Abstract
A 65‐year‐old man was referred to our hospital for abdominal pain. He had a history of enterotomy with stone extraction for gallstone ileus. On abdominal computed tomography, a stone measuring 32 × 28 mm lodged in the jejunum was identified. He was diagnosed with gallstone ileus and treated using a nasal ileus tube. Four days after admission, computed tomography showed that the stone had passed into the rectum. The gallstone was spontaneously evacuated on the same day. A fistula with the gallbladder was found in the duodenal bulb. The patient's condition improved, and he was discharged 9 days after admission.
Keywords: cholecystoduodenal fistula, gallstone, ileus, spontaneous evacuation
1. INTRODUCTION
Ileus is often encountered in daily medical practice. It can be caused by various reasons, but rarely by gallstones. It can result from a gallstone passing into the intestinal tract, usually through a fistula between the gallbladder and duodenum. It accounts for only 1%‐4% of all intestinal obstructions.1 In the literature, the mortality associated with gallstone ileus ranges from 7% to 30%.2 Most patients generally require surgical management.3, 4 Here, we report a case of gallstone ileus that recurred after enterotomy with stone extraction, which was then spontaneously evacuated.
2. CASE REPORT
A 65‐year‐old man was referred to our hospital due to abdominal pain and vomiting. Two years ago, he had been diagnosed with gallstone ileus and underwent enterotomy of the jejunum with surgical extraction of the gallstone. The stone measured 42 × 28 mm in the computer tomography (CT) image. However, another stone remained in the gallbladder, and the patient did not undergo cholecystectomy.
On admission, his physical examination showed whole abdominal tenderness but no muscular defense. Laboratory data showed slightly elevated CRP level (0.83 mg/dL) and WBC count (9500/μL), but other results showed no remarkable deviations. In addition, arterial blood gas did not show acidosis. CT showed that a gallstone, which was previously confirmed, was no longer in the gallbladder but had lodged in the jejunum. The gallstone measured 32 × 28 mm in the CT image. In addition, consecutive expansion of the oral side of the intestinal tract was confirmed (Figure 1). However, areas of the intestinal wall with poor contrast or ascites were not observed. The patient had moderate to severe aortic regurgitation and a 55‐mm‐diameter ascending aortic aneurysm. The risk of surgery was high, and we decided to perform conservative treatment first. Therefore, a nasal ileus tube was immediately inserted.
Figure 1.
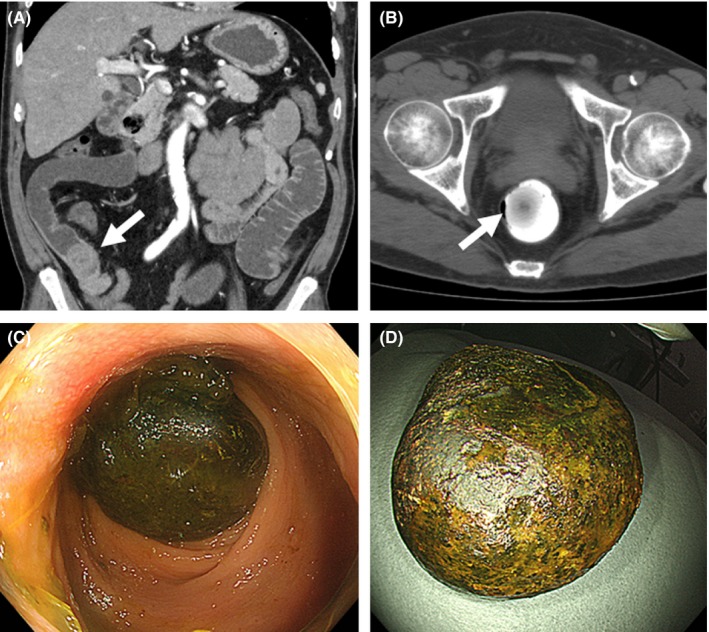
A, Computed tomography (CT) showing gallstone (arrow) lodged in the jejunum and intestinal dilation on the oral side of the intestine. The gallstone measured 32 × 28 mm in the CT image. B, The gallstone (arrow) passed into the rectum 4 d after admission. It is surrounded with the contrast medium. C, The gallstone confirmed using an endoscope in the rectum. D, The gallstone evacuated spontaneously
After insertion of the tube, the patient's symptoms were improved. Two days after admission, he had diarrhea several times. Four days after admission, CT showed that the gallstone had passed into the rectum, which was subsequently confirmed using colonoscopy. On the same day, the gallstone was spontaneously evacuated. Analysis of the calculus showed that the component of the stone was bilirubin 52%, cholesterol 43%, and calcium fatty acid 5%, respectively, which was consistent with gallstone.
The presence of cholecystoduodenal fistula was suspected in the CT image at the time of admission. On the following day of stone evacuation, a fistula in the posterior wall of the duodenal bulb measuring approximately 8 mm in diameter was confirmed using gastrointestinal endoscopy. A catheter was inserted into the fistula, and a contrast medium was injected. Through the fistula, the gallbladder and bile duct were imaged, and a cholecystoduodenal fistula was diagnosed. There were no residual gallstones in the gallbladder or bile duct, and no tumor was admitted into the gallbladder (Figure 2). The clinical course remained uneventful, and the patient was discharged 9 days after admission. Because there were no stones left in the gallbladder, the cholecystoduodenal fistula was not treated.
Figure 2.
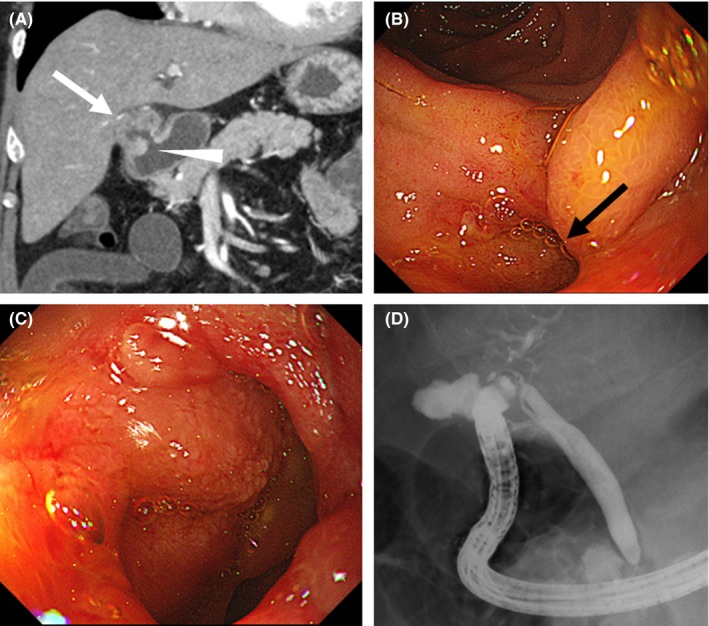
A, The presence of cholecystoduodenal fistula (arrowhead) was suspected in the computed tomography image at the time of admission. No tumor was found in the gallbladder (white arrow). B,C, Cholecystoduodenal fistula found in the posterior wall of the duodenal bulb (black arrow). D, Gallbladder and bile duct imaged using contrast medium injection from the fistula of the duodenal bulb
3. DISCUSSION
Gallstone ileus is a rare disease, which is reported in 0.3%‐0.5% of patients with gallstones.1 It is more common in females, and the ratio of occurrence in females to males is 3.5:1.5 The cholecystoduodenal fistula is caused by inflammations of the gallbladder. The inflamed gallbladder with stone adheres to the duodenum. Necrosis, ulceration, and perforation through the adherent area form fistula.6 Through this fistula, gallstones may enter the gastrointestinal tract. Depending on the size of the gallstones, they may cause mechanical intestinal obstruction, resulting in abdominal pain and vomiting. Most reports indicate that the gallstone must be >2.5 cm in diameter to cause gallstone ileus.7 For the diagnosis of gallstone ileus, CT is the gold standard tool to confirm the condition and guide its management.2
Most patients generally require surgical management for gallstone ileus.3, 4 Surgical operation methods include enterotomy with stone extraction alone (ES), enterotomy and cholecystectomy with fistula closure (EF), bowel resection alone (BR), and bowel resection with fistula closure. A retrospective study showed EF and BR were independently associated with higher mortality than ES, on multivariate analysis.8 And enterotomy with stone extraction remains the most popular surgical option;8 however, consistent with our case, there are some reports of spontaneous resolution of gallstone ileus, with patients passing the stones through the rectum,9 although there is no clear indicator of whether spontaneous evacuation of gallstones can be expected. Recurrence of gallstone ileus occurs in 5% of cases, with 85% within 6 months of the initial episode.10
In our case of recurrent gallstone ileus, enterotomy was performed 2 years previously for the first episode, but the gallstone spontaneously evacuated in the second episode. The second gallstone was smaller than the first, which is considered to be the key factor in the gallstone evacuating spontaneously. The evaluation of the cholecystoduodenal fistula is important for gallstone ileus, and it should be considered that gallstone ileus can recur if gallstones remain in the gallbladder, and in our case, the cholecystoduodenal fistula was 8 mm in diameter at the time of the endoscope observation, but there was a possibility that the fistula had become smaller by mucosal healing with the passage of time. Establishing an indicator of whether spontaneous evacuation of gallstone can be expected is desired. Although enterotomy with stone extraction alone remains the most popular operative method, it is essential to carefully monitor the long‐term effects of a persisting cholecystoduodenal fistula. We are following the patient with abdominal echo and contrast‐enhanced CT scan, especially paying attention to the occurrence of gallbladder tumor.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
ACKNOWLEDGEMENTS
The authors would like to thank all the staff involved in the treatment of the patient at Mito Saiseikai General Hospital. We would also like to thank Enago for the English language review.
Takahashi K, Kashimura H, Konno N , et al. Gallstone ileus with spontaneous evacuation: A case report. J Gen Fam Med. 2018;19:173–175. 10.1002/jgf2.196
REFERENCES
- 1. Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77:737–42. [DOI] [PubMed] [Google Scholar]
- 2. Chang L, Chang M, Chang HM, Chang AI, Chang F. Clinical and radiological diagnosis of gallstone ileus: a mini review. Emerg Radiol. 2018;25:189–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60:441–6. [PubMed] [Google Scholar]
- 4. Sesti J, Okoro C, Parikh M. Laparoscopic enterolithotomy for gallstone ileus. J Am Coll Surg. 2013;217:e13–5. [DOI] [PubMed] [Google Scholar]
- 5. Chatterjee S, Chaudhuri T, Ghosh G, Ganguly A. Gallstone ileus–an atypical presentation and unusual location. Int J Surg. 2008;6:e55–6. [DOI] [PubMed] [Google Scholar]
- 6. Fox PF. Planning the operation for cholecystoenteric fistula with gallstone ileus. Surg Clin North Am. 1970;50:93–102. [DOI] [PubMed] [Google Scholar]
- 7. Hussain Z, Ahmed MS, Alexander DJ, Miller GV, Chintapatla S. Recurrent recurrent gallstone ileus. Ann R Coll Surg Engl. 2010;92:W4–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Halabi WJ, Kang CY, Ketana N, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014;259:329–35. [DOI] [PubMed] [Google Scholar]
- 9. De Giorgi A, Caranti A, Moro F, et al. Spontaneous resolution of gallstone ileus with giant stone: a case report and literature review. J Am Geriatr Soc. 2015;63:1964–5. [DOI] [PubMed] [Google Scholar]
- 10. Martín‐Pérez J, Delgado‐Plasencia L, Bravo‐Gutiérrez A, et al. Gallstone ileus as a cause of acute abdomen. Importance of early diagnosis for surgical treatment. Cir Esp. 2013;91:485–9. [DOI] [PubMed] [Google Scholar]


