [Google Scholar]
- Meehan WP, Mannix RC, O’Brien MJ, Collins MW. The prevalence of undiagnosed concussions in athletes. Clinical Journal of Sport Medicine. 2013;23:339–342. doi: 10.1097/JSM.0b013e318291d3b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montano DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. 3. San Francisco, CA: Jossey-Bass; 2015. [Google Scholar]
- Morrongiello BA, Cusimano M, Orr E, Barton B, Chipman M, Tyberg J, … Bekele T. School-age children’s safety attitudes, cognitions, knowledge, and injury experiences: How do these relate to their safety practices? Injury Prevention. 2008;14:176–179. doi: 10.1136/ip.2007.016782. [DOI] [PubMed] [Google Scholar]
- Murphy R, Penuel WR, Means B, Korbak C, Whaley A, Allen JE. E-DESK: A review of recent evidence on the effectiveness of discrete educational software. Palo Alto, CA: SRI International; 2002. [Google Scholar]
- The NPD Group. Over half of children now using smart devices. 2013 Retrieved from https://www.npd.com/wps/portal/npd/us/news/press-releases/over-half-of-children-now-using-smart-devices/
- Piaget J. Cognitive development in children: Piaget: Development and learning. Journal of Research in Science Teaching. 2003;40:S8–S18. [Google Scholar]
- Prins M, Giza CC. Repeat traumatic brain injury in the developing brain. International Journal of Developmental Neuroscience. 2012;30:185–190. doi: 10.1016/j.ijdevneu.2011.05.009. [DOI] [PubMed] [Google Scholar]
- Sarmiento K, Hoffman R, Dmitrovsky Z, Lee R. A 10-year review of the Centers for Disease Control and Prevention’s HEADS UP initiatives: Bringing concussion awareness to the forefront. Journal of Safety Research. 2014;50:143–147. doi: 10.1016/j.jsr.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer B, Smith P. Serious games taxonomy. Slides from the Serious Games Summit at the Game Developers Conference.2008. [Google Scholar]
- Stewart TC, Gilliland J, Fraser DD. An epidemiologic profile of pediatric concussions: Identifying urban and rural differences. Journal of Trauma and Acute Care Surgery. 2014;76:736–742. doi: 10.1097/TA.0b013e3182aafdf5. [DOI] [PubMed] [Google Scholar]
- Tate R, Haritatos J, Cole S. HopeLab’s approach to remission. 2009 Retrieved from https://dmlcentral.net/wp-content/uploads/files/tate-2009.pdf.
- Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR: Morbidity and Mortality Weekly Report. 2017;66(9):1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HG, Orchinik LJ, Minich N, Dietrich A, Nuss K, Wright M, … Yeates KO. Symptoms of persistent behavior problems in children with mild traumatic brain injury. Journal of Head Trauma Rehabilitation. 2015;30:302–310. doi: 10.1097/HTR.0000000000000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Pittsburgh Medical Center. How knowledgeable are Americans about concussions? Assessing and recalibrating the public’s knowledge. 2016 Retrieved from http://rethinkconcussions.upmc.com/wp-content/uploads/2015/09/harris-poll-report.pdf.
- Zin NAM, Jaafar A, Yue WS. Digital game-based learning (DGBL) model and development methodology for teaching history. WSEAS Transactions on Computers. 2009;8:322–333. [Google Scholar]