Abstract
Objective
To determine the importance of preburn adjustment, injury related variables and selection of coping style on various outcome measures using a biopsychosocial model.
Design
Longitudinal.
Setting
Outpatient burn clinics.
Participants
A total of 231 burn survivors participated in this study as part of a larger burn model system study of 645 patients with major burn injuries.
Interventions
N/A/.
Main Outcome Measures
The SF-36 was used to assess pre burn adjustment. Other outcome measures entered into the model included the ways of Coping Checklist-revised, the Brief Symptom Inventory, the Beck Depression Inventory-II, the Davidson Trauma Scale.
Results
Correlational and mediational analysis revealed that preburn emotional health predicted better adjustment at year one and more PTSD symptoms at year two. Better preburn emotional health was also related to less use of avoidant coping strategies, which was also found to be a mediator of the effect of preburn emotional health and PTSD symptoms. Burn injury characteristics were not significantly associated with psychological adjustment at either year one or year two.
Conclusions
The results indicate that there is a complex relation between premorbid mental health and the selection of coping strategies that impact long term adjustment in persons recovering from a burn injury. This relation seems to have more impact on long-term outcome than preburn emotional or physical health alone or the severity of the burn.
Keywords: burns, coping, adjustment, avoidance, approach, biopsychosocial model
Each year over 486,000 people receive medical treatment and 40,000 are hospitalized for burn injury in the U.S.1 Recovery from a major burn includes painful wound care and months of intense physical therapy to regain strength and function. The intense acute recovery period has a lasting impact on adjustment.2 A majority of patients report symptoms of depression and anxiety, including PTSD, even two years post discharge.3,4,5,6 Survivors of large burns also experience a change in vocational and family roles.7,8 Given the relative infancy of the relevant knowledgebase, we need to look to models of stress, coping, and adjustment from other areas of medicine (e.g. chronic illness) to predict recovery and to identify effective and appropriate targets of interventions.
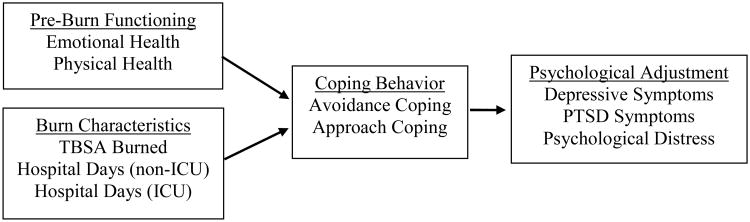
Researchers have identified pre-burn affective disorders, injury characteristics (e.g. burn size and location, inpatient pain), dispositional variables and coping by avoidance as risk factors for the poor adjustment and post-injury onset of psychological disorders.9,10,11 Based on current literature, we have proposed a conceptual model (see Figure 1) to better understand the complex interplay of factors that can potentially affect burn recovery.
Figure 1.
Hypothesized model of psychological adjustment to burn injury
Preburn Emotional and Physical Health
Pre-injury variables are among the strongest determinants of quality of life after burn injuries.4, 9, 12 For example, patients with diabetes, COPD, and other medical comorbidities have lower survival rates, longer initial hospital stays, and poorer overall clinical outcomes.13,14,15 Moreover, persons with burn injuries have higher rates of mental illness prior to their burn.9
Burn Characteristics
The course of hospitalization may have long-term impact on adjustment.16,17,18 Total Burn Surface Area (TBSA), length of hospitalization, and days spent in the ICU or on a ventilator have been used as indicators of the severity of a burn injury. However, research on the relation between these variables and outcomes has been equivocal.16,17,18
Coping
Coping behaviors can be broadly classified as the extent to which one actively approaches the demands of a particular stressor, versus avoidance of that stressor.19,20 For instance, active strategies such as problem-solving, information seeking, and social support seeking can be construed as approach-oriented coping, whereby disengagement, denial, or distraction are avoidance-oriented efforts. Neither approach nor avoidant coping behaviors are inherently adaptive or maladaptive; coping effectiveness is better determined by the characteristics of the individual and the situation.21,22,23,24 Little research has attempted to characterize the adaptiveness of approach and avoidance coping in burn patients over time.
Adjustment
Psychological adjustment is multifaceted and has been construed as including emotional (e.g. anxiety and depressive symptoms), social (e.g. role function and relationship maintenance), and behavioral (e.g. medical adherence) domains. 25 Studies of adjustment after burn injuries have largely focused on the incidence of depression and post-traumatic stress disorder (PTSD). Depression rates following burn injury have varied across studies from 17% to 34% at one year post discharge26 and 27-45% at two years post discharge.3,8 PTSD rates at one year following the burn injury range from 19-45%4. However, experiences across varied adjustment domains is largely undocumented. Patient distress and satisfaction with life are best explained by a combination of psychological and physical variables; no single predictor will be sufficient to explain how a person responds to a burn injury. 27,28,29,30,31
The Current Study
Empirically validated biopsychosocial models of long-term (2 years post burn) psychological adjustment to burn injury are needed to guide future research efforts and to aid in the development of appropriate interventions. The current study addresses this significant gap in the literature by testing a model to better understand the complex interplay between preburn physical and emotional functioning, injury characteristics and coping in a large sample of burn injured patients.
We hypothesized that: (1) lower pre-burn emotional and physical functioning, will predict poorer post-burn adjustment beyond burn-specific factors; (2) lower pre-burn emotional and physical functioning will be associated with greater use of avoidance coping and lower use of approach coping; (3) use of avoidance coping will predict poorer adjustment and approach coping will predict better adjustment; and (4) coping will mediate the relationship of pre-burn functioning and adjustment over time.
Method
Participants
With Institutional Review Board approval, participants were recruited and consented to participate in a larger study of burn patient experiences. Participants were 231 adults who were admitted to a large, regional burn center. Questionnaires were sent via mail. Inclusion criteria included: able to complete subjective evaluations, absence of delirium or psychosis, and able to communicate verbally. Demographic and injury characteristics are presented in Tables 1 and 2. Importantly, as part of the larger study, measures were administered and discontinued at various points throughout the study period, so there is not complete longitudinal data on all 231 patients (see Table 3). Participants lost to follow-up were slightly younger and more likely to have a foot or leg burn compared to study completers. However, they did not differ on any other demographic or clinical variable, nor did they differ on level of adjustment or pre-burn health status. Measures were given at 1 and 2 years post discharge from the hospital.
Table 1. Participant Demographics (N=231).
| Demographic Variable | |
|---|---|
| Mean Age | 40.5 (SD=13.96) |
| Gender: | |
| Male | 72.7% |
| Female | 27.3% |
| Ethnicity: | |
| White (non-Hispanic) | 87.0% |
| Asian/Pacific Islander | 3.5% |
| Hispanic/Latino | 2.6% |
| African American/Black | 2.6% |
| Native American | 2.6% |
| Other | 1.7% |
| Education: | |
| less than high school | 10.4% |
| high school grad/GED | 66.7% |
| associates/technical degree | 8.7% |
| college degree | 10.0% |
| unknown | 4.2% |
| Married/Significant Relationship | 52.0% |
| Job Status: | |
| employed | 66.2% |
| unemployed | 26.8% |
| retired | 4.8% |
| other | 2.2% |
| TBSA Burned: | |
| 0 to 15% | 56.7% |
| 16 to 30% | 26.4% |
| 31 to 45% | 9.1% |
| 46 to 60% | 6.1% |
| More than 60% | 1.7% |
| Mean Number of Hospital Days: | |
| Non-ICU | M = 19.01 (Range: 1 to 70) |
| ICU | M = 10.47 (Range: 0 to 78) |
| Injury Location: | |
| Head/Neck | 51.5% |
| Trunk | 57.6% |
| Perineum | 3.5% |
| Hand | 64.9% |
| Leg | 52.8% |
| Foot | 25.1% |
| Injury Etiology: | |
| Fire/Flame | 64.8% |
| Scald | 7.0% |
| Grease/Tar | 10.4% |
| Electricity | 6.1% |
| Hot Object Contact | 4.3% |
| Chemical | 2.6% |
| Other | 4.8% |
Table 2. Participant Clinical Information (N=231).
| Injury-Related Variable | |
|---|---|
| TBSA Burned: | |
| 0 to 15% | 56.7% |
| 16 to 30% | 26.4% |
| 31 to 45% | 9.1% |
| 46 to 60% | 6.1% |
| More than 60% | 1.7% |
| Mean Number of Hospital Days: | |
| Non-ICU | M = 19.01 (Range: 1 to 70) |
| ICU | M = 10.47 (Range: 0 to 78) |
| Injury Location: | |
| Head/Neck | 51.5% |
| Trunk | 57.6% |
| Perineum | 3.5% |
| Hand | 64.9% |
| Leg | 52.8% |
| Foot | 25.1% |
| Injury Etiology: | |
| Fire/Flame | 64.8% |
| Scald | 7.0% |
| Grease/Tar | 10.4% |
| Electricity | 6.1% |
| Hot Object Contact | 4.3% |
| Chemical | 2.6% |
| Other | 4.8% |
Table 3. Means and standard deviations for Preburn SF-36 and Primary Outcome Measures.
| M | SD | N | ||||
|---|---|---|---|---|---|---|
| Pre-Burn SF-36 Physical Health Score | 86.78 | 19.05 | 231 | |||
| Pre-Burn SF-36 Emotional Health Score | 90.91 | 21.81 | 231 | |||
| Psychological Adjustment | ||||||
| 1 year post-discharge | 2 years post-discharge | |||||
| M | SD | N | M | SD | N | |
|
| ||||||
| BDI-II | 12.03 | 11.81 | 78 | 12.70 | 13.07 | 54 |
| BSI – GSI | 55.71 | 15.17 | 69 | 51.35 | 13.69 | 20 |
| Davidson Trauma Scale | 37.28 | 35.52 | 75 | 29.87 | 28.08 | 62 |
Note. BSI = Brief Symptom Inventory; BDI = Beck Depression Inventory.
Measures
Medical Outcome Study Short Form-36 (SF-36)32
The SF-36 served as the indicator of premorbid mental and physical functioning. This 36-item inventory assesses health status across eight health concepts: limitations in physical activities; limitations in social activities; limitations in usual role activities; bodily pain; general mental health; limitations in usual role activities because of emotional problems; vitality (energy and fatigue); perceived overall health. Reliability coefficients across subscales range from .65 to .94 (median = .85) and vary somewhat across patient populations. The SF-36 is widely used and has been established across diverse patient groups 33 patients answered questions according to their perceptions of functioning in the two weeks prior to their injury.
Ways of Coping Checklist–Revised
Coping was assessed by the Ways of Coping Checklist-Revised. 23 This 42-item scale assessed how frequently they used each particular coping strategy in dealing with their burn injury on a 4-point scale ranging from 0 (never used) to 3 (regularly used). The scale yields five subscales including self-blame, wishful thinking, avoidance, social support seeking, and problem-focused coping. Given that coping is hypothesized as a mediator of pre-burn health and long-term adjustment, coping measures obtained at 6-months post discharge were utilized. For this study, composite measures of avoidance and approach coping were determined by the use of exploratory factor analysis with Varimax rotation. The self-blame, wishful thinking, and avoidance scales comprised the avoidance coping composite. Factor loadings were .54, .85 and .71, respectively. Social support seeking and problem-focused coping scales comprised the approach coping composite. Factor loadings were .98 and .61, respectively. No secondary loadings were > .29.
Brief Symptom Inventory (BSI)
The BSI is a 53-item measure that is an abbreviated version of the Symptom Checklist-90.34 Patients rate the occurrence of symptoms on a 0-4 scale. Higher scores indicate the presence of more symptoms. For the analysis of this study, we used the Global Severity Index subscale.
Beck Depression Inventory II (BDI-II)
The BDI-II is a widely used, 21-item measure that assesses depressive symptoms. The BDI-II demonstrates strong psychometric properties including correlations with clinical ratings of depression ranging from .65 to .67.35,36 The BDI-II was used as an outcome measure at the one-year and two-year timepoints.
Davidson Trauma Scale (DTS)
The DTS is a 17-item measure that assesses frequency and severity of symptoms of emotional trauma. The DTS demonstrates strong psychometric properties including adequate test-retest reliability and internal consistency (Cronbach's alphas over .90 37 across scales). This was used as an outcome measure at the one-year and two-year timepoints.
Medical Variables
Burn-specific variables were collected via medical chart review. These included, number of ICU days, number of non-ICU hospital days, and TBSA. TBSA is commonly used as an indication of burn severity and is expressed in terms of a percentage. Demographic information including age, gender, ethnicity, education level, and marital status were self-reported.
Data Analyses
Descriptive statistics were computed for key study variables including sociodemographic and relevant clinical characteristics, including indicators of adjustment. Relationships of relevant demographic with adjustment indicators were examined to identify possible covariates. Variables with significant relationships with adjustment were included as covariates in all subsequent analyses. Additional clinical covariates were identified a priori including pre-burn physical health, pre-burn emotional health, and relevant burn characteristics (i.e., TBSA, days of hospitalization).
Multiple linear regression was used to test study hypotheses. Adjustment indicators were separately regressed on pre-burn physical and pre-burn emotional health, as well as identified covariates. Relevant demographic covariates were entered in the first step, burn characteristics were entered in step 2, pre-burn physical health in step 3, and pre-burn emotional health was entered in the final step. This approach will allow for examination of ΔR2, though only the results of the full simultaneous model are reported. In analyses predicting year 2 adjustment, corresponding year 1 adjustment scores were entered in the first step to provide the opportunity to predict change in adjustment over time.
Finally, principles outlined by Baron and Kenny (1986) were used to identify candidates for mediation. Thus, avoidance and approach coping potentially function as mediators between pre-burn emotional health and pre-burn physical health, and the related dependent variables of psychological adjustment if: (1) Variations in levels of pre-burn emotional health, pre-burn physical health, or burn characteristics account for significant variations in adjustment outcomes; (2) Variations in levels of pre-burn emotional or physical health account for significant variations in avoidance and approach coping; and (3) Variations in coping behaviors account for significant variations in adjustment outcomes. Multiple linear regressions were conducted to test these relationships. Further, mediated effects were tested based on bootstrapped standard errors for indirect paths generated in Mplus 3.0. This method makes fewer assumptions about the sampling distribution, is more accurate, and yields more powerful tests than other statistical methods for assessing mediated effects (e.g., Sobel test).38
Results
Preliminary Analyses
Means and standard deviations of pre-burn physical and emotional health, and primary outcomes are presented in Table 3.
To identify possible demographic covariates of psychological adjustment, correlations among demographic and adjustment variables were examined (see Table 4). Of these, only gender was significantly correlated with measures of adjustment such that being female was associated with greater self-reported psychological distress and PTSD symptoms at year 1. Gender was therefore included as a covariate in all subsequent analyses.
Table 4.
Inter-scale Correlations of Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Depressive Symptoms | .89*** | .92*** | .85*** | -.08 | .13 | -.06 | -.04 | .02 | -.02 |
| 2. Psychological Distress | .65** | .65** | .77*** | -.05 | .30* | -.17 | -.15 | .18 | -.13 |
| 3. PTSD Symptoms | .82*** | .29 | .85*** | -.17 | .23* | -.03 | -.06 | .05 | -.09 |
|
| |||||||||
| Demographics and Burn Characteristics | |||||||||
|
| |||||||||
| 4. Age | -.02 | .26 | -.12 | - | .01 | .33*** | -.07 | .17** | .00 |
| 5. Gender | -.09 | .08 | .08 | - | .01 | -.11 | .02 | -.10 | |
| 6. Marital Status | .10 | -.17 | -.06 | - | -.10 | -.08 | -.07 | ||
| 7. TBSA Burned | .08 | -.12 | -.05 | - | .21** | .80*** | |||
| 8. Hospital Days (Non-ICU) | -.04 | .52* | -.05 | - | .17* | ||||
| 9. ICU Days | .08 | .17 | -.08 | - | |||||
Note. Correlations with year 1 adjustment variables are above the diagonal; year 2 associations are below the diagonal; and year 1 – year 2 associations are reported on the diagonal. BSI = Brief Symptom Inventory; DTS = Davidson Trauma Score; TBSA = total body surface area; ICU = Intensive Care Unit. Gender was coded 0 = male and 1 = female. Marital Status was coded 0 = single and 1 = married/partnered.
p<.05;
p<.01;
p<.00
Predictors of Adjustment
Results of regression analyses are reported in Table 5.
Table 5. Results Regression Analyses on Indicators of Year 1 and Year 2 Adjustment.
| Outcome and predictor variables | Depressive Symptoms | Psychological Distress | PTSD Symptoms | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| B | SE B | β | ΔR2 | B | SE B | β | ΔR2 | B | SE B | β | ΔR2 | |
| 1 Year Post-Discharge | ||||||||||||
| Step 1: Gender | -.10 | .10 | -.12 | .006 | -.01 | .01 | -.07 | .003 | -.53 | .30 | -.21 | .027 |
| Step 2: TBSA Burned | -.03 | .14 | -.03 | .007 | .00 | .01 | -.01 | .073 | -.15 | .45 | -.07 | .025 |
| Days in Hospital (non-ICU) | .05 | .13 | .05 | .02 | .01 | .20 | .39 | .41 | .16 | |||
| Days in ICU | -.05 | .13 | -.07 | -.02 | .01 | -.37 | -.23 | .39 | -.11 | |||
| Step 3: Pre-Burn Physical Health | .09 | .11 | .16 | .082 | .01 | .01 | .33* | .006 | .27 | .33 | .15 | .043 |
| Step 4: Pre-Burn Emotional Health | -.32 | .10 | -.56** | .106 | -.02 | .01 | -.69*** | .224 | -.78 | .31 | -.45* | .076 |
| F(6, 77) = 2.97, p < .05 | F(6, 68) = 4.57, p < .001 | F(6, 74) = 2.35, p < .05 | ||||||||||
| 2 Years Post-Discharge | ||||||||||||
| Step 1: Year 1 Score | .97 | .09 | .87*** | .795 | .31 | .10 | .53** | .427 | .89 | .09 | .91*** | .726 |
| Step 2: Gender | -.01 | .08 | -.02 | .001 | -.01 | .01 | -.13 | .052 | -.08 | .20 | -.04 | .001 |
| Step 3: TBSA Burned | .06 | .12 | .10 | .009 | -.01 | .01 | -.32 | .272 | .33 | .29 | .15 | .016 |
| Days in Hospital (non-ICU) | -.07 | .13 | -.05 | .02 | .01 | .47 | .13 | .31 | .04 | |||
| Days in ICU | .01 | .12 | .01 | .01 | .01 | .24 | -.17 | .28 | -.08 | |||
| Step 4: Pre-Burn Physical Health | -.07 | .01 | -.12 | .000 | -.01 | .01 | -.17 | .021 | -.71 | .24 | -.47** | .018 |
| Step 5: Pre-Burn Emotional Health | .02 | .09 | .04 | .000 | -.01 | .01 | -.11 | .002 | .56 | .24 | .37* | .031 |
| F(7, 39) = 19.64, p < .001 | F(7, 18) = 5.04, p < .01 | F(7, 43) = 19.57, p < .001 | ||||||||||
| Note: TBSA = total body surface area. Discrepancies in df's are a result of missing values. Gender was coded 0 = male and 1 = female. | ||||||||||||
| Outcome | Mediated effect | Significance of test statistic |
|---|---|---|
| Pre-burn physical health | ||
| Psychological distress at year 1 | <.01 | .25 |
| PTSD symptoms at year 2 | -.01 | -.01 |
| Pre-burn emotional health | ||
| Depressive symptoms at year 1 | -.03 | -.66 |
| Psychological distress at year 1 | <-.01 | -.89 |
| PTSD symptoms at year 1 | 1.01 | 2.11* |
| PTSD symptoms at year 2 | 1.25 | 2.45* |
Better pre-burn physical health was significantly related to greater psychological disptress at year 1 (p<.05), and lower PTSD symptoms at year 2 (p<.01). Pre-burn emotional health significantly predicted better adjustment for all three indicators of adjustment at year 1; as well as greater year 2 PTSD symptoms (p<.05). It should be noted that pre-burn emotional health accounted for 10.6% of the variance of year 1 depressive symptoms, 22.4% of the variance of year 1 psychological distress, and 7.6% of the year 1 PTSD symptoms variance; in contrast, pre-burn physical health accounted for less than 1% of the year 1 psychological distress variance and less than 1.8% of the year 2 PTSD symptoms variance. Neither burn related factors nor gender were significantly related to adjustment outcomes.
Mediation Analysis
When avoidance coping was regressed on pre-burn emotional health and pre-burn physical health simultaneously, both pre-burn emotional health (β = -.48, p < .05) and pre-burn physical health (β = .39, p < .05) were significant predictors. Better pre-burn emotional health was related to lower use of avoidance coping, while better pre-burn physical health was related to greater use of avoidance coping strategies. However, neither pre-burn physical (β = .05, ns) nor emotional health (β = -.09, ns) predicted approach coping behavior.
Adjustment outcomes at year 1 and 2 were regressed on avoidance coping, controlling for gender. Greater use of avoidance coping significantly predicted depressive symptoms at year 1 (β = .41, p < .05; ΔR2 = .147); greater psychological distress at year 1 (β = .37, p < .05; ΔR2 = .115); and greater PTSD symptoms at year 1 (β = .40, p < .05; ΔR2 = .174) and year 2 (β = .56, p < .05; ΔR2 = .255). Avoidance coping was not related to year 2 depressive symptoms (β = .40, ns) or year 2 psychological distress (β = .62, ns).
Mediated effects were tested based on bootstrapped standard errors for indirect paths generated in Mplus 3.0. This method makes fewer assumptions about the sampling distribution, is more accurate, and yields more powerful tests than other statistical methods for assessing mediated effects (e.g., Sobel test).38 Based on the results of the analyses presented above, mediated effects were examined for avoidance coping for significant relationships between pre-burn physical and emotional health and indicators of psychological adjustment at year 1 and year 2. Only the mediated chains from pre-burn emotional health to PTSD symptoms at years 1 and 2 were significant.
In summary, better pre-burn physical health was related to more psychological distress at year 1 and less PTSD symptoms at year 2. Further, better pre-burn physical health was associated with greater use of avoidant coping strategies. Pre-burn emotional health showed a somewhat different pattern in that better pre-burn emotional health predicted better adjustment at year 1 and more PTSD symptoms at year 2. Pre-burn emotional health was also related to less use of avoidance coping, which was also found to be a mediator of the effect of pre-burn emotional health on PTSD symptoms at 2 years. These relationships are depicted in Figure 2. It is also noteworthy that burn injury characteristics were not significantly associated with psychological adjustment.
Figure 2.
Resulting model of pre-burn physical health (top) and pre-burn emotional health (bottom) on long-term adjustment to burn injury.
Conclusions
This study provides insight into the longer term psychological adjustment following burn injury and helps elucidate a stress and coping model of adjustment in this patient population. Our hypotheses in this study were only partially supported. Despite our prediction that better pre-burn functioning would be associated with better post-burn adjustment, results suggest a more complex pattern. For instance, we found that better preburn physical health was related to more distress at year 1, but lower PTSD symptoms at year 2. Such findings support that adjustment is a dynamic process that unfolds over time and one that is bound by context. It might be that those with better pre-injury physical health have a greater initial adjustment with post-burn impairments and are less experienced at coping with health-related adversity. Future studies should better elucidate such possibilities, but our data supports this theory as better pre-burn physical health was also associated with more maladaptive coping (avoidance) at 6 months. At the same time, better initial health might protect over longer periods of time. Associations with lower PTSD symptoms at the distal time point highlights this possibility.
The case of pre-burn emotional health also highlights the need to examine adjustment patterns over time. As predicted, better pre-burn emotional functioning was associated with better adjustment at year 1, as well as less avoidance coping. Yet, by year 2 better pre-burn emotional functioning was associated with worse adjustment, as indicated by PTSD symptoms. Certainly, more research is needed to understand this changing relationship. Observations in trauma-exposed individuals 39 and patients with chronic illness 40suggest that there are patient subgroups with distinct trajectories distress over time. Longitudinal, prospective studies that utilize multiple measurements are critical to identifying these patterns in burn patients. In this sample, it is possible that symptoms of PTSD had not yet manifested at year 1 and better pre-burn emotional functioning predicts delayed onset of symptoms. It is also possible that life demands change after the first year, such as return to work and enhanced social demands. For instance, clinically, we see patients who had been adjusting well suddenly develop more intense PTSD symptoms around the time that they return to work, particularly if they were burned on the job. Finally, it is also possible that those with better preburn emotional heath may not have been subjected to adequate mental health screening early in their hospitalization and prodromal PTSD conditions may not have been identified. In contrast, someone identified as struggling early on may have received more aggressive intervention.
The current study also informs the role of coping in adjustment to burn injury. Consistent with literatures on coping and chronic illness, 25 avoidance-oriented coping was generally related to poorer adjustment, at least for year 1. Avoidance likely thwarts efforts of emotional processing, engagement in care, garnering of support, as well as acceptance and growth. Results partially support that avoidance coping acts as a cognitive or behavioral pathway by which pre-burn functioning influences adjustment over time. However, coping itself is dynamic. This study relied on a single measurement of coping that may or may not be reflective of coping behavior across recovery. Future studies should examine coping across time.
Contrary to our expectations, approach-oriented coping had seemingly no relationship with adjustment. It will be important for researchers to measure adjustment across domains to fully understand the role of approach coping. Again, calling upon research in chronic illness, approach coping might be associated with positive and/or biobehavioral domains not measured in the current study.40, 41
Finally, as expected, burn-related factors were not significant predictors of adjustment. Researchers and clinicians should be cautious in assuming that those with smaller burns will have more positive adjustment, and vice versa. At the same time, burn survivors need to be active participants in their burn recovery. Range of motion exercises and physical therapy, daily wound debridement, and adherence to other therapy recommendations might be more frequent, demanding, or complex for those with larger or more complicated injuries. Greater engagement in approach coping and reduced avoidance may be particularly essential when self-care demands are greater.
Study Limitations
First, follow-up rates for each measure varied and affected our n at each timepoint. Second, we were not able to measure all variables that might be of importance, including pain levels, injury severity beyond TBSA (e.g. amputations, inhalation injury) and relevant personality factors. Prior studies have indicated that these variables may be important in predicting long term adjustment and they deserve consideration in future studies. Despite these limitations, the complexity of our findings illustrate the importance of using a biopsychosocial model to guide future research.
The current study provides some direction for clinical utility. Perceptions of pre-injury emotional and physical health, as well as coping behaviors, might be included among hospital-based assessments to begin to identify patients at higher risk for poorer long-term adjustment. Also, behavioral interventions that reduce the use of avoidance-oriented coping, particularly those with poorer pre-burn emotional function might have a salutary effect on adjustment over time.
Acknowledgments
Funding Information: This study was funded by a grant from NIH: NIH ROIGMO42725
Abbreviations
- TBSA
Total Burn Surface Area
- ICU
Intensive Care Unit
- PTSD
Post-Traumatic Stress Disorder
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Association AB. American Burn Association Burn Incidence and treatment in the US: National Burn Repository. American Burn Association. 2015;139 [Google Scholar]
- 2.Corry NH, Klick B, Fauerbach JA. Posttraumatic stress disorder and pain impact functioning and disability after major burn injury. Journal of burn care & research : official publication of the American Burn Association. 2010 Jan-Feb;31(1):13–25. doi: 10.1097/BCR.0b013e3181cb8cc8. [DOI] [PubMed] [Google Scholar]
- 3.Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. The Journal of burn care & rehabilitation. 2001 Nov-Dec;22(6):417–424. doi: 10.1097/00004630-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Van Loey NE, Van Son MJ. Psychopathology and psychological problems in patients with burn scars: epidemiology and management. American journal of clinical dermatology. 2003;4(4):245–272. doi: 10.2165/00128071-200304040-00004. [DOI] [PubMed] [Google Scholar]
- 5.McKibben JB, Bresnick MG, Wiechman Askay SA, Fauerbach JA. Acute stress disorder and posttraumatic stress disorder: a prospective study of prevalence, course, and predictors in a sample with major burn injuries. Journal of burn care & research : official publication of the American Burn Association. 2008 Jan-Feb;29(1):22–35. doi: 10.1097/BCR.0b013e31815f59c4. [DOI] [PubMed] [Google Scholar]
- 6.Edwards RR, Magyar-Russell G, Thombs B, et al. Acute pain at discharge from hospitalization is a prospective predictor of long-term suicidal ideation after burn injury. Archives of physical medicine and rehabilitation. 2007 Dec;88(12 Suppl 2):S36–42. doi: 10.1016/j.apmr.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 7.Mason ST, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K. Return to work after burn injury: a systematic review. Journal of burn care & research : official publication of the American Burn Association. 2012 Jan-Feb;33(1):101–109. doi: 10.1097/BCR.0b013e3182374439. [DOI] [PubMed] [Google Scholar]
- 8.Holavanahalli R, Acton A, Wiechman S. Psychological Outcomes of Burn Injuries. Burn Care for General Surgeons and General Practitioners. Burn Care for General Surgeons and General Practitioners. 2016 Jan;2016:261–271. [Google Scholar]
- 9.Patterson DR, Finch CP, Wiechman SA, Bonsack R, Gibran N, Heimbach D. Premorbid mental health status of adult burn patients: comparison with a normative sample. The Journal of burn care & rehabilitation. 2003 Sep-Oct;24(5):347–350. doi: 10.1097/01.BCR.0000086070.91033.7F. [DOI] [PubMed] [Google Scholar]
- 10.Fauerbach JA, McCann UD. Traumatic burn injury: neuropsychiatric perspectives on risk, outcomes and treatment. International review of psychiatry. 2009 Dec;21(6):501–504. doi: 10.3109/09540260903340832. [DOI] [PubMed] [Google Scholar]
- 11.Lawrence JW, Fauerbach JA. Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: a path analysis. The Journal of burn care & rehabilitation. 2003 Jan-Feb;24(1):63–72. doi: 10.1097/00004630-200301000-00016. discussion 62. [DOI] [PubMed] [Google Scholar]
- 12.Patterson DR, Everett JJ, Bombardier CH, Questad KA, Lee VK, Marvin JA. Psychological effects of severe burn injuries. Psychological bulletin. 1993 Mar;113(2):362–378. doi: 10.1037/0033-2909.113.2.362. [DOI] [PubMed] [Google Scholar]
- 13.O'Keefe GE, Hunt JL, Purdue GF. An evaluation of risk factors for mortality after burn trauma and the identification of gender-dependent differences in outcomes. Journal of the American College of Surgeons. 2001 Feb;192(2):153–160. doi: 10.1016/s1072-7515(00)00785-7. [DOI] [PubMed] [Google Scholar]
- 14.Schwartz SB, Rothrock M, Barron-Vaya Y, et al. Impact of diabetes on burn injury: preliminary results from prospective study. Journal of burn care & research : official publication of the American Burn Association. 2011 May-Jun;32(3):435–441. doi: 10.1097/BCR.0b013e318217f954. [DOI] [PubMed] [Google Scholar]
- 15.Murabit A, Tredget EE. Review of burn injuries secondary to home oxygen. Journal of burn care & research : official publication of the American Burn Association. 2012 Mar-Apr;33(2):212–217. doi: 10.1097/BCR.0b013e3182331dc6. [DOI] [PubMed] [Google Scholar]
- 16.Ptacek JT, Patterson DR, Montgomery BK, Heimbach DM. Pain, coping, and adjustment in patients with burns: preliminary findings from a prospective study. Journal of pain and symptom management. 1995 Aug;10(6):446–455. doi: 10.1016/0885-3924(95)00083-b. [DOI] [PubMed] [Google Scholar]
- 17.Patterson DR, Tininenko J, Ptacek JT. Pain during burn hospitalization predicts long-term outcome. Journal of burn care & research : official publication of the American Burn Association. 2006 Sep-Oct;27(5):719–726. doi: 10.1097/01.BCR.0000238080.77388.FE. [DOI] [PubMed] [Google Scholar]
- 18.Edwards RR, Smith MT, Klick B, et al. Symptoms of depression and anxiety as unique predictors of pain-related outcomes following burn injury. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2007 Nov-Dec;34(3):313–322. doi: 10.1007/BF02874556. [DOI] [PubMed] [Google Scholar]
- 19.Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annual review of clinical psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- 20.Suls J, Fletcher B. The relative efficacy of avoidant and nonavoidant coping strategies: a meta-analysis. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 1985;4(3):249–288. doi: 10.1037//0278-6133.4.3.249. [DOI] [PubMed] [Google Scholar]
- 21.Folkman S, Lazarus RS. Stress, Appraisal, and Coping. 1984 Mar 15;1984:456. [Google Scholar]
- 22.Stanton AL, Revenson TA, Tennen H. Health psychology: psychological adjustment to chronic disease. Annual review of psychology. 2007;58:565–592. doi: 10.1146/annurev.psych.58.110405.085615. [DOI] [PubMed] [Google Scholar]
- 23.Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of health and social behavior. 1980 Sep;21(3):219–239. [PubMed] [Google Scholar]
- 24.Roberts SM. Applicability of the goodness-of-fit hypothesis to coping with daily hassles. Psychological reports. 1995 Dec;77(3 Pt 1):943–954. doi: 10.2466/pr0.1995.77.3.943. [DOI] [PubMed] [Google Scholar]
- 25.Hoyt MA, Stanton AL. Adjustment to chronic illness. In: Baum AS, Revenson TA, Singer JE, editors. Handbook of health psychology. 2nd. New York, NY: Taylor & Francis; 2012. pp. 219–246. [Google Scholar]
- 26.Wiechman S, Kalpakjian CZ, Johnson KL. Measuring Depression in Adults With Burn Injury: A Systematic Review. Journal of burn care & research : official publication of the American Burn Association. 2016 Sep-Oct;37(5):e415–426. doi: 10.1097/BCR.0000000000000384. [DOI] [PubMed] [Google Scholar]
- 27.Thombs BD, Haines JM, Bresnick MG, Magyar-Russell G, Fauerbach JA, Spence RJ. Depression in burn reconstruction patients: symptom prevalence and association with body image dissatisfaction and physical function. General hospital psychiatry. 2007 Jan-Feb;29(1):14–20. doi: 10.1016/j.genhosppsych.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Pavoni V, Gianesello L, Paparella L, Buoninsegni LT, Barboni E. Outcome predictors and quality of life of severe burn patients admitted to intensive care unit. Scandinavian journal of trauma, resuscitation and emergency medicine. 2010 Apr 27;18:24. doi: 10.1186/1757-7241-18-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Orwelius L, Willebrand M, Gerdin B, Ekselius L, Fredrikson M, Sjoberg F. Long term health-related quality of life after burns is strongly dependent on pre-existing disease and psychosocial issues and less due to the burn itself. Burns : journal of the International Society for Burn Injuries. 2013 Mar;39(2):229–235. doi: 10.1016/j.burns.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 30.Doctor JN, Patterson DR, Mann R. The 1997 Clinical Research Award. Health outcome for burn survivors. The Journal of burn care & rehabilitation. 1997 Nov-Dec;18(6):490–495. doi: 10.1097/00004630-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Questad KA, Patterson DR, Boltwood MD, et al. Relating mental health and physical function at discharge to rehabilitation status at three months postburn. The Journal of burn care & rehabilitation. 1988 Jan-Feb;9(1):87–89. doi: 10.1097/00004630-198801000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Corporation R. Medical Outcome Study Short Form-36 (SF-36) Medical Outcome Study Short Form-36 (SF-36) 1993 http://www.rand.org/health/surveys_tools/mos/36-item-short-form.html.
- 33.McHorney CA, Ware JEJR, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36):ii Psychometric and clinical tests of validity in measuring physical and mental health constructs. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacology bulletin. 1973 Jan;9(1):13–28. [PubMed] [Google Scholar]
- 35.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961 Jun;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 36.Beck AT, Steer RA, Brown G. Beck Depression Inventory-Second Edition. Manual for the Beck Depression Inventory-II. 1996;1996 [Google Scholar]
- 37.Davidson JRT. Davidson Trauma Scale. Multi-Health Systems, Inc; 1996. [Google Scholar]
- 38.Kobrin S, Rothman A, Aiken L. Understanding why and when intervention strategies work: How mediation and moderation analyses can link psychosocial models and behavioral interventions [Abstract] Annals of Behavioral Medicine. 2008;2008:35. s2. [Google Scholar]
- 39.Burton CL, Galatzer-Levy IR, Bonanno GA. Treatment type and demographic characteristics as predictors for adjustment: Prospective trajectories of depressive symptoms in a population sample. Health Psychology. 2015;34:602–609. doi: 10.1037/hea0000145. [DOI] [PubMed] [Google Scholar]
- 40.Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- 41.Thomas KS, Bower J, Hoyt MA, Sepah S. Disrupted sleep in breast and prostate cancer patients. Psycho-Oncology. 2010;19(7):767–778. doi: 10.1002/pon.1639. [DOI] [PMC free article] [PubMed] [Google Scholar]