Abstract
Osteoporosis is a major, growing healthcare issue. This is especially of concern in an ageing population like that of Singapore. Osteoporotic patients are at risk of fractures, which can result in increased morbidity and mortality. The use of antiresorptive therapy with bisphosphonates or denosumab has been proven to reduce fracture risk. However, the use of these medications has rarely been associated with the development of osteonecrosis of the jaw, a potentially debilitating condition affecting one or both jaws. Appropriate understanding of the patient’s antiresorptive therapy regime, as well as early institution of preventive dental measures, can play an important role in preventing medication-related osteonecrosis of the jaw (MRONJ). Regular monitoring and prompt referral to specialist care is warranted for patients with established MRONJ.
Keywords: bisphosphonates, osteonecrosis, osteoporosis, MRONJ
66-year-old Mrs Seah had a recent Colles’ fracture after she slipped and fell in her bathroom. She visited your clinic to review her bone mineral density test, which confirmed that she has osteoporosis (spine –2.6 standard deviation, hip –2.8 standard deviation). You advised her to take fall prevention measures as well as calcium and Vitamin D supplements. You also discussed starting her on alendronate, a bisphosphonate, to prevent further fractures. She returned two weeks later with a letter from her dentist. The dentist requested for Mrs Seah not to be started on the bisphosphonates, so as to avoid the risk of developing osteonecrosis of the jaw. Mrs Seah was very worried about this and asked for the medication to be changed.
WHAT IS OSTEOPOROSIS AND WHAT ARE ITS COMPLICATIONS?
Osteoporosis is a major non-communicable disease characterised by reduced bone mass and disruption of bone architecture, resulting in increased bone fragility and fracture risk. The condition has long been identified as a significant healthcare issue worldwide,(1) especially in countries with an ageing population such as Singapore. It was forecast that by 2030, one out of five persons residing in Singapore will be 65 years old and above.(2) Therefore, the incidence of osteoporosis with its associated fractures is likely to increase over the coming decades.
Worldwide, the lifetime risk for hip, vertebral and forearm (wrist) fractures has been estimated to be approximately 40%, similar to that for coronary heart disease.(1) Fractures are of particular concern in the elderly osteoporotic patient. According to the Asian Osteoporosis Study published in 2001, by the next century, 50% of all hip fractures in the world will occur in Asia.(3) The Singapore Ministry of Health (MOH) Clinical Practice Guidelines on Osteoporosis have reported that since the 1960s, hip fractures have increased by 1.5 times in men and five times in women.(2) The incidence of hip fracture in Singapore is estimated to be 402 out of 100,000 women and 152 out of 100,000 men, making it one of the highest incidences in Asia.(4) Apart from resulting in fractures, osteoporosis may also cause patients to become bedridden with secondary complications that may be life-threatening.(1)
Numerous factors contribute to the risk of osteoporosis and fractures. To aid in treatment decision-making, fracture risk can be assessed using the WHO Fracture Risk Assessment (FRAX™) tool,(5) which takes into account the morbidity and economic burden.(2,6,7) It was reported by MOH that the mortality rate one year after experiencing a hip fracture is approximately 20%–27%. One-fifth of patients who survive the fracture either become semi- or fully-dependent, and 39% are affected by reduced mobility.(2) Patients who survive the event but are left with residual impairment to mobility and self-care require long-term nursing care and rehabilitation. This contributes to economic costs for the patients and society.
WHAT IS MEDICATION-RELATED OSTEONECROSIS OF THE JAW?
Osteonecrosis of the jaw is a rare adverse effect that may occur in patients being treated for osteoporosis with antiresorptive medications.(8) A position paper issued by the American Association of Oral and Maxillofacial Surgeons (AAOMS) in 2014 suggested the term medication-related osteonecrosis of the jaw (MRONJ). This was in recognition of the potential for other antiresorptive and antiangiogenic medications, apart from bisphosphonates, to cause osteonecrosis of the jaw,(9) such as the human monoclonal antibody, denosumab. This article provides advice on the possible risks of developing MRONJ in these patients, as well as the recommended preventive and management strategies for such patients, from a multidisciplinary team perspective.
HOW RELEVANT IS THIS TO MY PRACTICE?
Management of osteoporosis
Osteoporosis management aims to reduce the impact of the condition and its associated complications. Each fragility fracture incurred increases the risk of future fractures: research has shown that 50% of those who break their hip previously presented with a minimal trauma (fragility) fracture and that a prior fracture is associated with an 86% increased risk of any fracture in the future.(10,11) The risk of a future fracture can be reduced by up to 80% if the root causes (i.e. osteoporosis and falls) are appropriately managed. Antiresorptive agents such as alendronate, risedronate, zoledronic acid and denosumab have also demonstrated evidence of future fracture risk reduction, by as much as 70% in one year.(12-16) Patients that demonstrated the greatest fracture reduction were women with lower bone mineral density, osteoporotic patients with T-score ≤ –2.5, and patients with a previous fragility fracture.(2,17) Patients with osteoporosis can be treated by administration of antiresorptive medications via the oral route, the parenteral route, or both.
However, treatment gaps are prevalent; worldwide, only 10%–20% of patients with osteoporosis are diagnosed and 8% are commenced on treatment. Compliance is also a major barrier, with 10% remaining on treatment at five years. In Singapore, it was estimated that only 16% of patients were started on treatment for their osteoporosis within two years of hip fracture.(18) Studies have shown that the rates of bisphosphonate prescription have declined significantly from 15% to 3% since 2004 in countries such as the United States, as a result of the media attention that bisphosphonates received after Food and Drug Administration safety announcements, despite the known benefits of these drugs in preventing patients from sustaining osteoporotic fractures.(19) To this end, it is of utmost importance that patients be appropriately informed about their diagnosis and the availability of effective or proven treatments, with primary care physicians serving as accurate sources of information in the community.
Diagnosis of MRONJ
Osteonecrosis of the jaw was first associated with bisphosphonate therapy in a 2003 report, which involved patients with metastatic cancer who received high-dose intravenous (IV) bisphosphonate therapy. MRONJ can be diagnosed clinically based on the following characteristics described in the AAOMS position paper:(9,20) (a) current or previous treatment with antiresorptive or antiangiogenic agents; (b) exposed bone or bone that can be probed through an intraoral or extraoral fistula in the maxillofacial region that has persisted for more than eight weeks; and (c) no history of radiation therapy to the jaws or obvious metastatic disease to the jaw.
Risk of MRONJ from oral bisphosphonate therapy
In numerous studies that were conducted to evaluate the risk of MRONJ in patients on oral bisphosphonate therapy, the overall risk of developing MRONJ was found to be low.(9,21) The risk of developing MRONJ in postmenopausal patients on oral bisphosphonate was reported to be between one in 1,262 and one in 4,419 (0.02%–0.07%).(22) This was slightly lower than the estimated risk of 0.1% reported in the AAOMS position paper. However, based on the limited information available, the incidence of MRONJ occurring in patients was found to double, from 0.1% to 0.21%, if they were on oral bisphosphonates therapy for more than four years.(9)
Risk of MRONJ from intravenous bisphosphonate/denosumab therapy
According to the AAOMS position paper, osteoporotic patients receiving yearly administration of bisphosphonate therapy via the IV route were found to have a 0.017% risk of developing MRONJ. This percentage did not appear to increase even when the duration of therapy was longer than four years.(9) Other studies reported a risk of up to 0.35% in patients on IV bisphosphonate.(8) The risk of developing MRONJ while on denosumab was reported to be around 0.04%,(9) although research conducted in the United Kingdom reported a risk of up to 0.3%.(21) Osteoporotic patients on IV bisphosphonate or denosumab therapy are generally given much lower dosages and frequencies of medication, as compared to oncology patients on therapy for prevention of skeletal-related events and metastases in cancer.
Other medical factors were found to increase the risk of developing MRONJ. These include: duration of therapy, chemotherapy, erythropoietin therapy, renal dialysis, hypothyroidism, corticosteroid therapy and diabetes mellitus.(8,9,20) The patient’s age, smoking habit and obesity are also significant contributing factors.(20) It is important to emphasise good dental hygiene and practices in these patients to avoid the rare side effect of MRONJ.
Box 1 summarises the risk of developing MRONJ associated with various types of therapy.
Box 1.
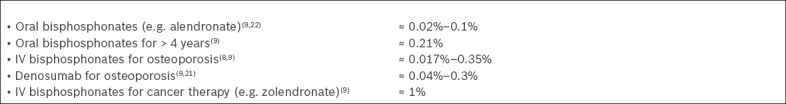
Risk of developing MRONJ:
WHAT CAN I DO IN MY PRACTICE?
Fig. 1 summarises the recommended management of osteoporotic patients, including those with MRONJ.
Fig. 1.
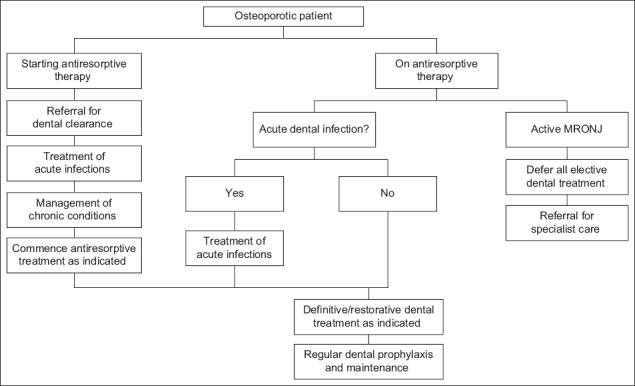
Flowchart shows the recommended management of osteoporotic patients. Definitive and restorative procedures include dental extractions, dental implant placement and prosthetic treatment. MRONJ: medication-related osteonecrosis of the jaw
Dental treatment in patients on antiresorptive therapy
Dental infections and invasive treatments are the most common factors that result in the development of MRONJ. Teeth that require extraction are often associated with periapical and periodontal infections. Infection and inflammation, dental extractions, irritation and trauma to the oral mucosa from ill-fitting oral appliances can result in an increased risk of developing MRONJ.(9,20,23-26)
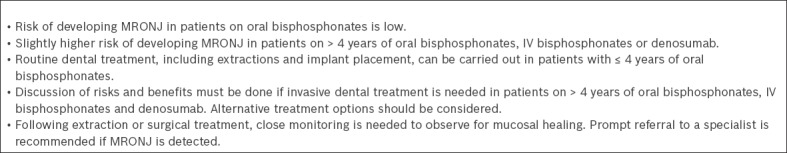
However, it should be noted that MRONJ can also occur spontaneously even without any obvious pre-existing dental infections or treatment,(21) and the risk of MRONJ in patients undergoing dental treatment should be assessed with this in mind. Studies have shown that 20%–33% of cases of MRONJ occur spontaneously in patients on antiresorptive therapy.(20) The incidence of MRONJ in patients treated with antiresorptive medications was reported to be comparable to the risk of MRONJ developing spontaneously in patients only exposed to placebo medications (0.017%–0.04% vs. 0%–0.02%, respectively).(9) Box 2 provides useful information for physicians with patients on antiresorptive therapy who require dental treatment.
Box 2.
Dental treatment for patients on antiresorptive therapy:(9,20,21,27,28)
Prevention of MRONJ
General practitioners should optimise patients’ medical condition prior to commencement of antiresorptive therapy. Modifiable medical conditions and factors that increase the risk of MRONJ should be properly managed. Physicians should advise their patients to stop smoking and reduce alcohol intake.(9,21) Patients should be referred to a dental practitioner for dental clearance to rule out and treat any dental diseases before starting antiresorptive therapy. Adequate time of approximately one month or more should be provided for the dentist to complete treatment of acute conditions, as well as to put in place a preventive oral hygiene plan. Management of any chronic dental conditions can be started concurrently while managing the acute problems.
A thorough dental clearance includes a thorough clinical and radiographic examination. Proper oral hygiene and preventive practices must be instituted. Dietary modifications to reduce sugar intake should be done to prevent dental caries (tooth decay) and the need for dental extractions. A study by Dimopoulos et al demonstrated a significant reduction in MRONJ occurrence in patients who received preventive dental treatment prior to commencing therapy.(29) These findings were further supported by Bonacina et al and Vandone et al, who discovered no new cases of MRONJ in patients who underwent dental clearance, and that the overall risk of developing MRONJ was halved.(30,31) Acute infections such as abscesses of pulpal or periodontal origin must be treated to remove the source of infection. This treatment should be carried out prior to or even during antiresorptive therapy, as the presence of infection and inflammation is a well-recognised risk factor for development of MRONJ.(26) Chronic periodontal conditions must also be managed to avoid further bony and gingival recession and subsequent tooth loss. Dental therapy aimed at removing infection and inflammation can be done in a primary dental care setting and as part of a preventive treatment strategy against MRONJ. It has been reported that dental extraction is a major factor in the development of MRONJ, such as in Filleul et al, where 67% of cases of bisphosphonate-related osteonecrosis of the jaw were precipitated by dental extractions.(25) This was similar to the range reported by AAOMS of 52%–61%, which corresponded to a risk of 0.09%–0.34%.(19) However, it is still necessary to actively treat or remove teeth that can be a source of infection and inflammation, in order to avoid an increase in MRONJ risk.
In general, patients on antiresorptive therapy for management of osteoporosis have a low risk of developing MRONJ. As mentioned earlier, the reported incidence of MRONJ developing in patients on oral bisphosphonates for less than four years was 0.1% or less; this is lower than the incidence of sustaining an injury from a road traffic accident in Singapore, which was 0.12% in 2016.(32)
Patients with uncomplicated medical histories who are on oral bisphosphonates can undergo routine dental treatment and extractions in a dental primary care setting.(9,21) The incidence of MRONJ occurring after dental extractions in patients on oral bisphosphonates was low, at 0.09%–0.5%. It has been suggested that minimally traumatic extraction techniques, trimming off of sharp bony edges and achieving mucosal closure wherever possible would decrease the risk of MRONJ development.(25) Early follow-up of about eight weeks after extraction should be done to monitor for healing and mucosal coverage of the extraction socket.(21)
Dental implants can also be placed in patients with less than five years of oral bisphosphonate therapy,(20,27) with no reported increase in MRONJ risk or implant loss. High implant success rates (95%) were also reported.(28) Nonetheless, proper informed consent weighing the risk and benefits of invasive dental procedures must be done prior to the commencement of treatment. Complicated dental surgical procedures should be referred to a specialist for management.
Patients on long-term oral bisphosphonates (> 4 years), IV bisphosphonates, and denosumab are at a slightly higher risk of developing MRONJ.(9) Therefore, it is extremely important to institute a personalised preventive plan, as well as to make the necessary lifestyle and dietary modifications. Routine dental treatment can still be carried out in a dental primary care setting. Alternative treatments to dental extractions should be considered and carried out, if possible.(9,21) Should dental extractions be necessary, a proper informed consent weighing the risk and benefits of the dental treatment must be done with the patient. The procedure should be carried out in an atraumatic manner, with mucosal closure if possible. The AAOMS position paper advocates a ‘drug holiday’ of at least two months before the procedure if there are no contraindications due to the patient’s systemic condition. The antiresorptive medication is only resumed after osseous healing is observed.(9) However, clinicians should be aware that the overall value of a ‘drug holiday’ has not been adequately proven, and the effects of bisphosphonates on bone turnover are known to persist for many months.(21) Consideration of the patient’s fracture risk must also be done, and a ‘drug holiday’ may be contraindicated in a high fracture risk patient.(33) Prophylactic antibiotics are not required unless indicated by other systemic conditions.(21)
Management of MRONJ
Patients diagnosed with MRONJ should not undergo any elective dental surgical procedures. The management of MRONJ is dependent on the stage of the condition, as well as the corresponding symptoms and effects on the patient’s daily life and functioning. Prompt referral to an oral and maxillofacial surgeon for further management is warranted. Treatment of MRONJ ranges from observation, local debridement or sequestrectomy, to resection of necrotic bone with or without reconstruction with vascularised free flap.(9)
TAKE HOME MESSAGES
Osteoporosis and its associated risk of fractures is a major, growing healthcare issue in Singapore’s ageing population.
Osteoporotic fractures are associated with increased morbidity and mortality
Antiresorptive therapies (e.g. bisphosphonates and denosumab) are proven to reduce fracture risk in osteoporotic patients.
The risk of MRONJ formation in osteoporotic patients on antiresorptive therapy is real but low.
Routine dental treatment and invasive dental treatment such as extractions and implants can be carried out for the majority of osteoporotic patients on antiresorptive therapy.
After a discussion with Mrs Seah, you convinced her that the risk of developing medication-related osteonecrosis of the jaw from taking alendronate is low and that the benefit of reducing her fracture risk clearly outweighs the risk. You also prepared a list of related journal articles, which she passed to her dentist. Upon reading them, her dentist was willing to provide routine dental treatment. Mrs Seah commenced alendronate therapy after receiving dental clearance.
REFERENCES
- 1.World Health Organization. WHO Technical Report Series 921. Prevention and Management of Osteoporosis: Report of a WHO Scientific Group [online] [Accessed January 9, 2018]. Available at: http://apps.who.int/iris/bitstream/10665/42841/1/WHO_TRS_921.pdf .
- 2.Ministry of Health Singapore. Osteoporosis: MOH Clinical Practice Guidelines 3/2008. [Accessed January 9, 2018]. Available at: https://www.moh.gov.sg/content/dam/moh_web/HPP/Doctors/cpg_medical/withdrawn/cpg_Osteoporosis.pdf .
- 3.Lau EM, Lee JK, Suriwongpaisal P, et al. The incidence of hip fracture in four Asian countries: The Asian Osteoporosis Study (AOS) Osteoporos Int. 2001;12:239–43. doi: 10.1007/s001980170135. [DOI] [PubMed] [Google Scholar]
- 4.Koh LK, Saw SM, Lee JJ, Leong KH, Lee J, National Working Committee on Osteoporosis Hip fracture incidence rates in Singapore 1991-1998. Osteoporos Int. 2001;12:311–8. doi: 10.1007/s001980170121. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Fracture Risk Assessment. [Accessed January 9, 2018]. Available at: https://www.sheffield.ac.uk/FRAX/
- 6.Tan LT, Wong SJ, Kwek EB. Inpatient cost for hip fracture patients managed with an orthogeriatric care model in Singapore. Singapore Med J. 2017;58:139–44. doi: 10.11622/smedj.2016065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee YH, Lim YW, Lam KS. Economic cost of osteoporotic hip fractures in Singapore. Singapore Med J. 2008;49:980–4. [PubMed] [Google Scholar]
- 8.Anagnostis P, Stevenson JC. Bisphosphonate drug holidays--when, why and for how long? Climacteric. 2015;18(Suppl2):32–8. doi: 10.3109/13697137.2015.1099092. [DOI] [PubMed] [Google Scholar]
- 9.American Association of Oral and Maxillofacial Surgeons. Position Paper: Medication-Related Osteonecrosis of the Jaw—2014 Update. [Accessed January 9, 2018]. Available at: https://www.aaoms.org/docs/govt_affairs/advocacy_white_papers/mronj_position_paper.pdf .
- 10.Port L, Center J, Briffa NK, et al. Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int. 2003;14:780–4. doi: 10.1007/s00198-003-1452-x. [DOI] [PubMed] [Google Scholar]
- 11.Edwards BJ, Bunta AD, Simonelli C, Bolander M, Fitzpatrick LA. Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res. 2007;461:226–30. doi: 10.1097/BLO.0b013e3180534269. [DOI] [PubMed] [Google Scholar]
- 12.Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–41. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 13.Harris ST, Watts NB, Genant HK, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–52. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 14.Black DM, Thompson DE, Bauer DC, et al. Fracture Intervention Trial Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85:4118–24. doi: 10.1210/jcem.85.11.6953. [DOI] [PubMed] [Google Scholar]
- 15.Lyles KW, Colón-Emeric CS, Magaziner JS, et al. HORIZON Recurrent Fracture Trial Zoledronic acid in reducing clinical fracture and mortality after hip fracture. N Engl J Med. 2007;357 doi: 10.1056/NEJMoa074941. nihpa40967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cummings SR, Martin JS, McClung MR, et al. FREEDOM Trial Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 17.Levis S, Theodore G. Summary of AHRQ's comparative effectiveness review of treatment to prevent fractures in men and women with low bone density or osteoporosis: update of the 2007 report. J Manag Care Pharm. 2012;18(4 Suppl B):S1–15. doi: 10.18553/jmcp.2012.18.s4-b.1. discussion S13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chandran M, Tan MZ, Cheen M, et al. Secondary prevention of osteoporotic fractures--an “OPTIMAL” model of care from Singapore. Osteoporos Int. 2013;24:2809–17. doi: 10.1007/s00198-013-2368-8. [DOI] [PubMed] [Google Scholar]
- 19.Kim SC, Kim DH, Mogun H, et al. Impact of the U.S. Food and Drug Administration's safety-related announcements on the use of bisphosphonates after hip fracture. J Bone Miner Res. 2016;31:1536–40. doi: 10.1002/jbmr.2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mücke T, Krestan CR, Mitchell DA, Kirschke JS, Wutzl A. Bisphosphonate and medication-related osteonecrosis of the jaw: a review. Semin Musculoskelet Radiol. 2016;20:305–14. doi: 10.1055/s-0036-1592367. [DOI] [PubMed] [Google Scholar]
- 21.Scottish Dental Clinical Effectiveness Programme. Oral health management of patients at risk of medication-related osteonecrosis of the jaw. [Accessed January 9, 2018]. Available at: http://www.sdcep.org.uk/wp-content/uploads/2017/04/SDCEP-Oral-Health-Management-of-Patients-at-Risk-of-MRONJ-Guidance-full.pdf .
- 22.Tanna N, Steel C, Stagnell S, Bailey E. Awareness of medication related osteonecrosis of the jaws (MRONJ) amongst general dental practitioners. Br Dent J. 2017;222:121–5. doi: 10.1038/sj.bdj.2017.79. [DOI] [PubMed] [Google Scholar]
- 23.Furuya T, Maeda S, Momohara S, Taniguchi A, Yamanaka H. Dental treatments, tooth extractions, and osteonecrosis of the jaw in Japanese patients with rheumatoid arthritis: results from the IORRA cohort study. J Bone Miner Metab. 2017;35:344–50. doi: 10.1007/s00774-016-0763-x. [DOI] [PubMed] [Google Scholar]
- 24.Lescaille G, Coudert AE, Baaroun V, et al. Osteonecrosis of the jaw and nonmalignant disease: is there an association with rheumatoid arthritis? J Rheumatol. 2013;40:781–6. doi: 10.3899/jrheum.120810. [DOI] [PubMed] [Google Scholar]
- 25.Filleul O, Crompot E, Saussez S. Bisphosphonate-induced osteonecrosis of the jaw: a review of 2,400 patient cases. J Cancer Res Clin Oncol. 2010;136:1117–24. doi: 10.1007/s00432-010-0907-7. [DOI] [PubMed] [Google Scholar]
- 26.Yamagata K, Uchida F, Kanno N, Yanagawa T, Bukawa H. Medication-related osteonecrosis of the jaw. InTech [online] 2017. [Accessed January 9, 2018]. Available at: https://www.intechopen.com/books/osteonecrosis/medication-related-osteonecrosis-of-the-jaw .
- 27.Advisory Task Force on Bisphosphonate-Related Osteonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007;65:369–76. doi: 10.1016/j.joms.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Jeffcoat MK. Safety of oral bisphosphonates: controlled studies on alveolar bone. Int J Oral Maxillofac Implants. 2006;21:349–53. [PubMed] [Google Scholar]
- 29.Dimopoulos MA, Kastritis E, Bamia C. Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventive measures in patients with multiple myeloma treated with zoledronic acid. Ann Oncol. 2009;20:117–20. doi: 10.1093/annonc/mdn554. [DOI] [PubMed] [Google Scholar]
- 30.Bonacina R, Mariani U, Villa F, Villa A. Preventive strategies and clinical complications for bisphosphonate-related osteonecrosis of the jaw: a review of 282 patients. J Can Dent Assoc. 2011;77:b147. [PubMed] [Google Scholar]
- 31.Vandone AM, Donadio M, Mozzati M. Impact of dental care in the prevention of bisphosphonate-associated osteonecrosis of the jaw: a single-center clinical experience. Ann Oncol. 2012;23:193–200. doi: 10.1093/annonc/mdr039. [DOI] [PubMed] [Google Scholar]
- 32.Singapore Police Force. Annual Road Traffic Situation 2016. [Accessed January 9, 2018]. Available at: https://www.police.gov.sg/~/media/spf/files/statistics/20170215_stats_road_traffic_situation_2016.pdf .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


