Abstract
Decision fatigue is an applicable concept to healthcare psychology. Due to a lack of conceptual clarity, we present a concept analysis of decision fatigue. A search of the term “decision fatigue” was conducted across seven research databases, which yielded 17 relevant articles. The authors identified three antecedent themes (decisional, self-regulatory, and situational) and three attributional themes (behavioral, cognitive, and physiological) of decision fatigue. However, the extant literature failed to adequately describe consequences of decision fatigue. This concept analysis provides needed conceptual clarity for decision fatigue, a concept possessing relevance to nursing and allied health sciences.
Introduction
It is estimated that an American adult makes 35,000 decisions a day (Sollisch 2016). While some of these day-to-day decisions are seemingly benign, an emerging body of science indicates that making decisions may possess negative ramifications for controlling ones’ behavior and the quality of subsequent decisions. This phenomenon, known as decision fatigue, describes the impaired ability to make decisions and control behavior as a consequence of repeated acts of decision-making. Evidence suggests that individuals experiencing decision fatigue demonstrate an impaired ability to make trade-offs, prefer a passive role in the decision- making process, and often make choices that seem impulsive or irrational (Tierney 2011).
The concept of decision fatigue is derived from the Strength Model of Self-Control posited by Baumeister, Bratslavsky, Muraven, & Tice (1998). A central tenet of their model is that humans have a limited capacity to regulate their behavior. Akin to muscle fatigue after exertion, humans deplete internal resources when performing acts of self-regulation, such as processing information to formulate a decision. The depleted state of internal resources (executive function, emotion regulation) is referred to as ego depletion (Baumeister et al., 1998). Evidence from Vohs et al. (2008) suggests that making decisions can elicit ego depletion. Our understanding of the literature suggests that decision fatigue is a symptom or phenotypic expression of ego-depletion; therefore, individuals in states of ego-depletion are at risk of experiencing the cognitive, psychological, and behavioral manifestations associated with decision fatigue.
In addition to the Strength Model of Self-Control, Inzlicht & Schmeichel (2012) propose a Process Model of Ego-Depletion. This model posits that the ego-depletion effect is the result of alterations to attentional regulation and behavioral motivation. Specifically, symptoms of ego-depletion (i.e., decision fatigue) result from motivational shifts that potentiate impulsivity and attentional deficits that detract from one’s ability to recognize internal conflicts or discrepancies that would normally indicate behavior modification. This model possesses ample theoretical evidence, yet requires further empirical testing for its subsequent validation; nonetheless, it may serve as a suitable alternative to the underlying mechanisms of decision fatigue.
Decision-making is a central component of modern health care. Nurses and physicians make numerous decisions each day, with each decision possessing some level of influence on patient outcomes (Bakalis & Watson 2005; Thompson et al. 2013). Thus, there is an emerging body of science exploring the decision-making process of healthcare providers and how to enhance clinician decision-making to ensure optimal outcomes for patients (Patel et al. 2002). With the recent advent of a shared decision-making framework within health care, clinicians, patients, and family members collaborate as a unit for the sake of health promotion and maintenance (Elwyn et al. 2012). In addition, with half of all adults possessing at least one chronic condition, decision-making is a central facet of day-to-day chronic disease self-management (Ryan and Sawin, 2009).
Accordingly, the National Institute of Nursing Research’s (NINR) most recent strategic plan (2016–2020) emphasizes the need for scientific advancement in the domain of decision science; specifically, the NINR calls for the development of interventions to address “variations in cognitive function/decision-making to improve self-management behaviors…” (The NINR Stategic Plan, 2016, p.57). To promote such advancement, nurse scientists must expand upon current models of decision-making and explore emerging concepts and theoretical models. Possessing ample theoretical and empirical support from the psychological literature, decision fatigue may serve as a relevant concept of interest for nurse scientists looking to further explore the complexities associated with healthcare decision-making. We hypothesize clinicians experiencing decision fatigue may use practice methods that do not align with evidence-based recommendations; patients experiencing decision fatigue may demonstrate a marked inability to self-manage health conditions; and family members experiencing decision fatigue may make surrogate decisions that do not align with the patient’s preferences.
Despite its potential to inform healthcare science, decision fatigue is a relatively nascent concept with limited application in health care. Before the widespread integration of decision fatigue into novel models of healthcare decision-making, an exploration of its evolution as a concept is warranted. The purpose of this concept analysis is to explore the current application of decision fatigue and provide clarity of its use as a concept. Conceptual clarification will provide consistency for developing models of healthcare decision-making and assist in the determination of decision fatigue as relevant concept of concern.
Methods
Literature Review
A literature search was performed to identify instances of decision fatigue within academic literature by author GP. Seven databases were queried (Academic Search Complete, CINAHL Plus with Full Text, MEDLINE with Full Text, PsycINFO, PsycNET, and PubMed) in May 2017 for the phrase “decision fatigue.” Sources were excluded if they were not published in English. Additionally, the lead author performed an ancillary search of the reference sections of the articles identified through these sources for titles that also contained decision fatigue. The authors acknowledge that additional materials possessing relevance for this analysis may have arisen after the initial literature review, and may have been excluded from this concept analysis.
Methodology
Because decision fatigue is a concept that is still emerging, we used Rodgers' (1989) evolutionary concept analysis methodology. Compared to the Walker & Avant (2005) concept analysis procedures, Rodgers (1989) imposes less constraint on the analysis of the concept in question. Using an iterative process that provides a foundation for subsequent development of the concept, the Rodgers (1989) evolutionary model accounts for the constantly evolving nature of a concept and seeks to understand the common use of the concept in question. After identification of a concept of interest, Rodgers (1989) evolutionary concept analysis involves reviewing the existing literature for conceptual definitions, the identification of surrogate terms (i.e., other words or concepts that mean the same or similar thing as the concept in question), antecedents (i.e., events that precede the concept), attributes (i.e., characteristics of the concept), examples of the concept, and consequences (i.e., the events resulting from the concept) (Tofthagen & Fagerstrøm 2010). Author GP provided the initial recommendations for antecedents, attributes, examples, and consequences. The co-authors (RM and RH) reviewed the selected articles to ascertain the validity of the suggested conceptual entities.
Findings
Prevalence and Definitions
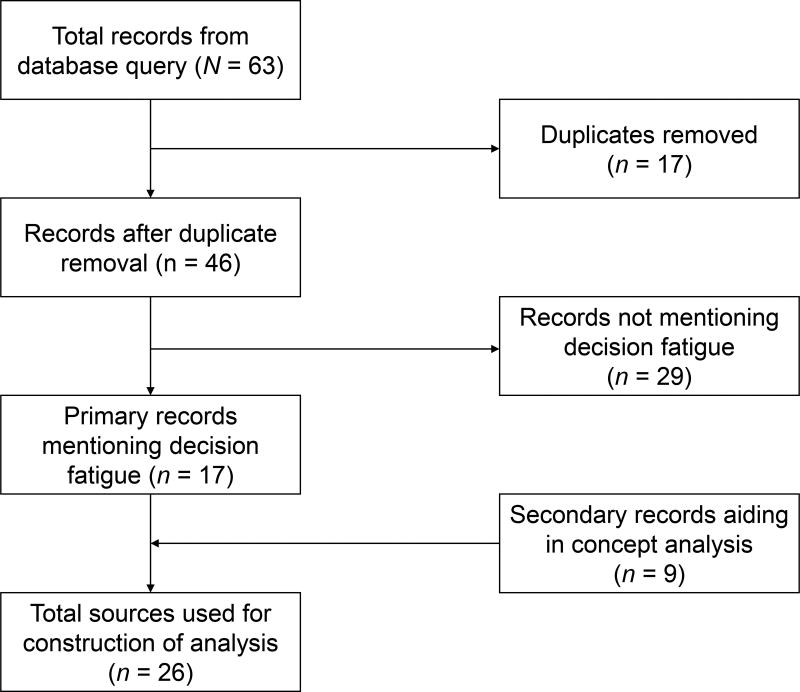
A search of the seven databases for “decision fatigue” yielded 63 potential sources for analysis (Figure 1). Of the 63 original sources, 17 were duplicated at least once. Of the remaining 46 original sources, 29 of the sources did not mention decision fatigue within the title, abstract, or main body – thus, they were excluded from the analysis. Of the remaining 17 sources, decision fatigue was mentioned 99 times. Notably, three sources accounted for 43% of the instances in which decision fatigue was mentioned (Olsen et al. 2017; Polman & Vohs 2016; Tierney 2011). Eight of the original sources were periodicals, news articles, or editorials; the remaining nine sources were peer-reviewed and published in academic journals, of which four were healthcare-related (Kwan et al. 2016; Palinkas et al. 2017; Oto 2012; Riedel & Colao 2014). However, despite the high prevalence in which decision fatigue was mentioned, little effort was made in the process of providing a concise definition; instead, authors commonly relied on attributional qualities to describe the experience of decision fatigue (Table 1). Furthermore, despite providing descriptions of decision fatigue, none of articles in Table 1 made an attempt to operationalize decision fatigue. Furthermore, a detailed review of the primary articles referenced nine secondary sources that aided in the construction of this concept analysis (Vohs et al. 2006; Augenblick & Nicholson 2016; Pocheptsova et al. 2009; Wang et al. 2010; Levav et al. 2010; Kouchaki & Smith 2014; Linder et al. 2014; Chan et al. 2009; Baldwin & Daugherty 2004).
Figure 1.
Visual representation of decision fatigue database query.
Table 1.
Descriptions of decision fatigue in the queried literature
| Author | Description of decision fatigue |
|---|---|
| Bartlett (2015, p. 1) | “Some decisions are minor… Some decisions are much more complex and consequential” |
| Halamka (2011, p. 40) | “… that numbness you feel at the end of an overloaded day, after you’ve decided how much to spend, whom to hire and what to do, over and over.” |
| Hosp (2012, p. 3) | “… the processes used to make choices, ranging from seemingly simple… to more complex… are similar to using a muscle… the more decisions we make, the more those processes get fatigued and the more difficulty we have making decisions.” |
| Kwan et al. (2016, p. 1) | “… reviewing manuscripts can be an arduous and time-consuming process, making editors susceptible to a particular source of bias: decision fatigue.” |
| McDonnell (2016, p. 10) | “… human beings can make only so many high-quality decisions per day. After a while, we develop ‘decision fatigue’.” |
| Olsen et al. (2017, pp. 497–498) | “… making choices requires a cognitive effort. Since cognitive capacity is limited, making choices may thus lead to decision fatigue.” |
| Oto (2012, p. 46) | “No matter how smart or diligent we are, our ability to make good decisions eventually runs out.” |
| Polman & Vohs (2016, p. 471) | “… the limited reserve of stamina for decision-making becomes drained, which leads to poor self-control subsequently.” |
| Stewart et al. (2012, p. A5) | “… human beings have a limited reserve of stamina for decision-making that depletes gradually throughout the day as we navigate our lives.” |
| Sollisch (2016, p. 1) | “… the draining of will that comes from the act of decision-making” |
| Tierney (2011, p. 33) | “No matter how rational and high-minded you try to be, you can’t make decision after decision without paying a biological price… The more choices you make throughout the day, the harder each one becomes for your brain, and eventually it looks for shortcuts…” |
Surrogate Terms
Our review of the literature revealed additional concepts that may be related to decision fatigue. These concepts include ego depletion (Baumeister et al., 1998) and mental fatigue (Lorist et al. 2000). While conceptually related, these concepts are distinctly different from decision fatigue. Ego depletion describes the state of a depleted central executive (executive functioning), during which individuals are prone to experience decision fatigue. Notably, ego depletion is a higher-order construct that may manifest as decision fatigue. Mental fatigue describes the impaired ability to use cognitive processing; thus, individuals experiencing decision fatigue may feel mentally fatigued. However, decision fatigue also incorporates the impaired ability to regulate and experience emotions. Moreover, Augenblick & Nicholson (2016) describe “choice fatigue,” which they define as when “the pure act of decision-making [is]… exhausting or effort-consuming” (p.460). Upon further exploration, the authors deem choice fatigue as a uniquely coined surrogate term for decision fatigue. In addition, Riedel & Colao (2014, p. TAHP-8) state that decision fatigue is synonymous with the term “choice overload,” which the authors did not come across in any other queried sources.
Antecedents
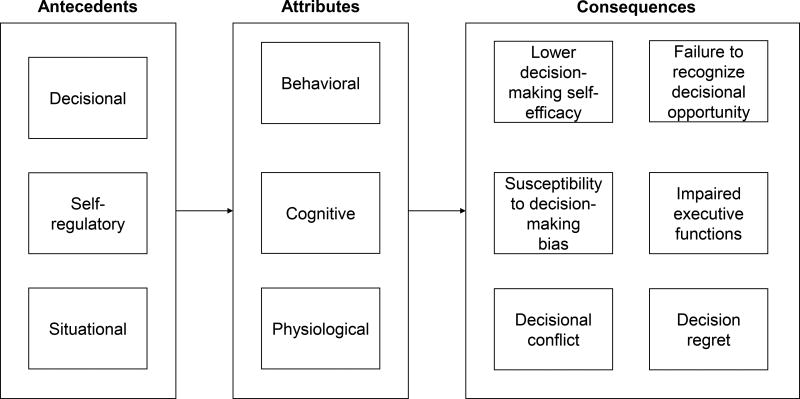
Identifying the antecedents to decision fatigue is a relevant and necessary component of this concept analysis, as it may serve as a basis for future research and targeted intervention. The authors identified three themes when evaluating the literature for antecedents to decision fatigue: decisional, self-regulatory, and situational.
Decisional antecedents
Having made a series of previous decisions was a salient antecedent to the development of decision fatigue. A series of empirical studies indicated that when individuals were subjected to making a series of choices, it predisposed them to the sequelae of decision fatigue. These results were consistent across investigators and settings, regardless of whether the investigation occurred in a controlled laboratory setting or in ecologically valid environments. For example, decision fatigue was demonstrated among college students making consumer goods purchase choices (Vohs et al., 2008), judges performing multiple parole hearings (Danziger et al. 2011), journal editors reviewing submitted manuscripts (Stewart et al. 2012), and air traffic control workers (Orasanu et al. 2012). In each instance, individuals were predisposed to decision fatigue because of experimental design or situational demand when they took part in repeated acts of decision- making. However, a notable distinction, highlighted by Vohs et al. (2008), claims that the actual process of making decisions—not just deliberating on available options—was associated with a greater degree of decision fatigue. Moreover, Oto (2012) states that as the complexity or difficulty of a decision rises, the more decision fatigue an individual will experience.
Self-regulatory antecedents
Defined as one’s capacity to alter his or her behavior, performing acts of self-regulation was a common antecedent to the expression of decision fatigue (Baumeister & Heatherton, 1996). Broadly speaking, self-regulation refers to the maintenance and control of one’s executive functions and emotions (Diamond 2013; Lerner et al. 2015). Consistent with this definition, the literature consistently identified that partaking in acts of self-regulation predicted the manifestation of decision fatigue. For example, directed effort to regulate one’s attention (Gilbert et al. 1988), emotion, thoughts, and self-control contributed to the development of decision fatigue (Baumeister, Bratslavsky, Muraven, & Tice, 1998; Muraven, Tice, & Baumeister, 1998).
Situational antecedents
Our review of the literature also identified several key situational antecedents that were commonly predictive of decision fatigue. The first situational antecedent relates to the time of day. An investigation by Sievertsen, Gino, & Piovesan (2016) revealed that the time of day was associated with decision fatigue among students taking standardized tests, with students performing poorer as the day progressed. These results are supported by findings from Kouchaki & Smith (2014), who reported that decision-making was dependent on time of day; specifically, moral decisions decreased as the day progressed. Similar findings were also observed within healthcare domains: gastroenterologists’ decision-making related to polyp identification during colonoscopies was dependent on the time of day (Chan et al. 2009); moreover, the time of day predicted a physician’s likelihood to prescribe an antibiotic, even if it was not indicated (Kemper 2015).
Related to time of day, circulating levels of blood glucose and physiologic predisposition to efficient glucose metabolism is implicated in the development of decision fatigue (Gailliot & Baumeister 2007). Decision-making by judges during parole hearings significantly varied before and after a lunch break period (Danziger et al. 2011). An additional situational antecedent related to time of day and blood glucose levels implicated in the development of decision fatigue is physiological fatigue. Specifically, sleep deprivation and physiological fatigue are implicated in impaired decision-making (Harrison & Horne 2000). This is readily apparent for healthcare workers, who often work long and nontraditional hours. Thus, sleep deprivation and fatigue are largely implicated in the manifestation of decision fatigue among nurses and physicians (Baldwin & Daugherty 2004; Scott et al. 2014).
Attributes
The authors identified three themes that are recognized as attributes of decision fatigue. These themes that emerged were classified as behavioral, cognitive, and physiological attributes, which are described in detail in the following text:
Behavioral attributes
The most common attribute of decision fatigue relates to behavioral attributes. Often, these behavioral attributes reflect an underlying state of ego depletion and symbolize an unconscious method in which individuals alter their behavior when making decisions to prevent further ego depletion. For example, individuals experiencing decision fatigue are more prone to avoidant behaviors; a study from Vohs et al. (2008) found that the process of making choices was associated with increased procrastination tendencies. In addition to procrastinating, individuals experiencing decision fatigue demonstrate passive behavior during subsequent decision-making, and this passivity can even reach the point where individuals simply choose to not act (Palinkas et al., 2017.; Riedel & Colao, 2014). Apart from avoidant or passive behaviors, individuals experiencing decision fatigue demonstrate less persistence; thus, they are prone to choosing a default option when provided with a series of options (Riedel & Colao, 2014; Tierney, 2011; Vohs et al., 2008).
Individuals who are experience decision fatigue may also be prone to impulsive behavior and decision-making (Tierney 2011). Thus, there is a diverse spectrum of decision-making behaviors that may be anticipated from those experiencing decision fatigue—one may act impulsively, delay action, not act at all, or simply choose a default option. Moreover, not only are our behavioral propensities altered during states of decision fatigue, but our experience of our emotions is altered as well (Bruyneel et al. 2006). As Tierney (2011, p. 33) claims, decision fatigue can cause one to “experience things more intensely… frustrations seem more irritating than usual.”
Cognitive attributes
In addition to behavioral alterations related to decision fatigue, the reviewed body of evidence suggests that individuals experiencing alterations in cognitive functioning. For example, Vohs et al. (2008) reported that college students experiencing decision fatigue spent more time completing and performed worse on a math test than students who were not experiencing decision fatigue. The disparate performance in quantitative skills is consistent with Baumeister, Vohs, & Tice's (2007) Strength Model of Self-Control, as quantitative function is largely dependent on executive functioning (Cragg & Gilmore 2014). Furthermore, decision fatigue not only reduces executive functioning, but it also inhibits reasoning ability. Individuals who make decisions and experience decision fatigue are more susceptible to the use of cognitive heuristics – i.e., a mental shortcut. For example, individuals required to make decisions in states of decision fatigue are prone to rely on heuristics that may bias decision making – potentially resulting in decisions that yield undesirable outcomes (Pocheptsova et al. 2009).
Physiological attributes
In addition to the debilitating effects decision fatigue has on behavioral, emotional, and cognitive function, there is evidence suggesting that individuals experiencing decision fatigue suffer from a subsequent deterioration in physical endurance. In a series of laboratory studies by Vohs et al. (2006; 2008), research participants who made a series of choices about shopping for consumer goods or college courses demonstrated decreased physical endurance than subjects who did not make choices when subjected to the cold pressor test – which evaluates the length of time an individual can withstand the discomfort of having their hand submerged in ice-water. (von Baeyer et al. 2005; Schwabe et al. 2008). In short, purposeful tolerance of physical stressors can induce ego-depletion, which may manifest as decision fatigue.
Consequences
Our review of the literature identified a salient deficiency regarding the identification of decision fatigue consequences, as the majority of studies involving decision fatigue described what we have identified as attributes (e.g., impulsivity, passivity, avoidance, diminished executive function, and less physiological endurance). Acknowledging that decision-making is a process, decision fatigue can theoretically manifest during, and influence any point of, the decision-making process. Therefore, it is important to consider the potential influence of decision fatigue on decision-making before, during, and after the decision-making process.
Decision-making deliberation
Two key components of Baumeister and Heatherton's (1996) explication of the self-regulation process involves the identification of standards (i.e., identification of a goal) and monitoring (i.e., recognizing the position of one in relation to an idealized goal). Moreover, Baumeister and Heatherton (1996) attribute ego depletion as a primary determinant of self-regulation failure (i.e., failure to establish standards or monitor behavior). Therefore, it is not unreasonable to suggest that individuals experiencing decision fatigue as a consequence of ego depletion may fail to recognize that a decision needs to be made or be unable to clarify and articulate a desired decisional outcome. Considering the tendency for individuals experiencing decision fatigue to demonstrate avoidant or passive behaviors, a decisionally fatigued individual who cannot engage through the remaining steps of the decision-making process may experience diminished decision-making self-efficacy— a decreased belief in one’s ability to engage in decision-making. This hypothesis is theoretically consistent with Bandura's (1977) self-efficacy theory, as self-efficacy for a particular behavior is developed through the execution of the behavior in question (Ryan & Sawin 2009).
As discussed, individuals experiencing decision fatigue often rely on particular heuristics or biases to guide their decision-making; this is hypothesized to reflect an unconscious desire to prevent further ego depletion (Tierney 2011). However, the use of heuristics and other cognitive-sparing efforts are associated with what Hsee, Yu, Zhang, & Zhang (2003) describe as psychological myopia, the tendency of an individual to focus on information immediately related to a decision and ignore background information (despite its potential pertinence). Therefore, individuals experiencing decision fatigue may fail to recognize all the potential alternatives of the decision they’re facing; furthermore, individuals experiencing psychological myopia may weigh alternatives in such a manner that potential losses are disproportionately valued over potential gains (Thaler et al. 1997). Thus, individuals experiencing decision fatigue may be subject to debilitating bias when evaluating or deliberating over a course of action.
Moreover, because individuals experiencing decision fatigue may be unaware of all potential options, demonstrate bias when comparing alternatives to one another, and experience the burden of decision-making more intensely, it is reasonable to suggest that they also may experience a greater degree of decisional conflict (O’Connor 1994). Described as a state of uncertainty about a potential course of action, decisional conflict’s characteristics align closely with those of decision fatigue; those experiencing decisional conflict express doubt and avoidance. Of note, experiencing decisional conflict when deliberating the course of a decision is significantly correlated with experiencing decision regret, a profoundly negative cognitive and emotional phenomenon indicative of the thought or realization that a situation would be appraised as more desirable if an alternative course of action had been taken after the decision is made (Brehaut et al. 2003; Zeelenberg 1999) (Hickman, Daly, & Lee, 2012).
Decision planning and execution
Theoretical evidence suggests the ego depletion experienced by those suffering from decision fatigue may result in a detriment to the executive functions related to planning and execution of a decision. A higher-order executive function, planning requires complex coordination of lower-order executive functions such as working memory, attention, and cognitive flexibility (Diamond 2013). Moreover, neuroscience imaging studies suggest that during periods of intense emotional regulation, such as during decision fatigue, cortices of the brain involved in reasoning and decision-making are less active (Heatherton & Wagner 2011). Therefore, individuals in states of decision fatigue may experience an impaired ability to incorporate the necessary executive functions to sufficiently plan for a choice of action. Furthermore, attributes of decision fatigue such as decision avoidance, passivity, and impulsivity are related to the available options to consider when evaluating a choice of action. If an individual delays action through passivity and avoidance, potential options for a decision may no longer be available; but conversely, delaying action may possibly allow other options to become available. In addition, the impulsive behavior attributed with decision fatigue may prevent an individual from being aware of or thoroughly evaluating each potential option, resulting in the execution of a decision that results in an undesirable outcome. Regardless of attributional behavior (i.e., passivity or impulsivity), the execution of a suboptimal decision due to failure to evaluate all available options may potentiate the development of decision regret (Brehaut et al. 2003; Zeelenberg 1999).
Discussion
This concept analysis provides needed clarification for an emerging concept of decision fatigue, which is well described within the psychological literature (Bruyneel et al., 2006; Vohs et al., 2008), with subsequent application in other disciplines, such as consumer science (Bruyneel et al. 2006), technology (Halamka 2011), business (Sollisch 2016), and behavioral economics (Riedel & Colao 2014). Our review of the literature allowed for the identification of several antecedents (i.e., decisional, self-regulatory, and situational) and attributional themes (i.e., behavioral, cognitive, and physiological). The identification of the antecedents and attributional themes serve as useful precursors for the development of future theoretical frameworks for the exploration of decision fatigue. Acknowledging the significant lack of documented consequences of decision fatigue, the authors attempted to synthesize the existing theoretical and empirical literature to identify outcome variables influenced by the existence of decision fatigue (Figure 2).
Figure 2.
Decision fatigue antecedents, attributes, and consequences.
Notably, decision fatigue as a concept has been scantly applied to nursing science and other allied healthcare disciplines, despite its potential relevance to inform the decision-making behaviors of nurses, patients, and other clinicians. This in part may be related to the fact that past measurements of decision fatigue are inconsistent as they have been dependent on the observation of secondary tasks related to self-control (Vohs et al. 2008), judges’ rulings on cases throughout the day, editors’ tendency to reject journal articles (Stewart et al. 2012), and decisions made by air traffic control workers (Orasanu et al. 2012). This inconsistency in measurement limits generalizability of findings. In response, Hickman and colleagues (2016) presented the first known psychometrically sound self-report measure of decision fatigue. With the introduction of this valid and reliable measure, future inquiries involving the investigation of decision fatigue are strengthened, as decision fatigue can be conceptually triangulated to Hickman et al.’s (2016) measure and previously used secondary tasks.
With this newly developed instrument that captures the phenomenon of decision fatigue, nurse scientists can now begin to incorporate decision fatigue into existing models of healthcare behavior; moreover, serving as an indicator of ego depletion, this instrument allows for the development and application of innovative frameworks which incorporate Baumeister, Vohs, & Tice's (2007) Strength Model of Self-Control, a framework with limited application to healthcare models of decision-making. Furthermore, existing models of self-management theory (Lorig & Holman 2003; Ryan & Sawin 2009) fail to account for the limited decision-making capacity of humans; thus, this concept analysis serves as an impetus for the subsequent improvement of commonly used theoretical models that inform healthcare delivery and patient care.
This concept analysis also possesses implications for nursing practice. It is well known that nurses face a large number of decisions each day, all of which strongly influence the outcomes of patients and their family members (Thompson et al. 2004; Thompson & Yang 2009). Furthermore, as the American population continues to age, the demand for nurses is increasing substantially, but unfortunately, this demand is not being met. Thus, nurses face a greater workload and encounter more responsibility than ever before and often work to the point of and through exhaustion (Carayon & Gurses 2008; Rogers 2008).
Although not currently explored, decision fatigue may serve as an indicator of workload burden associated with the delivery of nursing care. Moreover, the application of decision fatigue is not solely limited to nurses, as the workload and decision fatigue of resident physicians is well-documented (Baldwin & Daugherty 2004; Berlin 2008; Thomas 2004). If nurses, physicians, and other healthcare clinicians are working to the point where they are in severe states of ego-depletion (manifesting as decision fatigue) and are in an unideal cognitive state to make logical and safe decisions for patients, the exploration of decision fatigue may serve as a highly relevant and necessary endeavor. Therefore, decision fatigue may possess significance to inform regulatory policies related to the healthcare employee workload.
Limitations
This concept analysis possesses several limitations. First, it is possible that the authors failed to capture every use of decision fatigue within the existing literature; however, to address this potential limitation, the authors conducted a thorough search of seven academic databases and performed an ancillary review of reference lists when appropriate. Moreover, the application of decision fatigue to models of healthcare decision-making has only recently come into existence; thus, when identifying potential consequences of decision fatigue, the authors were forced to use logical and theoretical support to justify the hypothesized consequences. Nevertheless, the lack of empirical evidence highlights an opportunity for future exploration and development of decision fatigue as a concept. Furthermore, despite a meta-analysis by Hagger, Wood, Stiff, & Chatzisarantis (2010) supporting the existence of the ego depletion effect, subsequent analyses by other scholars call into question the theoretical and empirical validity of the ego-depletion phenomenon (Carter et al. 2015). Because there isn’t conclusive evidence which confirms nor refutes the strength model of self-control, we suggest subsequent empirical testing of the model. Should overwhelming evidence support its refutation, the process model of ego-depletion serves a theoretically valid and logical paradigm by which to further evaluate the seemingly limited capacity humans possess to control their behavior.
In addition, we must acknowledge the potential source of bias imparted by the authors previous use and application of the decision fatigue concept. Thus, it is possible that our appreciation, understanding, and application of decision fatigue inherently influenced the development of this work. Also since the primary literature search was conducted by author GP, the article selection process was potentially biased, which may have unduly influenced the identification of the concept’s antecedents, consequences, and attributes. Additionally, only including articles that were published in English provides another source of bias, as it limited our availability to explore the additional applications of decision fatigue and how its application differs across cultures. Finally, it is possible that subsequent articles related to decision fatigue were released during and after the construction of this analysis that may have further informed our efforts.
Conclusion
This concept analysis indicates decision fatigue is a widespread phenomenon that has yet to be widely applied to healthcare decision-making and behavioral frameworks. The manifestation of decision fatigue is contingent upon several factors related to decision-making, self-regulation, and idiosyncratic scenarios. Moreover, in addition to the psychometrically sound instrument presented by Hickman et al. (2016), this analysis identified several relevant attributes related to alterations in reasoning, behavior, and physiology that serve as useful indicators of decision fatigue. Our analysis was limited by the dearth of consequences related to decision fatigue in the reviewed literature; however, this limitation provides a unique opportunity for scholarly inquiry into the potential outcomes of individuals who make decisions while experiencing decision fatigue. To this end, decision fatigue is a highly relevant concept of interest that possesses ramifications for healthcare science, theory, practice, and policy.
Acknowledgments
The authors would like to acknowledge Matthew McManus for providing editorial assistance with this manuscript.
Financial Disclosure:
This publication was made possible by funding from the National Institute of Nursing Research (NINR; NR014213), a component of the National Institutes of Health (NIH), as well as the Robert Wood Johnson Foundation (RWJF) Nurse Faculty Scholars Program (#72118). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH, NINR, or the RWJF.
References
- Anon The NINR Strategic Plan: Advancing Science, Improving Lives. 2016 doi: 10.1111/jnu.12286. Available at: https://www.ninr.nih.gov/sites/www.ninr.nih.gov/files/NINR_StratPlan2016_reduced.pdf. [DOI] [PubMed]
- Augenblick N, Nicholson S. Ballot position, choice fatigue, and voter behaviour. Review of Economic Studies. 2016;83(2):460–480. [Google Scholar]
- Bakalis NA, Watson R. Nurses' decision-making in clinical practice. Nursing Standard. 2005;19(23):33–39. doi: 10.7748/ns2005.02.19.23.33.c3805. [DOI] [PubMed] [Google Scholar]
- Baldwin DC, Daugherty SR. Sleep deprivation and fatigue in residency training: results of a national survey of first- and second-year residents. Sleep. 2004;27(2):217–23. doi: 10.1093/sleep/27.2.217. [DOI] [PubMed] [Google Scholar]
- Bandura A, SBandura A. Self-efficacy: toward a unifying theory of behavioral change. In: Baumeister RF, editor. Psychological Review. 2. Vol. 84. 1977. pp. 191–215. 1977. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, et al. Ego depletion: is the active self a limited resource? Journal of personality and social psychology. 1998;74(5):1252–1265. doi: 10.1037//0022-3514.74.5.1252. [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Heatherton TF. Self-Regulation Failure: An Overview. Psychological Inquiry Copyright. 1996;7(1):1–15. [Google Scholar]
- Baumeister RF, Vohs KD, Tice DM. The strength model of self-control. Current Directions in Psychological Science. 2007;16(6):351–355. [Google Scholar]
- Baumeister RF, Vohs KD, Tice DM. The Strength Model of Self-Control. Current Directions in Psychological Science. 2007;16(6):351–355. [Google Scholar]
- Berlin L. Liability of the Sleep-Deprived Resident. American Journal of Roentgenology. 2008;190(4):845–851. doi: 10.2214/AJR.07.3311. [DOI] [PubMed] [Google Scholar]
- Brehaut JC, et al. Validation of a decision regret scale. Medical decision making?: an international journal of the Society for Medical Decision Making. 2003;23:281–292. doi: 10.1177/0272989X03256005. [DOI] [PubMed] [Google Scholar]
- Bruyneel S, Dewitte S, Vohs KD, Warlop L. Repeated choosing increases susceptibility to affective product features. International Journal of Research in Marketing. 2006;23(2):215–225. [Google Scholar]
- Carayon P, Gurses AP. Nursing Workload and Patient Safety—A Human Factors Engineering Perspective. Agency for Healthcare Research and Quality (US); 2008. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21328758. [PubMed] [Google Scholar]
- Carter EC, et al. A series of meta-analytic tests of the depletion effect: Self-control does not seem to rely on a limited resource. Journal of Experimental Psychology: General. 2015;144(4):796–815. doi: 10.1037/xge0000083. [DOI] [PubMed] [Google Scholar]
- Chan MY, Cohen H, Spiegel BMR. Fewer Polyps Detected by Colonoscopy as the Day Progresses at a Veteran’s Administration Teaching Hospital. Clinical Gastroenterology and Hepatology. 2009;7(11):1217–1223. doi: 10.1016/j.cgh.2009.07.013. [DOI] [PubMed] [Google Scholar]
- Cragg L, Gilmore C. Skills underlying mathematics: The role of executive function in the development of mathematics proficiency. Trends in Neuroscience and Education. 2014;3(2):63–68. [Google Scholar]
- Danziger S, Levav J, Avnaim-Pesso L. Extraneous factors in judicial decisions. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(17):6889–92. doi: 10.1073/pnas.1018033108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A. Executive functions. Annual review of psychology. 2013;64:135–68. doi: 10.1146/annurev-psych-113011-143750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, et al. Shared decision making: a model for clinical practice. Journal of general internal medicine. 2012;27(10):1361–7. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gailliot MT, Baumeister RF. The physiology of willpower: linking blood glucose to self-control. Personality and social psychology review?: an official journal of the Society for Personality and Social Psychology, Inc. 2007;11(4):303–327. doi: 10.1177/1088868307303030. [DOI] [PubMed] [Google Scholar]
- Gilbert DT, Pelham BW, Krull DS. On cognitive busyness: When person perceivers meet persons perceived. Journal of personality and social psychology. 1988;54(5):733. [Google Scholar]
- Hagger MS, et al. Ego depletion and the strength model of self-control: a meta-analysis. Psychological bulletin. 2010;136(4):495–525. doi: 10.1037/a0019486. [DOI] [PubMed] [Google Scholar]
- Halamka J. Coping With IT Decision Fatigue. Computerworld. 2011;45(17):40–40. [Google Scholar]
- Harrison Y, Horne JA. The impact of sleep deprivation on decision making: a review. J Exp Psychol Appl. 2000;6(3):236–249. doi: 10.1037//1076-898x.6.3.236. Available at: http://www.ncbi.nlm.nih.gov/pubmed/11014055. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Wagner DD. Cognitive neuroscience of self-regulation failure. Trends in Cognitive Sciences. 2011;15(3):132–139. doi: 10.1016/j.tics.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickman R, Pignatiello G, Tahir S. Evaluation of the decisional fatigue scale among surrogate decision makers of the critically ill. Western Journal of Nursing Research. 2017 doi: 10.1177/0193945917723828. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickman RL, Daly BJ, Lee E. Decisional conflict and regret: consequences of surrogate decision making for the chronically critically ill. Applied nursing research?: ANR. 2012;25(4):271–5. doi: 10.1016/j.apnr.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsee CK, Yu F, Zhang J, Zhang Y. Medium maximization. Journal of Consumer Research. 2003;30(1):1–14. [Google Scholar]
- Inzlicht M, Schmeichel BJ. What Is Ego Depletion? Toward a Mechanistic Revision of the Resource Model of Self-Control. Perspectives on Psychological Science. 2012;7(5):450–463. doi: 10.1177/1745691612454134. [DOI] [PubMed] [Google Scholar]
- Kemper CA. Updates. Infectious Disease Alert. 2015;34(5):57–59. [Google Scholar]
- Kouchaki M, Smith IH. The morning morality effect: the influence of time of day on unethical behavior. Psychological science. 2014;25(1):95–102. doi: 10.1177/0956797613498099. [DOI] [PubMed] [Google Scholar]
- Kwan J, et al. Does “Decision Fatigue” Impact Manuscript Acceptance? An Analysis of Editorial Decisions by the American Journal of Gastroenterology. The American Journal of Gastroenterology. 2016;111(11):1511–1512. doi: 10.1038/ajg.2016.452. [DOI] [PubMed] [Google Scholar]
- Lerner J, et al. Emotion and decision making. Psychology 66. 2015;45(1–3):133–155. doi: 10.1146/annurev-psych-010213-115043. [DOI] [PubMed] [Google Scholar]
- Levav J, et al. Order in Product Customization Decisions: Evidence from Field Experiments. Journal of Political Economy. 2010;118(2):274–299. [Google Scholar]
- Linder JA, et al. Time of Day and the Decision to Prescribe Antibiotics. JAMA Internal Medicine. 2014;174(12):2029. doi: 10.1001/jamainternmed.2014.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Annals of behavioral medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- Lorist MM, et al. Mental fatigue and task control: Planning and preparation. Psychophysiology. 2000;37(5):614–625. [PubMed] [Google Scholar]
- Muraven M, Tice DM, Baumeister RF. Self-control as limited resource: regulatory depletion patterns. Journal of personality and social psychology. 1998;74(3):774–789. doi: 10.1037//0022-3514.74.3.774. [DOI] [PubMed] [Google Scholar]
- O’Connor aM. Validation of a decisional conflict scale. Medical decision making?: an international journal of the Society for Medical Decision Making. 1994;15(1):25–30. doi: 10.1177/0272989X9501500105. [DOI] [PubMed] [Google Scholar]
- Olsen SB, Olsen SB, Meyerhoff J, Meyerhoff J, Mørkbak MR, Mørkbak MR, Bonnichsen O. The influence of time of day on decision fatigue in online food choice experiments. British Food Journal. 2017;119(3):497–510. [Google Scholar]
- Orasanu J, Parke B, Kraft N, Tada Y, Hobbs A, Anderson B, McDonnell L, Dulchinos V. Evaluating the Effectiveness of Schedule Changes for Air Traffic Service (ATS) Providers: Controller Alertness and Fatigue Monitoring Study (No. DOT/FAA/HFD-13/001) 2012 [Google Scholar]
- Oto B. When thinking is hard: managing decision fatigue. EMS world. 2012;41(5):46–50. [PubMed] [Google Scholar]
- Palinkas LA, et al. Adoption of innovative and evidence-based practices for children and adolescents in state-supported mental health clinics: a qualitative study. Health research policy and systems. 2017;15(1):27. doi: 10.1186/s12961-017-0190-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel VL, Kaufman DR, Arocha JF. Emerging paradigms of cognition in medical decision-making. Journal of biomedical informatics. 2002;35(1):52–75. doi: 10.1016/s1532-0464(02)00009-6. [DOI] [PubMed] [Google Scholar]
- Pocheptsova A, et al. Deciding Without Resources: Resource Depletion and Choice in Context. Journal of Marketing Research. 2009;46(3):344–355. [Google Scholar]
- Polman E, Vohs KD. Decision Fatigue, Choosing for Others, and Self-Construal. Social Psychological and Personality Science. 2016;7(5):471–478. [Google Scholar]
- Riedel J, Colao R. Change is hard: The promise of behavioral economics. American Journal of Health Promotion. 2014;28(6):TAHP8–TAHP11. [PubMed] [Google Scholar]
- Rodgers BL. Concepts, analysis and the development of nursing knowledge: The evolutionary cycle. Journal of advanced nursing. 1989;14(4):330–335. doi: 10.1111/j.1365-2648.1989.tb03420.x. [DOI] [PubMed] [Google Scholar]
- Rogers AE. The Effects of Fatigue and Sleepiness on Nurse Performance and Patient Safety. Agency for Healthcare Research and Quality (US); 2008. [Accessed June 22, 2017]. Available at: http://www.ncbi.nlm.nih.gov/pubmed/21328747. [PubMed] [Google Scholar]
- Ryan P, Sawin KJ. The Individual and Family Self-Management Theory: background and perspectives on context, process, and outcomes. Nursing outlook. 2009;57(4):217–225.e6. doi: 10.1016/j.outlook.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwabe L, Haddad L, Schachinger H. HPA axis activation by a socially evaluated cold-pressor test. Psychoneuroendocrinology. 2008;33(6):890–895. doi: 10.1016/j.psyneuen.2008.03.001. [DOI] [PubMed] [Google Scholar]
- Scott LD, Arslanian-Engoren C, Engoren MC. Association of sleep and fatigue with decision regret among critical care nurses. American Journal of Critical Care. 2014;23(1):13–23. doi: 10.4037/ajcc2014191. [DOI] [PubMed] [Google Scholar]
- Sievertsen HH, Gino F, Piovesan M. Cognitive fatigue influences students’ performance on standardized tests. Proceedings of the National Academy of Sciences. 2016;113(10):2621–2624. doi: 10.1073/pnas.1516947113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sollisch J. The cure for decision fatigue. Wall Street Journal 2016 [Google Scholar]
- Stewart AF, et al. Fighting decision fatigue. Annals of Neurology. 2012;71(1):A5–A15. doi: 10.1002/ana.23531. [DOI] [PubMed] [Google Scholar]
- Thaler R, et al. The effect of myopia and loss aversion on risk taking: An experimental test. The Quarterly Journal of Economics. 1997;112(2):647–661. [Google Scholar]
- Thomas NK. Resident Burnout. JAMA. 2004;292(23):2880. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- Thompson C, et al. An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies. 2013;50(12):1720–1726. doi: 10.1016/j.ijnurstu.2013.05.003. [DOI] [PubMed] [Google Scholar]
- Thompson C, et al. Nurses, information use, clinical decision making--the real world potential for evidence-based decisions in nursing. Evidence-based nursing. 2004;7(3):68–72. doi: 10.1136/ebn.7.3.68. [DOI] [PubMed] [Google Scholar]
- Thompson C, Yang H. Nurses’ Decisions, Irreducible Uncertainty and Maximizing Nurses’ Contribution to Patient Safety. [Accessed June 22, 2017];Healthcare Quarterly. 2009 12(sp):e178–e185. doi: 10.12927/hcq.2009.20946. Available at: http://www.longwoods.com/content/20946. [DOI] [PubMed] [Google Scholar]
- Tierney J. Do You Suffer From Decision Fatigue? New York Times. 2011:1–11. [Google Scholar]
- Tofthagen R, Fagerstrøm L. Rodgers’ evolutionary concept analysis–a valid method for developing knowledge in nursing science. Scandinavian journal of caring. 2010;24(s1):21–31. doi: 10.1111/j.1471-6712.2010.00845.x. [DOI] [PubMed] [Google Scholar]
- Vohs KD, et al. Decision fatigue exhausts self-regulatory resources - but so does accomodating to unchosen alternatives. Unpublished manuscript. 2006 Available at: http://onlinelibrary.wiley.com/doi/10.1002/cbdv.200490137/abstract.
- Vohs KD, et al. Making choices impairs subsequent self-control: A limited-resource account of decision making, self-regulation, and active initiative. Journal of Personality and Social Psychology. 2008a;94(5):883–898. doi: 10.1037/0022-3514.94.5.883. Available at: http://doi.apa.org/getdoi.cfm?doi=10.1037/0022-3514.94.5.883. [DOI] [PubMed] [Google Scholar]
- Vohs KD, et al. Making choices impairs subsequent self-control: A limited-resource account of decision making, self-regulation, and active initiative. Journal of Personality and Social Psychology. 2008b;94(5):883–898. doi: 10.1037/0022-3514.94.5.883. [DOI] [PubMed] [Google Scholar]
- Walker LO, Avant KC. Concept analysis. Strategies for theory construction in nursing. 2005;3:37–54. [Google Scholar]
- Wang J, et al. Trade-Offs and Depletion in Choice. Journal of Marketing Research. 2010;47(5):910–919. [Google Scholar]
- Zeelenberg M. The use of crying over spilled milk: A note on the rationality and functionality of regret. Philosophical Psychology. 1999;12(3):325–340. [Google Scholar]