Abstract
Background
The increasing use of intraoperative neuromonitoring (IONM) in thyroid surgery has revealed the need to develop new strategies for cases in which a loss of signal (LOS) occurs on the first side of a planned total thyroidectomy.
Objectives
This study reviews the experience of the authors in using IONM for planned total thyroidectomy after LOS on the first thyroid lobe. The aims were to estimate the incidence of LOS on the first side of resection and to compare intraoperative strategies applied after this event.
Materials and Methods
Intermittent IONM was performed with stimulation of both the vagal nerve and the recurrent laryngeal nerve (RLN) (V1, R1, R2, V2). Patients underwent pre‐ and postoperative laryngoscopy. Before surgery, patients were informed that staged thyroidectomy might be required.
Results
This study analyzed 803 consecutive thyroid procedures. Of these, V2 LOS (<100 mcV) occurred after first lobe exeresis in 23 (2.8%) procedures. The surgical procedure was stopped in 20 cases (ie, staged thyroidectomy was performed). In three cases with malignancy and severe comorbidity (ASA score 3‐4), total bilateral thyroidectomy was performed as planned. No cases of bilateral RLN palsy occurred. Postoperative laryngoscopy confirmed RLN palsy in 21 of the 23 cases. All true positive patients received speech therapy. Patients who had false positive LOS (n = 2) or malignancy (n = 8) and patients who were symptomatic (n = 7) received completion thyroidectomy within 6 months. One patient received radioactive iodine therapy for hyperthyroidism. Two patients received follow up.
Conclusions
Neuromonitoring changes the surgical decision‐making process in a multidisciplinary manner. A shared decision‐making process involving the patient, anesthesiologist, and endocrinologist is suggested. In the case of intraoperative LOS on the first‐operated side in a planned total thyroidectomy, the thyroid surgeon essentially has three options for surgery on the contralateral side: 1) Perform staged thyroidectomy. This option is recommended in bilateral goiter, Graves' disease, or low‐risk thyroid carcinoma (differentiated or medullary thyroid carcinoma). The aim is to avoid bilateral vocal cord palsy. Two‐stage completion surgery is delayed until recovery of ipsilateral nerve function. 2) Perform subtotal resection on the contralateral side ventrally to the RLN plane at a safe distance from the nerve. The aim is to avoid further disease recurrence and revision surgery. 3) Perform total thyroidectomy as planned for advanced thyroid carcinoma (including undifferentiated thyroid carcinoma). The aim is to improve disease control through radioactive iodine therapy, radiation therapy, or target therapy immediately after surgery.
Level of Evidence
4
Keywords: Thyroid surgery, recurrent laryngeal nerve, nerve injury, staged thyroidectomy, loss of signal
INTRODUCTION
Bilateral vocal cord palsy (VCP) is among the most feared complications in thyroid surgery and may require emergent tracheotomy.1 Patients with bilateral VCP may develop severe symptoms such as breathlessness and stridor caused by upper airway obstruction or symptoms of aspiration caused by altered sensory innervation of the laryngeal mucosa or by ineffective motor innervation of the laryngeal muscles during laryngeal closure.1, 2, 3, 4, 5
Although intraoperative neuromonitoring (IONM) is considered the gold standard for verifying the functional status of the recurrent laryngeal nerve (RLN), unexpected intraoperative failure of the electromyography (EMG) signal (ie, loss of signal, LOS) is a common occurrence.6
The reported accuracy of IONM for predicting vocal function early after surgery is highly variable. The reported positive predictive value ranges from as low as 10% to as high as 90%.7, 8 This lack of diagnostic precision combined with the strong possibility of intraoperative normalization of the EMG signal as RLN function recovers raises doubts about the conventional strategy applied when LOS occurs, ie, terminating surgery on the affected side and continuing surgery on the bilateral side.
Algorithms for predicting vocal fold function early after surgery indicate that an intraoperative change in resection strategy may be desirable after LOS occurs in a planned total thyroidectomy.9 Here, the authors describe their experience in developing and applying strategies for responding to a loss of neuromonitoring signal on the first thyroid lobe in planned total thyroidectomy.
The aims were to estimate the incidence of LOS on the first side of resection and to evaluate the applicable intraoperative strategies.
METHODS
Patients
This prospective observational cohort study collected data from all patients who had received a scheduled total thyroidectomy with or without neck dissection at a single institution. The protocol was approved by the Institutional Review Board. All patients signed informed consent forms before undergoing surgery. No authors of this study had financial relationships with manufacturers of nerve‐monitoring systems.
Figure 1 depicts a flow chart of the study procedure. Recruitment criteria for the study were the following: A) Pre‐ and postoperative laryngoscopy performed 24 hours before surgery and on postoperative day 1. B) Surgery beginning on the dominant side, ie, on the side with nodules that had a malignancy, a suspected malignancy, or an abnormally large size. C) A signed preoperative consent form specifying that a staged procedure may be required in the case of LOS on the initially operated side. D) Referral for total bilateral thyroidectomy with or without neck dissection. Any questions raised by the patient were resolved in preoperative consultations with a multidisciplinary team comprising the endocrinologist, surgeon, and anesthesiologist assigned to perform the surgery. Patients were excluded if they had a history of lobectomy since LOS in patients with anatomically intact RLN does not affect the operative resection strategy in the case of a planned one‐sided thyroid procedure. Other exclusion criteria were previous parathyroid surgery, preexisting VCP, refusal to undergo surgery (Fig. 1), and personal experience in using IONM technology.
Figure 1.
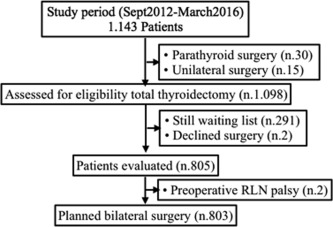
Flow chart of patient progress through different phases of the study (n.803)RLN: recurrent laryngeal nerve.
IONM Standards
In all patients, intermittent IONM (NIM‐Response 3.0, Medtronic, Jacksonville, Florida, USA) was performed according to standard procedures for equipment setup, induction and maintenance anesthesia, and verification of tube positioning. The EMG definitions developed by the International Neural Monitoring Study Group (INMSG) were applied.6 The definition of an intraoperative LOS assumed a correct initial signal response (Table 1). An LOS was assumed in the event of intraoperative signal failure or EMG signal below 100 μV with a primary intact signal and adequate stimulation with 1–2 mA.6
The IONM troubleshooting algorithm was performed in the following two steps (Fig. 2): A) Exclusion of anesthesia‐induced neuromuscular blockade and exclusion of technical disturbances such as dislocation of neural electrodes, cable connections, tubes, or surface electrodes; and B) Stimulation of the ipsilateral RLN before its entry into the larynx and stimulation of the ipsilateral vagal nerve (VN) followed by EMG verification of the stimulation response and possibly palpation of the dorsal larynx wall (laryngeal twitch) as a positive sign of equilateral action of the vocalis muscle.6 The response to stimulation at each site was interpreted as follows: Positive laryngeal twitch at all stimulation sites (Fig. 2) was considered a “recording site” error, ie, dislocation of the EMG endotracheal tube. Recording site errors were corrected by adjusting the tube position.6
A normal EMG and/or positive laryngeal twitch during RLN stimulation at the point of entry into the larynx simultaneous with absence of an EMG response or laryngeal twitch under VN stimulation was interpreted as an actual loss of function in the ipsilateral RLN (Fig. 2). In these nerve disorders, the nerve lesions could usually be localized by “mapping” (type 1, point/segmental injury).10, 11, 12
Lack of an EMG response and lack of laryngeal twitch regardless of stimulation site (ie, RLN or VN) was interpreted as a diffuse nervous disorder (type‐2 global injury) if stimulation was correct and if the above causes could be excluded.11, 12
In the case of any uncertainty regarding equipment function or tube position, the contralateral VN was stimulated (Fig. 2). If the contralateral VN showed intact function, a disturbed nerve function was assumed in the absence of a stimulation response from the side in question.6
Table 1.
Definition of EMG Signal Loss
|
EMG = electromyography.
Figure 2.
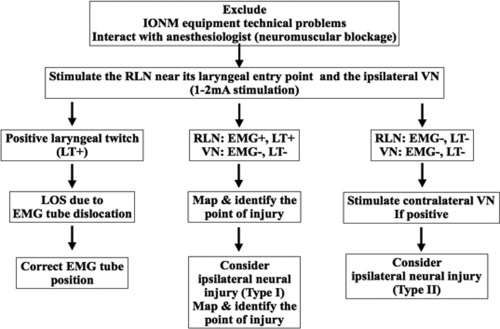
IONM troubleshooting algorithm
RLN: recurrent laryngeal nerve; IONM: intraoperative neural monitoring; VN: vagal nerve; LT: laryngeal twitch; LOS: loss of signal; EMG: electromyography.
Primary and Secondary Outcome Measures
The primary outcome measure was the incidence of LOS on the first side of resection.
The secondary outcome measures were the ratio of monolateral to bilateral RLN injuries and the ratio of transient to permanent RLN injuries. A permanent RLN injury was defined as an RLN dysfunction that persisted for 12 months or longer.10 Finally, this study described A) the strategies applied in cases of LOS on the first side of a planned total thyroidectomy, and B) methods and timing of completion thyroidectomy.
Statistical Analysis
All patient data were prospectively collected with a dedicated electronic Microsoft Office Access Data Base (Microsoft Corp, Redmond, WA, USA). Unless otherwise stated, all data were expressed as median and range. Statistical analyses were performed with SPSS, release 20.0 for Windows (SPSS Inc, Chicago, Illinois, USA). A P value less than .05 was considered statistically significant.
RESULTS
Figures 1 and 3 show that this study included 803 planned bilateral procedures. Figure 3 compares the prevalence of LOS between the first side and second side of resection (2.86% and 2.1%, respectively). In Tables 2 and 3, patient characteristics and RLN characteristics are stratified as patients with uneventful bilateral procedures, patients with LOS, and patients with false negative EMG results. No significant features were identified (Tables 2 and 3). The injury was type 1 in 91% (21 of 23) of procedures with first side LOS.
Figure 3.
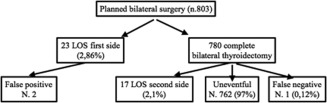
Prevalence of neuromonitoring signal loss in planned total thyroidectomy LOS: loss of signal.
Table 2.
Patient Characteristics
| LOS first side (n=23) | Total thyroidectomy (n=780) | Uneventful (n = 762) | LOS second side (n=17) | False negative (n=1) | P | |
|---|---|---|---|---|---|---|
| Age (yrs) Mean | 44.5 | 47.9 | 47.6 | 48.9 | 61 | .079 |
| Range | 11–79 | 14–83 | 14–83 | 22–69 | – | – |
| Gender (M/F, %) | 6 (26%) / 17 (74%) | 170 (21.7%) / 610 (79.3%) | 161 (21%) / 609 (79%) | 5 (29%) / 12(70%) | Male | .53 |
| Planned surgery | 11 (47%) | 680 (87.1%) | 672 (88.1%) | 12 (70%) | – | .321 |
| TT | 10 (43%) | 70 (8.9%) | 65 (8.5%) | 4 (23%) | 1 | .255 |
| TT + CND TT + CND + LND | 2 (8.6%) | 30 (3.8%) | 25 (3.2%) | 1 (5%) | – | .5 |
| Histology Goiter | 11 (47%) | 639 (81.9%) | 630 (80%) | 10 (58%) | – | .3 |
| PTC | 8 (34.7%) | 65 (8.3%) | 60 (8%) | 5 (29%) | 1 | .678 |
| MTC | 1 (4.3%) | 5 (0.6%) | 1 (0.5%) | 0 | – | .544 |
| Graves Disease | 3 (13%) | 71 (9.1%) | 71 (9%) | 2 (11%) | – | .43 |
CND = central node dissection; LND = lymph node dissection; LOS = loss of signal; MTC = medullary thyroid cancer; PTC = papillary thyroid cancer; TT = total thyroidectomy.
Table 3.
RLN Features
| LOS first side (n = 23) | Total thyroidectomy (n = 780) | Uneventful (n = 762) | LOS second side (n = 17) | False negative (n = 1) | P | |
|---|---|---|---|---|---|---|
| Ramification | 15 (65%) | 401 (51%) | 391 (51%) | 10 (58%) | 0 | .052 |
| Palsy (right/left) | 10/13 | – | – | 9/8 | 1/0 | .530 |
| NRLN | – | 2 | 2 | – | – | – |
| ITA entrapment | 12 (52%) | 202 (25%) | 212 (26%) | 9 (57%) | – | .066 |
ITA = inferior thyroid artery; LOS = loss of signal; NRLN = non recurrent laryngeal nerve.
Intraoperative Strategy
Figure 4 shows that LOS occurred on the first resected side in 23 procedures. Of these, no further resection was performed on the contralateral side in 20 procedures (85%). In this group, VCP on the first resected side was confirmed early after surgery in 19 (95%) patients, VCP was transient monolateral in 18 patients, and VCP was permanent monolateral in one patient. No patients in this group had bilateral VCP. One (5%) false positive LOS was detected (type 2 LOS).
Figure 4.
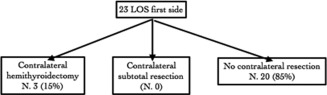
Intraoperative strategy after LOS on first side of resection
LOS = loss of signal.
Figure 4 shows that three (15%) patients received contralateral hemithyroidectomy. No patients received contralateral subtotal resections. These strategies were applied after preoperative discussions involving the patient, endocrinologist and anesthesiologist. Bilateral malignancy was confirmed in all three patients. One patient also had a high ASA3 score. Postoperative VCP was transient monolateral in two cases and permanent monolateral in one. No false positive LOS or bilateral VCP occurred in this second group of patients. All patients with true positive LOS received early speech therapy.
Completion Thyroidectomy
In 17 (85%) patients, completion thyroidectomy was performed after recovery of transient VCP (Fig. 5). In 95% of completion thyroidectomies, the surgery was performed within 6 months after the first surgery (Fig. 6). Three (15%) patients declined to undergo thyroidectomy after consultation with the multidisciplinary surgical team. Two patients had transient monolateral palsy, and one had permanent monolateral palsy. One patient with Graves' disease received ablation. Two other patients required further follow‐up of multinodular goiters.
Figure 5.
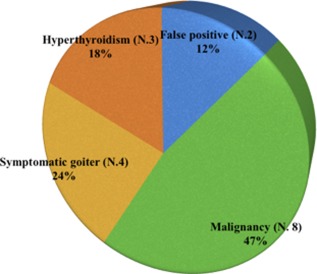
Indications for completion thyroidectomy (n.17)
Figure 6.
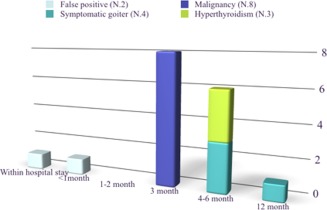
Timing of completion thyroidectomy (n.17)
DISCUSSION
This aim of this study was to describe the incidence of LOS on the first side of resection and the consequent intraoperative strategy (Figs. 1, 2, 3, 4, 5, 6, 7). An LOS that occurs with an anatomically intact RLN does not affect the resection strategy in the case of a planned one‐sided thyroid procedure. The situation is very different when LOS occurs during surgery on the first side of a planned bilateral thyroidectomy.
Figure 7.
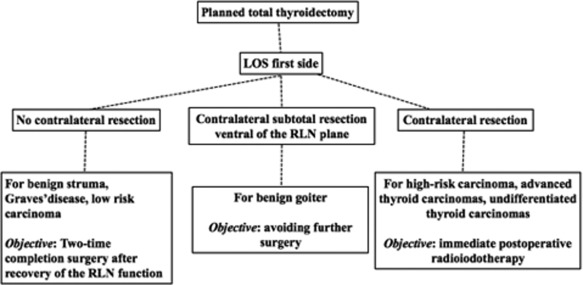
Surgical options after intraoperative signal loss on first operated side in planned total thyroidectomy (adapted from REF 9, Schneider R, Lorenz K, Sekulla C, Machens A, Nguyen‐Thanh P, Dralle H. Surgical strategy during intended total thyroidectomy after loss of EMG signal on the first side of resection. Chirurg 2015;86:154–163)LOS: loss of signal; RLN: recurrent laryngeal nerve.
The findings of this study showed that IONM information affected decision making by the multidisciplinary team. For example, when a reduced EMG signal was observed on the first side, some surgeons decided not to perform total thyroidectomy to avoid the risk of bilateral RLN injury. A first side LOS occurred in 23 (2.8%) of the cases. In 20 of 23 cases, the surgical procedure was stopped at the first dominant thyroid lobe side.
This observational cohort study also highlights the importance of a dedicated informed consent form that emphasizes a shared decision‐making process involving the patient, anesthesiologist, and endocrinologist. In three cases, we proceeded to total thyroidectomy due to thyroid malignancy (advanced multifocal bilateral cancer, cLN+) and comorbidity (ASA score 3–4). This strategy was discussed in the preoperative consent process. The discussion of risks specifically included the risk of tracheotomy.
Thus, in the case of intraoperative LOS on the first‐operated side in a planned total thyroidectomy, the thyroid surgeon essentially has three options for surgery on the contralateral side if RLN function is intact. Figure 7 summarizes the three options.13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25
Perform staged surgery on the second side. This option is recommended in bilateral goiter, Graves' disease, or low risk thyroid carcinoma (differentiated and medullary thyroid carcinomas). The aim is to avoid bilateral VCP. Two‐stage completion surgery is delayed until recovery of ipsilateral nerve function. This strategy was applied in 73% of patients with first side LOS.
Perform subtotal resection on the contralateral side ventrally to the RLN plane at a safe distance from the nerve. The aim is to avoid further disease recurrence and revision surgery. This strategy was not performed in this series of patients (0%).
Perform total thyroidectomy as planned for advanced thyroid carcinoma (including undifferentiated thyroid carcinoma). The aim is to improve disease control through radioactive iodine therapy, radiation therapy, or targeted therapy immediately after surgery. This strategy was applied in 13% of patients LOS on the initially operated side. After LOS on the initially operated side, resection of the contralateral side is technically possible if the surgeon has sufficient experience.9, 14, 20, 21, 22, 23, 24, 25 However, such a procedure should be discussed in detail with the patient and weighed against the possible need for a two‐stage procedure.
All 17 patients who underwent completion thyroidectomy after a staged procedure suffered from transient RLN lesions. No cases had transient or permanent bilateral RLN palsy. Figure 6 shows that completion thyroidectomy was scheduled after speech therapy and recovery of the VC in different time period. Studies show that more than 80% of functionally impaired RLNs completely recover within the first 75 days after injury. Therefore, a 2‐day completion operation can be performed after 3 months with no risk of bilateral VCP.9, 14, 20, 21, 22, 23, 24, 25 According to the literature, nerve function completely recovers within 3 to 12 months.9, 14, 20, 21, 22, 23, 24, 25
Managing patients who develop permanent RLN injury and who require complete thyroidectomy is challenging. In this series of 23 patients with LOS, two patients had definitive monolateral VC palsy. In one case, we proceeded without staging (in accordance with the strategy planned before surgery). In the second case of permanent RLN injury, a staged procedure was performed. Completion thyroidectomy was not performed because the patient had a benign multinodular goiter and the multidisciplinary board and patient convert for a follow‐up. In the event that RLN injury does not recover within 6 months after the initial surgery, further planning and discussion involving the multidisciplinary team and the patient is essential. The possible need for further observation or further radioactive iodine therapy should also be discussed in detail. If a completion surgery is unanimously deemed necessary, we suggest A) clearly informing the patient that tracheotomy may be required, B) seeking care from a healthcare provider with experience in tertiary surgical care and technology (ie, IONM), and C) obtaining patient consent to an extended and protracted period of preparation for a second intervention with pre‐operative respiratory rehabilitation and preoperative antiedemigens or corticosteroids. Before the patient consents to a second intervention, however, the patient should be advised that a preoperative cordectomy may be required.
In the event of LOS, including LOS on the contralateral side in completion thyroidectomy, tracheotomy should not be performed immediately. First, extubation should be attempted with immediate clinical evaluation. A laryngeal examination should be performed to determine the position of the VC and the respiratory space. If breathlessness and stridor are present, the recommended protocol is new intubation and remote reevaluation at 72 hours after infusion of antiedemigens and corticosteroids. Tracheotomy should be performed if no improvement is observed after the second extubation.
Due to the rare but feared complication of postoperative bilateral VCP, demonstrating that IONM significantly reduces postoperative paresis rates in comparison to visual RLN identification alone is very difficult.7, 9 When LOS occurs on the first side, terminating surgery without contralateral resection significantly reduces the occurrence of bilateral VCP (P = .017).20 A survey of thyroid surgeons in 1119 clinics in Germany revealed that 94% of the surgeons would change their resection strategy for the second side if LOS occurred on the first operated side; 85% said they would definitively end the resection on the first side; 9% said they would reduce the extent of resection on the contralateral side; only 6% said they would continue resection on both sides as planned.14
We believe that two essential requirements for a thyroidectomy surgeon are skills and experience in A) using neuromonitoring technology and B) changing the resection strategy intraoperatively in the case of an LOS on the first (dominant) operated side.9 In cases of an ipsilaterally derivable stimulation signal and EMG of the VN after resection of the thyroid gland, the probability of intact RLN function after surgery is very high (92–100%).7 In contrast, the positive predictive value is low and ranges between 10% and 90%.7, 8 This high proportion of false‐positive findings (ie, LOS and normal early postoperative RLN function) can be improved by a comprehensive intraoperative error search.7, 8 According to INMSG guidelines, a systematic review of the IONM system is mandatory when LOS occurs.6 When the ipsilateral laryngeal musculature is triggered by nerve stimulation (laryngeal twitch) or when the contralateral VN is not stimulable, a technical disturbance has occurred in the area where the measuring procedure is performed, ie, the recording site.6 In the absence of ipsilateral laryngeal twitch, a technical disturbance has occurred in the area where stimulation is applied, ie, the stimulation site (Fig. 2). When the contralateral VN can be stimulated, the absence of an ipsilateral laryngeal twitch indicates a true functional disorder of the ipsilateral RLN.6
Analyses of our data revealed the two fundamental limitations of intraoperative control of RLN function (Tables 2 and 3):
False negative findings with intact RLN function in IONM and VCP after surgery. Although rare (one case occurred in the present series), these pathological changes in vocal fold function are undetectable by IONM as revealed by the data in Périé et al. in a report of bilateral VCP in two patients.24
False‐positive findings with LOS and normal postoperative vocal cord function (two cases in the present series). The recently proposed alternative strategy of waiting for intraoperative signal recovery and contralateral continuation of the planned operation is based on data showing that signal recovery occurs within 20 min in 90% of cases.9, 14, 20, 21, 22, 23, 24, 25 However, the false‐positive rate is reportedly as high as 85%, which inevitably raises the question of whether troubleshooting is sufficient. Abortion of surgery after resection is completed on the first operated side would then indeed be associated with an excessively high proportion of unnecessary two‐stage thyroidectomies. Another question is the extent to which the time of LOS and the time until signal recovery can be predicted by intermittent neuromonitoring. Further studies of continuous neuromonitoring are needed to clarify these two aspects and the definition of signal recovery.26
In conclusion, this study revealed that, after LOS, VCP risk early after surgery is as high as 95%. In this case, the decision to perform a further procedure must consider the underlying thyroid disease of the patient and the expertise of the surgeon. The therapeutic algorithm described here (Fig. 7) presents three surgical options after LOS on the first operated side. Since more than 80% of nervous system disorders completely regress, a two‐stage procedure is recommended. High false‐positive rates indicate the need for internal review of clinical standards to avoid unnecessary two‐stage thyroidectomy. Further studies are needed to investigate the potential for EMG signal recovery after an intraoperative LOS and its importance for the progress of an operation performed using continuous neuromonitoring. Exceptional situations in advanced thyroid carcinomas must be discussed extensively with the patient before surgery. A noted limitation of this prospective study is that it did not include an appropriate comparison cohort.
COMPLIANCE WITH ETHICAL STANDARDS
Funding: This study was supported by grants from Kaohsiung Medical University, Taiwan (KMUH106‐6R49) and Ministry of Science and Technology (MOST 106‐2314‐B‐037‐042‐MY2), Taiwan
Conflict of Interest: The authors have no financial relationships with the surgical industry and have no other conflicts of interest to disclose.
Ethical approval: This study was approved by the Local Institutional Ethics Committee
Informed consent: Informed consent was obtained from all participants in this study.
Author Contributions: (I) Conception and design of study: Gianlorenzo Dionigi, Che Wei Wu; (II) Administrative support of study: Hoon Yub Kim, Hui Sun, Antonina Catalfamo, Mattia Portinari; (IV) Collection and assembly of data: Hoon Yub Kim; (V) Analysis and interpretation of data: All Authors (VI) Preparation of manuscript: All Authors; (VII) Final approval of manuscript: All Authors.
Parts of this work were presented at the 3rd World Congress on Thyroid Cancer, July 27–30, 2017 in Boston, Massachusetts, U.S.A.
Contributor Information
Hui Sun, Email: thyroidjl@163.com.
Gianlorenzo Dionigi, Email: gdionigi@unime.it.
BIBLIOGRAPHY
- 1. Hermann M, Keminger K, Kober F, Nekahm D. Risk factors in recurrent nerve paraysis: a statistical analysis of 7566 cases of struma surgery. Chirurg 1991;62(3):182–187; discussion 188. [PubMed] [Google Scholar]
- 2. Rosato L, Avenia N, Bernante P, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg 2004;28(3):271–276. [DOI] [PubMed] [Google Scholar]
- 3. Gilony D, Gilboa D, Blumstein T, et al. Effects of tracheostomy on well‐being and body‐image perceptions. Otolaryngol Head Neck Surg 2005;133(3):366–371. [DOI] [PubMed] [Google Scholar]
- 4. Hirano M, Ohala J, Vennard W. The function of laryngeal muscles in regulating fundamental frequency and intensity of phonation. J Speech Hear Res 1969;12(3):616–628. [DOI] [PubMed] [Google Scholar]
- 5. Nouraei SA, Whitcroft K, Patel A, Chatrath P, Sandhu GS, Kaddour H. Impact of unilateral vocal fold mobility impairment on laryngopulmonary physiology. Clin Otolaryngol 2014;39(4):210–215. [DOI] [PubMed] [Google Scholar]
- 6. Randolph GW, Dralle H; International Intraoperative Monitoring Study Group , et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121:S1–S16. [DOI] [PubMed] [Google Scholar]
- 7. Dralle H, Sekulla C, Lorenz K, et al. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 2008;32:1358–1366. [DOI] [PubMed] [Google Scholar]
- 8. Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg 2004;240:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schneider R, Lorenz K, Sekulla C, Machens A, Nguyen‐Thanh P, Dralle H. Surgical strategy during intended total thyroidectomy after loss of EMG signal on the first side of resection. Chirurg 2015;86(2):154–163. [DOI] [PubMed] [Google Scholar]
- 10. Dionigi G, Boni L, Rovera F, Rausei S, Castelnuovo P, Dionigi R. Postoperative laryngoscopy in thyroid surgery: proper timing to detect recurrent laryngeal nerve injury. Langenbecks Arch Surg 2010;395(4):327–331. [DOI] [PubMed] [Google Scholar]
- 11. Chiang FY, Lee KW, Chen HC, et al. Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg 2010;34(2):223–229. [DOI] [PubMed] [Google Scholar]
- 12. Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW. The mechanism of recurrent laryngeal nerve injury during thyroid surgery‐‐the application of intraoperative neuromonitoring. Surgery 2008;143(6):743–749. [DOI] [PubMed] [Google Scholar]
- 13. Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 2009;96(3):240–246. [DOI] [PubMed] [Google Scholar]
- 14. Dralle H, Sekulla C, Lorenz K, Nguyen Thanh P, Schneider R, Machens A. Loss of the nerve monitoring signal during bilateral thyroid surgery. Br J Surg 2012;99(8):1089–1095. [DOI] [PubMed] [Google Scholar]
- 15. Ho Y, Carr MM, Goldenberg D. Trends in intraoperative neural monitoring for thyroid and parathyroid surgery amongst otolaryngologists and general surgeons. Eur Arch Otorhinolaryngol 2013;270:2525–2530. [DOI] [PubMed] [Google Scholar]
- 16. Dionigi G, Lombardi D, Lombardi CP, et al; Working Group for Neural Monitoring in Thyroid and Parathyroid Surgery in Italy . Intraoperative neuromonitoring in thyroid surgery: a point prevalence survey on utilization, management, and documentation in Italy. Updates Surg 2014;66(4):269–276. [DOI] [PubMed] [Google Scholar]
- 17. Dralle H, Lorenz K, Machens A. Verdicts on malpractice claims after thyroid surgery: Emerging trends and future directions. Head Neck 2012;34(11):1591–1596. [DOI] [PubMed] [Google Scholar]
- 18. Snyder SK, Lairmore TC, Hendricks JC, Roberts JW. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg 2008;206(1):123–130. [DOI] [PubMed] [Google Scholar]
- 19. Dionigi G, Alesina PF, Barczynski M, et al. Recurrent laryngeal nerve injury in video‐assisted thyroidectomy: lessons learned from neuromonitoring. Surg Endosc 2012;26(9):2601–2608. [DOI] [PubMed] [Google Scholar]
- 20. Goretzki PE, Schwarz K, Brinkmann J, Wirowski D, Lammers BJ. The impact of intraoperative neuromonitoring (IONM) on surgical strategy in bilateral thyroid diseases: is it worth the effort? World J Surg 2010;34(6):1274–1284. [DOI] [PubMed] [Google Scholar]
- 21. Sadowski SM, Soardo P, Leuchter I, Robert JH, Triponez F. Systematic use of recurrent laryngeal nerve neuromonitoring changes the operative strategy in planned bilateral thyroidectomy. Thyroid 2013;23(3):329–333. [DOI] [PubMed] [Google Scholar]
- 22. Dionigi G, Frattini F. Staged thyroidectomy: time to consider intraoperative neuromonitoring as standard of care. Thyroid 2013;23:906–908. [DOI] [PubMed] [Google Scholar]
- 23. Melin M, Schwarz K, Lammers BJ, Goretzki PE. IONM‐guided goiter surgery leading to two‐stage thyroidectomy‐indication and results. Langenbecks Arch Surg 2013;398:411–418. [DOI] [PubMed] [Google Scholar]
- 24. Périé S, Aït‐Mansour A, Devos M, et al. Value of recurrent laryngeal nerve monitoring in the operative strategy during total thyroidectomy and parathyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis 2013;130:131–136 [DOI] [PubMed] [Google Scholar]
- 25. Sitges‐Serra A, Fontané J, Dueñas JP, et al. Prospective study on loss of signal on the first side during neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy. Br J Surg 2013;100:662–666. [DOI] [PubMed] [Google Scholar]
- 26. Schneider R, Randolph GW, Sekulla C, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck 2013;35:1591–1598 [DOI] [PubMed] [Google Scholar]


