Abstract
A 72‐year‐old Japanese woman presented with a fever, diarrhea, intermittent spotting, and constant fluid discharge from the vagina. Imaging studies revealed an enterovaginal fistula. She underwent radical hysterectomy and radiotherapy 35 years previously. She also had a surgical history of nephrostomy, nephrectomy, ileoascending anastomosis, and colostomy. As bleeding from the enterovaginal fistula was uncontrollable, ileocecal resection was performed. However, a colovesical fistula with urinary tract infection occurred 3 months later. The present case indicates that fistula formation occurs and causes various symptoms in patients who underwent postpelvic radiotherapy, particularly in those with prior surgeries in the irradiated field.
Keywords: colovesical fistula, enterovaginal fistula, gastrointestinal fistula, radiation‐related complications, urinary tract infection
1. INTRODUCTION
Radiation has been widely used for treating malignant diseases in the pelvic cavity such as cancers of the colorectum, urinary tract, prostate, uterus, and adnexa uteri. Pelvic radiotherapy has a close relation to radiotherapy‐related gastrointestinal complications, because irradiated tissue becomes increasingly deoxygenated and wound healing impaired.1 Such complications vary and include mucosal erosions and ulcers, intestinal stenosis, perforation, and fistula formation.2
Recently, we treated a patient with enterovaginal and colovesical fistulas. The patient had a history of pelvic radiotherapy for the treatment of uterus carcinoma 35 years previously. She also had multiple surgical histories of the urinary and gastrointestinal tract. Bleeding from the enterovaginal fistula was not controllable and thus required surgical management. This case indicates that pelvic radiotherapy has a potential to cause life‐threatening gastrointestinal complications after an extended period. Moreover, although some of such patients may require surgical salvage for radiotherapy‐related complications, surgical stress has a risk of inducing fistula formations.
2. CASE REPORT
A 72‐year‐old Japanese woman presented to our hospital for further examination because of a high fever, diarrhea, intermittent spotting into urine‐absorbing pads, and constant fluid discharge from the vagina. The patient had been taking Lactobacillus preparation, potassium chloride, vitamin D analogue, vitamin B12, vitamin B complex, and iron sulfate for diarrhea and subsequent malabsorption. Warfarin was also prescribed for deep vein thrombosis of the lower limbs. She underwent radical hysterectomy and radiotherapy for the treatment of carcinoma of the uterine cervix 35 years previously. After the treatment of cervix cancer, she developed bilateral hydronephrosis and multiple episodes of ileus. Thus, right percutaneous nephrostomy, left nephrectomy, ileoascending anastomosis, and colostomy in the transverse colon were performed (Figure 1). These treatments caused radiation colitis and short bowel syndrome, resulting in diarrhea, malabsorption, and protein‐losing enteropathy.
Figure 1.
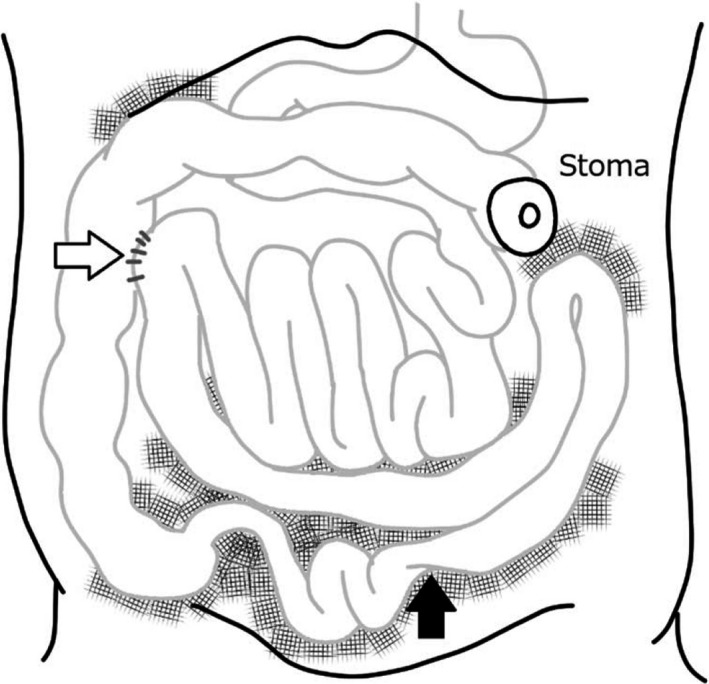
A schematic image of the patient's abdomen. As she developed bilateral hydronephrosis and multiple episodes of ileus, ileoascending anastomosis (white arrow) and colostomy in the transverse colon were performed. Mesh patterns indicate adhesions of the intestines because of previous surgeries and irradiation. Black arrow indicates the location of the enterovaginal fistula formation
Physical examination revealed anemia and leg edema. Laboratory examinations revealed anemia (red blood cell count, 266 × 104/mm3 and hemoglobin, 8.4 mg/dL), hypoproteinemia (total protein, 4.5 g/dL and albumin, 1.0 g/dL), hypokalemia (potassium, 2.5 mmol/L), hypocalcemia (calcium, 6.6 mg/dL), and hypophosphatemia (phosphorus, 2.1 mg/dL). A slight elevation in the C‐reactive protein level was noted (1.73 mg/dL), whereas the white blood cell count was decreased (3180/mm3; neutrophil, 74.0%).
Although fistula formation was suspected as a cause of intermittent blood spotting and constant fluid discharge from the vagina, computed tomography (CT) scanning with contrast media, colonoscopy, and video capsule enteroscopy examinations were nondiagnostic. The patient accidentally slipped and fell on the floor and hit her hip. Subsequently, massive bleeding from the vagina occurred, and pelvic examinations by a gynecologist revealed enterovaginal fistulas. A colposcopy examination using a videoscope (GIF TYPE PQ260; Olympus) showed two fistulas with active bleeding (Figure 2A‐C). Contrast medium (meglumine sodium amidotrizoate) was injected into the fistulas via the videoscope, and CT scanning confirmed the fistula formations between the ileum and vagina (Figure 2D,E). As the bleeding was uncontrollable, ileocecal resection was performed. Discharge of the blood and fluid resolved postoperatively.
Figure 2.
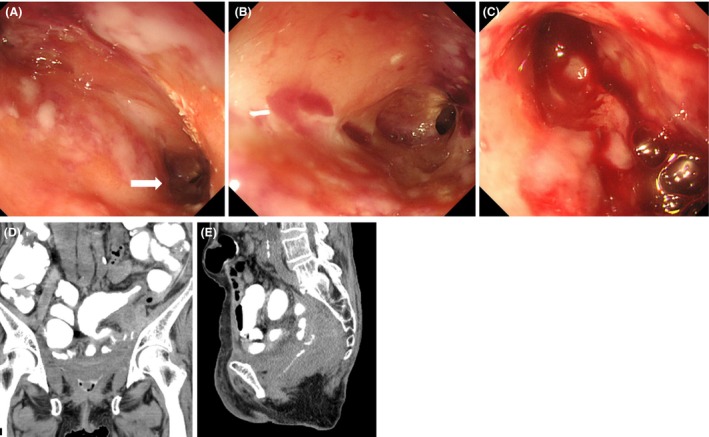
Videoscope revealing two fistulas in the vagina (A). Close‐up observation of the left fistula (A, arrow) showing the cavity (B). Active bleeding is observed from the right fistula (C). Collection of the contrast medium in the vagina (D) and fistula formations between the ileum and vagina (E) are observed after injecting contrast medium
Three months postoperatively, she presented with a low‐grade fever. Urinalysis revealed bacteriuria, and Klebsiella pneumoniae and Serratia species were detected by urine culture. A CT scan showed fluid collection in the pelvic cavity (Figure 3A). Colonoscopy from the anus revealed mucosal edema (Figure 3B) and stricture (Figure 3C) of the sigmoid colon. After the injection of contrast medium, a fistula in the bladder was visualized (Figure 3D, arrowhead), in addition to the pooling of contrast medium in the descending colon (Figure 3D,E, arrows). Consequently, a colovesical fistula was diagnosed. The urinary tract infection because of the fistula was conservatively treated with an injection of cefmetazole. The patient has been free from infection‐related symptoms for 4 months even after discontinuing the antibiotic treatment.
Figure 3.
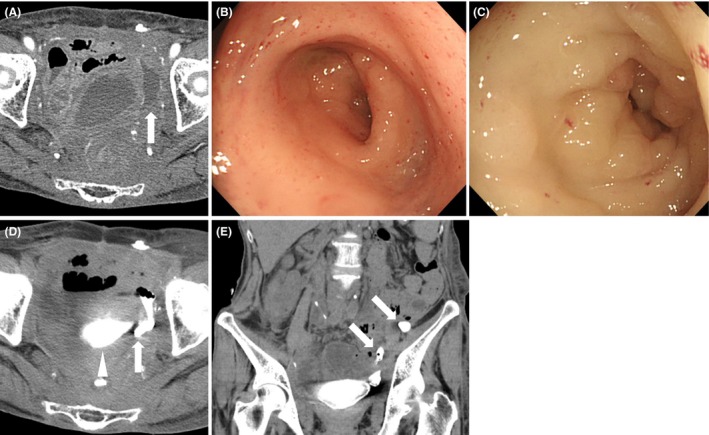
Fluid collection in the pelvic cavity is observed (A, arrow). Colonoscopy examination revealing mucosal edema (B) and stricture (C) in the sigmoid colon. After the injection of contrast medium via a colonoscope, the contrast medium flows into the space (D‐E, arrows) and urinary bladder (D, arrowhead)
3. DISCUSSION
In this case report, the patient presented with an enterovaginal fistula. She had multiple surgical histories of nephrostomy, nephrectomy, ileoascending anastomosis, and colostomy for the treatment of hydronephrosis and ileus. It has long been recognized that an invasive surgical procedure on previously irradiated areas increases the risk of developing infections, delayed wound healing, tissue necrosis, and fistula formation.3, 4, 5, 6, 7 For example, Galland et al8 retrospectively investigated 51 patients who underwent surgery for radiation enteritis, and they found postsurgical complications in 20 patients (39.2%), including stricture (N = 8), malabsorption (N = 5), and fistula (N = 1). Therefore, in the present patient, previous multiple surgeries may be associated with the development of an enterovaginal fistula. Moreover, bleeding from the enterovaginal fistula required surgical management, and the surgery may cause subsequent colovesical fistula formation.
Generally, radiotherapy‐related gastrointestinal complications occur within 2 years from the time of irradiation.9 For example, a review of 88 patients with radiation‐induced proctosigmoiditis revealed that the peak incidence of bleeding occurred after a 9‐month latent period after radiation treatment.10 A British multicentered survey including 541 women treated with radiotherapy with or without chemotherapy for cervical and endometrial cancer identified 152 women with bowel symptoms.11 The median time between completion of radiotherapy and emergence of bowel symptoms was 8 months in the patients with cervical cancer and 10 months in those with endometrial cancer. However, a retrospective study of 22 patients with rectourethral fistula reported that the time from the last radiation treatment to fistula presentation was 6 months to as long as 20 years (median: 25 months), indicating that fistulas can be formed even after an extended period from completion of radiotherapy.12 Our patient's clinical course reinforced this notion because the healing process is permanently altered by poor tissue perfusion and oxygenation because of vascular injuries after pelvic radiation. It should also be considered that surgical stress may lead to further fistula formation.
Management of the pelvic radiotherapy‐related fistula between the gastrointestinal tract and other organs should be tailored to the individual case. Surgical procedures for treating fistulas include interposition grafts, fecal diversion to a colostomy, resection of the fistula and responsive intestine, and pelvic exenteration.13 In some patients, local repair of the fistula can be treated by the transposition of healthy, vascularized tissue to the enterovaginal or rectovaginal fistulas. Although resection of the intestine forming the fistula or exenteration of the pelvic organs is a radical treatment, diversion of the gastrointestinal tract may be the only feasible treatment in patients with multiple comorbidities. As previously described, the irradiated field is often an inadequate operative environment with significant risks of complications and extensive adhesions.14 Thorough preoperative planning with imaging studies is essential for a successful outcome. In the present case, contrast radiography was useful for detecting the fistulas and deciding the treatment strategies.13, 14
4. CONCLUSIONS
We treated a patient with enterovaginal and colovesical fistulas that occurred 35 years after pelvic radiotherapy. Fistula formation should be considered as a differential diagnosis for various symptoms in patients with a history of pelvic radiation, particularly in those with prior surgeries in the irradiated field, because pelvic tissues may continue to accumulate, leaving them vulnerable to recurrent complications.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Iwamuro M, Hasegawa K, Hanayama Y, et al. Enterovaginal and colovesical fistulas as late complications of pelvic radiotherapy. J Gen Fam Med. 2018;19:166–169. 10.1002/jgf2.184
REFERENCES
- 1. Feddock J, Randall M, Kudrimoti M, et al. Impact of post‐radiation biopsies on development of fistulae in patients with cervical cancer. Gynecol Oncol. 2014;133:263–7. [DOI] [PubMed] [Google Scholar]
- 2. Deitel M, To TB. Major intestinal complications of radiotherapy. Management and nutrition. Arch Surg. 1987;122:1421–4. [DOI] [PubMed] [Google Scholar]
- 3. Payne WG, Walusimbi MS, Blue ML, Mosiello G, Wright TE, Robson MC. Radiated groin wounds: pitfalls in reconstruction. Am Surg. 2003;69:994–7. [PubMed] [Google Scholar]
- 4. Marchetta FC, Sako K, Maxwell W. Complications after radical head and neck surgery performed through previously irradiated tissues. Am J Surg. 1967;114:835–8. [DOI] [PubMed] [Google Scholar]
- 5. Joseph DL, Shumrick DL. Risks of head and neck surgery in previously irradiated patients. Arch Otolaryngol. 1973;97:381–4. [DOI] [PubMed] [Google Scholar]
- 6. Gürlek A, Miller MJ, Amin AA, et al. Reconstruction of complex radiation‐induced injuries using free‐tissue transfer. J Reconstr Microsurg. 1998;14:337–40. [DOI] [PubMed] [Google Scholar]
- 7. Douville EC, Asaph JW, Dworkin RJ, et al. Sternal preservation: a better way to treat most sternal wound complications after cardiac surgery. Ann Thorac Surg. 2004;78:1659–64. [DOI] [PubMed] [Google Scholar]
- 8. Galland RB, Spencer J. The natural history of clinically established radiation enteritis. Lancet. 1985;1:1257–8. [DOI] [PubMed] [Google Scholar]
- 9. Debeche‐Adams TH, Bohl JL. Rectovaginal fistulas. Clin Colon Rectal Surg. 2010;23:99–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gilinsky NH, Burns DG, Barbezat GO, Levin W, Myers HS, Marks IN. The natural history of radiation‐induced proctosigmoiditis: an analysis of 88 patients. Q J Med. 1983;52:40–53. [PubMed] [Google Scholar]
- 11. Kuku S, Fragkos C, McCormack M, Forbes A. Radiation‐induced bowel injury: the impact of radiotherapy on survivorship after treatment for gynaecological cancers. Br J Cancer. 2013;109:1504–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lane BR, Stein DE, Remzi FH, Strong SA, Fazio VW, Angermeier KW. Management of radiotherapy induced rectourethral fistula. J Urol. 2006;175:1382–7. [DOI] [PubMed] [Google Scholar]
- 13. Narayanan P, Nobbenhuis M, Reynolds KM, Sahdev A, Reznek RH, Rockall AG. Fistulas in malignant gynecologic disease: etiology, imaging, and management. Radiographics. 2009;29:1073–83. [DOI] [PubMed] [Google Scholar]
- 14. Hogan NM, Kerin MJ, Joyce MR. Gastrointestinal complications of pelvic radiotherapy: medical and surgical management strategies. Curr Probl Surg. 2013;50:395–407. [DOI] [PubMed] [Google Scholar]


