Abstract
Background
Military service is associated with smoking initiation, but U.S. veterans are also eligible for special social, financial, and healthcare benefits, which are associated with smoking cessation. A key public health question is how these offsetting pathways affect health disparities; we assessed the net effects of military service on later life pulmonary function among Korean War era veterans by childhood socio-economic status (cSES).
Methods
Data came from U.S.-born male Korean War era veteran (service: 1950–1954) and non-veteran participants in the observational U.S. Health and Retirement Study who were alive in 2010 (average age = 78). Veterans (N = 203) and non-veterans (N = 195) were exactly matched using coarsened exact matching on birth year, race, coarsened height, birthplace, childhood health, and parental and childhood smoking. Results were evaluated by cSES (defined as maternal education <8 yr/unknown or ≥8 yr), in predicting lung function, as assessed by peak expiratory flow (PEF), measured in 2008 or 2010.
Findings
While there was little overall association between veterans and PEF [β = 12.8 L/min; 95% confidence interval (CI): (−12.1, 37.7); p = 0.314; average non-veteran PEF = 379 L/min], low-cSES veterans had higher PEF than similar non-veterans [β = 81.9 L/min; 95% CI: (25.2, 138.5); p = 0.005], resulting in smaller socio-economic disparities among veterans compared to non-veterans [difference in disparities: β = −85.0 L/min; 95% CI: (−147.9, −22.2); p = 0.008].
Discussion
Korean War era military service appears to disproportionately benefit low-cSES veteran lung functioning, resulting in smaller socio-economic disparities among veterans compared with non-veterans.
Keywords: veterans, health disparities, pulmonary function, lung function, matching
INTRODUCTION
There were approximately 18.5 million veterans in the USA in 2016,1 making military service a common and important social experience. Although typically completed in early adulthood, military service entails major social, behavioral, environmental, socio-economic, and psychological exposures, potentially influencing health for decades after the completion of service2. Because today’s armed forces draw disproportionately from socially vulnerable groups (e.g., >20% of military service members fathers have less than a high school education compared with <15% in the general population; <70% of military service members come from a dual-parent households, compared to 85% in the general population3), military service could be an important driver of health disparities, either reducing disparities if these exposures are health-promoting, or exacerbating disparities if these exposures are harmful for long-term health.
Prior work on U.S. military service and health reveals that various aspects of military service affect health in competing or conflicting ways, particularly in terms of smoking initiation and cessation. Compared with non-veterans, Vietnam veterans have elevated smoking rates shortly after the completion of service,4 but not in the long-term.4–6 These discrepant results reflect the complex relationship between military service and health, which appears to change as veterans age,2,7 and vary by population subgroup.5,8
Analyses of the health of military veterans have often focused on smoking behaviors4–6,9 due to the large and long-term negative effects of smoking on health,10 as well as the free distribution of cigarettes in service members rations (until 1975)11–13 and the continued availability of discounted cigarettes at military installations (assessed in 2013),14,15 which may have induced smoking initiation among service memebers.4,16 Due to substantial misreporting of smoking by former smokers,4,17,18 rigorous assessment of lung function is important. Lung function (Fig. 1) is strongly influenced by smoking but also highly socially patterned by life-course socio-economic status (SES), such that individuals with lower SES have worse lung function, on average.19 Reduced lung function additionally predicts worse functional health,20,21 survival,22–26 cognitive function, and increased risk for stroke, heart disease,27 and hospitalizations.28 We might thus expect short-term increases in smoking associated with military service to adversely affect veterans’ lung functioning.
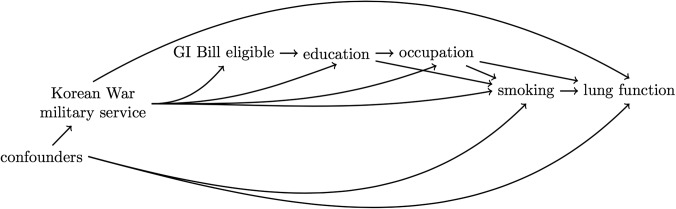
FIGURE 1.
Graphical depiction of several possible pathways via which military service may influence later life lung function. The wide availability of free and discounted cigarettes, coupled with the stress military life, may have induced smoking among service members, which, in turn, may reduce lung function. Military service is also associated with higher educational attainment and occupational class both of which are associated with increased smoking cessation. The net effect of these offsetting pathways on lung function is unclear.
U.S. war veterans are also eligible for special social, financial, and healthcare benefits, which may be responsible for higher rates of smoking cessation among veterans.4,5 For example, the Korean War GI Bill included (1) an educational subsidy that cut college costs by 39–71%,29 (2) a low-interest, government-backed loan benefit, (3) unemployment benefits, and (4) mustering out pay.30 Military service and benefits are associated with increased educational attainment,8,29,31,32 occupational class,33,34 income,32–34 and earlier homeownership.35 These increases in adult SES achieved via military service may offset the harm of smoking on lung function (Fig. 1). Specifically, increased educational attainment by veterans may have paid off over the long term by increasing smoking cessation rates.36–38 Additionally, increases in education and occupational class may have allowed veterans to reduce their exposure to workplace hazards, such as asbestos39 or coal mine dust,40 while increases in income may have allowed veterans to move to neighborhoods with less air pollution,41 resulting in better lung function.
A key public health question is how these competing exposures affect health disparities. The effects of military service may depend on the SES of the individual prior to service. Previous work has shown that socially vulnerable subgroups may disproportionately benefit from military service and benefits,33,34,42,43 potentially leading to a reduction in health disparities.
In this paper, we investigate the long-term effect of Korean War era military service on measured lung function. We advance the literature in two distinct ways. First, we examine the long-term effect of military service on lung function, which to our knowledge, has not been examined previously compared to a non-veteran control group. Second, we test for effect modification by childhood SES (cSES), to determine if lung function disparities changed as a result of Korean War era military service.
MATERIALS AND METHODS
Sample
Data come from the Health and Retirement Study, an observational, longitudinal sample of non-institutionalized persons, and their spouses, 50+ years, living in the USA, and born before 1959. Participants are interviewed approximately every 2 yr; every 6 yr a new cohort of individuals aged 50–55 yr is added to maintain a “steady state” sample.44,45 These analyses were restricted to U.S.-born men who served in the military during the Korean War and non-veterans (veterans from other time periods were excluded), who were alive in 2010 (N = 6,449) and had data on lung function (the outcome) in 2008 or 2010 (N = 3,908, 60.6%; 545 Korean War veterans and 3,363 non-veterans included in matching procedure). We used coarsened exact matching (CEM, detailed below) as our main analytic technique because supplemental analyses show CEM produced better covariate balance compared to the other analytic approaches evaluated (Supplementary Appendix, Section I, Table II). CEM matches exposed and unexposed individuals together on the measured confounders, and “prunes” non-matches from the analytic data set by giving them a weight of 0. The resulting matched analytic sample contained 398 men total, 203 veterans and 195 matched non-veterans.
Exposure
U.S. military service during the Korean War era (1950–1954).
Outcome
Lung function was operationalized as peak expiratory flow (PEF), a measure of obstructive lung disease that is assessed more accurately among older adults with cognitive impairment than forced expiratory volume.46–49 PEF is associated with stroke, heart disease, functional limitations, cognitive function,27 hospitalizations,28 and increased mortality among both smokers and non-smokers.50 PEF was measured with a Mini-Wright Peak Flow meter for a random 41.1% of the sample in 2008 and 58.9% in 2010. Higher measures reflect better lung function, however, the validity of the measure depends on participant’s effort.51 Three measurements were taken 30 s apart, and the top two were averaged as this operationalization was most predictive of death by 2014. Given that the average age of included respondents was 78 yr in 2010, we used outcome data from 2008 and 2010 rather than more recent waves of data collection to minimize bias due to selective survival.
Effect Modification
Childhood SES was evaluated as an effect modifier, and operationalized as years of maternal education. We used mother’s educational attainment because prior work has found that mother’s education is more predictive of adult outcomes than father’s education.52 We additionally found that mother’s education was more predictive of respondent’s educational attainment, a key hypothesized mediator for these analyses, than father’s education (analysis not displayed). We classified high cSES as ≥8 yr of education and low cSES as <8 yr or unknown maternal education. This dichotomization point was used because data were recorded dichotomized at 8 for a subset of respondents,53 however, given that mothers of Korean War veterans were likely born before 1920, when less than half the U.S. population enrolled in high school,54 we believe this dichotomization point is relevant for these birth cohorts. Individuals with missing information on parental education were thought to have a distinct family structure (e.g., grew up in a single-parent household55) and were therefore included in the low-cSES group, similar to other HRS researches examining childhood SES.56 We conducted sensitivity analyses evaluating cSES operationalized as paternal education (Supplementary Appendix, Section II, Table I).
Covariates/Matching Variables
We matched veterans to non-veterans on birth year, race / ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other Race), cSES (detailed above), self-reported childhood health (excellent, very good, good, fair, poor), youth disability (yes/no), parental smoking (yes/no), childhood smoking (yes/no), and self-reported height in 2010 (as an additional control for childhood social and nutritional factors, median dichotomized). To account for selection into military service, we also matched on common reasons for rejection from military service in World War II57: childhood (before age 16) difficulty seeing, learning difficulties, heart trouble, ear problems, psychiatric problems, and depression. Because we matched on coarsened height, we included continuous height in regression models58, along with a missing indicator as 0.05% men were missing height data. We did not adjust for smoking status in adulthood because we conceptualized it as a mediator of the relationship between military service and lung function (Fig. 1); adjusting for mediators may bias estimates.59
Analysis
To implement CEM, veterans and non-veterans were exactly matched on the multivariate distribution of the matching covariates (except for height, which was dichotomized), and weighted. Non-matches were given a weight of 0, treated units were given a weight of 1, and control units were weighted to equal the number of treated units in the stratum, normalized to the number of observations in the matched sample.60 We then used linear regression in the matched and weighted analytic sample to estimate the local sample average treatment effect among the treated (“local SATT”). We ran two analytic models; our first model estimated the overall effect of Korean War era military service on pulmonary function and included the exposure, continuous height as it was coarsened before matching,58,61 and a height missing indicator. Our second analytic model tested to see if disparities changed as a result of military service and, therefore, additionally included the main effect for cSES and a military service by cSES interaction term. To ensure our estimates (1) came from data with good common support and (2) were robust to different analytic techniques, we conducted supplemental analyses using propensity score matching and linear regression to adjust for confounding, and performed several assessments of common support. We used CEM as our main analytic approach because our supplemental analyses show the CEM matching procedure produced better covariate balance than other analytic approaches evaluated (Supplementary Appendix, Section I, Table II). We additionally conducted sensitivity and supplemental analyses to assess the robustness of our results, and control for potential residual confounding by pre-service SES (Supplementary Appendix, Section II, Tables I–IV).
RESULTS
As expected with the CEM matching procedure, all matching covariates were equally distributed between the exposed group (veterans) and the unexposed group (non-veterans) in the analytic sample (Table I). On average, men included in these analyses were 78 yr old and overwhelmingly Non-Hispanic White (96%). More than 80% of veterans and non-veterans mothers’ completed 8 or more years of schooling, and more than 20% started smoking before age 16.
Table I.
Distribution of Confounders in the Weighted Analytic Sample
| Non-Veterans (N = 203) | Veterans (N = 195) | |
|---|---|---|
| Weighted % (Weighted Mean) | Weighted % (Weighted Mean) | |
| Age at 2010 | (78.2) | (78.2) |
| Race | ||
| Non-Hispanic White | 95.6 | 95.6 |
| Non-Hispanic Black | 3.9 | 3.9 |
| Hispanic | 0.5 | 0.5 |
| Other Race | 0.0 | 0.0 |
| Height in 2010 | (70.2) | (70.2) |
| Mother’s Education ≥ 8 yr | 81.3 | 81.3 |
| Childhood health (self-rated) | ||
| Excellent | 67.0 | 67.0 |
| Very good | 25.1 | 25.1 |
| Good | 6.9 | 6.9 |
| Fair | 1.0 | 1.0 |
| Poor | 0.0 | 0.0 |
| Childhood conditions (before age 16) | ||
| Heart problems | 0.0 | 0.0 |
| Ear problems | 1.7 | 1.7 |
| Difficulty seeing | 0.0 | 0.0 |
| Depression | 0.0 | 0.0 |
| Psychiatric problems | 0.0 | 0.0 |
| Disability | 0.0 | 0.0 |
| Learning problems | 0.0 | 0.0 |
| Parental smoking | 76.3 | 76.3 |
| Childhood smoking | 21.2 | 21.2 |
| Outcome | ||
| Lung function (PEF) | (401.3) | (414.0) |
| Ever smokinga | 60.0 | 64.8 |
aWe did not match on ever smoking, but included this distribution in Table I because smoking is a leading cause of reduced lung function, our primary outcome. We did not match on ever smoking because it is a hypothesized mediator of the relationship between military service and lung function (i.e., smoking may be induced by military service); controlling for mediators can lead to biased estimates of the effect of interest. We did, however, match on parental and childhood (before age 16) smoking because both preceded military service. The proportions of veterans who were ever smokers in our sample (65%) and non-veterans who were ever smokers (60%) are similar to previous reports for Vietnam veterans using National Health Interview Survey data from 1978–1980 (65% of veterans, 59% of non-veterans4).
The values presented in Table I are weighted to represent the analytic sample produced by the CEM matching procedure. Because CEM matches exposed (veterans) and unexposed (non-veterans) individuals based on the multivariate distribution of the matching covariates, the matching covariates are equally distributed in the analytic sample.
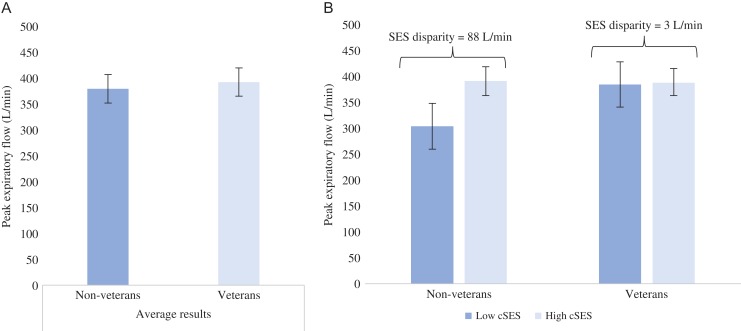
While there was no relationship between Korean War era military service and lung function overall (β = 12.8 L/min; 95% confidence interval (CI): −11.9, 37.5; p = 0.310) (Fig. 2A), the pooled results mask interesting subgroup effects. Interaction results show that the effect of military service varied by cSES (p = 0.008 for interaction), such that veterans from low-cSES backgrounds had better lung function than comparable non-veterans [β = 81.9 L/min; 95% CI: (25.2, 138.5); p = 0.005], while veterans from high cSES backgrounds had equivalent lung function as similar non-veterans [β = −3.2 L/min; 95% CI: (−30.3, 24.0); p = 0.820]. This differential effect of military service by cSES resulted in smaller socio-economic disparities among veterans compared with non-veterans [difference in disparities β = −85.0 L/min; 95% CI: (−147.9, −22.2); p = 0.008] (Fig. 2B). Results were substantively similar when cSES was operationalized by father’s education, and after additional adjustment for pre-service SES (Supplementary Appendix, Section II, Tables I–IV).
FIGURE 2.
The relationship between military service and lung function on average and in low- and high-cSES subgroups. In pooled analysis, there was no effect of military service on lung function (β = 12.8; 95% CI: −12,1, 37.7; p = 0.314), however, the average effect covers up interesting subgroup effects by cSES. Figure 2B shows that socio-economic disparities in lung function among non-veterans are, on average, 88 L/min, while the socio-economic disparity among veterans are 3 L/min; the reduction in socio-economic disparities for veterans compared with non-veterans is 85.0 L/min (95% CI: −147.9, −22.2; p = 0.008). Prior work has found that, among men over 50, PEF fell about 4 L/min each year66, while analysis of the HRS sample indicates that PEF fell about 5.3 L/min each year; together, these results suggest that the observed socio-economic disparity in PEF of 88 L/min among non-veterans could be expected with aging 17–22 yr.
DISCUSSION
These analyses examine the long-term consequences of military service on pulmonary function in a community sample of older adults. Despite substantial targeting of the armed forces by the tobacco industry for decades,11–15 we found no overall relationship between Korean War era military service and lung function among older adults. However, the overall results masked interesting subgroup effects by cSES. Our results suggest veterans from low-cSES backgrounds disproportionately benefited from Korean War era military service and benefits, resulting in an apparent reduction in socio-economic disparities in lung function among veterans compared to non-veterans.
Our finding that Korean War era military service did not adversely affect lung function advances the literature on the long-term health effects of military service. While our results are consistent with prior work showing no long-term differences between veterans and non-veterans on smoking behaviors,4–6 or mortality,62 we examined lung function, an objectively measured intermediate health outcome that is a downstream consequence of smoking, but precedes mortality. Similar conclusions on the long-term effect of military service on smoking, lung function, and mortality (which were examined in different data sets using different methodological approaches), bolsters confidence in all three conclusions.
These findings of no long-term effect of military service on smoking behaviors,4–6 lung function, or mortality62 are somewhat surprising given that the tobacco industry has targeted the military since World War I,63 and cigarettes were freely distributed as rations until 1975,11,13 well after the Korean War ended. The tobacco industry targeted the armed forces, at least in part, for the opportunity to attract people who fit a socio-demographic and cultural profile the industry believed would be beneficial to sales13 at an age near the typical age of smoking initiation.11 This targeting appears to have been successful, with many smokers reporting initiation after joining the military.4,16 However, among Vietnam War veterans, the increase in smoking prevalence among service members does not appear to persist for long after service ends4–6 (although, veterans overall have a higher smoking prevalence than non-veterans64). Our results suggest that Korean War veteran lung functioning was not adversely affected by this suspected short-term increase in smoking prevalence.
Our finding suggesting men from low-cSES backgrounds may have disproportionately benefited from military service advances the literature on the effects of military service among socially vulnerable groups by examining an objectively measured health outcome, lung function (prior work focused on economic,8,33,34,43 or self-reported health outcomes42). We hypothesize several potential pathways from military service to improved lung function through higher SES in adulthood (Fig. 1). First, military service may have provided a “bridging environment” for men from disadvantaged backgrounds, teaching them now to navigate bureaucracies, adhere to institutional norms and rules, or develop other soft skills that improved subsequent labor market outcomes.33 Second, military service may lead directly to higher educational attainment or occupational status through serving as a “screening device” to schools and employers, by signaling dedication and resilience.43 Finally, military service may have led indirectly to higher adult SES through the GI Bill benefits, which provided numerous economic benefits including a substantial education subsidy (the Korean War GI Bill reduced college costs by an estimated 39-71%29), resulting in higher educational attainment,29,31,65 and better occupational outcomes.34 Higher educational attainment may have been especially advantageous for men who grew up in low-cSES families, leading to higher likelihood of smoking cessation, and, thereby, improved lung function. Additionally, higher occupational status may have led to exposure to fewer workplace hazards, such as asbestos39 or coal mine dust,40 while higher income and education may lead veterans to live in higher SES neighborhoods with less air pollution,41 all benefiting lung function. This evidence is encouraging for the potential to remediate health disparities with interventions on adults, and points to the potential specific relevance of late adolescence and early adulthood, the years when veterans typically complete military service.
Some important limitations with these analyses should be acknowledged. First, because the Health and Retirement Study is not designed to be representative of veterans, and due to the method we implemented, coarsened exact matching (CEM), these results may not be generalizable. The CEM analyses include only veterans and non-veterans for whom good matches on the measured covariates can be identified. As a result, these results may not generalize other Korean War veterans. Similar to a randomized trial with stringent inclusion criteria, CEM produces a selected analytic sample that balances confounders between the exposed and unexposed groups (e.g., in Table I, the distributions of all measured confounders is similar among veterans and non-veterans), improving internal validity, but potentially limiting generalizability (or external validity).58 Second, our results may be affected by selective survival such that veteran smokers died before 2010 (surviving to 2010 was an inclusion criteria for our study), leaving the remaining veterans disproportionally healthy, and biasing our results away from the null; however, given that prior analyses found no difference in mortality between Vietnam War veterans and non-veterans (using data from 2002),62 we expect this potential bias to be small. Third, residual confounding is a possibility in this observational study. Because service members need to be physically and mentally fit before joining the armed forces,57 insufficient control for selection into the military may bias results away from the null.67 Specifically, we were unable to assess or control for pre-service differences in lung functioning; it is possible that the observed association between military service and lung functioning among veterans from low-cSES backgrounds is partially or entirely due to pre-services differences in health. For this reason, we interpret our findings as associational, not causal. To control for confounding we matched on common reasons for rejection for military service in WWII, conducted numerous rigorous assessments of common support (Supplementary Appendix, Section I, Tables I and II), and conducted sensitivity and supplemental analyses to assess the robustness of our results and control for potential residual confounding by pre-service SES (Supplementary Appendix, Section II, Tables I–IV). Despite these limitations, this paper is first, to our knowledge, to explore the long-term effects of U.S. military service on lung function using a non-veteran control group, and is therefore an important contribution to the literature.
While these findings have implications for more recent service members, our findings may not generalize to this population for a few reasons. First, the Korean War occurred in a different historical time, and the experiences of both veterans and non-veterans are different today than they were in the 1950s. For example, in recent years the prevalence of chronic obstructive pulmonary disease and asthma has been increasing in the VA population, potentially due to deployment-related exposures from the wars in Afghanistan and Iraq.68 Second, the Korean War GI Bill is one of the possible mechanisms through which military service impacts lung function, however, the current GI Bill provides far less generous benefits than the Korean War GI Bill. If the current GI Bill were strengthened to provide Korean War era level benefits, we may observe a similar reduction in health disparities; however, this hypothesized reduction in disparities is speculative. Given the socio-economic patterning of the contemporary U.S. military, in which individuals from lower socio-economic backgrounds are over-represented (e.g., >20% of service members in the Army and Marine Corps fathers have less than a high school education compared with <15% in the general population3), the current GI Bill may provide a powerful mechanism to alleviate health disparities. The “dose” of behavioral and socio-economic resources delivered in the context of military service is much larger than feasible in even the most ambitious behavioral or social interventions fielded in public health efforts. To the extent that these resources have important health benefits, military service could substantially reduce population health disparities over the long term. Conversely, if the exposures of contemporary military service harm the health of veterans and the benefits provided to veterans are insufficient to offset these exposures, military service may substantially widen population health disparities. These hypotheses should be tested in future research.
In this community sample of older adults, we found no long-term pulmonary consequences of Korean War era military service for veterans compared with non-veterans in pooled analysis. Our interaction results suggest that veterans from lower socio-economic backgrounds may have disproportionately benefited from military service, resulting in a reduction in socio-economic disparities in lung function among veterans compared with non-veterans. Our results suggest there are long-term pulmonary health benefits from military service for men from low-cSES backgrounds, and that health and health disparities are mutable across the life-course.
Supplementary Material
Funding
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities under Award Number DP2MD010478 and the National Cancer Institute under Award Number 2R25CA057711 and the National Institute on Aging (grant P30-AG017253) through the Stanford Center on the Demography and Economics of Health and Aging.
References
- 1. United States Census Bureau : Available at https://www.census.gov/newsroom/facts-for-features/2017/veterans-day.html; accessed November 16, 2017.
- 2. Angrist JD, Chen SH, Frandsen BR: Did Vietnam veterans get sicker in the 1990s? The complicated effects of military service on self-reported health. J Public Econ 2010; 94(11–12): 824–37. 10.1016/j.jpubeco.2010.06.001. [DOI] [Google Scholar]
- 3. Booth SJ, Kevin M Schmiegel. Socioeconomic Status and Performance in the US Army and Marine Corps. 1998. Available at http://www.dtic.mil/dtic/tr/fulltext/u2/a345037.pdf; accessed May 12, 2017.
- 4. Eisenberg D, Rowe B: The effect of smoking in young adulthood on smoking later in life: evidence based on the Vietnam era draft lottery. Forum Health Econ Policy 2009; 12(2): 32p–p. 10.2202/1558-9544.1155. [DOI] [Google Scholar]
- 5. Schmitz L, Conley D: The long-term consequences of Vietnam-Era conscription and genotype on smoking behavior and health. Behav Genet 2015; 46(1): 43–58. 10.1007/s10519-015-9739-1. [DOI] [PubMed] [Google Scholar]
- 6. Dobkin C, Shabani R: The health effects of military service: evidence from the vietnam draft. Econ Inq 2009; 47(1): 69–80. 10.1111/j.1465-7295.2007.00103.x. [DOI] [Google Scholar]
- 7. Angrist JD, Chen SH, Song J: Long-term consequences of vietnam-era conscription: New estimates using social security data. Am Econ Rev 2011; 101: 334–8. 10.1257/aer.101.3.334. [DOI] [Google Scholar]
- 8. Turner S, Bound J: Closing the gap or widening the divide: the effects of the G. I. Bill and World War II on the educational outcomes of Black Americans. J Econ Hist 2013; 63(1): 145–77. [Google Scholar]
- 9. Bedard K, Deschênes O: the long-term service on health: evidence impact of military from World War II and Korean War Veterans. Am Econ Rev 2006; 96(1): 176–94. 10.1257/000282806776157731. [DOI] [PubMed] [Google Scholar]
- 10. Mokdad AH, Marks JS, Stroup DF, Gerberding JL: Actual causes of death in the United States, 2000. JAMA 2004; 291: 1238–45. 10.1001/jama.271.9.660c. [DOI] [PubMed] [Google Scholar]
- 11. Smith EA, Malone RE: Tobacco promotion to military personnel: “the plums are here to be pucked”. Mil Med 2009; 174(8): 797–806. 10.1016/j.surg.2006.10.010.Use. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith EA, Blackman VS, Malone RE: Death at a discount: how the tobacco industry thwarted tobacco control policies in US military commissaries. Tob Control 2007; 16(1): 38–46. 10.1136/tc.2006.017350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Joseph AM, Muggli M, Pearson KC, Lando H: The cigarette manufacturers’ efforts to promote tobacco to the U.S. Military. Mil Med 2005; 170(10): 874–80. [DOI] [PubMed] [Google Scholar]
- 14. Jahnke SA, Haddock CK, Poston WWC, Hyder ML, Lando H: A national survey of cigarette prices at military retail outlets. JAMA 2011; 306(22): 2456/2457 10.1093/ageing/afp226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Haddock CK, Hyder ML, Poston WSC, Jahnke SA, Williams LN, Lando H: A longitudinal analysis of cigarette prices in military retail outlets. Am J Public Health 2014; 104(4): 82–7. 10.2105/AJPH.2013.301660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bray RM, Hourani LL, Rae Olmsted KL, et al. Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel; 2006. Available at http://oai.dtic.mil/oai/oai?verb=getRecord&metadataPrefix=html&identifier=ADA465678; accessed April 12, 2017.
- 17. Kenkel DS, Lillard DR, Mathios AD: Accounting for misclassification error in retrospective smoking data. Health Econ 2004; 13(10): 1031–44. 10.1002/hec.934. [DOI] [PubMed] [Google Scholar]
- 18. Glied S: Youth tobacco control: reconciling theory and empirical evidence. J Health Econ 2002; 21: 117–35. 10.1016/S0167-6296(01)00118-7. [DOI] [PubMed] [Google Scholar]
- 19. Haas S: Trajectories of functional health: The “long arm” of childhood health and socioeconomic factors. Soc Sci Med 2008; 66(4): 849–61. 10.1016/j.socscimed.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 20. Eisner MD, Iribarren C, Yelin EH, et al. : Pulmonary Function and the Risk of Functional Limitation in Chronic Obstructive Pulmonary Disease. Am J Epidemiol 2008; 167(9): 1090–1101. 10.1093/aje/kwn025.Pulmonary. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Coultas DB, Mapel D, Gagnon R, Lydick EVA: The health impact of undiagnosed airflow obstruction in a national sample of United States adults. Am J Respir Crit Care Med 2001; 164(3): 372–7. 10.1164/ajrccm.164.3.2004029. [DOI] [PubMed] [Google Scholar]
- 22. Miller MR, Pedersen OF, Lange P, Vestbo J: Improved survival prediction from lung function data in a large population sample. Respir Med 2009; 103(3): 442–8. 10.1016/j.rmed.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 23. Vaz Fragoso CA, Gahbauer EA, Van Ness PH, Concato J, Gill TM: Peak expiratory flow as a predictor of subsequent disability and death in community-living older persons. J Am Geriatr Soc 2008; 56(6): 1014–20. 10.1111/j.1532-5415.2008.01687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Young RP, Hopkins R, Eaton TE: Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Respir J 2007; 30(4): 616–22. 10.1183/09031936.00021707. [DOI] [PubMed] [Google Scholar]
- 25. Sin DD, Wu L, Man SF: The relationship between reduced lung function and cardiovascular mortality: a population-based study and a systematic review of the literature. Chest 2005; 127(6): 1952–9. 10.1378/chest.127.6.1952. [DOI] [PubMed] [Google Scholar]
- 26. Schünemann HJ: Pulmonary function is a long-term predictor of mortality in the general population: 29-year follow-up of the Buffalo Health Study. CHEST J 2000; 118(3): 656 10.1378/chest.118.3.656. [DOI] [PubMed] [Google Scholar]
- 27. Cook NR, Evans DA, Scherr PA, et al. : Peak expiratory flow rate in an elderly population. Am J Epidemiol 1989; 130: 66–78. [DOI] [PubMed] [Google Scholar]
- 28. Roberts MH, Mapel DW: Limited lung function: impact of reduced peak expiratory flow on health status, health-care utilization, and expected survival in older adults. Am J Epidemiol 2012; 176(2): 127–34. 10.1093/aje/kwr503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stanley M: College education and the midcentury GI bills. Q J Econ 2003; 118(2): 671–708. 10.1162/003355303321675482. [DOI] [Google Scholar]
- 30. Congress US. Veterans Readjustment Assistance Act of 1952 United States of America; 1952. Available at https://www.gpo.gov/fdsys/pkg/STATUTE-66/pdf/STATUTE-66-Pg663.pdf; accessed January 23, 2014.
- 31. Bound J, Turner S: Going to war and going to college: did World War II and the G.I. bill increase educational attainment for returning veterans? J Labor Econ 2002; 20(4): 784–815. 10.1086/342012. [DOI] [Google Scholar]
- 32. Xie Y: The Socioeconomc status of young male veterans, 1964–1984. Soc Sci Q (University Texas Press) 1992; 73(2): 379–96. [Google Scholar]
- 33. Browning HL, Lopreato SC, Poston DL: Income and veteran status: variations among Mexican Americans, Blacks and Anglos. Am Sociol Rev 1973; 38(1): 74 10.2307/2094332. [DOI] [Google Scholar]
- 34. Sampson RJ, Laub JH: Socioeconomic achievement in the life course of disadvantaged men: military service as a turning point, Circa 1940-1965. Am Sociol Rev 1996; 61(3): 347–67. 10.2307/2096353. [DOI] [Google Scholar]
- 35. Fetter DK: How do mortgage subsidies affect home ownership? evidence from the mid-century GI bills. Am Econ J Econ Policy 2013; 5(2): 111–47. 10.1257/pol.5.2.111. [DOI] [Google Scholar]
- 36. Galea S, Nandi A, Vlahov D: The social epidemiology of substance use. Epidemiol Rev 2004; 26: 36–52. 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 37. Breslau N, Peterson EL, Schultz LR, Chilcoat HD, Andreski P: Major depression and stages of smoking. A longitudinal investigation. Arch Gen Psychiatry 1998; 55(2): 161–6. 10.1001/archpsyc.55.2.161. [DOI] [PubMed] [Google Scholar]
- 38. Royce JM, Corbett K, Sorensen G, Ockene J: Gender, social pressure, and smoking cessations: The community intervention trial for smoking cessation (COMMIT) at baseline. Soc Sci Med 1997; 44(3): 359–70. 10.1016/S0277-9536(96)00149-9. [DOI] [PubMed] [Google Scholar]
- 39. Weill H, Ziskind MM, Waggenspack C, Rossiter CE Lung Function Consequences of Dust Exposure in Asbestos Cement Manufacturing Plants. Arch Environ Health 1975; 30(2): 88–97. [DOI] [PubMed] [Google Scholar]
- 40. Coggon D, Taylor AN: Coal mining and chronic obstructive pulmonary disease: a review of the evidence. Thorax 1998; 53(5): 398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hajat A, Diez-Roux AV, Adar SD, et al. : Air pollution and individual and neighborhood socioeconomic status: Evidence from the multi-ethnic study of atherosclerosis (MESA). Environ Health Perspect 2013; 121(11–12): 1325–33. 10.1289/ehp.1206337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vable AM, Canning D, Glymour MM, Kawachi I, Jimenez MP, Subramanian SV: Can social policy influence socioeconomic disparities? Korean War GI Bill eligibility and markers of depression. Ann Epidemiol 2016; 26: 129–135.e3. 10.1016/j.annepidem.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. De Tray D: Veteran status as a screening device. Am Econ Rev 1982; 72(1): 133–42. 10.1257/jep.6.3.79. [DOI] [Google Scholar]
- 44. Heeringa SG, Connor JH Technical description of the Health and Retirement Survey sample design. Available at http://hrsonline.isr.umich.edu/sitedocs/userg/HRSSAMP.pdf; accessed September 20, 2014. [Google Scholar]
- 45. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR: Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol 2014; 576–85. 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Carvalhaes-Neto N, Lorino H, Gallinari C, et al. : Cognitive function and assessment of lung function in the elderly. Am J Respir Crit Care Med 1995; 152(5 Pt I): 1611–5. 10.1164/ajrccm.152.5.7582303. [DOI] [PubMed] [Google Scholar]
- 47. Bellia V, Pistelli R, Catalano F, et al. : Quality control of spirometry in the elderly: The SA.R.A. study. Am J Respir Crit Care Med 2000; 161(4 Pt I): 1094–1100. 10.1164/ajrccm.161.4.9810093. [DOI] [PubMed] [Google Scholar]
- 48. Licia P, Gianluca G, Silvia C, et al. : Quality of spirometric performance in older people. Age Ageing 2003; 32(February 1996): 43–6. [DOI] [PubMed] [Google Scholar]
- 49. Allen S, Yeung P, Janczewski M, Siddique N: Predicting inadequate spirometry technique and the use of FEV1/FEV3 as an alternative to FEV1/FVC for patients with mild cognitive impairment. Clin Respir J 2008; 2(4): 208–13. . [DOI] [PubMed] [Google Scholar]
- 50. Cook NR, Evans DA, Scherr PA, Speizer FE, Taylor JO, Hennekens CH: Peak expiratory flow rate and 5-year mortality in an elderly population. Am J Epidemiol 1991; 133(8): 784–94. [DOI] [PubMed] [Google Scholar]
- 51. Crimmins EM, Guyer H, Langa KM, Ofstedal MB, Wallace RB, Weir DR: Documentation of physical measures, anthropometrics and blood pressure in the Health and Retirement Study. Available at http://hrsonline.isr.umich.edu/sitedocs/userg/dr-011.pdf; accessed Septebmer 20, 2012. [Google Scholar]
- 52. Kuh D, Wadsworth M: Parental height: childhood environment and subsequent adult height in a national birth cohort. Int J Epidemiol 1989; 18(3): 663–8. [DOI] [PubMed] [Google Scholar]
- 53.Patricia St.Clair, Delia Bugliari, Nancy Campbell, et al: RAND HRS Data Documentation, Version L. RAND Center for the Study of Aging; 2011. Available at https://www.rand.org/content/dam/rand/www/external/labor/aging/dataprod/randhrsL.pdf; accessed September 20, 2012.
- 54. Snyder TDE. 120 Years of American Education: A Statistical Portrait; 1993. http://nces.ed.gov/pubs93/93442.pdf; accessed November 15, 2017.
- 55. Glymour MM, Avendano M, Haas S, Berkman LF: Lifecourse social conditions and racial disparities in incidence of first stroke. Ann Epidemiol 2008; 18(12): 904–12. 10.1016/j.annepidem.2008.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Luo Y, Waite LJ: The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life . J Gerontol Ser B Psychol Sci Soc Sci 2005; 60(2): S93–S101. 10.1093/geronb/60.2.S93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rowntree CL, McGill KH, Edwards TI: Causes of rejection and the incidence of defects. JAMA 1943; 123(4): 182–5. [Google Scholar]
- 58. Iacus SM, King G, Porro G: Causal inference without balance checking: coarsened exact matching. Polit Anal 2012; 20(1): 1–24. 10.1093/pan/mpr013. [DOI] [Google Scholar]
- 59. Victora C, Huttly S, Fuchs S, Olinto M: The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol 1997; 26(1): 224–7. 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- 60. King G, Nielsen R, Coberley C, Pope JE Comparative Effectiveness of Matching Methods for Causal Inference. Unpublished manuscript 2011. doi:10.1.1.230.3451.
- 61. Blackwell M, Iacus SM, King G, Porro G: Cem: Coarsened exact matching in Stata. Stata J 2009; 9(4): 524–46. [Google Scholar]
- 62. Conley D, Heerwig J: The long-term effects of military conscription on mortality: estimates from the Vietnam-era draft lottery. Demography 2012; 49(3): 841–55. 10.1007/s13524-012-0103-2. [DOI] [PubMed] [Google Scholar]
- 63. Smith EA, Malone RE: “Everywhere the soldier will be”: wartime tobacco promotion in the US military. Am J Public Heal 2009; 99(9): 1595–1602. 10.2105/AJPH.2008.152983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bondurant S, Wedge R: Combating tobacco use in military and veteran populations. Natl Academies Press 2009 10.17226/12632. [DOI] [PubMed] [Google Scholar]
- 65. Angrist JD, Chen SH: Schooling and the Vietnam-Era GI Bill: evidence from the draft lottery. Am Econ J Appl Econ 2011; 3: 96–119. 10.1257/app.3.2.96. [DOI] [Google Scholar]
- 66. Nunn AJ, Gregg I: New regression equations for predicting peak expiratory flow in adults. Br Med J 1989; 298: 1068–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Seltzer CC, Jablon S: Effects of selection on mortality. Am J Epidemiol 1974; 100(6): 367 10.1093/oxfordjournals.aje.a112157. [DOI] [PubMed] [Google Scholar]
- 68. Pugh MJ, Jaramillo CA, Leung K-W, et al. : Increasing prevalence of chronic lung disease in veterans of the wars in Iraq and Afghanistan. Mil Med 2016; 181(5): 476–81. 10.7205/MILMED-D-15-00035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.