Abstract
A national survey conducted for the Office of Rural Health Policy in 1995 identified 558 participants in rural telemedicine; 499 (89%) responded to a detailed follow-up survey to describe type of use. While 84% of respondents reported using interactive video, only 25% reported access to e-mail for exchange of data. The challenge to medical informatics is to connect dispersed providers, not just with videoconferencing, but also with other information-sharing methods.
Under contract to the Office of Rural Health Policy (ORHP), Abt Associates, Inc., conducted two surveys to determine the status of rural telemedicine. A nationwide screening survey of all non-federal rural hospitals was conducted in the summer of 1995 to identify those hospitals actively using telemedicine. All 2,472 non-federal rural hospitals were surveyed, and 96% responded.1 The screening survey identified 558 participants in telemedicine (a program with a main site and three affiliates counts as four participants). Each participant received a detailed follow-up survey in January 1996 to describe the uses of telemedicine, the equipment and transmission media in use, the funding sources and costs of telemedicine installations, the volume of care being provided, the volume of non-clinical uses of the systems, and the use of telemedicine to fill gaps in specialty access in remote rural areas. A total of 499 participants (89%) responded. Both surveys were conducted via mailed questionnaires, with telephone follow-up to non-respondents. The full results of this study are available from ORHP.2.
Of the 499 respondents, 340 used only teleradiology, and 159 used at least one clinical application other than teleradiology. This report discusses data reported by these latter 159 rural telemedicine sites and the implications for medical informatics.
Rural Telemedicine
Current rural telemedicine programs are new and expanding quickly. Forty-one percent of survey respondents reported that they had been providing clinical teleconsults for 1 year or less (as of January 1996), and two thirds had been operational for 2 years or less. The average rural telemedicine network had 9 affiliated facilities and planned to have 13 by the end of 1996. These networks were typically complex, with one or more “hub” sites providing clinical teleconsultations, several “spoke” sites receiving these teleconsultations, and several other sites providing consultations in some specialties and receiving consultations in other specialties.
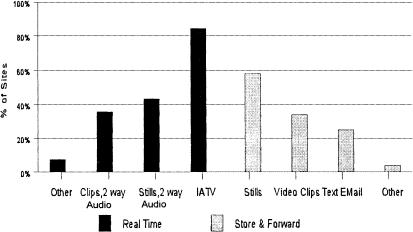
▶ displays the methods the 159 telemedicine facilities reported for transfer of data and images.
Figure 1.
Data image transfer technologies (159 rural telemedicine facilities).
Eighty-four percent of telemedicine programs used full-motion interactive video. Of those reporting real-time videoconferencing, 16% employed desktop technologies, and a few had both studio and desktop videoconferencing available. Sixty-three percent report some form of store-and-forward image transfer.
Only 25% of respondents reported access to e-mail for sending textual data. Numerous phone calls are required to schedule and arrange each telemedicine session; the patient, the primary care practitioner, the consulting clinician, and the equipment all have to be ready at the same time. Prior to each video consultation, medical records, intake forms, insurance forms, and so on are routinely faxed between the patient's facility and the consultant's facility. When telemedicine is used for urgent or emergent care coverage, this faxing of material can delay connection between physician and patient by 30 minutes or more.
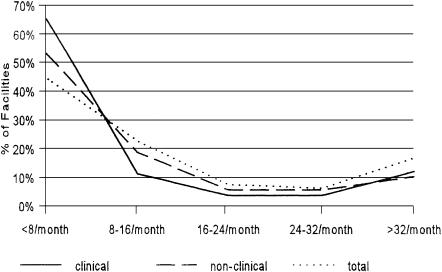
In addition to clinical consultations, equipment is used for non-clinical purposes such as administrative meetings and training sessions. ▶ depicts the volume of use by site. Sixty-seven percent of the 159 telemedicine facilities used their equipment fewer than 16 times per month for any purpose (clinical and non-clinical combined), with 45% using it fewer than 8 times per month. The average number of total sessions per month was 24, but the median was only 11. A subset of 107 respondents reported the number of sessions that were clinical and those that were non-clinical. These respondents reported an average of 13 non-clinical sessions per month (median 7) and an average of 18 clinical sessions per month (median 4.5). The data reveal a modest trend toward increased volume with increased maturity.
Figure 2.
Volume of telemedicine sessions, clinical and non-clinical.
Implications for Medical Informatics
Rural telemedicine programs have emphasized high-bandwidth interactive video technology, largely in isolation from other forms of information management and data exchange. The low emphasis on data transfer may reflect the generally under-automated nature of rural health care in the United States as well as the fact that telemedicine programs tend to be somewhat self-contained “projects” rather than integrated components of larger health information systems.
The isolated nature of these programs within their parent medical centers may be partially due to the funding stream for telemedicine. Primary support is often through a time-limited grant with some matching hospital support. Thus telemedicine projects are rarely initiated as fully integrated business solutions to rural access problems, and data collected during these remote clinical interactions are not exported to larger clinical information systems.
The feasibility of using multimedia technology for remote clinical interpretation has been demonstrated. The next challenge will be to connect dispersed providers, not just with videoconferencing but with other information-sharing methods. Incorporation of e-mail and enhanced store-and-forward strategies would be first steps toward decreasing the cost and inconvenience of existing telemedicine programs. Ultimately, video communication must be integrated with clinical record management, access to electronic knowledge resources, and practice management systems.
Presented in part at the AMIA Spring Conference, Kansas City, Missouri, June 1996.
This research was supported by the Federal Office of Rural Health Policy and the Health Resources and Services Administration; contract number 240-94-0034.
References
- 1.Hassol A, Gaumer G, Grigsby J, Mintzer CL, Puskin D, Brunswick M. Rural telemedicine: A national snapshot; Telemedicine Journal.1996. ;2:43 -8. [DOI] [PubMed] [Google Scholar]
- 2.Hassol A, Irvin C, Gaumer G. Exploratory evaluation of rural applications of telemedicine. Final Report. September1996. .